Abstract
Background
Liver transplantation (LT) for alcohol-related liver disease has historically been reserved for patients who have been six months abstinent. Given the increasing incidence of alcohol-related hepatitis (AH) and dismal survival in patients who fail medical therapy, transplant centers are extending their acceptance criteria for patients with less than 6 months of sobriety. We sought to determine the barriers for listing.
Methods
We conducted a retrospective chart review of all inpatient LT referrals for a diagnosis of AH between September 2019 and December 2020. LT evaluations were performed by a multidisciplinary team. Descriptive statistics were reported using mean and standard deviation (SD) or percentage where appropriate.
Results
During our study period, 82 patients were evaluated for LT. Of these 82 patients, 62 were declined for liver transplantation. The mean (SD) age of the 62-patient cohort was 44 years (10.7), and most patients were men. The mean (SD) number of reasons for denial was 2 (0.97). Four patients had medical contraindications for transplant. Twenty-seven (44%) and 35 (56%) patients lacked insight and were at risk of alcohol relapse, respectively. Forty-three (69%) and fourteen (22.5%) patients had insufficient social support and an inability to maintain a therapeutic relationship with the transplant team, respectively.
Conclusion
Patients are more likely denied for psychosocial factors than medical comorbidities. The majority were due to lack of insight, insufficient social support, and inability to maintain a therapeutic relationship with the transplant team. Resources should be allocated to address these issues.
Keywords: liver transplant, alcohol hepatitis, patient outcome
Abbreviations: ALD, alcohol-related liver disease; AH, alcohol-related hepatitis; SD, standard deviation; INR, international normalized ratio; IQR, interquartile range
Liver transplantation is the life-saving therapy for many patients with end-stage liver disease. Its indications have evolved across the globe largely as a result of increasing alcohol consumption and the elimination of hepatitis C.1,2 Recent estimates indicate that the prevalence of any alcohol use in the last 12 months has risen from 65% to an alarming 72%.1 Though many patients with alcohol-related liver disease (ALD) remain minimally symptomatic, others rapidly progress to liver failure with limited treatment options.3 Today, ALD has emerged as the most common indication for liver transplantation with the increasing burden being driven by alcohol-related hepatitis (AH).4 Unlike patients with a diagnosis of alcohol-related cirrhosis, patients presenting with alcohol-related hepatitis tend to be significantly younger and have less medical comorbidities.
Liver transplantation for ALD has historically been reserved for patients who have been six months abstinent.5 The required period of abstinence served as an opportunity for liver function to improve and for patients to prove their potential to maintain sobriety after liver transplantation. This requirement has been based more on expert opinion than empirical data. However, given the recent recognition of the increasing incidence of AH, dismal survival in patients who failed medical therapy, and uncompromised post-transplant survival in select patients, many transplant centers are extending their transplant acceptance criteria to select patients who are sober for less than 6 months.6, 7, 8 Despite the interest in the utility of liver transplantation for AH, few evaluated patients are ultimately medically accepted for liver transplantation listing.9
Given the medical and public health implications of AH, and the seemingly low rate of acceptance for liver transplantation listing, we sought to determine the barriers for listing at our high volume tertiary care center. Prior studies suggested that medical comorbidities superceded addiction rehabilitation as the most common cause of LT denial.10 Few studies have been published delineating the reasons for denial specifically in patients with AH.7,11, 12, 13 Our hypothesis is that patients are more likely denied liver transplantation due to psychosocial factors than medical comorbidities.
Methods
Study Design
This single-center retrospective study examined inpatients referred for liver transplantation for a diagnosis of AH between September 2019 and December 2020. Beginning in September 2019, the criteria for liver transplantation evaluation was expanded at our center to include a diagnosis of AH. Prior to this date, our center denied transplant evaluation for patients with alcohol abstinence of less than six months. Alcohol hepatitis was defined as the onset of jaundice within 8 weeks of last alcohol use in patients with ongoing excessive alcohol consumption; AST >50 IU/L, AST:ALT ratio of >1.5 and both values <400 IU/L, and total bilirubin of >3.0 mg/dL.14 Liver biopsies were not performed in our cohort. This study was approved by the UCLA Institutional Review Board (#20-002295) and was performed in accordance with the declaration of Helsinki. Inclusion criteria in this study included patients over the age of 18, hospitalized, patients with a diagnosis of AH, and patients who completed the liver transplant evaluation.
