Abstract
This systematic review examined the effectiveness in a hybrid telehealth model for adolescents with autism spectrum disorder (ASD), exploring the evidence base, methodology, and outcomes of health and behavior-related interventions for adolescents with ASD. The 11 included studies (a) were quantitative, (b) evaluated interventions delivered through a hybrid telehealth model (i.e., combined remote intervention with minimal in-person procedures), (c) measured health and behavior-related outcomes, and (d) considered adolescence as ages 12 through 25 years. The studies were a mixture of designs, methods, and outcome measures, and participant numbers were extremely low. Results demonstrated an overall lack of empirical evidence on the efficacy of hybrid-delivered interventions for adolescents with ASD, and more studies are needed to explore their effectiveness.
Keywords: Adolescence, Autism spectrum disorder, Hybrid, Intervention
An increasing number of individuals with autism spectrum disorders (ASD) are entering adolescence and require interventions to address health and behavior-related outcomes. Given the increase in telehealth-delivered interventions due to the COVID-19 pandemic, practitioners need to understand the evidence of hybrid telehealth-delivered (i.e., combination of in-person and remote) interventions for adolescents with ASD. Although interventions often promote activities of daily living, social participation, academic and work skills, and well-being (Tomchek & Koenig, 2016), it is unclear whether those delivered in a hybrid telehealth approach are rooted in evidence. Therefore, the purpose of this systematic review was to identify and evaluate studies related to interventions delivered through a hybrid telehealth model for adolescents with ASD.
Telehealth refers to the use of information and communication technologies to deliver health care and behavioral services by professionals (World Health Organization [WHO], 2010). Telehealth services are rendered using real-time or store-and-forward techniques (Bradford et al., 2016), and may include video- and audioconferencing, chat messaging, wearable and sensor technologies, virtual reality, robotics, and therapeutic gaming (Rispoli & Machalicek, 2020). There was a rapid increase of telehealth during the COVID-19 pandemic, which precluded in-person contact due to social distancing and quarantine demands. As of today, the COVID-19 pandemic is still present, and telehealth remains an available and active service-delivery model. Practitioners, families, and service-delivery systems are grappling with which intervention elements are most efficaciously delivered in-person versus remotely. For example, given the emerging nature of reliability and validity of remote assessment procedures (see Ellison et al., 2021), researchers may administer diagnostic and language assessments in-person and then deliver intervention components remotely. In this review, hybrid telehealth interventions are considered those that include both in-person and remote components; remote components may occur synchronously or asynchronously. An examination of the evidence related to hybrid telehealth interventions is vital to inform future research of which elements of interventions for adolescents with ASD may be efficaciously delivered and through which mechanism (in-person vs. remote).
In the next 10 years, an estimated 707,000 to 1,116,000 teens (70,700 to 111,600 each year) in USA will enter adulthood and age out of school-based autism services (Autism Speaks, 2021). Adolescence is a period of psychosocial, cognitive, physical, and sexual maturation characterized as an advancement towards social and economic independence (Curtis, 2015; Meeus, 2016; Sawyer et al., 2018;WHO, 2007). The WHO (2013) initially defined adolescents as individuals between 10 and 19 years of age; however, an expanded and more inclusive definition—that of individuals from 10 through 25 years old—aligned with contemporary patterns of adolescent growth (Sawyer et al., 2018).
The adolescence period can be particularly challenging among youth with ASD, who struggle with difficulties in identity-development processes, adaptive behaviors, transition to independent living, and development of autonomous behaviors (Cooper et al., 2017; Hume et al., 2014; Seltzer et al., 2003; Smith & Anderson, 2014). Compared to the general population, adolescents with ASD are more likely to have cooccurring mental health conditions and are less likely to manage activities of daily living or prepare for college or employment (e.g., Roux, 2015). The COVID-19 pandemic has had an unprecedented effect on life around the world. The closure of schools, clinics, and community programs puts individuals with ASD at increased risk for negative outcomes. Thus, the delivery of services and therapies in an online or remote format may partially ameliorate the impact of secondary effects of COVID-19 on adolescents with ASD (White et al., 2021).
