Abstract
Suppressing inflammation has been the primary focus of therapies in autoimmune rheumatic diseases (AIRDs), including rheumatoid arthritis and systemic lupus erythematosus. However, conventional therapies with low target specificity can have effects on cell metabolism that are less predictable. A key example is lipid metabolism; current therapies can improve or exacerbate dyslipidemia. Many conventional drugs also require in vivo metabolism for their conversion into therapeutically beneficial products; however, drug metabolism often involves the additional formation of toxic by-products, and rates of drug metabolism can be heterogeneous between patients. New therapeutic technologies and research have highlighted alternative metabolic pathways that can be more specifically targeted to reduce inflammation but also to prevent undesirable off-target metabolic consequences of conventional antiinflammatory therapies. This Review highlights the role of lipid metabolism in inflammation and in the mechanisms of action of AIRD therapeutics. Opportunities for cotherapies targeting lipid metabolism that could reduce immunometabolic complications and potential increased cardiovascular disease risk in patients with AIRDs are discussed.
Introduction
The inflammation associated with autoimmune rheumatic diseases (AIRDs), including rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE), is dependent on multiple immune cell subsets within disease-specific settings, each having different metabolic demands (1). For example, effector T cells are dependent on glycolytic metabolism for their growth and effector functions, whereas regulatory T cells utilize lipids via mitochondrial β-oxidation and the generation of ATP through oxidative phosphorylation (OXPHOS) (2). Naive B cells are maintained in a reduced metabolic state, while their activation relies on metabolic programming toward OXPHOS (3). Similarly, during inflammation, inflammatory M1 macrophages use glycolysis, whereas more antiinflammatory M2 macrophages typically use β-oxidation (4). Autoinflammatory responses in AIRDs have high energy demands and involve elevated lipogenesis, glucose and glutamine metabolism, and a switch toward cellular glycolysis from OXPHOS for energy metabolism. For example, hypoxia in the RA synovium induces chronic T cell mitochondrial hyperpolarization associated with increased glucose metabolism and ATP synthesis, and in SLE patients and lupus-prone mice, chronically activated T cells have increased mitochondrial glucose oxidation and hyperpolarization, as reviewed previously (1, 5). Many of the current therapies for AIRDs influence lipid metabolic pathways to exert their therapeutic benefit; furthermore, lipid metabolism could play a role in the pathogenesis of AIRDs and associated comorbidities. This Review discusses lipid metabolism in inflammation and mechanisms of action of AIRD therapeutics, addresses the on- and off-target metabolic effects induced by these therapies, and highlights opportunities for cotherapies targeting lipid metabolism that could benefit patients, with a focus on cardiovascular disease (CVD) risk, an important comorbidity in patients with AIRDs.
Lipid metabolic pathways in inflammation
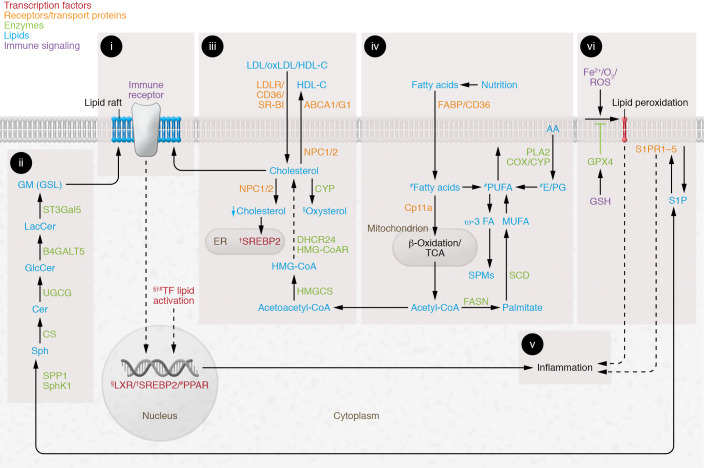
Lipid metabolism is a crucial aspect of cellular metabolism and effective immune responses; lipids derived from both de novo biosynthesis and exogenous sources are essential for fuel and growth and as membrane components, and mediate cell signaling (6), as summarized in Figure 1. Aspects of lipid metabolism that could contribute to disease pathogenesis and associated comorbidities in patients with AIRDs and serve as therapeutic targets are outlined below.
Immune cell lipid membranes and dyslipidemia
Immune cell plasma membranes comprise a phospholipid bilayer containing highly ordered areas enriched in glycosphingolipids and cholesterol, called lipid rafts. Immune cell surface receptors (including T cell and B cell receptors and costimulatory molecules) reside within lipid rafts and facilitate appropriate cell signaling in response to antigen or other cellular ligands (refs. 7–9 and Figure 1, A–C). Lipid rafts are altered in SLE, in which an increase in both cell membrane glycosphingolipids and cholesterol attributable to increased cellular lipid synthesis is associated with increased T cell and B cell receptor signaling and ultimately activation and inflammation (10, 11). Circulating lipids also play a role in immune cell function, through lipid uptake from VLDL or LDL via the VLDL or LDL receptor (VLDLR or LDLR), respectively, or from HDL via scavenger receptor class B type I (SR-BI) and CD36; or through lipid efflux to HDL or apolipoprotein A1 via ATP-binding cassette transporter A1 (ABCA1) and ABCG1. Both uptake and efflux influence cellular lipid burden and function (ref. 12 and Figure 1C). This is of particular importance in autoimmunity, where dyslipidemia and cardiovascular complications are common (13). Many studies report altered lipoprotein metabolism in AIRDs. This includes reduced serum total cholesterol, triglycerides, and LDL-cholesterol (LDL-C) in patients with untreated RA that increase when patients are treated (the so-called lipid paradox in RA; ref. 14), and elevated LDL-C and medium-chain/free fatty acids and reduced HDL and long-chain fatty acids in SLE (15–18). Interestingly, a dysfunctional proinflammatory HDL, lacking the antioxidant capacity of conventionally cardioprotective HDL, is described in 48.2% of women with SLE (15), and in patients with active RA (19), highlighting the prevalence of this form of HDL in AIRDs that is rarely measured and could be associated with elevated cardiovascular risk.
Figure 1. Summary of lipid metabolism pathways important for inflammation.
(i) Lipid rafts: cholesterol- and glycosphingolipid (GSL)-enriched cell signaling platforms. (ii) De novo GSL biosynthesis: differential expression influences immune receptor–mediated signaling and cell function. (iii) Intracellular cholesterol is regulated by liver X receptor (LXR) and sterol regulatory element–binding protein 2 (SREBP-2) (see v). LXR activation by oxysterols induces cholesterol efflux (ABCA1, ABCG1) and reduces lipid uptake (LDLR, VLDLR, SR-BI, CD36). Niemann-Pick type C1 (NPC1) and NPC2 regulate lysosomal/late endosomal trafficking/recycling of intracellular lipids. SREBP-2 opposes LXR and promotes cholesterol biosynthesis and uptake (HMGCoAR, LDLR). (iv) Nutrition influences fatty acid composition and metabolism. Fatty acids are metabolized to produce energy (ATP) by mitochondrial β-oxidation and TCA. Monounsaturated fatty acids (MUFAs) are synthesized via acetyl-CoA, fatty acid synthase (FASN), and stearoyl-CoA desaturase (SCD). Polyunsaturated fatty acids (PUFAs), diet-derived or biosynthesized in vivo, influence arachidonic acid (AA) metabolism. PUFAs are precursors to triglycerides, phospholipids in plasma membrane, second messengers, hormones, and ketone bodies. Prostaglandins (PGs) are produced following AA release from membrane phospholipids. Downstream PG signaling and eicosanoids have direct metabolic effects on immune cells via PPARs, mediating antiinflammatory effects and modulating LXRs (see v). Omega-3 (ω-3) PUFAs are enzymatically converted to antiinflammatory resolvins (specialized pro-resolving mediators [SPMs]). (v) Lipid metabolism activates transcription factors and influences inflammation via multiple mechanisms (see text). (vi) PUFA phospholipid peroxidation is induced by iron overload and ROS. Products of lipid peroxidation are eliminated via glutathione peroxidase-4 (GPX4); clearance defects induce cell membrane damage and ferroptosis. Sphingosine 1-phosphate (S1P) is derived from membrane phospholipids; activation via binding to S1P receptors (S1PR1–5) initiates immune cell localization to inflammatory sites and T cell differentiation. §, †, and # indicate processes activating LXR, SREBP2, or PPARs, respectively. Other abbreviations: B4GALT5, β-1,4-galactosyltransferase-5; Cer, ceramide; CS, ceramide synthase; DHCR24, 24-dehydrocholesterol reductase; FABPs, fatty acid–binding proteins; GlcCer, glucosylceramide; GM, GM1 ganglioside; GSH, glutathione; HMGCS, 3-hydroxy-3-methylglutaryl–CoA synthase-1; LacCer, lactosylceramide; ox, oxidized; Sph, sphingosine; SphK1, sphingosine kinase-1; SPP1, S1P phosphohydrolase-1; SR-BI, scavenger receptor class B type I; ST3Gal5, ST3 β-galactoside α-2,3-sialyltransferase-5; UGCG, UDP-glucose ceramide glucosyltransferase.
Pro- and antiinflammatory lipid metabolism
Proinflammatory lipids including eicosanoids contribute to some of the typical clinical symptoms associated with many AIRDs, such as joint pain, stiffness, and swelling (ref. 20 and Figure 1D). Eicosanoids are produced following the phospholipase A2–mediated release of arachidonic acid from membrane phospholipids (21). Arachidonic acid (an essential polyunsaturated omega-6 fatty acid) is subsequently converted into active metabolites by cyclooxygenase (COX), lipoxygenase, and cytochrome p450 (CYP) enzymes (20, 22). Downstream eicosanoid signaling can have a direct metabolic effect on immune cell subsets via the modulation of PPARs, nuclear hormone receptors that mediate antiinflammatory effects and modulate liver X receptors (LXRs), regulators of cholesterol homeostasis (23). Prostaglandin signaling can either stimulate (prostaglandin D2) or inhibit (prostaglandins F2α and E2) the antiinflammatory ability of PPARγ to antagonize NF-κB in multiple immune cells, including T cells, B cells, macrophages, and dendritic cells (refs. 24, 25, and Figure 1E). PPARγ has been detected in macrophage-rich regions of human atherosclerotic plaques, where it controls lipid homeostasis and inhibits activation induced by proinflammatory cytokines (26). Although the functions of PPARs are tissue specific, some functions affecting lipoprotein metabolism include induction of lipolysis, reduced cellular triglyceride synthesis and VLDL production, enhanced intracellular LDL catabolism, and increased HDL production (27).
More recently, lipid metabolites termed specialized pro-resolving mediators (SPMs) have been shown to mediate resolution of inflammation and the restoration of tissue homeostasis. SPMs (including lipoxins, resolvins, and protectins) are produced by immune cells from the enzymatic conversion of omega-3 fatty acids and could be dysregulated in the context of AIRDs (refs. 20, 28, and Figure 1D). SPM levels correlate with decreased joint pain in RA patients (29) and are reduced in experimental models of RA with non-resolving joint inflammation (30). SPMs and other metabolites could also serve as biomarkers for predicting drug efficacy. A machine learning study in RA identified that peripheral blood SPM levels correlated positively with antirheumatic drug responsiveness at 6 months; notably decreased SPM concentrations were seen in nonresponders (31).
Sphingosine 1-phosphate
Sphingosine 1-phosphate (S1P), derived from membrane phospholipids, exerts its effect by binding GPCRs (S1P receptors) (Figure 1F). S1P binding initiates multiple cellular and physiological events, including immune cell localization to inflammatory sites, trafficking of lymphocytes to and from secondary lymphoid organs, and the regulation of T cell differentiation (between proinflammatory Th17 cells and Tregs) (32). Interestingly, HDL is an important S1P chaperone, and cellular uptake of HDL-S1P by SR-BI facilitates binding to S1P receptors with subsequent signaling in a cell-specific manner (33). Targeting of S1P receptors is an effective therapy to inhibit lymphocyte trafficking in patients with multiple sclerosis, and clinical trials are exploring similar therapies in AIRDs (34).
Ferroptosis
Ferroptosis is a form of regulated cell death driven by iron-dependent lipid oxidation (Figure 1F). Peroxidation of phospholipids containing polyunsaturated fatty acids is mediated by iron overload (free iron and iron-dependent lipoxygenases) and ROS. Under normal homeostatic conditions, cells can eliminate products of lipid peroxidation via several complex mechanisms (including glutathione peroxidase 4, an inhibitor of phospholipid peroxidation); however, in numerous conditions, including inflammation, these mechanisms are defective, leading to cell membrane damage and ferroptosis (35). Notably, increased ROS levels induced during inflammation in AIRDs could contribute to increased ferroptosis (36). Higher concentrations of free iron and other iron-binding proteins in synovial fluid and infusion of iron-dextran increase lipid peroxidation, decrease red cell glutathione, and exacerbate RA synovitis (36). In SLE, increased dietary iron and iron infusion also exacerbate disease activity (37). However, it remains to be confirmed whether inhibiting ferroptosis could be beneficial in AIRDs (36, 37).
Conventional antiinflammatory therapies
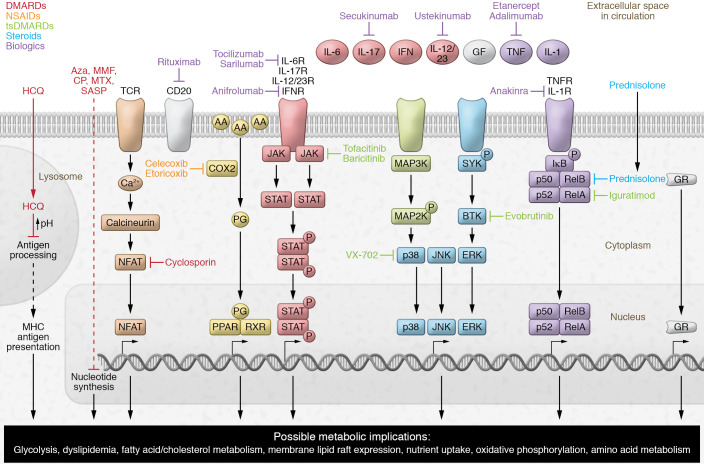
Many of the antiinflammatory therapies used to treat AIRDs influence multiple metabolic pathways, as summarized in Figure 2 and Tables 1–4; the effects of these drugs on lipid metabolism are described below.