Evaluation Process
The liver transplant evaluation process includes consultations by Hepatologists, Transplant Surgeons, Cardiologists, Pulmonologists, Transplant Coordinator nursing, Social Work, Psychiatrist, and Nutritionists. Specifically, the social work assessment included a review of housing, social support (our institution requires two caregivers), and patient and family therapeutic relationship with the transplant team. Psychiatric review is consistent with assessing patient insight of their liver disease and estimating the patient risk of alcohol relapse. The presence and severity of sarcopenia were estimated by nutritionists using the Nutrition-focused physical exam.15 Estimates of Karnofsky Performance Status scale were accomplished by the transplant coordinator.16 Hepatology assessed for severity of ALD, indication, and the likelihood of response to steroid therapy and quantifying amount of alcohol. There was redundancy in the history across all disciplines. Conflicts were resolved by consensus during a weekly Multidisciplinary Patient Selection Committee meeting where all specialties were personally represented.
Laboratory tests included but were not limited to complete blood count, comprehensive metabolic panel, prothrombin time/international normalized ratio (INR), viral and autoimmune serologies, and urine toxicology screens. Abdominal imaging was performed with abdominal computerized tomography and/or ultrasound.
Statistical Analysis
Descriptive statistics were reported using mean with standard deviation (SD), median with interquartile range (IQR), or percentage where appropriate.
Results
During the study period, a total of 199 out of 393 (50.6%) liver transplant referrals were made for alcoholic liver disease. Of the 199 patients, 82 patients had a diagnosis of alcoholic hepatitis, while the rest were referred for alcoholic cirrhosis. Twenty of the 82 patients were medically accepted for liver transplantation, and 62 were declined for liver transplantation. Patient demographics, socioeconomic background, and insurance type are listed in Table 1 for the 62 patients denied transplant. Briefly, the mean (SD) age of the cohort was 44 years (10.7), and most patients were male. Non-Hispanic and Hispanic whites accounted for most patients denied. Over a third of patients had some college education. Approximately half of the cohort had a household income of at least $75,000 a year.
Table 1.
Demographics of Patients Denied Liver Transplantation.
| Mean Age (standard deviation) | 44 (10.67) |
| Gender | |
| Male | 33 (53%) |
| Female | 29 (47%) |
| Race/Ethnicity | |
| Non-Hispanic White | 24 (39%) |
| Hispanic or Latino White | 26 (42%) |
| Non-Hispanic Asian | 5 (8%) |
| Non-Hispanic Black | 1 (1%) |
| Unknown/Other | 6 (10%) |
| Education | |
| No Degree | 4 (6.5%) |
| High School | 20 (32%) |
| Some College | 22 (35.5%) |
| 4 Years of College | 6 (10%) |
| Graduate school or Higher | 5 (8%) |
| Other | 1 (1.5%) |
| Unknown | 4 (6.5%) |
| Household Income | |
| Less than $25,000 | 0 (0%) |
| $25,000 to $34,999 | 0 (0%) |
| $35,000 to $49,999 | 5 (8%) |
| $50,000 to $74,999 | 26 (42%) |
| $75,000 to $99,999 | 20 (32%) |
| $100,000 to $149,999 | 6 (10%) |
| $150,000 or more | 5 (8%) |
| Insurance | |
| PPO | 20 (32%) |
| HMO | 27 (43%) |
| MediCaid | 15 (25%) |
Abbreviations: PPO ∼ Preferred Provider Organization, HMO ∼ Health Maintenance Organization.
Medical comorbidities were not common in our cohort. Thirteen patients had hypertension, five had diabetes, and no person had coronary artery disease. The mean BMI was 28.96 kg/m2 (7.6). The most common manifestation of hepatic decompensation other than jaundice was ascites (77%) and hepatic encephalopathy (74%). Fifty-five percent of patients had a history of variceal bleeding, and 24% were on hemodialysis at the time of evaluation. The mean (SD) Karnofsky score was 45.5 (10.0), and 29 patients were noted to have sarcopenia. Sarcopenia was noted to be mild, moderate, and severe in 72%, 24%, and 3% of the patients with sarcopenia, respectively.
