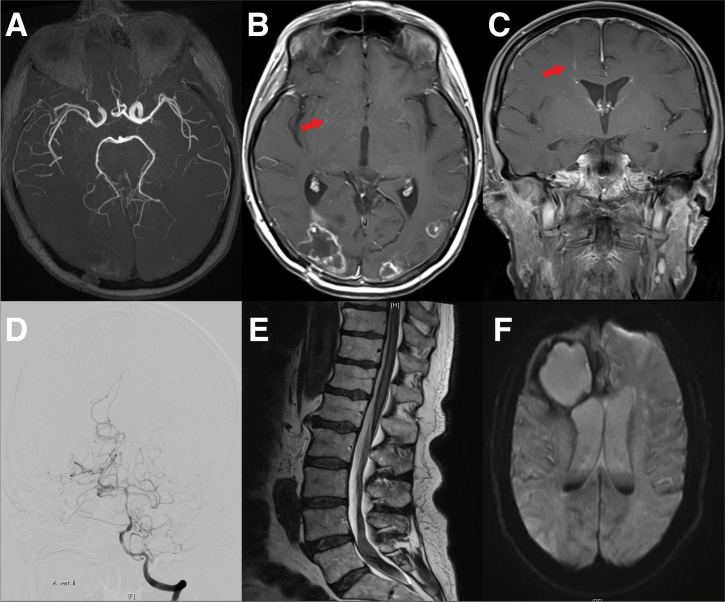
Figure 6.
Cranial MRI of a 44-year-old female patient with NSCLC and pembrolizumab therapy. (A) Shows vascular imaging with no evidence of vasculitis-type changes in the large cerebral vessels. (B) Transversal gadolinium enhanced T1 weighted MRI with the remains of the occipitally located brain metastasis, as well as periventricular contrast medium accumulations suspicious for vasculitis (arrow). (C) A frontal gadolinium enhanced T1 weighted MR of the same patient. Again, the arrow indicates suspicious contrast agent accumulations. (D–F) Cranial MRI Scans and vertebral column MRI of a 72-year-old patient with melanoma. The Patient had been treated with nivolumab for 15 months. The patient then developed a headache and paraparesis. Cerebral angiography showed caliber changes of the left middle cerebral artery and the basilar artery. Due to vasculitis, the patient developed prolonged bleeding with siderosis-associated myelopathy. (D) Cerebral angiography with caliber changes of the cerebral vessels. (E) Cranial MRI of the lower spinal cord with bleeding in the caudal region. (F) Cranial MRI with bleeding of the metastasis and blood in the liquor system.