Figure 2. Summary of the mechanisms of action of current therapies used in AIRDs.
Schematic representation summarizing the key mechanistic pathways affected by both traditional and modern therapies used to treat AIRDs, including disease-modifying antirheumatic drugs (DMARDs), target synthetic DMARDs (tsDMARDs), nonsteroidal antiinflammatory drugs (NSAIDs), steroids, and biologics. The majority of these therapeutics result in the modification of immune functions and metabolic pathways through alterations in gene transcription. These pathways provide insight into opportunities for cotherapies to prevent off-target immunometabolic effects. AA, arachidonic acid; Aza, azathioprine; CP, cyclophosphamide; GF, growth factor; GR, glucocorticoid receptor; HCQ, hydroxychloroquine; NF-κB, nuclear factor NF-κB (p50/p52/RelA/RelB/); IκB, inhibitor of κB; MAP2/3K, mitogen-activated protein 2-kinase or 3-kinase; MMF, mycophenolate mofetil; MTX, methotrexate; NFAT, nuclear factor of activated T cells; PG, prostaglandin; R, receptor; RXR, retinoid X receptor; SASP, sulfasalazine; SYK, spleen-associated tyrosine kinase; TCR, T cell receptor.
Table 1. Mechanisms of action of current conventional therapies used in AIRDs (part 1).
Nonsteroidal antiinflammatory drugs
Eicosanoids are drivers of inflammation in AIRDs and are major targets of antiinflammatory therapies, including nonsteroidal antiinflammatory drugs (NSAIDs), which inhibit prostaglandin synthesis through the inhibition of COX enzymes (ref. 20 and Table 1). NSAIDs include both nonselective NSAIDs (e.g., aspirin, ibuprofen, diclofenac, phenylbutazone, mefenamic acid) and selective COX-2 inhibitors (e.g., celecoxib and rofecoxib) (38). The antiinflammatory potency of COX-2 inhibitors is higher than that of nonselective NSAIDs, which is reflected in better clinical outcomes in RA and other types of inflammatory arthritis (39, 40). While all COX inhibitors are effective at treating inflammation, their side effects include cardiovascular, gastrointestinal, and renal complications (41). Of relevance to AIRDs is the association of selective COX-2 inhibition with increased risk of thrombotic events. Thromboxane A2 is an eicosanoid lipid mediator derived mainly from activated platelets, which constitutively express only COX-1. Thromboxane A2 induces vasoconstriction, endothelial adhesion molecule expression, and platelet aggregation and production among other effects, and is elevated in cardiovascular and inflammatory diseases; whereas COX-2 mediates the production of prostacyclin, which mediates vasodilation, inhibits platelet aggregation, and restrains the cardiovascular effects of thromboxane A2. Thus, both thromboxane A2 and prostacyclin are important mediators of CVD risk (42). CVD risk may also be associated with localized alterations in prostaglandin metabolism and PPARγ activity where the COX isoforms are coexpressed in atherosclerotic plaques (43, 44). Consequently, while COX-1 inhibition protects against atherosclerotic progression (for example, low-dose aspirin inhibits platelet-derived thromboxane A2), selective COX-2 inhibitors block cardioprotective prostacyclin and are associated with increased CVD risk (45). In clinical practice, individual CVD risk can be predicted using validated clinical scores; however, the complexity and heterogeneity of therapeutic responses and their direct or indirect impact on lipid metabolism could influence long-term outcomes (45).
Disease-modifying antirheumatic drugs
Disease-modifying antirheumatic drugs (DMARDs) inhibit inflammatory immune cell responses through various mechanisms (Figure 2 and Tables 1 and 2) and have been used reliably to treat AIRDs for many years. However, DMARD use can be associated with dyslipidemia, driven either by the impact of drugs on the liver or by the toxic side effects of drug metabolites (46, 47). More recent insights into the lipid metabolic pathways influenced by many DMARDs have provided new understanding of their antiinflammatory and immunomodulatory properties.
Prednisolone.
Prednisolone (glucocorticoid steroid hormone) effectively reduces inflammation, but long-term use has many side effects, including hypertension, obesity, dyslipidemia, and atherosclerosis (refs. 48–50 and Table 1). The mechanisms underpinning these effects could be associated with the promotion of fatty acid synthase and acetyl-CoA carboxylase activity, as well as inhibition of fatty acid β-oxidation by blocking of acyl-CoA dehydrogenase activity (ref. 51 and Figure 1D). Together, these processes result in hepatic fat accumulation and increased circulating triglycerides and VLDL. There is evidence that low-dose prednisolone attenuates postprandial suppression of lipid oxidation in patients with RA (52). Prolonged prednisolone use exacerbates dyslipidemia despite the preferential antiinflammatory effects of treatment (53, 54), although some studies show that RA patients treated with prednisolone can have increased levels of HDL (55). Hepatic lipid accumulation induced by prednisolone can impair insulin signaling through increased activation of MAPK signaling (51). As with many therapies, it has been important to measure these adverse metabolic effects against clinical benefits (48). Baseline lipid profile is considered when patients are started on corticosteroids, but the clinical need for treatment likely takes priority. If prednisolone treatment is of short duration (e.g., acute flare of gout, bridging therapy in RA) (56), then dyslipidemia is not clinically managed in any particular way. However, long-term prednisolone treatment requires monitoring of lipid profile as indicated in various guidelines and as part of CVD risk management recommendations (53, 57).
Hydroxychloroquine.
Despite the widespread use and efficacy of hydroxychloroquine in the treatment of AIRDs (58), its mechanism of action is relatively unclear. It has beneficial effects on lipid and glucose metabolism but also exerts multiple other immunomodulatory actions (ref. 59 and Table 1). The atheroprotective role of hydroxychloroquine is likely due to both its antiinflammatory and its lipid-modifying effects. Hydroxychloroquine is protective against endothelial cell damage, hypertension, and thrombosis (CVD risk factors) via the inhibition of endothelin-1 (a potent vasoconstrictor), downregulation of proinflammatory cytokines such as TNF-α, and reduced levels of proinflammatory ROS, which inhibit platelet aggregation (60–62). The mechanisms underlying its direct effect on lipid metabolism remain largely unknown. There is evidence that hydroxychloroquine reduces atherogenic triglycerides and total and LDL-cholesterol and increases atheroprotective HDL-cholesterol (63, 64). Hydroxychloroquine is also a substrate for CYP enzymes, which are associated with the metabolism of many drugs; thus, it could interfere with the efficacy of combination therapies that are metabolized via the CYP pathway, including calcineurin inhibitors (59, 65), or increase the cardiovascular risk in association with various antibiotics (66). Hydroxychloroquine-mediated changes in lipid metabolism could influence immune cell function. Interestingly, research investigating hydroxychloroquine in SARS-CoV-2 infection shows that the drug binds to sialic acid–containing glycolipids within plasma membrane lipid rafts and inhibits viral uptake (67). It has also been shown to disrupt lysosomal membranes; therefore, hydroxychloroquine could also mediate its effects in AIRDs by modifying lipid raft–mediated immune cell signaling, which can in turn modulate immune cell function (refs. 9, 68, and Figure 1A).
Calcineurin inhibitors.
Calcineurin inhibitors (cyclosporin, voclosporin, tacrolimus) block T cell signaling and activation (Table 1) but also have noteworthy off-target effects, including impairment of endothelial cell function associated with COX-2 inhibition and reduced production of prostaglandin E2 (69) and dyslipidemia (increased total cholesterol, LDL-C, triglycerides, and apolipoprotein B) (70, 71). Various mechanisms could contribute to altered lipid levels, including reduced hepatic LDL-C clearance and increased cholesterol biosynthesis via the HMG-CoA pathway mediated by inhibition of 27-hydroxycholesterol, an oxysterol that inhibits cholesterol metabolism via HMG-CoA (ref. 72 and Figure 1C). Interestingly, voclosporin, recently approved for use in adult lupus nephritis, shows a significant reduction in total cholesterol and LDL-C, potentially due to its superior antiinflammatory properties (73). Cyclosporin also inhibits bile acid synthesis via 26-hydroxylase and could reduce triglyceride degradation by inhibiting lipoprotein lipase activity (71, 74). Thus, although calcineurin inhibitors are favorable in AIRDs, further mechanistic research is required to assess the antiinflammatory benefits against the off-target effects of blocking fundamental metabolic processes.
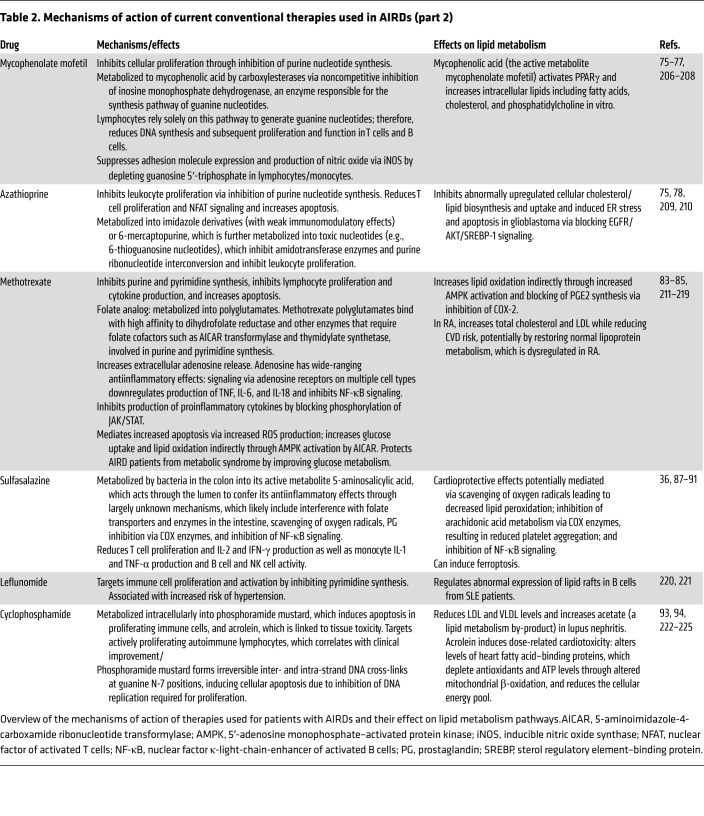
Mycophenolate mofetil and azathioprine.
Mycophenolate mofetil (MMF) and azathioprine inhibit cellular proliferation through inhibition of purine nucleotide synthesis pathways (ref. 75 and Table 2). Mycophenolic acid (the active metabolite of MMF) can also activate PPARγ (76) and increase intracellular lipids including fatty acids, cholesterol, and phosphatidylcholine in vitro (77). Such metabolic dysregulation could contribute to MMF function via disruption of cell signaling and membrane integrity. Another study shows that azathioprine reduced abnormally upregulated cellular cholesterol/lipid biosynthesis and uptake and induced ER stress and apoptosis in glioblastoma; this effect was likely mediated by blocking of EGFR/AKT/SREBP-1 signaling and not via the typical ABCA1-mediated cholesterol efflux through the LXR transcription factor, as neither LXR nor ABCA1 levels were altered by azathioprine (78). Interestingly, small-molecule inhibitors of sterol regulatory element–binding protein (SREBP) such as betulin, in addition to their antitumoral effects (79), can reduce cholesterol and fatty acid biosynthesis and atherogenic hyperlipidemia in animal models, suggesting that azathioprine could have a similar effect (80). SREBP-1 also reduces proinflammatory signaling and modulates macrophage phagocytosis (81, 82), additional pathways that could be affected by the inhibition of this transcription factor.
Table 2. Mechanisms of action of current conventional therapies used in AIRDs (part 2).
Methotrexate, sulfasalazine, and leflunomide.
Methotrexate suppresses lymphocyte proliferation and cytokine production and increases apoptosis via multiple metabolic pathways (Table 2). Patients with RA have atypically reduced lipid levels considering their increased CVD risk (14); in line with this, recent studies show that methotrexate increases total cholesterol and LDL while reducing CVD risk (83), potentially by restoring normal lipoprotein metabolism (84, 85), although reduced proinflammatory cytokine levels and associated inflammation are also likely to play a role (86). The antiinflammatory mechanisms of sulfasalazine are also thought to have cardioprotective effects (87), potentially mediated by scavenging of oxygen radicals leading to decreased lipid peroxidation, inhibition of arachidonic acid metabolism via COX enzymes that results in reduced platelet aggregation, and inhibition of NF-κB signaling (88–91). Alternatively, sulfasalazine can induce ferroptosis, although it is not established whether this influences drug efficacy (ref. 36 and Figure 1F). Leflunomide, another antiproliferative drug, is known to increase hypertension and thus increase CVD risk, although the mechanism is unknown (ref. 92 and Table 2).
Cyclophosphamide.
Cyclophosphamide can reduce LDL and VLDL levels and increase acetate (a lipid metabolism by-product) in lupus nephritis patients (93). However, acrolein, a cyclophosphamide metabolite (Table 1), can result in dose-related cardiotoxicity, which is a limiting factor for cyclophosphamide use (94). Acrolein alters levels of heart fatty acid–binding proteins, which deplete antioxidants and ATP levels through altered mitochondrial β-oxidation, thereby reducing the cellular energy pool. Together, these metabolic changes increase apoptosis in cardiomyocytes and can lead to heart failure and myocardial infarction (94). These off-target metabolic effects require close cyclophosphamide dose monitoring and modification in patients with AIRDs. There are few other reports that cyclophosphamide influences metabolite levels in AIRDs (95).