A growing body of research has evaluated the effectiveness and benefits of telehealth to deliver services to individuals with ASD (Ellison et al., 2021; Rodriguez, 2020). Studies have tested a variety of interventions, such as teaching functional communication skills (Simacek et al., 2017) and treating challenging behaviors (Lindgren et al., 2016). Others explored opportunities for these interventions to support children and adolescents in their daily lives, notably in school settings (Mazon et al., 2019; Tomchek & Koenig, 2016). Telehealth has been shown to be cost-effective (Little et al., 2018) and to address provider shortages (Baweja et al., 2021; Shulver et al., 2016). Parents of children with ASD report high acceptability, satisfaction (Little et al., 2018), convenience, and feelings of empowerment (Wallisch et al., 2019) with telehealth.
Several literature reviews published about the use of technology in interventions with children and adolescents with ASD (e.g., Grynszpan et al., 2014; Odom et al., 2015; Sutherland et al., 2019) indicated that interventions largely target preschool- or school-aged children with ASD (Mazon et al., 2019). There is, however, a paucity of intervention studies on the use of hybrid telehealth interventions among adolescents with ASD (Odom et al., 2015). Additionally, hybrid telehealth-intervention studies are limited by small sample sizes, use of nonstandardized measures, and the absence of comparative control groups (Mazon et al., 2019). Yet, outcomes of various services via telehealth (including diagnostic assessments, preference assessments, early interventions, applied behavior analysis, functional assessment, functional communication training, and parent training) were found to be equivalent to or better than face-to-face services (Ellison et al., 2021).
In sum, adolescents with ASD have considerable need for intervention, especially towards the end of compulsory education and during their transition to adulthood (Odom et al., 2015). Hybrid interventions provide an innovative way to offer cost-effective and client-centered interventions from a distance. Due to the imminent and ongoing impact of the COVID-19 pandemic and increasingly expansive improvements in telehealth platforms and technology, there is a need to review the literature on the use and efficacy of hybrid services for adolescents with ASD. Therefore, the purpose of this systematic review was to evaluate existing empirical studies of hybrid interventions for individuals with ASD aged 12 through 25 years.
Method
The preferred reporting items of systematic reviews and meta-analyses (PRISMA; Moher et al., 2009) document was used to guide this systematic review. The review was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database (http://www.crd.york.ac.uk/prospero). Table 1 shows the search terms used. The databases to conduct searches were MEDLINE, PubMed, CINAHL, PsycINFO, Web of Science, Cochrane Library, ERIC, Scopus, and EBSCO Discovery Service. All titles and abstracts were imported into Covidence systematic review software (Veritas Health Innovation, n.d.), which was used for screening.
Table 1.
Search term strategy
| Field | Terms (all fields) |
|---|---|
| 1 | ASD, autistic, autism, autistic disorder, autism spectrum disorder, Asperger, pervasive developmental disorder |
| 2 | adolescents, youth, teens, teenagers, youngsters, young people, young adults, emerging adults, young adulthood, secondary school, middle school, high school |
| 3 | hybrid, remote, telehealth, telemedicine, telerehabilitation, tele-practice, telecare, tele-exercise, teleconference, e-health, mobile health, m-health, web-based, internet-based, digital health, tele education, telemonitoring, telecommunications, teleconsultation, telepsychiatry |
Inclusion Criteria
Only quantitative studies that empirically evaluated interventions delivered in a hybrid approach (i.e., that included some in-person time, but the main intervention occurred remotely) were included. The interventions could address any adolescent outcome (e.g., health, education, or work). A study was included only if at least 30% of that study’s participants were described as diagnosed with ASD (DSM-V; American Psychiatric Association [APA], 2013) or one of the autistic spectrum diagnoses according to the DSM-IV-R (e.g., autism, Asperger syndrome, and pervasive developmental disorders; APA, 1994) and age 12 through 25 years (Jaworska & MacQueen, 2015; Steinberg, 2014; WHO, 2020). However, studies about females with Rett Syndrome were excluded. All studies must have been available in English and peer reviewed, without limit to year of publication.
Exclusion Criteria
Reviews, meta-analyses, dissertations, study protocols, and conference proceedings were excluded. In addition, assessment studies that investigated telehealth delivery of diagnostic measures and studies whose outcomes were not focused on adolescents (e.g., parent or teacher measures) were excluded. Studies examining interventions that only integrated technology into sessions conducted in person or in the same space (e.g., videomodeling studies) were also excluded, as were feasibility studies without any examined intervention.
