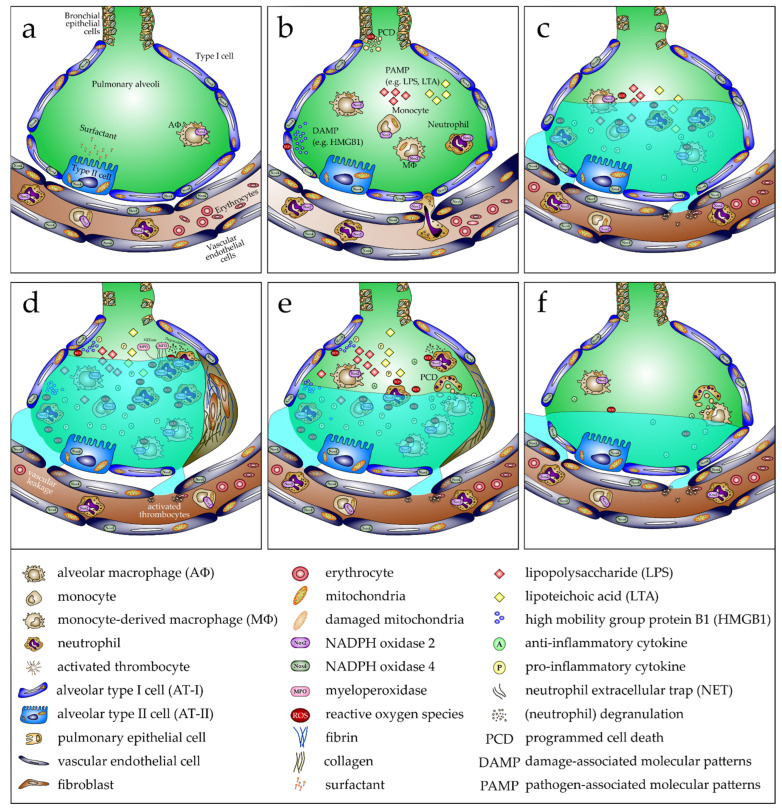
Figure 3.
Development, progression, and resolution of ARDS in response to pathogen-associated molecular patterns (PAMPs). (a) In the healthy lung, alveoli show no neutrophil infiltration and only limited alveolar macrophages (AΦ). Alveolar type II cells (AT-II) produce adequate surfactant to keep the alveolar epithelium covered effectively, thus reducing the surface tension, necessary to prevent a collapse of the alveoli after expiration. Consequently, optimal gas exchange occurs. (b) Following inhalation of bacteria or bacterial components such as lipopolysaccharide (LPS) or lipoteichoic acid (LTA), which are PAMPs, bronchial and alveolar epithelial cells are activated, increasing expression of proinflammatory chemokines and cytokines. This provokes infiltration of immune cells, mainly neutrophils and some monocytes, from the bloodstream. Consequently, the proinflammatory response is enhanced, including proinflammatory cytokines and mediators such as reactive oxygen species (ROS), produced primarily by the phagocytic NADPH oxidase (Nox2) expressed by neutrophils and monocytes/MΦ. Programmed cell death (PCD) of bronchial epithelial cells is induced and HMGB1 as a damage-associated molecular pattern (DAMP) from alveolar type I cells (AT-I) is released, which is also associated with cell demise. (c) Cell death is linked to the damage of the alveolar–capillary barrier, causing lung edema, which significantly reduces lung function with reduced blood gas exchange. (d) High numbers of neutrophils and MΦ in the alveoli, a consequence of cell death and a proinflammatory environment, facilitate proliferation of fibroblasts, expressing fibronectin and collagen. These contribute to fibrosis and reduce the normal function of the alveoli. (e) Reduction of the proinflammatory profile emphasizes an anti-inflammatory response and fibrosis is reversed. Proliferation of alveolar and bronchial cells closes the gap, which arises due to prior cell death. Therefore, lung edema abates. Finally, (f) fibrosis completely reverses, and the cell composition of alveoli is almost completely restored. When edema is also entirely resolved, lung function is reestablished.