Target synthetic DMARDs
Target synthetic DMARDs (tsDMARDs) are small-molecule inhibitors used increasingly to treat AIRDs since they are less toxic, have fewer adverse effects, and have increased specificity to proteins and signaling pathways associated with disease pathogenesis (96). An array of tsDMARDs exist targeting key proinflammatory signaling pathways that are stimulated by inflammatory mediators (cytokines, chemokines, growth factors, and antigens), including JAK, MAPK, NF-κB, and spleen-associated tyrosine kinase (SYK)/Bruton’s tyrosine kinase (BTK) pathways (refs. 96–98 and Table 3). The full impact of inhibition of these pathways on specific metabolic mechanisms is unclear but likely plays an important role in the performance of specific tsDMARDs. Furthermore, crosstalk between various signaling pathways adds complexity to therapeutic strategies; for example, NF-κB target genes can inhibit MAPK signaling (99).
Table 3. Mechanisms of action of tsDMARDs used in AIRDs.
JAK inhibitors
JAK inhibitors block cell signaling via the JAK/STAT pathway (Table 3) but also have cell metabolic effects (including decreased mitochondrial membrane potential, mitochondrial mass, and ROS and inhibition of metabolic genes in synovial tissue) (100) and modify systemic lipid metabolism. Tofacitinib and baricitinib significantly increased HDL-C and LDL-C compared with baseline and other DMARD treatments alone in randomized controlled trials in RA and SLE (101–106), an effect reversed by statins (107). JAK inhibitors also improve HDL function by increasing the activity of lecithin-cholesterol acyltransferase (LCAT; an enzyme that converts free cholesterol to cholesterol esters and supports cholesterol efflux to lipoproteins), thereby increasing HDL efflux capacity (refs. 103, 106, and Figure 1C). Other effects such as alterations in lipoprotein size and content have been described (103, 108); therefore, these therapies may contribute to drug-induced dyslipidemia and exacerbate the lipid imbalances already associated with AIRDs. Past trials have highlighted concerns surrounding the risk of arterial and venous thrombotic events with JAK inhibition, and emerging evidence suggests that this risk is dependent on JAK selectivity and is potentially confounded by indication (109, 110). Based on a review of a randomized controlled trial of tofacitinib versus anti-TNF treatment, the Food and Drug Administration issued an urgent revision for all JAK inhibitors to include information about potential increased risks of serious heart-related events, cancer, blood clots, and death. These emerging concerns are mirrored in recommendations to assess the benefits and risks for patients before initiating or continuing JAK inhibitor therapy (111).
Targeting the MAPK pathway
The MAPK pathway, comprising ERK, JNK, and p38 kinase (p38) (112), regulates cellular function via activation of transcription factors (Table 3). Although targeting of MAPKs such as p38 by VX-702 has shown clinical benefit in RA and animal models of SLE, the use of MAPK inhibitors is confounded by the vast and pleiotropic effects of MAPKs on immune cell functions and cellular metabolism; this has resulted in multiple failures of MAPK inhibitors in clinical trials (96, 113). Mouse models of kinase deficiency clearly show that interconnected metabolic relationships exist between kinase function and liver-mediated lipid metabolism; altered activity and expression of MAPKs and their inactivating phosphatases are present in models of metabolic disease (114). Notably, downstream insulin signaling stimulates MAPK signaling, ERK can phosphorylate SREBP-2 (a regulator of cholesterol biosynthesis) (115), and ERK/JNK phosphorylates PPARγ (116), linking the MAPK pathway to key regulators of lipid metabolism. The MAPK pathway can also be activated by JAK/STAT signaling (117).
Targeting NF-κB signaling
Aberrant NF-κB signaling is implicated in many inflammatory (RA, SLE) and metabolic (atherosclerosis, obesity, diabetes) diseases (118, 119). Iguratimod, an inhibitor of RelA, a component of the NF-κB heterodimer, is approved for use in patients with RA in China and Japan (refs. 120, 121, and Table 3). Iguratimod could also affect the cellular metabolic responses associated with NF-κB signaling, including macrophage foam cell formation (lipid accumulation), via reduced expression of lipid transporters (ABCA1 and ABCG1), reduced cholesterol efflux, and increased lipid uptake via scavenger receptors (refs. 122, 123, and Figure 1C). Blocking NF-κB signaling could therefore increase cellular cholesterol efflux and reduce lipid uptake, with both atheroprotective implications through reduced foam cell formation (124) and antiinflammatory benefits via modulation of cell plasma membrane lipid rafts and reduction of Toll-like receptor trafficking and signaling (125). Alternatively, inhibition of NF-κB activation in macrophages can increase atherosclerosis in LDLR-deficient mice (126); disparity between studies may be due to different models and experimental approaches, indicating that such off-target effects need to be studied in more detail in patients. Additionally, the atheroprotective transcription factor PPARα, activated by endogenous fatty acid ligands such as arachidonic acid, can suppress entry of NF-κB to the nucleus owing to increased IκBα expression (127), demonstrating the complexity of NF-κB signaling in lipid metabolism.
Targeting SYK/BTK pathways
Finally, SYK/BTK–mediated signaling is proximal to multiple downstream signaling pathways, including the MAPK and NF-κB pathways (ref. 128 and Table 3); BTK inhibition can inhibit free fatty acid metabolism in chronic lymphocytic leukemia through reduction of lipoprotein lipase (129). Furthermore, crosstalk between BTK signaling and bioenergetic stress responses in leukemic B cells suggests that cellular metabolic rewiring could mediate the metabolic effects of these molecules (130). Multiple BTK inhibitors are currently in clinical trials for AIRDs.
Biologics
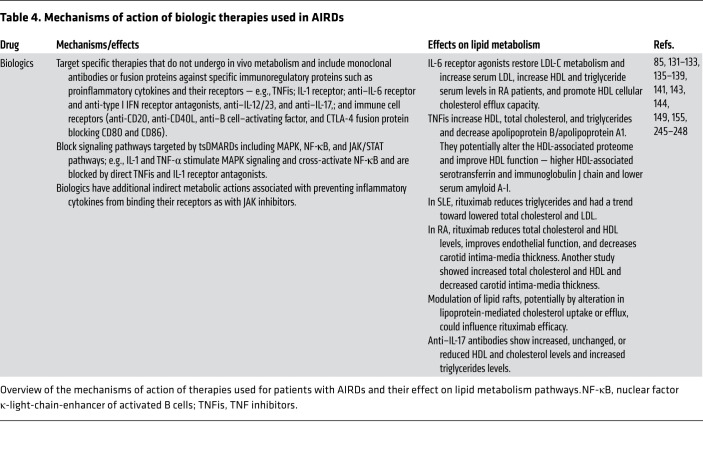
Biologic therapies are target specific and, despite their eventual catabolism by proteases and complications surrounding anti-drug antibodies, they do not undergo in vivo metabolism within immune cells to elicit their desired effects (ref. 131 and Table 4). Notably, several biologics influence lipid and lipoprotein metabolism, and it is likely that biologics have additional indirect metabolic actions associated with preventing inflammatory cytokines from binding their receptors, as seen with JAK inhibitors (132, 133).
Table 4. Mechanisms of action of biologic therapies used in AIRDs.
IL-6 receptor antagonists
Tocilizumab and sarilumab inhibit IL-6 receptor binding to IL-6 and block downstream signaling via multiple pathways, including JAK/STAT, p38/JNK, and MAPK (134). Patients with RA are typically characterized by low levels of LDL, potentially due to LDL-C hypercatabolism driven by the IL-6/acute-phase response (85). By blocking hepatic IL-6 signaling, tocilizumab restores LDL-C metabolism and increases serum LDL-C (85, 135, 136). Tocilizumab also increases HDL and triglyceride serum levels in RA patients (137) and promotes HDL cellular cholesterol efflux capacity (ref. 138 and Figure 1C).
TNF inhibitors
Treatment with TNF inhibitors (e.g., etanercept or adalimumab) also increases HDL, total cholesterol, and triglycerides, while the apolipoprotein B/apolipoprotein A1 ratio is decreased and LDL-C levels remain unchanged (139). These effects could reduce CVD risk in RA patients (140), potentially by altering the HDL-associated proteome and improving HDL function, when inflammation is reduced by either adalimumab or abatacept (CTLA-4 fusion protein blocking CD80/CD86 costimulation) (141). Interestingly, adalimumab was associated with higher HDL-associated serotransferrin and immunoglobulin J chain and lower serum amyloid A-I in comparison with patients treated with abatacept (141). It has also been shown that RA patients receiving tocilizumab have a greater increase in LDL-C levels compared with those treated with adalimumab (142), highlighting the differential effects of various biologics on lipid metabolism.
Rituximab
Several studies have reported altered lipid profiles following rituximab (anti-CD20 monoclonal antibody) treatment in AIRDs. In SLE, rituximab reduced triglycerides and resultant atherogenic index of plasma values, likely associated with improvement in disease activity, although reductions in total cholesterol and LDL-C did not reach statistical significance and HDL levels remained stable (143). In contrast, a separate study showed that RA patients treated with rituximab had reduced total cholesterol and HDL levels associated with improved endothelial function and decreased carotid intima-media thickness (144), supporting beneficial metabolic effects. However, another study investigating RA patients responding to rituximab therapy only partially replicated this, showing an increase in total cholesterol and HDL with a paradoxical decreased atherogenic index of plasma and carotid intima-media thickness (145). The disparities between these studies could be dependent on the level of baseline dyslipidemia.
It is plausible that biologic therapies influence systemic lipid metabolism partly via the general dampening of inflammation, particularly considering that the liver is largely responsible for circulating lipoprotein metabolism, as seen in transplant recipients (146). This could also be due to altered hepatic cytokine signaling, as, for example, TNF-α can reduce lipoprotein lipase activity and liver metabolism (147), while in hepatic steatosis IL-1 signaling increased fatty acid synthase expression and triglyceride accumulation (148). Alternatively, in RA, blocking hepatic IL-6 signaling (tocilizumab) restored normal LDL catabolism induced by IL-6 suppression of CYP enzymes. Normalizing CYP enzyme expression could also have a wider effect on cell metabolism generally (85). The effect of anti–IL-17 antibodies (secukinumab) on lipid metabolism remains uncertain, with reports showing increased, unchanged, or reduced HDL and cholesterol levels as well as increased triglyceride levels (149). This uncertainty exists even though IL-17, a proinflammatory cytokine implicated in AIRD and atherosclerosis pathogenesis, is known to affect cholesterol and lipoprotein metabolism (150, 151) and promote foamy macrophage formation (152).
Immune cell lipid metabolism could also be influenced by biologics. Recently, IFNs were shown to have differential effects on membrane cholesterol metabolism in macrophages, including downregulation of cholesterol biosynthesis (153, 154); this effect was not observed with TNF-α, IL-1β, or IL-6, suggesting that new therapies such as anifrolumab (anti–type I IFN receptor antibody) could have effects on both systemic (hepatic) and local (immune cell) lipid metabolism. Changes in immune cell lipid metabolism can also influence cell signaling via changes in lipid rafts (9, 68). By binding membrane CD20, rituximab induces its translocation to lipid rafts, which is crucial, under some conditions, for induction of B cell apoptosis and can be prevented by disruption of lipid rafts by cholesterol depletion (155). However, binding of anti-CD20 antibodies can also trigger antiapoptotic signaling via SYK and AKT pathways, an effect that was also inhibited by cholesterol depletion (156, 157). Thus, modulation of lipid rafts, potentially by alteration of lipoprotein-mediated cholesterol uptake or efflux, could influence drug efficacy. Experimental evidence in cancer immunotherapy shows that inhibition of acetyl-CoA acetyltransferase-1 (ACAT1), an enzyme that increases intracellular esterified cholesterol levels, improves the efficacy of anti–PD-1 therapy in melanoma (158). Reduced cholesterol esterification in CD8+ T cells increased plasma membrane cholesterol levels and subsequent lipid raft–associated T cell receptor clustering and signaling, thereby increasing T cell cytotoxicity against melanoma growth. ACAT inhibition can also boost the antiviral activity of CD8+ T cells against hepatitis B by promoting lipid raft signaling in vitro (159).
Advances supporting metabolism- and inflammation-targeted therapies in AIRDs
Chronic inflammation and dyslipidemia (which can be exacerbated by current therapies) both contribute to increased CVD risk in patients with AIRDs. However, studies show that lipid-lowering drugs (such as statins) are not sufficient to reduce CVD risk in some AIRDs, possibly because they cannot completely restore the antiinflammatory properties of HDL (160, 161). Thus, an unmet clinical need exists for better therapies to address both inflammation and atherosclerosis.
Altered lipid metabolism is frequently associated with the use of nonselective and targeted AIRD treatments. The impact of therapy on lipid profiles can be beneficial, as in the case of hydroxychloroquine, which reduces LDL-C in SLE (63), or lead to new drug-induced dyslipidemia or exacerbate current dyslipidemia associated with AIRD (Tables 1–4) with various clinical outcomes. In the context of high mortality rates associated with CVD in AIRDs, lipid modification therapies are a key cotherapy of interest. Statins are inhibitors of HMG-CoA reductase, the rate-limiting enzyme in cholesterol biosynthesis, that reduce levels of circulating cholesterol, particularly cholesterol carried in LDL particles. Atorvastatin can reverse tofacitinib-induced elevation of total cholesterol, LDL-C, and triglycerides in patients with RA (107), and patients treated with statins for over 6 months have improved disease activity scores in comparison with conventional RA therapies, supporting a potential beneficial role for statins in patients with active RA (162). Other trials have assessed the use of statins to reduce inflammation. High-dose statins reduced brain atrophy and disability progression in patients with secondary progressive multiple sclerosis in a randomized controlled trial (163, 164). Statins have also been tested in SLE to treat inflammation and dyslipidemia, with mixed outcomes. Some studies show beneficial effects such as improved lipid and inflammatory cytokine levels and reductions in vascular inflammation, atherosclerotic plaque progression, mortality, and morbidity (165–168). However, statins have not met their primary endpoint in clinical trials, including the Atherosclerosis Prevention in Pediatric Lupus Erythematosus (APPLE) trial in children (169) and the Lupus Atherosclerosis Prevention Study (LAPS) in adults (170). Interestingly, although the LAPS 2-year intervention trial did not meet the atherosclerosis primary and secondary endpoints, significant changes in lipid profiles [lipoprotein(a) and total cholesterol] were reported. Difficulties in stratifying patients based on their initial dyslipidemia status as well as their background medication could be the reason for this.