The median duration of alcohol abstinence was 21.5 (IQR 6.25–48.25) days. Thirty-one percent of patients had a prior Driving Under the Influence citation, and 33% of patients had participated in an alcohol rehabilitation program. Current nonalcoholic substance use was uncommon (11%). The most common current substance use included a single or combination of cannabinoid, cocaine, and methamphetamine (Table 2). Laboratory values are shown in Table 3. The mean (SD) AST/ALT ratio was 2.82 (1.5), and the mean (SD) MELD-Na was 34.9 (6.1).
Table 2.
Alcohol and Other Substance Use of Patients Denied Liver Transplantation.
| <30 days | 27 (44%) |
| 30–90 days | 28 (45%) |
| >90 days | 7 (11%) |
| History of Driving Under the Influence | 19 (31%) |
| Rehabilitation programs (AA/NA) | 21 (35%) |
| Relapses | 35 (56%) |
| Tobacco use | |
| Current | 13 (21%) |
| Previous | 13 (21%) |
| No | 36 (58%) |
| Other substance used | |
| Current | 7 (11%) |
| Previous | 18 (29%) |
| No | 37 (60%) |
| Substance used | |
| THC/Marijuana | 0 |
| Cocaine | 1 |
| Meth | 3 |
| Meth/THC | 2 |
| Meth/THC/Cocaine | 1 |
Abbreviations: AA/NA ∼ Alcoholics Anonymous/Narcotics Anonymous, THC ∼ Tetrahydrocannobinol, Meth ∼ Methamphetamine.
Table 3.
Laboratory Data of Patients Denied Liver Transplantation.
| AST | 165.03 (178.32) IU/L |
| ALT | 67.31 (52.58) IU/L |
| AST/ALT | 2.82 (1.5) |
| Alk Phos | 164.22 (88.0) IU/L |
| Bilirubin, total | 24.20 (9.47) mg/dL |
| Platelet count | 122.90 (81.74) × 109/L |
| Albumin | 3.10 (0.59) g/dL |
| White blood cell | 19.26 (11.25) × 109/L |
| Hemoglobin | 8.97 (1.86) g/dL |
| INR | 2.50 (0.80) |
| MELD-Na | 34.85 (6.12) |
Abbreviations: AST ∼ aspartate transaminase, ALT ∼ alanine transaminase, Alk Phos ∼ alkaline phosphatase, INR ∼ international normalized ratio, MELD ∼ Model for End-Stage Liver Disease.
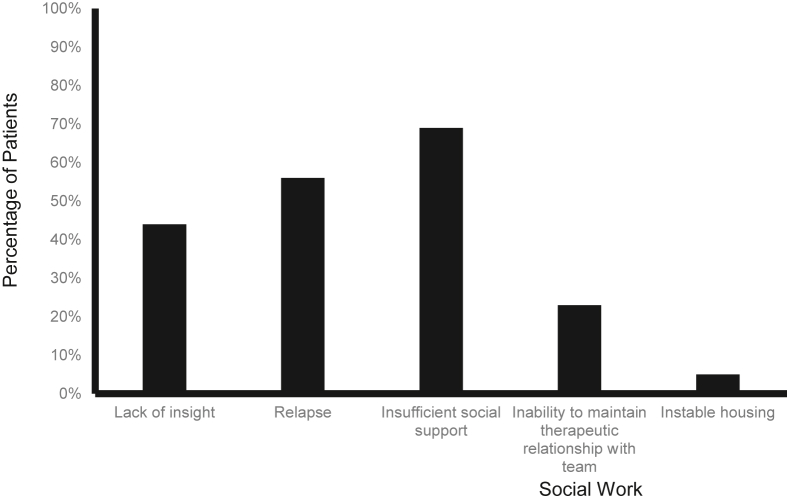
The mean (SD) time from referral to initiation of liver transplantation evaluation was one (2.1) day. The median time from evaluation to final committee decision regarding transplant status was 4 (IQR 2–7.75) days. The mean (SD) overall number of reasons for liver transplant denials was 2 (0.92). Four patients (6.5%) also had a medical contraindication to transplantation (pancreatitis [2], acute respiratory distress syndrome [1], and hepatocellular carcinoma tumor burden [1]) (Table 4). When assessing only the psychiatric and social work contraindications for transplantation, 22 (35.5%), 22 (35.5%), and 18 (29%) had one, two, or more than three reasons for denial, respectively. Specifically, 27 (44%) and 35 (56%) were noted to have a lack of insight and were at risk of alcohol relapse, respectively. Forty-three (69%), fourteen (22.5%), and three (5%) patients had insufficient social support, an inability to maintain a therapeutic relationship with the transplant team, and unstable housing, respectively (Figure 1).
