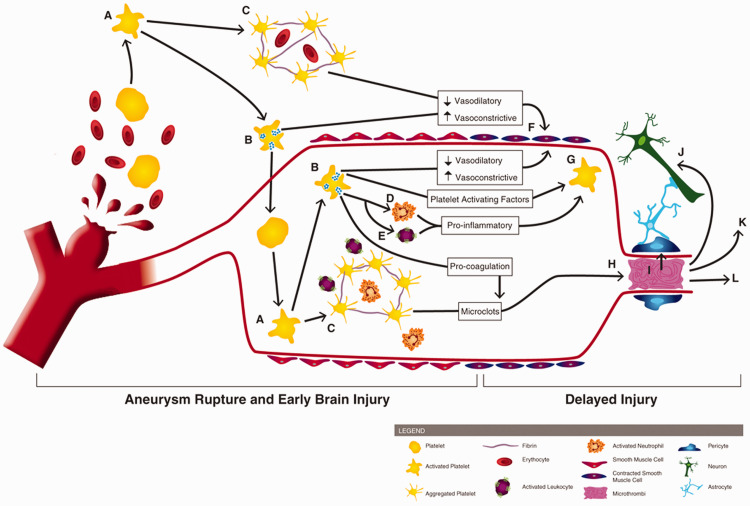
Figure 1.
Involvement of platelets in early brain injury and the pathogenesis of delayed cerebral ischemia. Following aneurysm rupture, erythrocytes and platelets are spilled into the subarachnoid space. Upon exposure to the extracellular space (and its matrix proteins, collagen and laminin), platelets become activated (A) Activated platelets degranulate (B) and form aggregates which can contain erythrocytes and immune cells (C). Platelet degranulation can activate intraluminal platelets (thereby propagating platelet activation, degranulation, and aggregation), neutrophils (D) and leukocytes (E). Activated platelets reduce their vasodilation mechanisms and release vasoconstrictive molecules, promoting large artery vasospasm (F). Degranulating platelets, along with activated leukocytes/neutrophils, exacerbate platelet activation (G). Pro-coagulant factors, released by platelets, promotes microclot formation which can deposit within brain microvessels (H). Platelet aggregates and microthrombi in the microvessels can induce pericyte constriction (I), cause neurotoxicity (J), initiate cortical spreading depolarization (K), and occlude blood flow, thereby reducing cerebral blood flow and causing development of delayed infarctions (L).