Recent studies of lipoprotein taxonomy in patients with adult and juvenile-onset SLE (171, 172) and multiple sclerosis (173) have highlighted the heterogeneity in patient lipoprotein profiles. Therefore, baseline lipid levels could be important predictors of therapeutic benefit, as has been shown in RA patients treated with tocilizumab and JAK inhibitors, among whom patients with increased lipid levels had a better response to lipid-lowering drugs (107, 135). Other therapies targeting lipid metabolism include reconstituted HDL (shown to reduce plaque in lipid content, macrophage size, and inflammation; ref. 174) and the recently approved statin alternative inclisiran, which increases LDLR levels in the liver (by inhibiting proprotein convertase subtilisin/kexin type 9, the enzyme responsible for LDLR inhibition), thereby reducing LDL-C in the blood by up to 50%, similarly to high-dose statins (175). In the future, new lipid-modifying drugs could be used as an alternative to, or in combination with, statins for patients with AIRDs and dyslipidemia not controlled by conventional treatment and at high risk of cardiovascular events, particularly in those on antiinflammatory treatments that exacerbate dyslipidemia as discussed above.
Some immune receptors that reside in lipid rafts are targeted by AIRD treatments — including CD20 targeted by rituximab (155), CD80/CD86 targeted by abatacept (141), and IL-6R targeted by tocilizumab (176) — suggesting that lipid modification could potentially alter the efficiency of these therapies by regulating membrane turnover of these receptor targets. Some biologic agents require intact lipid rafts to exert their therapeutic function, e.g., rituximab (155–157). Furthermore, pharmacologic inhibition of lipid raft components (cholesterol and glycosphingolipids) using statins and glycolipid synthase inhibitors (N-butyldeoxynojirimycin) restored defective lipid raft levels and normalized in vitro function in CD4+ T cells from patients with SLE. This included T cell receptor signaling and function and anti-dsDNA antibody production by autologous B cells (10, 177). Interestingly, elevated glycosphingolipid levels in SLE T cells were associated with the increased expression of the LXR master lipid transcriptional regulator, which directly modulates enzymes involved in glycosphingolipid synthesis (9). Whether supplementation with compounds targeting LXR could further modulate lipid rafts and AIRD drug efficacies remains to be explored.
In some circumstances, the dose of lipid-modifying therapies must be adjusted when they are used in combination with AIRD therapies. Tocilizumab normalizes CYP enzyme expression and increases LDL-C; therefore patients on statin cotherapy may require an increased dose to maintain therapeutic lipid-lowering benefits (135). Cyclosporin can also affect the pharmacokinetics of statins through the inhibition of both organic anion transporter polypeptide-1B1 and CYP3A4 (178). Also, lipids including HDL play an important role as S1P chaperones; therefore, alterations in lipoprotein metabolism could influence the efficacy of drugs modulating the S1P pathway (e.g., fingolimod), which are now used in multiple sclerosis and being investigated in AIRDs (34, 179).
Dietary patterns also modify inflammation; those with a higher inflammatory potential are significantly associated with unfavorable lipid profiles and a higher incidence of CVD (180). Despite these observations, the relationship between nutrition and inflammation in AIRDs is not well established. Oral lipid supplements may aid the effectiveness of conventional therapies, such as essential fatty acid supplementation to increase STM levels; these have been linked to decreased joint pain and predict DMARD responsiveness in RA (31). Dietary polyunsaturated fatty acids can also inhibit ferroptosis (181) and incorporate into T cell membranes, thus altering plasma membrane phospholipid expression and the localization of immunogenic receptors such as IL-2 receptor and Fc receptors into lipid raft microdomains (182). Dietary intervention to alter blood lipids can be beneficial in SLE and RA and reduce disease activity scores (183–185). Increased dietary intake of omega-3 fatty acids increased HDL and reduced triglycerides in juvenile-onset SLE (183, 186) and increased HDL and reduced VLDL in adult SLE (187). Thus omega-3 dietary supplements could be promising therapeutic options for some patients. In contrast, a randomized controlled trial of dietary restrictive patterns reduced weight and fatigue in adults with SLE, but did not affect disease activity or cardiovascular parameters including lipid profiles and inflammatory markers (188).
Conclusion
Understanding how lipid metabolism influences immune responses and the effect of both conventional and new therapies on lipid metabolism is an ongoing challenge but could identify new ways to target AIRDs. Better control of inflammation using optimal combinations of immunosuppressive treatments, as shown in inflammatory bowel disease (189), could lead to an improved metabolic/lipid profile in AIRDs. Improved monitoring of pro-/antiinflammatory lipoprotein fractions using a granular lipoprotein taxonomy approach and improved CVD risk stratification biomarkers (171, 172), rather than total HDL/LDL levels, could improve targeted patient management. This is relevant since statins do not completely normalize proinflammatory HDL fractions (160). Such improved monitoring could enable novel combination interventions, such as nonspecific dietary intervention with specific lipid lowering and targeted antiinflammatory therapy. Finally, the clinical relevance of metabolic/lipid biomarkers in AIRDs needs to be explored in long-term studies to capture the long-term toxicity of combined therapies as well as their impact on cardiovascular events.
Acknowledgments
GAR is supported by Lupus UK, the Rosetrees Trust (M409), and a National Institute for Health Research (NIHR) University College London Hospitals (UCLH) Biomedical Research Centre grant (BRC773/III/CC/101350). IPT is funded by a Medical Research Council New Investigator Grant (G0801278), a British Heart Foundation Project Grant (PG/13/10/30000), and an Academy of Medical Sciences Newton Advanced Fellowship. CC is supported by a grant from the Centre for Adolescent Rheumatology Versus Arthritis at University College London UCLH and Great Ormond Street Hospital (GOSH) supported by grants from Versus Arthritis (21593 and 20164), Great Ormond Street Hospital Children’s Charity (GOSCC), and the NIHR Biomedical Research Centres at both GOSH and UCLH. ECJ is supported by grants from the Dunhill Medical Trust (RPGF1902\117) and NIHR UCLH Biomedical Research Centre grant BRC772/III/EJ/101350 and Fast Track grant F215. The views expressed are those of the authors and not necessarily those of the National Health Service, the NIHR, or the Department of Health.
Version 1. 01/18/2022
Electronic publication
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Copyright: © 2022, Robinson et al. This is an open access article published under the terms of the Creative Commons Attribution 4.0 International License.
Reference information: J Clin Invest. 2022;132(2):e148552.https://doi.org/10.1172/JCI148552.
Contributor Information
Ines Pineda-Torra, Email: i.torra@ucl.ac.uk.
Coziana Ciurtin, Email: c.ciurtin@ucl.ac.uk.
Elizabeth C. Jury, Email: e.jury@ucl.ac.uk.
References
- 1.Rhoads JP, et al. Fine tuning of immunometabolism for the treatment of rheumatic diseases. Nat Rev Rheumatol. 2017;13(5):313–320. doi: 10.1038/nrrheum.2017.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gerriets VA, Rathmell JC. Metabolic pathways in T cell fate and function. Trends Immunol. 2012;33(4):168–173. doi: 10.1016/j.it.2012.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Waters LR, et al. Initial B cell activation induces metabolic reprogramming and mitochondrial remodeling. iScience. 2018;5:99–109. doi: 10.1016/j.isci.2018.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galván-Peña S, O’Neill LAJ. Metabolic reprograming in macrophage polarization. Front Immunol. 2014;5:420. doi: 10.3389/fimmu.2014.00420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perl A. Activation of mTOR (mechanistic target of rapamycin) in rheumatic diseases. Nat Rev Rheumatol. 2016;12(3):169–182. doi: 10.1038/nrrheum.2015.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Han X. Lipidomics for studying metabolism. Nat Rev Endocrinol. 2016;12(11):668–679. doi: 10.1038/nrendo.2016.98. [DOI] [PubMed] [Google Scholar]
- 7.Jury EC, et al. Lipid rafts in T cell signalling and disease. Semin Cell Dev Biol. 2007;18(5):608–615. doi: 10.1016/j.semcdb.2007.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pierce SK. Lipid rafts and B-cell activation. Nat Rev Immunol. 2002;2(2):96–105. doi: 10.1038/nri726. [DOI] [PubMed] [Google Scholar]
- 9.Waddington KE, et al. LXR directly regulates glycosphingolipid synthesis and affects human CD4+ T cell function. Proc Natl Acad Sci U S A. 2021;118(21):e2017394118. doi: 10.1073/pnas.2017394118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McDonald G, et al. Normalizing glycosphingolipids restores function in CD4+ T cells from lupus patients. J Clin Invest. 2014;124(2):712–724. doi: 10.1172/JCI69571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flores-Borja F, et al. Altered lipid raft-associated proximal signaling and translocation of CD45 tyrosine phosphatase in B lymphocytes from patients with systemic lupus erythematosus. Arthritis Rheum. 2007;56(1):291–302. doi: 10.1002/art.22309. [DOI] [PubMed] [Google Scholar]
- 12.Luo J, et al. Mechanisms and regulation of cholesterol homeostasis. Nat Rev Mol Cell Biol. 2020;21(4):225–245. doi: 10.1038/s41580-019-0190-7. [DOI] [PubMed] [Google Scholar]
- 13.Hahn BH, et al. The pathogenesis of atherosclerosis in autoimmune rheumatic diseases: roles of inflammation and dyslipidemia. J Autoimmun. 2007;28(2-3):69–75. doi: 10.1016/j.jaut.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 14.Myasoedova E, et al. Lipid paradox in rheumatoid arthritis: the impact of serum lipid measures and systemic inflammation on the risk of cardiovascular disease. Ann Rheum Dis. 2011;70(3):482–487. doi: 10.1136/ard.2010.135871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McMahon M, et al. Dysfunctional proinflammatory high-density lipoproteins confer increased risk of atherosclerosis in women with systemic lupus erythematosus. Arthritis Rheum. 2009;60(8):2428–2437. doi: 10.1002/art.24677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ardoin S, et al. Management of dyslipidemia in children and adolescents with systemic lupus erythematosus. Lupus. 2007;16(8):618–626. doi: 10.1177/0961203307079566. [DOI] [PubMed] [Google Scholar]
- 17.Szabo MZ, et al. Dyslipidemia in systemic lupus erythematosus. Immunol Res. 2017;65(2):543–550. doi: 10.1007/s12026-016-8892-9. [DOI] [PubMed] [Google Scholar]
- 18.Wu T, et al. Metabolic disturbances associated with systemic lupus erythematosus. PLoS One. 2012;7(6):e37210. doi: 10.1371/journal.pone.0037210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Charles-Schoeman C, et al. Abnormal function of high-density lipoprotein is associated with poor disease control and an altered protein cargo in rheumatoid arthritis. Arthritis Rheum. 2009;60(10):2870–2879. doi: 10.1002/art.24802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dennis EA, Norris PC. Eicosanoid storm in infection and inflammation. Nat Rev Immunol. 2015;15(8):511–523. doi: 10.1038/nri3859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Norris PC, et al. Phospholipase A2 regulates eicosanoid class switching during inflammasome activation. Proc Natl Acad Sci U S A. 2014;11(35):12746–12751. doi: 10.1073/pnas.1404372111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang B, et al. Metabolism pathways of arachidonic acids: mechanisms and potential therapeutic targets. Signal Transduct Target Ther. 2021;6(1):94. doi: 10.1038/s41392-020-00443-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wahli W, Michalik L. PPARs at the crossroads of lipid signaling and inflammation. Trends Endocrinol Metab. 2012;23(7):351–363. doi: 10.1016/j.tem.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 24.Daynes RA, Jones DC. Emerging roles of PPARs in inflammation and immunity. Nat Rev Immunol. 2002;2(10):748–759. doi: 10.1038/nri912. [DOI] [PubMed] [Google Scholar]
- 25.Tontonoz P, Spiegelman BM. Fat and beyond: the diverse biology of PPARgamma. Annu Rev Biochem. 2008;77:289–312. doi: 10.1146/annurev.biochem.77.061307.091829. [DOI] [PubMed] [Google Scholar]
- 26.Ricote M, et al. The peroxisome proliferator-activated receptor-gamma is a negative regulator of macrophage activation. Nature. 1998;391(6662):79–82. doi: 10.1038/34178. [DOI] [PubMed] [Google Scholar]