Table 4.
Reasons for Denial of Patients Denied Liver Transplantation.
| Category | Number (%) |
|---|---|
| Medical | 4 (6.5%) |
| Pancreatitis | 2 |
| Acute respiratory distress syndrome | 1 |
| Hepatocellular Carcinoma tumor burden | 1 |
| Psychiatry | |
| Lack of insight | 27 (44%) |
| Relapse | 35 (56%) |
| Social Work | |
| Insufficient social support | 43 (69%) |
| Inability to maintain therapeutic relationship with team | 14 (22.5%) |
| Instable housing | 3 (5%) |
Figure 1.
Proportion of patients with social work and psychiatric reasons for liver transplant denial.
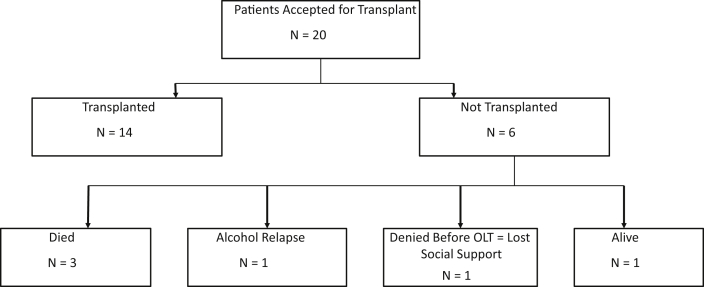
Twenty patients were ultimately accepted for liver transplant and fourteen of the twenty patients underwent transplantation, while six patients did not undergo transplantation. Among the six patients who were accepted but did not have transplantation, three died, one patient had alcohol relapse prior to liver transplant, and one patient lost secondary caregiver support and one patient remains alive without transplant (Figure 2).
Figure 2.
Outcome of patients accepted for liver transplant.
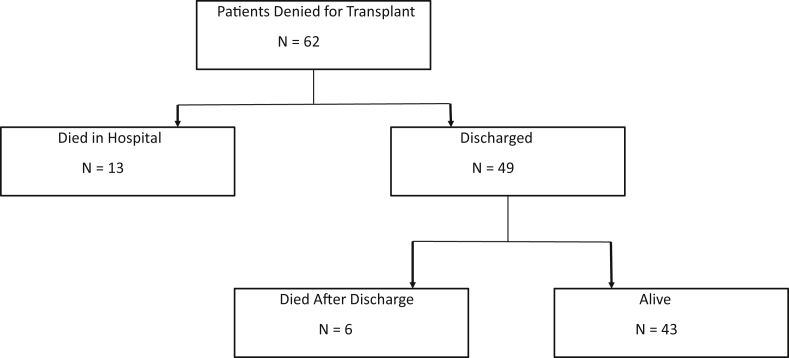
Sixty-two patients were denied liver transplant. Thirteen of the sixty-two patients died during their hospitalization (mean 16.85 (SD 12.8) days. Among 49 patients discharged, 6 died (83.8 [SD 43.17] days) and 43 remain alive (mean 113 [SD 160] days) (Figure 3). There was no recidivism among patients transplanted for this indication for recipients as of June 2021.
Figure 3.
Outcome of patients denied liver transplant. Among patients denied transplant, 13 died in hospital (mean 16.85 days [SD 12.8]). Among 49 patients discharged, 6 died (83.8 days [SD 43.17]) and 43 are alive (mean 113 days [SD 160]).
Discussion
Alcohol-associated liver disease is both complex and heterogeneous in its presentation and disease course. Transplant providers struggle to quantify an often subjective set of data, especially since psychosocial factors are difficult to ascertain and are dynamic in nature. From a strictly medical perspective, clinicians have developed models to help prognosticate the morbidity and mortality of patients with AH.17,18 However, these models often fall short and fail to accurately capture the individual patient’s course. Even the use of steroids is controversial and cannot be applied to all patients with AH.19 For patients who present with a high MELD score or acute renal failure, medical therapies are few and inadequately studied.20,21 These patients are thus referred for liver transplant evaluation at which point, transplant centers are faced with life and death decisions that are nuanced and difficult to measure. The well-ingrained six-month rule is under scrutiny as transplant centers push the boundaries to expand criteria and determine the patients who truly need and will succeed after transplant.9 Patient selection is key, and this has been well documented in the literature since 2011 when fewer than 2% of patients admitted for an episode of AH were selected and had improved survival with early liver transplant.7 However, the reasons for the denial are less studied. The transplant community has thus struggled with identifying and caring for these patients. This study shows that patients are more likely denied liver transplantation due to psychosocial factors rather than medical comorbidities.