Study Selection
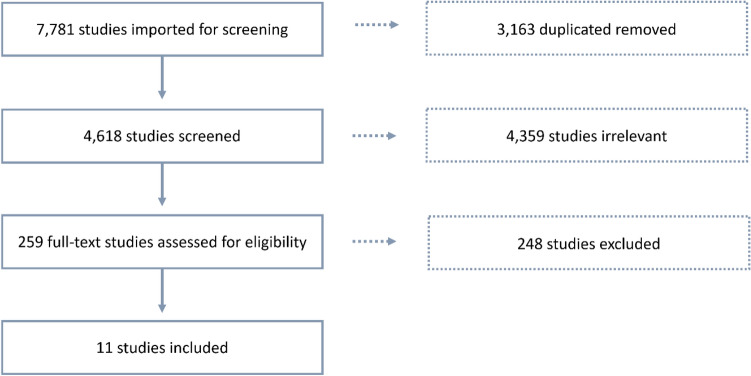
Following the Cochrane guidance (Higgins et al., 2011), two reviewers independently assessed the titles and abstracts to select articles for further assessment based on the inclusion criteria. In this phase, duplicates were removed. When there was a doubt about an article, a third reviewer provided another opinion. Next, the three reviewers reviewed and decided about including full texts according to the inclusion criteria (N = 259). In cases of disagreement, the final decision was made through discussion. This method reduced the chance of error and ensured proper conduct (Tawfik et al., 2019). Figure 1 illustrates the review process and reduction of studies to the 11 studies ultimately included in the review.
Fig. 1.
PRISMA summary of the screening process
Results
Descriptive Information of Study Characteristics
The preliminary search phase yielded 7781 articles; 3163 duplicates articles were deleted. The full-text review phase comprised 259 articles. Examination of the full-text articles yielded a total of 11 studies that met all inclusion criteria and were subsequently analyzed. All included studies had been published between 2012 and 2021.
Evaluation of the Risk of Bias in the Included Studies
To conclude whether the data and results from the included studies were valid, it was essential to evaluate the risk of bias. Therefore, as in similar works (e.g., Benevides et al., 2020), the risk-of-bias criteria proposed by the Cochrane group (Clarke & Oxman, 2002; Higgins et al., 2011) was used. Regarding design, six studies included a control group (Hatfield et al., 2017; Hayes et al., 2015; Hepburn et al., 2016; Sehlin et al., 2020; Strickland et al., 2013; Tang et al., 2021); in four of those studies, the division into groups was random. Two studies were pretest–posttest single-group designs (Backman et al., 2018; Wentz et al., 2012). Three studies used a single-subject design that include a multiple-baseline design as a control, which was considered to have a low risk of bias (Bross et al., 2020; Ford et al., 2020; Joseph et al., 2021). No study used blinding of participants and personnel, but three studies blinded the outcome assessors. All 11 included studies appeared to complete the outcome data and provide full-results reporting. Table 2 summarizes the risk-of-bias assessment.
Table 2.
Summarized risk of bias in all reviewed studies (N = 11)
| Author(s) (Year) | Study design | Controla | Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessors | Incomplete outcome data (attrition) | Selective reporting |
|---|---|---|---|---|---|---|---|---|
| Backman et al. (2018) | Mixed-methods + pretest–post-test single group | – | – | – | – | – | + | + |
| Bross et al. (2020) | Multiple baseline (MBL) single design | + | – | – | – | – | + | + |
| Ford et al. (2020) | Nonconcurrent MBL across participants design | + | – | – | – | – | + | + |
| Hatfield et al. (2017) | Quasi-randomized controlled trial | + | + | – | – | – | + | + |
| Hayes et al. (2015) | Mixed-methods with two group | + | + | + | – | – | + | + |
| Hepburn et al. (2016) | Pretest–posttest with equivalent control group | + | – | + | – | + | + | + |
| Joseph et al. (2021) | Single-subject MBL design | + | – | – | – | ? | + | + |
| Sehlin et al. (2020) | Nonrandomized control study | + | – | – | – | – | + | + |
| Strickland et al. (2013) | Pretest–posttest with control group | + | + | + | – | + | + | + |
| Tang et al. (2021) | Mixed-methods with control group | + | + | + | – | + | + | + |
| Wentz et al. (2012) | Pretest–posttest with follow-up in single group | – | – | – | – | – | + | + |
+ = Low risk of bias; –= High risk of bias; ? = Unclear risk of bias
aA comparison group that was equivalent to the intervention group upon pre-testing was assessed as a low risk of bias. For single-subject designs, we marked low risk of bias for use of a stable baseline and a stable withdrawal phase
Summary of Key Features of Included Studies
Table 3 summarizes the key features of the reviewed 11 studies, including the author(s); country in which the study was conducted; descriptions of participants, examined interventions, and controls; desired outcomes; outcome measures (dependent variables only), and technologies (hardware and software) used.