- 27.Gervois P, et al. Regulation of lipid and lipoprotein metabolism by PPAR activators. Clin Chem Lab Med. 2000;38(1):3–11. doi: 10.1515/CCLM.2000.002. [DOI] [PubMed] [Google Scholar]
- 28.Buckley CD, et al. Proresolving lipid mediators and mechanisms in the resolution of acute inflammation. Immunity. 2014;40(3):315–327. doi: 10.1016/j.immuni.2014.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barden AE, et al. Specialised pro-resolving mediators of inflammation in inflammatory arthritis. Prostaglandins Leukot Essent Fatty Acids. 2016;107:24–29. doi: 10.1016/j.plefa.2016.03.004. [DOI] [PubMed] [Google Scholar]
- 30.Arnardottir HH, et al. Resolvin D3 is dysregulated in arthritis and reduces arthritic inflammation. J Immunol. 2016;197(6):2362–2368. doi: 10.4049/jimmunol.1502268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gomez EA, et al. Blood pro-resolving mediators are linked with synovial pathology and are predictive of DMARD responsiveness in rheumatoid arthritis. Nat Commun. 2020;11(1):13. doi: 10.1038/s41467-019-13704-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cartier A, Hla T. Sphingosine 1-phosphate: lipid signaling in pathology and therapy. Science. 2019;366(6463):eaar5551. doi: 10.1126/science.aar5551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Galvani S, et al. HDL-bound sphingosine 1-phosphate acts as a biased agonist for the endothelial cell receptor S1P1 to limit vascular inflammation. Sci Signal. 2015;8(389):ra79. doi: 10.1126/scisignal.aaa2581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pérez-Jeldres T, et al. Targeting sphingosine-1-phosphate signaling in immune-mediated diseases: beyond multiple sclerosis. Drugs. 2021;81(9):985–1002. doi: 10.1007/s40265-021-01528-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jiang X, et al. Ferroptosis: mechanisms, biology and role in disease. Nat Rev Mol Cell Biol. 2021;22(4):266–282. doi: 10.1038/s41580-020-00324-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen X, et al. Ferroptosis in infection, inflammation, and immunity. J Exp Med. 2021;218(6):e20210518. doi: 10.1084/jem.20210518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wlazlo E, et al. Iron metabolism: an under investigated driver of renal pathology in lupus nephritis. Front Med (Lausanne) 2021;8:643686. doi: 10.3389/fmed.2021.643686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vane JR, Botting RM. Mechanism of action of aspirin-like drugs. Semin Arthritis Rheum. 1997;26(6 suppl 1):2–10. doi: 10.1016/s0049-0172(97)80046-7. [DOI] [PubMed] [Google Scholar]
- 39.Seppala E, et al. Effects of non-steroidal anti-inflammatory drugs and prednisolone on synovial fluid white cells, prostaglandin E2, leukotriene B4 and cyclic AMP in patients with rheumatoid arthritis. Scand J Rheumatol. 1990;19(1):71–75. doi: 10.3109/03009749009092624. [DOI] [PubMed] [Google Scholar]
- 40.van der Heijde D, et al. Evaluation of the efficacy of etoricoxib in ankylosing spondylitis: results of a fifty-two-week, randomized, controlled study. Arthritis Rheum. 2005;52(4):1205–1215. doi: 10.1002/art.20985. [DOI] [PubMed] [Google Scholar]
- 41.Bhala N, et al. Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials. Lancet. 2013;382(9894):769–779. doi: 10.1016/S0140-6736(13)60900-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mitchell JA, Warner TD. COX isoforms in the cardiovascular system: understanding the activities of non-steroidal anti-inflammatory drugs. Nat Rev Drug Discov. 2006;5(1):75–86. doi: 10.1038/nrd1929. [DOI] [PubMed] [Google Scholar]
- 43.Schonbeck U, et al. Augmented expression of cyclooxygenase-2 in human atherosclerotic lesions. Am J Pathol. 1999;155(4):1281–1291. doi: 10.1016/S0002-9440(10)65230-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thiemermann C. Ligands of the peroxisome proliferator-activated receptor-gamma and heart failure. Br J Pharmacol. 2004;141(1):1–3. doi: 10.1038/sj.bjp.0705586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tilley SL, et al. Mixed messages: modulation of inflammation and immune responses by prostaglandins and thromboxanes. J Clin Invest. 2001;108(1):15–23. doi: 10.1172/JCI200113416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Akman B, et al. Lipid profile during azathioprine or mycophenolate mofetil combinations with cyclosporine and steroids. Transplant Proc. 2007;39(1):135–137. doi: 10.1016/j.transproceed.2006.10.210. [DOI] [PubMed] [Google Scholar]
- 47.Panoulas V, Kitas GD. Pharmacological management of cardiovascular risk in chronic inflammatory rheumatic diseases. Expert Rev Clin Pharmacol. 2020;13(6):605–613. doi: 10.1080/17512433.2020.1766964. [DOI] [PubMed] [Google Scholar]
- 48.van der Goes MC, et al. The value of glucocorticoid co-therapy in different rheumatic diseases — positive and adverse effects. Arthritis Res Ther. 2014;16(suppl 2):S2. doi: 10.1186/ar4686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Petta I, et al. Risks and benefits of corticosteroids in arthritic diseases in the clinic. Biochem Pharmacol. 2019;165:112–125. doi: 10.1016/j.bcp.2019.04.009. [DOI] [PubMed] [Google Scholar]
- 50.Petri M, et al. Risk factors for coronary artery disease in patients with systemic lupus erythematosus. Am J Med. 1992;93(5):513–519. doi: 10.1016/0002-9343(92)90578-Y. [DOI] [PubMed] [Google Scholar]
- 51.Vegiopoulos A, Herzig S. Glucocorticoids, metabolism and metabolic diseases. Mol Cell Endocrinol. 2007;275(1-2):43–61. doi: 10.1016/j.mce.2007.05.015. [DOI] [PubMed] [Google Scholar]
- 52.Radhakutty A, et al. Effects of prednisolone on energy and fat metabolism in patients with rheumatoid arthritis: tissue-specific insulin resistance with commonly used prednisolone doses. Clin Endocrinol (Oxf) 2016;85(5):741–747. doi: 10.1111/cen.13138. [DOI] [PubMed] [Google Scholar]
- 53.Liu DR, et al. A practical guide to the monitoring and management of the complications of systemic corticosteroid therapy. Allergy Asthma Clin Immunol. 2013;9(1):25. doi: 10.1186/1710-1492-9-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sholter DE, Armstrong PW. Adverse effects of corticosteroids on the cardiovascular system. Can J Cardiol. 2000;16(4):505–511. [PubMed] [Google Scholar]
- 55.Garcia-Gomez C, et al. High HDL-cholesterol in women with rheumatoid arthritis on low-dose glucocorticoid therapy. Eur J Clin Invest. 2008;38(9):686–692. doi: 10.1111/j.1365-2362.2008.01994.x. [DOI] [PubMed] [Google Scholar]
- 56.Ettinger WH, et al. Effect of short-term, low-dose corticosteroids on plasma lipoprotein lipids. Atherosclerosis. 1987;63(2-3):167–172. doi: 10.1016/0021-9150(87)90117-1. [DOI] [PubMed] [Google Scholar]
- 57.Agca R, et al. EULAR recommendations for cardiovascular disease risk management in patients with rheumatoid arthritis and other forms of inflammatory joint disorders: 2015/2016 update. Ann Rheum Dis. 2017;76(1):17–28. doi: 10.1136/annrheumdis-2016-209775. [DOI] [PubMed] [Google Scholar]
- 58.Ben-Zvi I, et al. Hydroxychloroquine: from malaria to autoimmunity. Clin Rev Allergy Immunol. 2012;42(2):145–153. doi: 10.1007/s12016-010-8243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schrezenmeier E, Dorner T. Mechanisms of action of hydroxychloroquine and chloroquine: implications for rheumatology. Nat Rev Rheumatol. 2020;16(3):155–166. doi: 10.1038/s41584-020-0372-x. [DOI] [PubMed] [Google Scholar]
- 60.Gómez-Guzmán M, et al. Chronic hydroxychloroquine improves endothelial dysfunction and protects kidney in a mouse model of systemic lupus erythematosus. Hypertension. 2014;64(2):330–337. doi: 10.1161/HYPERTENSIONAHA.114.03587. [DOI] [PubMed] [Google Scholar]
- 61.Rahman R, et al. The effects of hydroxychloroquine on endothelial dysfunction. Pregnancy Hypertens. 2016;6(4):259–262. doi: 10.1016/j.preghy.2016.09.001. [DOI] [PubMed] [Google Scholar]
- 62.Espinola RG, et al. Hydroxychloroquine reverses platelet activation induced by human IgG antiphospholipid antibodies. Thromb Haemost. 2002;87(03):518–522. doi: 10.1055/s-0037-1613033. [DOI] [PubMed] [Google Scholar]
- 63.Cairoli E, et al. Hydroxychloroquine reduces low-density lipoprotein cholesterol levels in systemic lupus erythematosus: a longitudinal evaluation of the lipid-lowering effect. Lupus. 2012;21(11):1178–1182. doi: 10.1177/0961203312450084. [DOI] [PubMed] [Google Scholar]
- 64.Rempenault C, et al. Metabolic and cardiovascular benefits of hydroxychloroquine in patients with rheumatoid arthritis: a systematic review and meta-analysis. Ann Rheum Dis. 2018;77(1):98–103. doi: 10.1136/annrheumdis-2017-211836. [DOI] [PubMed] [Google Scholar]
- 65.Dutta S, Ahmad Y. The efficacy and safety of tacrolimus in rheumatoid arthritis. Ther Adv Musculoskelet Dis. 2011;3(6):283–291. doi: 10.1177/1759720X11419038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lane JCE, et al. Risk of hydroxychloroquine alone and in combination with azithromycin in the treatment of rheumatoid arthritis: a multinational, retrospective study. Lancet Rheumatol. 2020;2(11):e698–e711. doi: 10.1016/S2665-9913(20)30276-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fantini J, et al. Structural and molecular modelling studies reveal a new mechanism of action of chloroquine and hydroxychloroquine against SARS-CoV-2 infection. Int J Antimicrob Agents. 2020;55(5):105960. doi: 10.1016/j.ijantimicag.2020.105960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Miguel L, et al. Primary human CD4+ T cells have diverse levels of membrane lipid order that correlate with their function. J Immunol. 2011;186(6):3505–3516. doi: 10.4049/jimmunol.1002980. [DOI] [PubMed] [Google Scholar]
- 69.Höcherl K, et al. Cyclosporine A suppresses cyclooxygenase-2 expression in the rat kidney. J Am Soc Nephrol. 2002;13(10):2427–2436. doi: 10.1097/01.ASN.0000031702.86799.B9. [DOI] [PubMed] [Google Scholar]
- 70.Chakkera H, et al. Negative cardiovascular consequences of small molecule immunosuppressants. Clin Pharmacol Ther. 2017;102(2):269–276. doi: 10.1002/cpt.738. [DOI] [PubMed] [Google Scholar]
- 71.Farouk SS, Rein JL. The many faces of calcineurin inhibitor toxicity-what the FK? Adv Chronic Kidney Dis. 2020;27(1):56–66. doi: 10.1053/j.ackd.2019.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gueguen Y, et al. Compared effect of immunosuppressive drugs cyclosporine A and rapamycin on cholesterol homeostasis key enzymes CYP27A1 and HMG-CoA reductase. Basic Clin Pharmacol Toxicol. 2007;100(6):392–397. doi: 10.1111/j.1742-7843.2007.00066.x. [DOI] [PubMed] [Google Scholar]
- 73.Rovin BH, et al. Efficacy and safety of voclosporin versus placebo for lupus nephritis (AURORA 1): a double-blind, randomised, multicentre, placebo-controlled, phase 3 trial. Lancet. 2021;397(10289):2070–2080. doi: 10.1016/S0140-6736(21)00578-X. [DOI] [PubMed] [Google Scholar]
- 74.de Groen PC. Cyclosporine, low-density lipoprotein, and cholesterol. Mayo Clin Proc. 1988;63(10):1012–1021. doi: 10.1016/S0025-6196(12)64916-7. [DOI] [PubMed] [Google Scholar]
- 75.Broen JCA, van Laar JM. Mycophenolate mofetil, azathioprine and tacrolimus: mechanisms in rheumatology. Nat Rev Rheumatol. 2020;16(3):167–178. doi: 10.1038/s41584-020-0374-8. [DOI] [PubMed] [Google Scholar]
- 76.Zheng ZH, et al. Mycophenolic acid induces adipocyte-like differentiation and reversal of malignancy of breast cancer cells partly through PPARγ. Eur J Pharmacol. 2011;658(1):1–8. doi: 10.1016/j.ejphar.2011.01.068. [DOI] [PubMed] [Google Scholar]
- 77.Heischmann S, et al. The immunosuppressant mycophenolic acid alters nucleotide and lipid metabolism in an intestinal cell model. Sci Rep. 2017;7(1):45088. doi: 10.1038/srep45088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nam HJ, et al. Azathioprine antagonizes aberrantly elevated lipid metabolism and induces apoptosis in glioblastoma. iScience. 2021;24(3):102238. doi: 10.1016/j.isci.2021.102238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Krol SK, et al. Comprehensive review on betulin as a potent anticancer agent. Biomed Res Int. 2015;2015:584189. doi: 10.1155/2015/584189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tang JJ, et al. Inhibition of SREBP by a small molecule, betulin, improves hyperlipidemia and insulin resistance and reduces atherosclerotic plaques. Cell Metabolism. 2011;13(1):44–56. doi: 10.1016/j.cmet.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 81.Oishi Y, et al. SREBP1 contributes to resolution of pro-inflammatory TLR4 signaling by reprogramming fatty acid metabolism. Cell Metab. 2017;25(2):412–427. doi: 10.1016/j.cmet.2016.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lee JH, et al. SREBP-1a-stimulated lipid synthesis is required for macrophage phagocytosis downstream of TLR4-directed mTORC1. Proc Natl Acad Sci U S A. 2018;115(52):E12228–E12234. doi: 10.1073/pnas.1813458115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Navarro-Millán I, et al. Changes in lipoproteins associated with methotrexate or combination therapy in early rheumatoid arthritis: results from the treatment of early rheumatoid arthritis trial. Arthritis Rheum. 2013;65(6):1430–1438. doi: 10.1002/art.37916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Watanabe J, et al. Proteomic profiling following immunoaffinity capture of high-density lipoprotein: association of acute-phase proteins and complement factors with proinflammatory high-density lipoprotein in rheumatoid arthritis. Arthritis Rheum. 2012;64(6):1828–1837. doi: 10.1002/art.34363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Robertson J, et al. Interleukin-6 blockade raises LDL via reduced catabolism rather than via increased synthesis: a cytokine-specific mechanism for cholesterol changes in rheumatoid arthritis. Ann Rheum Dis. 2017;76(11):1949–1952. doi: 10.1136/annrheumdis-2017-211708. [DOI] [PubMed] [Google Scholar]