A total of 62 out of 82 AH (76%) patients were denied liver transplantation. The mean age was 44, which supports recent data that alcohol liver disease now impacts people at a younger age.4 Fifty-three percent were male, and 47% were female, which is consistent with emerging data regarding the rising impact of alcohol on women.4 Over a third of patients had some college education and approximately half of the cohort had a household income of at least $75,000 per year, which underscores that ALD is not directly proportional to household income. Furthermore, 32% of patients had PPO (private) insurance, 43% had HMO (managed care that requires referrals and prefers providers within their managed care network) insurance, and 25% of patients had California Medic-aid (public insurance program that provides health coverage to low incomes families and individuals). It is possible there may be more flexibility with private insurance companies accepting patients for transplantation prior to six months of abstinence.
Medical comorbidities were not common in our cohort. This may be reflective of the younger mean age of 44. Indeed, the lack of medical comorbidities may argue for liver transplant denial as patients with fewer comorbidities have more physiologic reserve to combat systemic illness. However, 29 patients (47%) had sarcopenia ranging from mild to severe with mean Karnofsky scores of 45.5. Sarcopenia is a known predictor of poor outcomes and independently impacts mortality.22 In addition, 15 patients (24%) were in renal failure on hemodialysis. The mean MELD-Na was 35 emphasizing the acuity of these patients.
The median duration of self-reported alcohol abstinence was 21.5 (IQR 6.25–48.25) days. 44% of patients had less than 30 days of sobriety, and 45% of patients had 30–90 days of sobriety. Almost a third of patients (31%) had a history of driving under the influence, which indicates this was not their first presentation into the legal or health system for alcohol misuse and abuse. Nonetheless, 35% of patients had participated in an alcohol rehabilitation program in an attempt to seek help for their disease. It is difficult to determine if participation in an alcohol rehabilitation program portends to better or worse outcomes as it reflects a relapse (56% of the cohort reported a relapse) and self-recognition of an alcohol problem. Although alcohol use disorder is a disease with a high likelihood of slips and relapses, the medical community struggles with predicting relapse. Encouragingly, there was no recidivism among patients transplanted for this indication in our cohort in the short term, but they continue to be closely followed. However, prior studies have reported recidivism rate up to 20% rate in patients transplanted for a diagnosis of alcohol cirrhosis and 14% in those transplanted for severe alcoholic hepatitis.23,24 The pertinent question is how to determine whether slips or relapses will lead to allograft failure. Another substance abuse was documented. However, we were unable to determine if concurrent substance abuse predicted poorer outcomes.
In terms of denial, the majority were due to insufficient social support (23%) and lack of insight (44%) as defined by the patient’s ability to candidly discuss the influence of alcohol on their liver disease and their receptiveness to engage in substance use treatment. Twenty-three percent were unable to maintain a therapeutic relationship with the team. This therapeutic relationship was determined by the patient’s ability to develop and maintain a partnership with the transplant team in a way that helps ensure the integrity of their graft while working toward mutually shared clinical goals. Five percent had unstable housing. These psychosocial factors, or a combination of the above, led to the most denials. This highlights that ALD is truly two diseases, both alcohol use disorder and decompensated cirrhosis, that are intertwined and need to be addressed simultaneously.
There were several limitations to our study. Many of the patients initially presented and were admitted to outside institutions before transferring to our center. As a result, several days of discrepancy in laboratory values, used in determining the onset of alcoholic hepatitis, exist. In addition, there is limited data on whether steroids were used prior to transfer and if this may impact outcomes. However, the mean MELD in our cohort was 35, and according to the STOPAH trial where the mean MELD score was 21, steroids were unlikely implemented.25 Self-reported length of sobriety is only as accurate as patients want them to be and cannot be used as meaningful indicators of relapse risk assessment. Last, due to the possibility of some patients denied by the committee to be re-evaluated, our result may not reflect the final outcomes of AH patients. Another limitation is that all patients were recruited from a single center, and thus the results may not be generalizable to other transplant programs. Formalized psychosocial questionnaires were not employed to assess patients in the evaluation process. Nonetheless, all patients were evaluated by experienced transplant psychiatrists and social workers at a high-volume transplant center.