Table 3.
Summary of included studies (N = 11)
| Author (year) | Country | ASD participants | Desired intervention outcome | Examined intervention | Control group intervention | Outcome measure (dependent variable) | Technology type (hardware/software) |
|---|---|---|---|---|---|---|---|
| Backman et al. (2018) | Sweden | N = 28; age 16–25 years | Knowledge of ASD | Spectrum COmputerized PsychoEducation (SCOPE), an Internet-delivered, coach-guided psychoeducational intervention comprising eight ASD-themed modules aimed to provide information about typical and specific ASD impairments and associated strengths. Weekly contact with an experienced clinician using a message function within the web-based platform involved feedback on comments or questions the participants asked | NA |
•Treatment Credibility Scale (Borkovec & Nau, 1972) •ASD Quiz, modified from a corresponding knowledge quiz (Bramham et al., 2009; Hirvikoski et al., 2011) |
Hardware: Not detailed; described as computer-based intervention Software: Swedish national platform for Internet-delivered treatments (mostly for messages); SCOPE, an Internet-delivered intervention |
| Bross et al. (2020) | US | N = 8; age 17–26 years | Planning skills, participation in social activities | Four online instructional modules: planning activities, using a personal calendar, self-monitoring, developing routines. Includes 6 weeks of in-person small-group primary intervention, with telecoaching sessions twice a week; 6 weeks of telecoaching fading (once a week or every other week); and 2 weeks of maintenance (concluding telecoaching sessions) | Participants were divided into three groups; each group received the intervention according to their assigned cohort |
•Planning vignettes. Participant scores on planning vignettes modeled after the story-based items in the self-regulation domain of the ARC’s Self Determination Guide (Wehmeyer, 1995) •Social activity sample. Self-reported number of weekly social activities in which participants participated |
Hardware: Any available device with webcam and headset or built-in microphones Software: Modules included slideshows and video; telecoaching using videoconference apps, software, or platforms |
| Ford et al. (2020) | US | N = 3, age 25, 29, 30 years | Perform daily living skills | Remote intervention conducted using videoconference to promote daily living skills. All sessions were implemented remotely, 1–2 times/week for 15–60 min each. Participants completed the treatment phases for all target behaviors after a total of 107, 28, and 22 intervention sessions over 54, 14, and 22 weeks. Task analysis and shaping strategies were used to assist each participant acquisition of the target behavior | NA |
•Dependent measures varied slightly according to each participant’s target behaviors •Self-reported satisfaction survey •Individualized questionnaire examined confidence level regarding targeted daily living skill |
Hardware: Any available device with webcam and headset or built-in microphones Software: Free videoconferencing programs (Skype and FaceTime) |
| Hatfield et al. (2017) | Australia | N = 94; age 12–18 years; intervention group n = 49, control group n = 45 | Transition program: self-determination, quality of life, access to environmental supports, career planning, exploration |
The Better OutcOmes & Successful Transitions for Autism (BOOST-A™), an online program to support adolescents on the autism spectrum with transition from high school. Based on the self-determination model, a strengths-based approach, and a technology-based approach, BOOST-A™ consists of four modules delivered via a website accessed by individual logins. The first and second modules a completed at home with the parent and the adolescent; the third module completed with team members in person; the fourth module completed at in-person meetings with the team |
Regular practice at their respective schools, which may have included any generic transition-planning processes used at the school but no structured or disability-specific transition-planning program |
•The American Institutes for Research (AIR) Self-Determination Scale •Career Development Inventory, Australia (short form) •Personal Wellbeing Index, School Children •Learning Climate Questionnaire •Transition Planning Objectives Scale, designed to evaluate identified transition-planning objectives |
Hardware: Any available device with webcam and headset or built-in microphones Software: BOOST-A™ online program |
| Hayes et al. (2015) | US | N = 15, age 17–18 years | Vocational skills of employment interviews | VidCoach, a customizable mobile video-modeling and -prompting application to help students with ASD learn interview skills. Participants could use VidCoach at any other time desired. All participants completed two mock job interviews and a research interview. Treatment group received VidCoach to use for 1 month. On a second visit 1 month later, they again completed two mock job interviews and a research interview | No intervention available between the two mock interviews | •Mock employment interview scoring according to rubric developed over the research course |