- 86.Micha R, et al. Systematic review and meta-analysis of methotrexate use and risk of cardiovascular disease. Am J Cardiol. 2011;108(9):1362–1370. doi: 10.1016/j.amjcard.2011.06.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tam H-W, et al. Sulfasalazine might reduce risk of cardiovascular diseases in patients with ankylosing spondylitis: a nationwide population-based retrospective cohort study. Int J Rheum Dis. 2017;20(3):363–370. doi: 10.1111/1756-185X.12986. [DOI] [PubMed] [Google Scholar]
- 88.Smedegard G, Bjork J. Sulphasalazine: mechanism of action in rheumatoid arthritis. Br J Rheumatol. 1995;34:7–15. doi: 10.1093/rheumatology/34.7.7. [DOI] [PubMed] [Google Scholar]
- 89.Klotz U. Clinical pharmacokinetics of sulphasalazine, its metabolites and other prodrugs of 5-aminosalicylic acid. Clin Pharmacokinet. 1985;10(4):285–302. doi: 10.2165/00003088-198510040-00001. [DOI] [PubMed] [Google Scholar]
- 90.Dirlik M, et al. Effects of sulfasalazine on lipid peroxidation and histologic liver damage in a rat model of obstructive jaundice and obstructive jaundice with lipopolysaccharide-induced sepsis. Curr Ther Res Clin Exp. 2009;70(4):299–315. doi: 10.1016/j.curtheres.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.MacMullan PA, et al. Sulfasalazine and its metabolites inhibit platelet function in patients with inflammatory arthritis. Clin Rheumatol. 2016;35(2):447–455. doi: 10.1007/s10067-014-2769-x. [DOI] [PubMed] [Google Scholar]
- 92.Breedveld FC, Dayer JM. Leflunomide: mode of action in the treatment of rheumatoid arthritis. Ann Rheum Dis. 2000;59(11):841–849. doi: 10.1136/ard.59.11.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Guleria A, et al. NMR-based serum metabolomics reveals reprogramming of lipid dysregulation following cyclophosphamide-based induction therapy in lupus nephritis. J Proteome Res. 2018;17(7):2440–2448. doi: 10.1021/acs.jproteome.8b00192. [DOI] [PubMed] [Google Scholar]
- 94.Iqubal A, et al. Molecular mechanism involved in cyclophosphamide-induced cardiotoxicity: old drug with a new vision. Life Sci. 2019;218:112–131. doi: 10.1016/j.lfs.2018.12.018. [DOI] [PubMed] [Google Scholar]
- 95.Zhang T, Mohan C. Caution in studying and interpreting the lupus metabolome. Arthritis Res Ther. 2020;22(1):172. doi: 10.1186/s13075-020-02264-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Massalska M, et al. Small molecule inhibitors in the treatment of rheumatoid arthritis and beyond: latest updates and potential strategy for fighting COVID-19. Cells. 2020;9(8):21. doi: 10.3390/cells9081876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Markopoulou A, Kyttaris VC. Small molecules in the treatment of systemic lupus erythematosus. Clin Immunol. 2013;148(3):359–368. doi: 10.1016/j.clim.2012.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Thompson C, et al. Anti cytokine therapy in chronic inflammatory arthritis. Cytokine. 2016;86:92–99. doi: 10.1016/j.cyto.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 99.Tang GL, et al. Inhibition of JNK activation through NF-kappa B target genes. Nature. 2001;414(6861):313–317. doi: 10.1038/35104568. [DOI] [PubMed] [Google Scholar]
- 100.McGarry T, et al. JAK/STAT blockade alters synovial bioenergetics, mitochondrial function, and proinflammatory mediators in rheumatoid arthritis. Arthritis Rheumatol. 2018;70(12):1959–1970. doi: 10.1002/art.40569. [DOI] [PubMed] [Google Scholar]
- 101.Lee EB, et al. Tofacitinib versus methotrexate in rheumatoid arthritis. N Engl J Med. 2014;370(25):2377–2386. doi: 10.1056/NEJMoa1310476. [DOI] [PubMed] [Google Scholar]
- 102.Souto A, et al. Lipid profile changes in patients with chronic inflammatory arthritis treated with biologic agents and tofacitinib in randomized clinical trials: a systematic review and meta-analysis. Arthritis Rheumatol. 2015;67(1):117–127. doi: 10.1002/art.38894. [DOI] [PubMed] [Google Scholar]
- 103.Charles-Schoeman C, et al. Potential mechanisms leading to the abnormal lipid profile in patients with rheumatoid arthritis versus healthy volunteers and reversal by tofacitinib. Arthritis Rheumatol. 2015;67(3):616–625. doi: 10.1002/art.38974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Qiu CF, et al. Baricitinib induces LDL-C and HDL-C increases in rheumatoid arthritis: a meta-analysis of randomized controlled trials. Lipids Health Dis. 2019;18(1):11. doi: 10.1186/s12944-018-0955-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wallace DJ, et al. Baricitinib for systemic lupus erythematosus: a double-blind, randomised, placebo-controlled, phase 2 trial. Lancet. 2018;392(10143):222–231. doi: 10.1016/S0140-6736(18)31363-1. [DOI] [PubMed] [Google Scholar]
- 106.Hasni SA, et al. Phase 1 double-blind randomized safety trial of the Janus kinase inhibitor tofacitinib in systemic lupus erythematosus. Nat Commun. 2021;12(1):3391. doi: 10.1038/s41467-021-23361-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.McInnes IB, et al. Open-label tofacitinib and double-blind atorvastatin in rheumatoid arthritis patients: a randomised study. Ann Rheum Dis. 2014;73(1):124–131. doi: 10.1136/annrheumdis-2012-202442. [DOI] [PubMed] [Google Scholar]
- 108.Charles-Schoeman C, et al. Effects of tofacitinib and other DMARDs on lipid profiles in rheumatoid arthritis: implications for the rheumatologist. Semin Arthritis Rheum. 2016;46(1):71–80. doi: 10.1016/j.semarthrit.2016.03.004. [DOI] [PubMed] [Google Scholar]
- 109.Samuelson BT, et al. The impact of ruxolitinib on thrombosis in patients with polycythemia vera and myelofibrosis: a meta-analysis. Blood Coagul Fibrinolysis. 2016;27(6):648–652. doi: 10.1097/MBC.0000000000000446. [DOI] [PubMed] [Google Scholar]
- 110.Cohen SB. JAK inhibitors and VTE risk: how concerned should we be? Nat Rev Rheumatol. 2021;17(3):133–134. doi: 10.1038/s41584-021-00575-5. [DOI] [PubMed] [Google Scholar]
- 111. US Food and Drug Administration. FDA requires warnings about increased risk of serious heart-related events, cancer, blood clots, and death for JAK inhibitors that treat certain chronic inflammatory conditions. https://www.fda.gov/drugs/drug-safety-and-availability/fda-requires-warnings-about-increased-risk-serious-heart-related-events-cancer-blood-clots-and-death Updated September 16, 2021. Accessed October 19, 2021.
- 112.Hernandez-Florez D, Valor L. Protein-kinase inhibitors: a new treatment pathway for autoimmune and inflammatory diseases? Reumatol Clin. 2016;12(2):91–99. doi: 10.1016/j.reuma.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 113.Damjanov N. Efficacy, pharmacodynamics, and safety of VX-702, a novel p38 MAPK inhibitor, in rheumatoid arthritis results of two randomized, double-blind, placebo-controlled clinical studies. Arthritis Rheum. 2009;60(5):1232–1241. doi: 10.1002/art.24485. [DOI] [PubMed] [Google Scholar]
- 114.Lawan A, Bennett AM. Mitogen-activated protein kinase regulation in hepatic metabolism. Trends Endocrinol Metab. 2017;28(12):868–878. doi: 10.1016/j.tem.2017.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kotzka J, et al. Insulin-activated Erk-mitogen-activated protein kinases phosphorylate sterol regulatory element-binding protein-2 at serine residues 432 and 455 in vivo. J Biol Chem. 2004;279(21):22404–22411. doi: 10.1074/jbc.M401198200. [DOI] [PubMed] [Google Scholar]
- 116.Hu ED, et al. Inhibition of adipogenesis through MAP kinase-mediated phosphorylation of PPAR gamma. Science. 1996;274(5295):2100–2103. doi: 10.1126/science.274.5295.2100. [DOI] [PubMed] [Google Scholar]
- 117.Malemud CJ. Suppression of autoimmune arthritis by small molecule inhibitors of the JAK/STAT pathway. Pharmaceuticals (Basel) 2010;3(5):1446–1455. doi: 10.3390/ph3051446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Pai S, Thomas R. Immune deficiency or hyperactivity-Nf-κb illuminates autoimmunity. J Autoimmun. 2008;31(3):245–251. doi: 10.1016/j.jaut.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 119.Baker RG, et al. NF-κB, inflammation, and metabolic disease. Cell Metab. 2011;13(1):11–22. doi: 10.1016/j.cmet.2010.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Xie SS, et al. Iguratimod as a new drug for rheumatoid arthritis: current landscape. Front Pharmacol. 2020;11:73. doi: 10.3389/fphar.2020.00073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Hara M, et al. Safety and efficacy of combination therapy of iguratimod with methotrexate for patients with active rheumatoid arthritis with an inadequate response to methotrexate: an open-label extension of a randomized, double-blind, placebo-controlled trial. Mod Rheumatol. 2014;24(3):410–418. doi: 10.3109/14397595.2013.843756. [DOI] [PubMed] [Google Scholar]
- 122.Yu XH, et al. Interleukin-18 and interleukin-12 together downregulate ATP-binding cassette transporter A1 expression through the interleukin-18R/nuclear factor-κB signaling pathway in THP-1 macrophage-derived foam cells. Circ J. 2012;76(7):1780–1791. doi: 10.1253/circj.CJ-11-1338. [DOI] [PubMed] [Google Scholar]
- 123.Yu XH, et al. Nuclear factor-κ B activation as a pathological mechanism of lipid metabolism and atherosclerosis. Adv Clin Chem. 2015;70:1–30. doi: 10.1016/bs.acc.2015.03.004. [DOI] [PubMed] [Google Scholar]
- 124.Ferreira V, et al. Macrophage-specific inhibition of NF-κ B activation reduces foam-cell formation. Atherosclerosis. 2007;192(2):283–290. doi: 10.1016/j.atherosclerosis.2006.07.018. [DOI] [PubMed] [Google Scholar]
- 125.Zhu XW, et al. Macrophage ABCA1 reduces MyD88-dependent Toll-like receptor trafficking to lipid rafts by reduction of lipid raft cholesterol. J Lipid Res. 2010;51(11):3196–3206. doi: 10.1194/jlr.M006486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kanters E, et al. Inhibition of NF-κ B activation in macrophages increases atherosclerosis in LDL receptor-deficient mice. J Clin Invest. 2003;112(8):1176–1185. doi: 10.1172/JCI200318580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Soskic SS, et al. Peroxisome proliferator-activated receptors and atherosclerosis. Angiology. 2011;62(7):523–534. doi: 10.1177/0003319711401012. [DOI] [PubMed] [Google Scholar]
- 128.Lowell CA. Src-family and Syk kinases in activating and inhibitory pathways in innate immune cells: signaling cross talk. Cold Spring Harb Perspect Biol. 2011;3(3):a002352. doi: 10.1101/cshperspect.a002352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Rozovski U, et al. Ibrutinib inhibits free fatty acid metabolism in chronic lymphocytic leukemia. Leuk Lymphoma. 2018;59(11):2686–2691. doi: 10.1080/10428194.2018.1439167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Sharif-Askari B, et al. Bruton’s tyrosine kinase is at the crossroads of metabolic adaptation in primary malignant human lymphocytes. Sci Rep. 2019;9(1):11069. doi: 10.1038/s41598-019-47305-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Strand V, et al. Immunogenicity of biologic agents in rheumatology. Nat Rev Rheumatol. 2021;17(2):81–97. doi: 10.1038/s41584-020-00540-8. [DOI] [PubMed] [Google Scholar]
- 132.Bishop EL, et al. Control of T cell metabolism by cytokines and hormones. Front Immunol. 2021;12:15. doi: 10.3389/fimmu.2021.653605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Shi J, et al. Cytokines and abnormal glucose and lipid metabolism. Front Endocrinol (Lausanne) 2019;10:16. doi: 10.3389/fendo.2019.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Sebba A. Tocilizumab: the first interleukin-6-receptor inhibitor. Am J Health Syst Pharm. 2008;65(15):1413–1418. doi: 10.2146/ajhp070449. [DOI] [PubMed] [Google Scholar]
- 135.Dhillon S. Intravenous tocilizumab: a review of its use in adults with rheumatoid arthritis. BioDrugs. 2014;28(1):75–106. doi: 10.1007/s40259-013-0076-8. [DOI] [PubMed] [Google Scholar]
- 136.McInnes IB, et al. Effect of interleukin-6 receptor blockade on surrogates of vascular risk in rheumatoid arthritis: MEASURE, a randomised, placebo-controlled study. Ann Rheum Dis. 2015;74(4):694–702. doi: 10.1136/annrheumdis-2013-204345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Giles JT, et al. Cardiovascular safety of tocilizumab versus etanercept in rheumatoid arthritis: a randomized controlled trial. Arthritis Rheumatol. 2020;72(1):31–40. doi: 10.1002/art.41095. [DOI] [PubMed] [Google Scholar]