Few evaluated patients are ultimately accepted for LT for reasons not well articulated in the literature. This work has identified psychosocial factors as the most common cause of transplant listing denial among a cohort with limited medical therapies. Resources from health care systems, insurance companies, and government funding should be allocated to address these issues. Society should also acknowledge the inherent biases and prejudices associated with ALD2. Unfortunately, liver transplant evaluation is often the only intervention when it should be the final intervention after multiple attempts to mediate two chronic illnesses. However, this is the grim reality that patients and clinicians struggle with daily. A transplant denial should trigger an automatic referral to therapeutic programs to help patients with these issues.
Role in the study
Study concept and design (SS); acquisition of data (all); analysis and interpretation of data (all); drafting of the manuscript (X); critical revision of the manuscript for important intellectual content (GC, JNB, DGF, SS); statistical analysis (not applicable); obtained funding (not applicable); administrative, technical, or material support (GC, SS); study supervision (SS).
CREDIT AUTHORSHIP CONTRIBUTION STATEMENT
Gina Choi: acquisition of data, analysis and interpretation, critical revision, technical support. Jihane N. Benhammou: acquisition of data, analysis, and interpretation, critical revision. Jung J. Yum: acquisition of data, analysis, and interpretation. Elena G. Saab: acquisition of data, analysis, and interpretation. Ankur P. Patel: acquisition of data, analysis, and interpretation. Andrew J. Baird: acquisition of data, analysis, and interpretation. Stephanie Aguirre: acquisition of data, analysis, and interpretation. Douglas G. Farmer: acquisition of data, analysis, and interpretation, critical revision. Sammy Saab: acquisition of data, analysis, and interpretation, critical revision, administrative/technical/material support, drafting of the manuscript, and study supervision.
Conflicts of interest
The authors have none to declare.
Acknowledgments
We would like to thank the members of the Multidisciplinary Patient Selection Committee for their unwavering support.
Financial support
None.
References
- 1.Grant B.F., Chou S.P., Saha T.D., et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: results from the national epidemiologic survey on alcohol and related conditions. JAMA Psychiatr. 2017;74:911–923. doi: 10.1001/jamapsychiatry.2017.2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saab S., Challita Y., Chen P.H., et al. Elimination of hepatitis C in liver transplant recipients. J Clin Transl Hepatol. 2018;6:247–250. doi: 10.14218/JCTH.2017.00079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lucey M.R., Im G.Y., Mellinger J.L., et al. Introducing the 2019 American association for the study of liver diseases guidance on alcohol-associated liver disease. Liver Transplant. 2020;26:14–16. doi: 10.1002/lt.25600. [DOI] [PubMed] [Google Scholar]
- 4.Tapper E.B., Parikh N.D. Mortality due to cirrhosis and liver cancer in the United States, 1999-2016: observational study. BMJ. 2018;362:k2817. doi: 10.1136/bmj.k2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Everhart J.E., Beresford T.P. Liver transplantation for alcoholic liver disease: a survey of transplantation programs in the United States. Liver Transplant Surg. 1997;3:220–226. doi: 10.1002/lt.500030305. [DOI] [PubMed] [Google Scholar]
- 6.Lee B.P., Mehta N., Platt L., et al. Outcomes of early liver transplantation for patients with severe alcoholic hepatitis. Gastroenterology. 2018;155:422–430. doi: 10.1053/j.gastro.2018.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mathurin P., Moreno C., Samuel D., et al. Early liver transplantation for severe alcoholic hepatitis. N Engl J Med. 2011;365:1790–1800. doi: 10.1056/NEJMoa1105703. [DOI] [PubMed] [Google Scholar]
