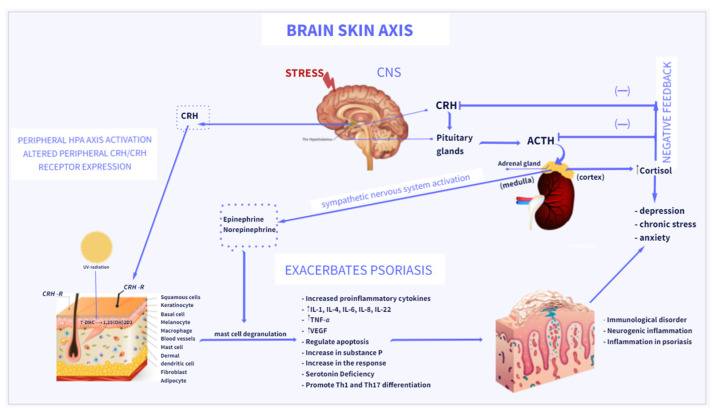
Figure 1.
Brain–skin axis: association between psoriasis and depression. Stress acts via several pathways to exacerbate psoriasis, via the central and peripheral HPA axes, regulation of cytokine production, and activation of the sympathetic nervous system. The final messengers of the sympathetic nervous system and HPA, norepinephrine and cortisol, can directly engage in regulation of various immune cells to modulate immune responses. Direct action of CRH induces inflammatory responses in psoriasis. CRH and CRH-related peptides can be produced by several cells in the skin and stimulate the local production of cytokines in the skin. By binding to CRH-R on mast cells, CRH induces mast cell degranulation and releases proinflammatory factors, which induces further inflammation in psoriasis. The increase in cortisol levels causes the exacerbation of psoriasis and the activation of Th-17 cells, which leads to an increase in the levels of pro-inflammatory cytokines IL-17, TNF-α contributing to the development and intensification of depressive disorders. Vitamin D3 (Vit D3) is synthesized in the skin from its precursor 7-DHC under the influence of UVB and metabolized to its active form, 1,25(OH)2D3.