- 138.Pierini FS, et al. Effect of tocilizumab on LDL and HDL characteristics in patients with rheumatoid arthritis. An observational study. Rheumatol Ther. 2021;8(2):803–815. doi: 10.1007/s40744-021-00304-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Daien CI, et al. Effect of TNF inhibitors on lipid profile in rheumatoid arthritis: a systematic review with meta-analysis. Ann Rheum Dis. 2012;71(6):862–868. doi: 10.1136/annrheumdis-2011-201148. [DOI] [PubMed] [Google Scholar]
- 140.Dixon WG, et al. Reduction in the incidence of myocardial infarction in patients with rheumatoid arthritis who respond to anti-tumor necrosis factor alpha therapy: results from the British Society for Rheumatology Biologics Register. Arthritis Rheum. 2007;56(9):2905–2912. doi: 10.1002/art.22809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Charles-Schoeman C, et al. Remodeling of the HDL proteome with treatment response to abatacept or adalimumab in the AMPLE trial of patients with rheumatoid arthritis. Atherosclerosis. 2018;275:107–114. doi: 10.1016/j.atherosclerosis.2018.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Gabay C, et al. Tocilizumab monotherapy versus adalimumab monotherapy for treatment of rheumatoid arthritis (ADACTA): a randomised, double-blind, controlled phase 4 trial. Lancet. 2013;381(9877):1541–1550. doi: 10.1016/S0140-6736(13)60250-0. [DOI] [PubMed] [Google Scholar]
- 143.Fernandez-Nebro A, et al. The effects of rituximab on the lipid profile of patients with active systemic lupus erythematosus: results from a nationwide cohort in Spain (LESIMAB) Lupus. 2014;23(10):1014–1022. doi: 10.1177/0961203314534909. [DOI] [PubMed] [Google Scholar]
- 144.Kerekes G, et al. Effects of rituximab treatment on endothelial dysfunction, carotid atherosclerosis, and lipid profile in rheumatoid arthritis. Clin Rheumatol. 2009;28(6):705–710. doi: 10.1007/s10067-009-1095-1. [DOI] [PubMed] [Google Scholar]
- 145.Novikova DS, et al. The effects of rituximab on lipids, arterial stiffness and carotid intima-media thickness in rheumatoid arthritis. J Korean Med Sci. 2016;31(2):202–207. doi: 10.3346/jkms.2016.31.2.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Huang HT, et al. Predicting dyslipidemia after liver transplantation: a significant role of recipient metabolic inflammation profile. World J Gastroenterol. 2020;26(19):2374–2387. doi: 10.3748/wjg.v26.i19.2374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.McDevitt H, et al. Multiple roles for tumor necrosis factor-alpha and lymphotoxin alpha/beta in immunity and autoimmunity. Arthritis Res. 2002;4:S141–S152. doi: 10.1186/ar570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Negrin KA, et al. IL-1 signaling in obesity-induced hepatic lipogenesis and steatosis. PLoS One. 2014;9(9):15. doi: 10.1371/journal.pone.0107265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Wang HN, Huang YH. Changes in metabolic parameters in psoriatic patients treated with secukinumab. Ther Adv Chronic Dis. 2020;11:2040622320944777. doi: 10.1177/2040622320944777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Varshney P, et al. Transcriptome profiling unveils the role of cholesterol in IL-17A signaling in psoriasis. Sci Rep. 2016;6(1):19295. doi: 10.1038/srep19295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Huang LH, et al. Interleukin-17 drives interstitial entrapment of tissue lipoproteins in experimental psoriasis. Cell Metab. 2019;29(2):475–487. doi: 10.1016/j.cmet.2018.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Yu X-H, et al. Interleukin-17A in lipid metabolism and atherosclerosis. Clin Chim Acta. 2014;431:33–39. doi: 10.1016/j.cca.2014.01.012. [DOI] [PubMed] [Google Scholar]
- 153.Zhou QD, et al. Interferon-mediated reprogramming of membrane cholesterol to evade bacterial toxins. Nat Immunol. 2020;21(7):746–755. doi: 10.1038/s41590-020-0695-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Blanc M, et al. Host defense against viral infection involves interferon mediated down-regulation of sterol biosynthesis. PLoS Biol. 2011;9(3):19. doi: 10.1371/journal.pbio.1000598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Janas E, et al. Rituxan (anti-CD20 antibody)-induced translocation of CD20 into lipid rafts is crucial for calcium influx and apoptosis. Clin Exp Immunol. 2005;139(3):439–446. doi: 10.1111/j.1365-2249.2005.02720.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Nozaki Y, et al. Rituximab activates Syk and AKT in CD20-positive B cell lymphoma cells dependent on cell membrane cholesterol levels. Exp Hematol. 2013;41(8):687–696. doi: 10.1016/j.exphem.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 157.Glennie MJ, et al. Mechanisms of killing by anti-CD20 monoclonal antibodies. Mol Immunol. 2007;44(16):3823–3837. doi: 10.1016/j.molimm.2007.06.151. [DOI] [PubMed] [Google Scholar]
- 158.Yang W, et al. Potentiating the antitumour response of CD8(+) T cells by modulating cholesterol metabolism. Nature. 2016;531(7596):651–655. doi: 10.1038/nature17412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Schmidt NM, et al. Targeting human Acyl-CoA:cholesterol acyltransferase as a dual viral and T cell metabolic checkpoint. Nat Commun. 2021;12(1):2814. doi: 10.1038/s41467-021-22967-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Fogelman AM. When good cholesterol goes bad. Nat Med. 2004;10(9):902–903. doi: 10.1038/nm0904-902. [DOI] [PubMed] [Google Scholar]
- 161.Ansell BJ, et al. Inflammatory/antiinflammatory properties of high-density lipoprotein distinguish patients from control subjects better than high-density lipoprotein cholesterol levels and are favorably affected by simvastatin treatment. Circulation. 2003;108(22):2751–2756. doi: 10.1161/01.CIR.0000103624.14436.4B. [DOI] [PubMed] [Google Scholar]
- 162.Das S, et al. Outcome of rheumatoid arthritis following adjunct statin therapy. Indian J Pharmacol. 2015;47(6):605–609. doi: 10.4103/0253-7613.169585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Chataway J, et al. Effect of high-dose simvastatin on brain atrophy and disability in secondary progressive multiple sclerosis (MS-STAT): a randomised, placebo-controlled, phase 2 trial. Lancet. 2014;383(9936):2213–2221. doi: 10.1016/S0140-6736(13)62242-4. [DOI] [PubMed] [Google Scholar]
- 164.Ifergan I, et al. Statins reduce human blood-brain barrier permeability and restrict leukocyte migration: relevance to multiple sclerosis. Ann Neurol. 2006;60(1):45–55. doi: 10.1002/ana.20875. [DOI] [PubMed] [Google Scholar]
- 165.Yu HH, et al. Statin reduces mortality and morbidity in systemic lupus erythematosus patients with hyperlipidemia: a nationwide population-based cohort study. Atherosclerosis. 2015;243(1):11–18. doi: 10.1016/j.atherosclerosis.2015.08.030. [DOI] [PubMed] [Google Scholar]
- 166.Ruiz-Limon P, et al. Atherosclerosis and cardiovascular disease in systemic lupus erythematosus: effects of in vivo statin treatment. Ann Rheum Dis. 2015;74(7):1450–1458. doi: 10.1136/annrheumdis-2013-204351. [DOI] [PubMed] [Google Scholar]
- 167.Aikawa M, et al. An HMG-CoA reductase inhibitor, cerivastatin, suppresses growth of macrophages expressing matrix metalloproteinases and tissue factor in vivo and in vitro. Circulation. 2001;103(2):276–283. doi: 10.1161/01.CIR.103.2.276. [DOI] [PubMed] [Google Scholar]
- 168.Waehre T, et al. Increased expression of interleukin-1 in coronary artery disease with downregulatory effects of HMG-CoA reductase inhibitors. Circulation. 2004;109(16):1966–1972. doi: 10.1161/01.CIR.0000125700.33637.B1. [DOI] [PubMed] [Google Scholar]
- 169.Schanberg LE, et al. Use of atorvastatin in systemic lupus erythematosus in children and adolescents. Arthritis Rheum. 2012;64(1):285–296. doi: 10.1002/art.30645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Petri MA, et al. Lupus Atherosclerosis Prevention Study (LAPS) Ann Rheum Dis. 2011;70(5):760–765. doi: 10.1136/ard.2010.136762. [DOI] [PubMed] [Google Scholar]
- 171.Coelewij L, et al. Serum metabolomic signatures can predict subclinical atherosclerosis in patients with systemic lupus erythematosus. Arterioscler Thromb Vasc Biol. 2021;41(4):1446–1458. doi: 10.1161/ATVBAHA.120.315321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Robinson GA, et al. Increased apolipoprotein-B:A1 ratio predicts cardiometabolic risk in patients with juvenile onset SLE. EBioMedicine. 2021;65:103243. doi: 10.1016/j.ebiom.2021.103243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Waddington KE, et al. Using serum metabolomics to predict development of anti-drug antibodies in multiple sclerosis patients treated with IFNβ. Front Immunol. 2020;11:1527. doi: 10.3389/fimmu.2020.01527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Shaw JA, et al. Infusion of reconstituted high-density lipoprotein leads to acute changes in human atherosclerotic plaque. Circ Res. 2008;103(10):1084–1091. doi: 10.1161/CIRCRESAHA.108.182063. [DOI] [PubMed] [Google Scholar]
- 175.Ray KK, et al. Two phase 3 trials of inclisiran in patients with elevated LDL cholesterol. N Engl J Med. 2020;382(16):1507–1519. doi: 10.1056/NEJMoa1912387. [DOI] [PubMed] [Google Scholar]
- 176.Schmidt-Arras D, Rose-John S. Endosomes as signaling platforms for IL-6 family cytokine receptors. Front Cell Dev Biol. 2021;9:688314. doi: 10.3389/fcell.2021.688314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Jury EC, et al. Atorvastatin restores Lck expression and lipid raft-associated signaling in T cells from patients with systemic lupus erythematosus. J Immunol. 2006;177(10):7416–7422. doi: 10.4049/jimmunol.177.10.7416. [DOI] [PubMed] [Google Scholar]
- 178.Shitara Y, Sugiyama Y. Pharmacokinetic and pharmacodynamic alterations of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors: drug-drug interactions and interindividual differences in transporter and metabolic enzyme functions. Pharmacol Ther. 2006;112(1):71–105. doi: 10.1016/j.pharmthera.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 179.Blaho VA, et al. HDL-bound sphingosine-1-phosphate restrains lymphopoiesis and neuroinflammation. Nature. 2015;523(7560):342–346. doi: 10.1038/nature14462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Li J, et al. Dietary inflammatory potential and risk of cardiovascular disease among men and women in the U.S. J Am Coll Cardiol. 2020;76(19):2181–2193. doi: 10.1016/j.jacc.2020.09.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Stockwell BR, et al. Ferroptosis: a regulated cell death nexus linking metabolism, redox biology, and disease. Cell. 2017;171(2):273–285. doi: 10.1016/j.cell.2017.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Fan YY, et al. Dietary docosahexaenoic acid suppresses T cell protein kinase C theta lipid raft recruitment and IL-2 production. J Immunol. 2004;173(10):6151–6160. doi: 10.4049/jimmunol.173.10.6151. [DOI] [PubMed] [Google Scholar]
- 183.da Silva SGL, et al. The effect of nutritional intervention on the lipid profile and dietary intake of adolescents with juvenile systemic lupus erythematosus: a randomized, controlled trial. Lupus. 2018;27(5):820–827. doi: 10.1177/0961203317751851. [DOI] [PubMed] [Google Scholar]
- 184.Walton AJ, et al. Dietary fish oil and the severity of symptoms in patients with systemic lupus erythematosus. Ann Rheum Dis. 1991;50(7):463–466. doi: 10.1136/ard.50.7.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Philippou E, et al. Rheumatoid arthritis and dietary interventions: systematic review of clinical trials. Nutr Rev. 2021;79(4):410–428. doi: 10.1093/nutrit/nuaa033. [DOI] [PubMed] [Google Scholar]
- 186.Ilowite NT, et al. Effects of dietary modification and fish oil supplementation on dyslipoproteinemia in pediatric systemic lupus erythematosus. J Rheumatol. 1995;22(7):1347–1351. [PubMed] [Google Scholar]
- 187.Clark WF, et al. Omega-3 fatty acid dietary supplementation in systemic lupus erythematosus. Kidney Int. 1989;36(4):653–660. doi: 10.1038/ki.1989.242. [DOI] [PubMed] [Google Scholar]
- 188.Davies RJ, et al. Weight loss and improvements in fatigue in systemic lupus erythematosus: a controlled trial of a low glycaemic index diet versus a calorie restricted diet in patients treated with corticosteroids. Lupus. 2012;21(6):649–655. doi: 10.1177/0961203312436854. [DOI] [PubMed] [Google Scholar]
- 189.Hirten RP, et al. Combining biologics in inflammatory bowel disease and other immune mediated inflammatory disorders. Clin Gastroenterol Hepatol. 2018;16(9):1374–1384. doi: 10.1016/j.cgh.2018.02.024. [DOI] [PubMed] [Google Scholar]
- 190.Mardini IA, FitzGerald GA. Selective inhibitors of cyclooxygenase-2: a growing class of anti-inflammatory drugs. Mol Interv. 2001;1(1):30–38. [PubMed] [Google Scholar]