- 8.Lee B.P., Vittinghoff E., Dodge J.L., et al. National trends and long-term outcomes of liver transplant for alcohol-associated liver disease in the United States. JAMA Intern Med. 2019;179:340–348. doi: 10.1001/jamainternmed.2018.6536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Asrani S.K., Trotter J., Lake J., et al. The Dallas consensus conference on liver transplantation for alcohol associated hepatitis. Liver Transplant. 2020;26:127–140. doi: 10.1002/lt.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arya A., Hernandez-Alejandro R., Marotta P., Uhanova J., Chandok N. Recipient ineligibility after liver transplantation assessment: a single centre experience. Can J Surg. 2013;56:E39–E43. doi: 10.1503/cjs.004512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee B.P., Chen P.H., Haugen C., et al. Three-year results of a pilot program in early liver transplantation for severe alcoholic hepatitis. Ann Surg. 2017;265:20–29. doi: 10.1097/SLA.0000000000001831. [DOI] [PubMed] [Google Scholar]
- 12.Im G.Y., Kim-Schluger L., Shenoy A., et al. Early liver transplantation for severe alcoholic hepatitis in the United States–a single-center experience. Am J Transplant. 2016;16:841–849. doi: 10.1111/ajt.13586. [DOI] [PubMed] [Google Scholar]
- 13.Sundaram V., Wu T., Klein A.S., et al. Liver transplantation for severe alcoholic hepatitis: report of a single center pilot program. Transplant Proc. 2018;50:3527–3532. doi: 10.1016/j.transproceed.2018.08.057. [DOI] [PubMed] [Google Scholar]
- 14.Crabb D.W., Bataller R., Chalasani N.P., et al. Standard definitions and common data elements for clinical trials in patients with alcoholic hepatitis: recommendation from the NIAAA alcoholic hepatitis consortia. Gastroenterology. 2016;150:785–790. doi: 10.1053/j.gastro.2016.02.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.MacQuillan E., Ford J., Baird K. Increased competency of registered dietitian nutritionists in physical examination skills after simulation-based education in the United States. J Educ Eval Health Prof. 2020;17:40. doi: 10.3352/jeehp.2020.17.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dolgin N.H., Smith A.J., Harrington S.G., Movahedi B., Martins P.N.A., Bozorgzadeh A. Association between sarcopenia and functional status in liver transplant patients. Exp Clin Transplant. 2019;17:653–664. doi: 10.6002/ect.2018.0018. [DOI] [PubMed] [Google Scholar]
- 17.Hosseini N., Shor J., Szabo G. Alcoholic hepatitis: a review. Alcohol Alcohol. 2019;54:408–416. doi: 10.1093/alcalc/agz036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thursz M., Morgan T.R. Treatment of severe alcoholic hepatitis. Gastroenterology. 2016;150:1823–1834. doi: 10.1053/j.gastro.2016.02.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lieber S.R., Rice J.P., Lucey M.R., Bataller R. Controversies in clinical trials for alcoholic hepatitis. J Hepatol. 2018;68:586–592. doi: 10.1016/j.jhep.2017.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Phillips P.K., Lucey M.R. Acute alcoholic hepatitis: therapy. Clin Liver Dis. 2016;20:509–519. doi: 10.1016/j.cld.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 21.Singal A.K., Louvet A., Shah V.H., Kamath P.S. Grand rounds: alcoholic hepatitis. J Hepatol. 2018;69:534–543. doi: 10.1016/j.jhep.2018.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lai J.C., Dodge J.L., Sen S., et al. Functional decline in patients with cirrhosis awaiting liver transplantation: results from the functional assessment in liver transplantation (FrAILT) study. Hepatology. 2016;63:574–580. doi: 10.1002/hep.28316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hasanin M., Dubay D.A., Mcguire B.M., Schiano T., Singal A.K. Liver transplantation for alcoholic hepatitis: a survey of liver transplant centers. Liver Transplant. 2015;21:1449–1452. doi: 10.1002/lt.24208. [DOI] [PubMed] [Google Scholar]
- 24.Marot A., Dubois M., Trepo E., Moreno C., Deltenre P. Liver transplantation for alcoholic hepatitis: a systematic review with meta-analysis. PLoS One. 2018;13 doi: 10.1371/journal.pone.0190823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thursz M.R., Richardson P., Allison M., et al. Prednisolone or pentoxifylline for alcoholic hepatitis. N Engl J Med. 2015;372:1619–1628. doi: 10.1056/NEJMoa1412278. [DOI] [PubMed] [Google Scholar]