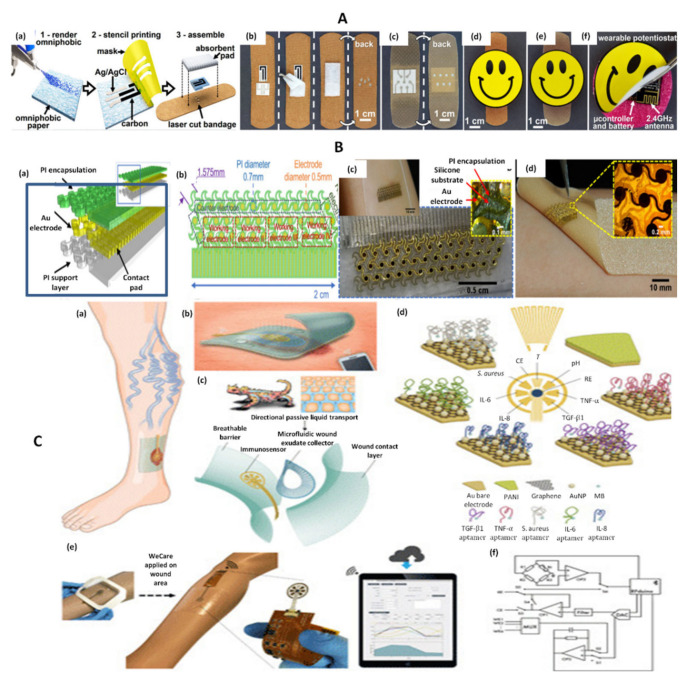
Figure 3.
(A) Fabrication protocol for omniphobic paper smart bandage (OPSB) fabrication and assembly process. (a) Schematic diagram of the fabrication of OPSBs with: (1) Whatman#1 paper rendered omniphobic by spraying a 2% solution of RF SiCl3 in isopropyl alcohol; (2) stencil printing is used to pattern flexible conductive electrodes using carbon and Ag/AgCl inks; (3) openings are laser cut on the adhesive layer of the bandage to interface the wearable potentiostat with the paper-based sensors in the OPSB. OPSBs are assembled by placing the paper-based sensors between the adhesive layer and the absorbent pad of the commercial bandages. (b) OPSBs used to monitor UA and pH levels in open wounds. (c) OPSBs used for the early detection of pressure ulcers. (d,e) Interfacing of the wearable potentiostat with OSPBs for monitoring open wounds and detecting 12 pressure ulcers, respectively. (f) Packaging of the electronics in the rechargeable, wearable Potentiostat Reprinted (adapted) with permission from Reference [36] Copyright 2021 Elsevier. (B) Skin-inspired gold electrodes (a); schematic diagram of the flexible device (b); schematic diagram with dimensions (c); image of the sensor on polymeric wound dressing (Walgreens—Silicone Scar Sheets) (d); image of the sensor on a textile-silicon bandage (ScarAway—Silicone Scar Sheets) Reprinted (adapted) with permission from Reference [38]. Copyright 2021 Elsevier. (C) Schematic representation of a multiplexed immunosensing system for chronic wound monitoring. (a) Illustration of a biomarker analytical dressing applied onto an open wound of patients with venous ulcer for in situ surveillance. (b) Illustration of a thin, soft, biomarker analytical dressing (VeCare) that allows normal skin function allowing the penetration of oxygen inside but also the evacuation of moisture vapor outside. Data was wirelessly transmitted to a mobile system over Bluetooth Low Energy. (c) Envisioned biomarker analytical dressing constituting of a perforated wound contact layer, a microfluidic wound exudate collector, an immunosensor, and a breathable barrier. The microfluidic collector was inspired by the skin of Texas horned lizard enabling predetermined flow direction toward the lizard’s snout defying gravity. (d) Schematic representation of the sensors applied for the detection of TNF-α, IL-6, IL-8, TGF-β1, S. aureus, pH, and temperature. PANI = polyaniline; MB = methylene blue; RE = reference electrode; CE = counter electrode. (e) VeCare prototype for envisioned chronic wound monitoring. The prototype was applied to a leg dummy as a demonstration. The immunosensor interfacing with a wireless portable analyzer fabricated on a flexible printed circuit board. A mobile application providing a graphical user interfaceas a one-stop patient’s profiles, medical records, data recording, data analysis, and result visualization system is shown. (f) Hardware block diagram for the VeCare platform. WE1 = working electrode 1; MUX = multiplexer Adapted from Reference [27] (Open Access).