- 191.Crofford LJ, et al. Cyclooxygenase-1 and -2 expression in rheumatoid synovial tissues. Effects of interleukin-1 beta, phorbol ester, and corticosteroids. J Clin Invest. 1994;93(3):1095–1101. doi: 10.1172/JCI117060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Rose JW, et al. Inflammatory cell expression of cyclooxygenase-2 in the multiple sclerosis lesion. J Neuroimmunol. 2004;149(1-2):40–49. doi: 10.1016/j.jneuroim.2003.12.021. [DOI] [PubMed] [Google Scholar]
- 193.Xu LT, et al. Human lupus T cells resist inactivation and escape death by upregulating COX-2. Nat Med. 2004;10(4):411–415. doi: 10.1038/nm1005. [DOI] [PubMed] [Google Scholar]
- 194.Petta I, et al. The interactome of the glucocorticoid receptor and its influence on the actions of glucocorticoids in combatting inflammatory and infectious diseases. Microbiol Mol Biol Rev. 2016;80(2):495–522. doi: 10.1128/MMBR.00064-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Barnes PJ. Molecular mechanisms and cellular effects of glucocorticosteroids. Immunol Allergy Clin North Am. 2005;25(3):451–468. doi: 10.1016/j.iac.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 196.Moghadam-Kia S, Werth VP. Prevention and treatment of systemic glucocorticoid side effects. Int J Dermatol. 2010;49(3):239–248. doi: 10.1111/j.1365-4632.2009.04322.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Mauthe M, et al. Chloroquine inhibits autophagic flux by decreasing autophagosome-lysosome fusion. Autophagy. 2018;14(8):1435–1455. doi: 10.1080/15548627.2018.1474314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Sundelin SP, Terman A. Different effects of chloroquine and hydroxychloroquine on lysosomal function in cultured retinal pigment epithelial cells. APMIS. 2002;110(6):481–489. doi: 10.1034/j.1600-0463.2002.100606.x. [DOI] [PubMed] [Google Scholar]
- 199.Lotteau V, et al. Intracellular transport of class II MHC molecules directed by invariant chain. Nature. 1990;348(6302):600–605. doi: 10.1038/348600a0. [DOI] [PubMed] [Google Scholar]
- 200.Kuznik A, et al. Mechanism of endosomal TLR inhibition by antimalarial drugs and imidazoquinolines. J Immunol. 2011;186(8):4794–4804. doi: 10.4049/jimmunol.1000702. [DOI] [PubMed] [Google Scholar]
- 201.An J, et al. Antimalarial drugs as immune modulators: new mechanisms for old drugs. Annu Rev Med. 2017;68:317–330. doi: 10.1146/annurev-med-043015-123453. [DOI] [PubMed] [Google Scholar]
- 202.Vaeth M, et al. Store-operated Ca2+ entry controls clonal expansion of T cells through metabolic reprogramming. Immunity. 2017;47(4):664–679. doi: 10.1016/j.immuni.2017.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Gwack Y, et al. Signalling to transcription: store-operated Ca2+ entry and NFAT activation in lymphocytes. Cell Calcium. 2007;42(2):145–156. doi: 10.1016/j.ceca.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 204.Park YJ, et al. The role of calcium-calcineurin-NFAT signaling pathway in health and autoimmune diseases. Front Immunol. 2020;11:14. doi: 10.3389/fimmu.2020.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Wu QH, Kuca K. Metabolic pathway of cyclosporine a and its correlation with nephrotoxicity. Curr Drug Metab. 2019;20(2):84–90. doi: 10.2174/1389200219666181031113505. [DOI] [PubMed] [Google Scholar]
- 206.Ransom JT. Mechanism of action of mycophenolate mofetil. Ther Drug Monit. 1995;17(6):681–684. doi: 10.1097/00007691-199512000-00023. [DOI] [PubMed] [Google Scholar]
- 207.Allison AC, Eugui EM. Mycophenolate mofetil and its mechanisms of action. Immunopharmacology. 2000;47(2):85–118. doi: 10.1016/s0162-3109(00)00188-0. [DOI] [PubMed] [Google Scholar]
- 208.Suthanthiran M, Strom TB. Immunoregulatory drugs: mechanistic basis for use in organ transplantation. Pediatr Nephrol. 1997;11(5):651–657. doi: 10.1007/s004670050359. [DOI] [PubMed] [Google Scholar]
- 209.Vanscoik KG, et al. The pharmacology and metabolism of the thiopurine drugs 6-mercaptopurine and azathioprine. Drug Metab Rev. 1985;16(1-2):157–174. doi: 10.3109/03602538508991433. [DOI] [PubMed] [Google Scholar]
- 210.VanOs EC, et al. Azathioprine pharmacokinetics after intravenous, oral, delayed release oral and rectal foam administration. Gut. 1996;39(1):63–68. doi: 10.1136/gut.39.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Baugh CM, et al. Polygammaglutamyl metabolites of methotrexate. Biochem Biophys Res Commun. 1973;52(1):27–34. doi: 10.1016/0006-291X(73)90949-2. [DOI] [PubMed] [Google Scholar]
- 212.Cutolo M, et al. Anti-inflammatory mechanisms of methotrexate in rheumatoid arthritis. Ann Rheum Dis. 2001;60(8):729–735. doi: 10.1136/ard.60.8.729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Gubner R, et al. Therapeutic suppression of tissue reactivity. II. Effect of aminopterin in rheumatoid arthritis and psoriasis. Am J Med Sci. 1951;221(2):176–182. doi: 10.1097/00000441-195102000-00009. [DOI] [PubMed] [Google Scholar]
- 214.Bedoui Y, et al. Methotrexate an old drug with new tricks. Int J Mol Sci. 2019;20(20):5023. doi: 10.3390/ijms20205023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Brown PM, et al. Mechanism of action of methotrexate in rheumatoid arthritis, and the search for biomarkers. Nat Rev Rheumatol. 2016;12(12):731–742. doi: 10.1038/nrrheum.2016.175. [DOI] [PubMed] [Google Scholar]
- 216.Bouma MG, et al. Differential regulatory effects of adenosine on cytokine release by activated human monocytes. J Immunol. 1994;153(9):4159–4168. [PubMed] [Google Scholar]
- 217.Pirkmajer S, et al. Methotrexate promotes glucose uptake and lipid oxidation in skeletal muscle via AMPK activation. Diabetes. 2015;64(2):360–369. doi: 10.2337/db14-0508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Solomon DH, et al. Association between disease-modifying antirheumatic drugs and diabetes risk in patients with rheumatoid arthritis and psoriasis. JAMA. 2011;305(24):2525–2531. doi: 10.1001/jama.2011.878. [DOI] [PubMed] [Google Scholar]
- 219.Toms TE, et al. Methotrexate therapy associates with reduced prevalence of the metabolic syndrome in rheumatoid arthritis patients over the age of 60- more than just an anti-inflammatory effect? A cross sectional study. Arthritis Res Ther. 2009;11(4):R110. doi: 10.1186/ar2765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Rozman B, et al. Leflunomide and hypertension. Ann Rheum Dis. 2002;61(6):567–569. doi: 10.1136/ard.61.6.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Dong GF, et al. Effect of leflunomide on the abnormal expression of lipid rafts and F-actin in B lymphocytes from patients with systemic lupus erythematosus. J Immunol Res. 2015;2015:832916. doi: 10.1155/2015/832916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Hipkens JH, et al. Role of aldehyde dehydrogenase in the metabolism-dependent biological activity of cyclophosphamide. Cancer Res. 1981;41(9):3571–3583. [PubMed] [Google Scholar]
- 223.Ahlmann M, Hempel G. The effect of cyclophosphamide on the immune system: implications for clinical cancer therapy. Cancer Chemother Pharmacol. 2016;78(4):661–671. doi: 10.1007/s00280-016-3152-1. [DOI] [PubMed] [Google Scholar]
- 224.Jones RJ, et al. Assessment of aldehyde dehydrogenase in viable cells. Blood. 1995;85(10):2742–2746. doi: 10.1182/blood.V85.10.2742.bloodjournal85102742. [DOI] [PubMed] [Google Scholar]
- 225. Thomas SS, et al. Immunosuppressives: cyclosporine, cyclophosphamide, azathioprine, mycophenolate mofetil. In: Hochberg MC, et al., eds. Rheumatology. 6th ed. Mosby; 2015:459–467. [Google Scholar]
- 226.O’Shea JJ, Plenge R. JAK and STAT signaling molecules in immunoregulation and immune-mediated disease. Immunity. 2012;36(4):542–550. doi: 10.1016/j.immuni.2012.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Dodington DW, et al. JAK/STAT — emerging players in metabolism. Trends Endocrinol Metab. 2018;29(1):55–65. doi: 10.1016/j.tem.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 228.Abbott MJ, et al. IL-15 activates the Jak3/STAT3 signaling pathway to mediate glucose uptake in skeletal muscle cells. Front Physiol. 2017;31:1. doi: 10.3389/fphys.2016.00626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Grzelkowska-Kowalczyk K, Wieteska-Skrzeczynska W. Treatment with IFN-gamma prevents insulin-dependent PKB, p70(S6k) phosphorylation and protein synthesis in mouse C2C12 myogenic cells. Cell Biol Int. 2010;34(1):117–124. doi: 10.1042/CBI20090135. [DOI] [PubMed] [Google Scholar]
- 230.Taylor PC. Clinical efficacy of launched JAK inhibitors in rheumatoid arthritis. Rheumatology (Oxford) 2019;58(suppl 1):17–i26. doi: 10.1093/rheumatology/key225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Kahl L, et al. Safety, tolerability, efficacy and pharmacodynamics of the selective JAK1 inhibitor GSK2586184 in patients with systemic lupus erythematosus. Lupus. 2016;25(13):1420–1430. doi: 10.1177/0961203316640910. [DOI] [PubMed] [Google Scholar]
- 232.Schett G, et al. Activation, differential localization, and regulation of the stress-activated protein kinases, extracellular signal-regulated kinase, c-JUN N-terminal kinase, and p38 mitogen-activated protein kinase, in synovial tissue and cells in rheumatoid arthritis. Arthritis Rheum. 2000;43(11):2501–2512. doi: 10.1002/1529-0131(200011)43:11<2501::AID-ANR18>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 233.Lopez-Santalla M, et al. Tyr(323)-dependent p38 activation is associated with rheumatoid arthritis and correlates with disease activity. Arthritis Rheum. 2011;63(7):1833–1842. doi: 10.1002/art.30375. [DOI] [PubMed] [Google Scholar]
- 234.Cully M, et al. A role for p38 stress-activated protein kinase in regulation of cell growth via TORC1. Mol Cell Biol. 2010;30(2):481–495. doi: 10.1128/MCB.00688-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Carr EL, et al. Glutamine uptake and metabolism are coordinately regulated by ERK/MAPK during T lymphocyte activation. J Immunol. 2010;185(2):1037–1044. doi: 10.4049/jimmunol.0903586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Yu H, et al. Targeting NF-κB pathway for the therapy of diseases: mechanism and clinical study. Signal Transduct Target Ther. 2020;5(1):209. doi: 10.1038/s41392-020-00312-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Marok R, et al. Activation of the transcription factor nuclear factor-kappa B in human inflamed synovial tissue. Arthritis Rheum. 1996;39(4):583–591. doi: 10.1002/art.1780390407. [DOI] [PubMed] [Google Scholar]
- 238.Fu LC, et al. BAFF-R promotes cell proliferation and survival through interaction with IKK beta and NF-kappa B/c-Rel in the nucleus of normal and neoplastic B-lymphoid cells. Blood. 2009;113(19):4627–4636. doi: 10.1182/blood-2008-10-183467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Xu YZ, et al. Regulatory effect of iguratimod on the balance of th subsets and inhibition of inflammatory cytokines in patients with rheumatoid arthritis. Mediators Inflamm. 2015;2015:13. doi: 10.1155/2015/356040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Lv JH, et al. Development of bruton’s tyrosine kinase inhibitors for rheumatoid arthritis. Curr Med Chem. 2018;25(42):5847–5859. doi: 10.2174/0929867325666180316121951. [DOI] [PubMed] [Google Scholar]
- 241.Iwata S, et al. Activation of Syk-Btk signal in peripheral blood B cells in patients with rheumatoid arthritis: a potential target for abatacept therapy. Arthritis Rheumatol. 2015;67(1):63–72. doi: 10.1002/art.38895. [DOI] [PubMed] [Google Scholar]
- 242.Ghosh D, Tsokos GC. Spleen tyrosine kinase: an Src family of non-receptor kinase has multiple functions and represents a valuable therapeutic target in the treatment of autoimmune and inflammatory diseases. Autoimmunity. 2010;43(1):48–55. doi: 10.3109/08916930903374717. [DOI] [PubMed] [Google Scholar]
- 243.Tan SL, et al. Targeting the SYK-BTK axis for the treatment of immunological and hematological disorders: recent progress and therapeutic perspectives. Pharmacol Ther. 2013;138(2):294–309. doi: 10.1016/j.pharmthera.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 244.Palacios EH, Weiss A. Distinct roles for Syk and ZAP-70 during early thymocyte development. J Exp Med. 2007;204(7):1703–1715. doi: 10.1084/jem.20070405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Strand V, et al. Biologic therapies in rheumatology: lessons learned, future directions. Nat Rev Drug Discov. 2007;6(1):75–92. doi: 10.1038/nrd2196. [DOI] [PubMed] [Google Scholar]
- 246.Park SH. Biologic therapies for the treatment of systemic lupus erythematosus. J Korean Med Assoc. 2021;64(2):109–115. doi: 10.5124/jkma.2021.64.2.109. [DOI] [Google Scholar]
- 247.Gabay C, et al. IL-1 pathways in inflammation and human diseases. Nat Rev Rheumatol. 2010;6(4):232–241. doi: 10.1038/nrrheum.2010.4. [DOI] [PubMed] [Google Scholar]
- 248.Cavalli G, Dinarello CA. Treating rheumatological diseases and co-morbidities with interleukin-1 blocking therapies. Rheumatology (Oxford) 2015;54(12):2134–2144. doi: 10.1093/rheumatology/kev269. [DOI] [PMC free article] [PubMed] [Google Scholar]