Hardware: Mobile device with iOS Software: VidCoach software for video-modeling and -prompting |
| Hepburn et al. (2016) | US | N = 33 (and their parents), age 7–19 years with anxiety; intervention group n = 17, wait-list control group n = 16 | Reduce anxiety | Telehealth Facing Your Fears, online version of cognitive–behavioral-supported intervention targeting anxiety in youth with ASD in 12 sessions of 1.5 h each across a 3–4 months. The first six sessions focus on psychoeducational aspects of anxiety; second six on reducing interference of anxiety and supporting the youth’s ability to cope with small amounts of physiological and cognitive distress | Entered a waitlist |
•Anxiety and Related Emotional Disorders in Children (Birmaher et al., 1999) •Parenting Sense of Competence Scale (Johnston & Mash, 1989) |
Hardware: Any available device with webcam and headset or built-in microphones Software: OoVoo videoconferencing platform |
| Joseph et al. (2021) | US | N = 2 (with ASD, of the 3 participants); age 20, 24 years | Increasing on-topic small-talk exchanges in social-conversations | Remote audio coaching to teach skills of engaging in small talk or simple social conversational exchanges. Coach suggested a specific topic for the student to talk about. Identical to baseline, the confederate had been instructed previously not to initiate a conversation but always to engage the student after every conversation the student initiated | NA | •Participants’ on-topic small-talk coding, prompted on-topic exchanges, unprompted on-topic exchanges, off-topic exchanges, and confederate initiations), developed for the research |
Hardware: Personal laptop or computer; mobile device if technical issues Software: Professional Zoom account |
| Sehlin et al. (2020) | Sweden | Intervention group n = 24; age 15–32 years (M = 21); control group n = 20 matched participants | Increased self-esteem, sense of coherence, subjective quality of life; reduced anxiety, depressive symptoms | Internet-based support and coaching intervention (IBSC) providing individualized psychoeducation about ADHD and/or ASD and support regarding aspects of daily life. Two weekly chat sessions (30–60 min each) and two complementary clinic visits with coaches over 8 weeks. Short communication also possible through an email function | Any typically occurring treatment |
•Manchester Short Assessment for Quality of Life (MANSA; Priebe et al., 1999) •Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, 1983) •Sense of Coherence scale (SOC-29; Antonovsky, 1979) •Self-Esteem Scale (RSES; Rosenberg, 1989) •Global Assessment of Functioning Scale (American Psychiatric Association, 1994) |
Hardware: Computer with Internet connection Software: Any chat program |
| Strickland et al. (2013) | US | N = 22; age 16–19 years | Employment interviews; improve presence and degree of AS symptoms | Four-weeks intervention, using JobTIPS program, an Internet-accessed employment-training program. Included theory-of-mind-based guidance, video models, visual supports, virtual reality practice sessions to teach appropriate job interview skills | No training intervention |
•Interview skills rating instrument developed for the research •Social Responsiveness Scale (SRS; Constantino & Gruber, 2005) |
Hardware: Computer with Internet connection Software: JobTIPS interviewing program; virtual world practice session conducted via the Venugen platform |
| Tang et al. (2021) | Australia | Intervention group n = 11; control group n = 14; about 60% had ASD; mean age = 22 years | Social-emotional understanding | MindChip™ (MC), telehealth facilitator-mediated social-emotional program delivered with a computer-based intervention (Mind Reading©; MR). Intervention ran 10 weeks, 1 h/week, combined with Mind Reading Toolbox (MC + MR) | Mind Reading© program only |
•Emotion-recognition skills assessment (derived from the Mind Reading Emotion Library; Baron-Cohen et al., 2004) •Movie for the Assessment of Social Cognition (Bölte et al., 2014; Dziobek et al., 2006) •Emotion Recognition Self-Efficacy Scale (adapted from Lorig et al., 1996) •Social Responsiveness Scale (SRS-2; Constantino & Gruber, 2012) •Depression, Anxiety & Stress Scales (Lovibond & Lovibond, 1995) •Social Anxiety Scale (Liebowitz, 1987) |
Hardware: Computer with Internet connection Software: MindChip™ (Tang et al., 2018); Mind Reading© (Baron-Cohen et al., 2004); Zoom video communication |
| Wentz et al. (2012) | Sweden | N = 10 (with ASD and/or ADHD); age 15–26 years | Increased sense of coherence, self-esteem, subjective quality of life; reduced anxiety, depressive symptoms | An Internet-based support and coaching model for young people with ASD (IBSC). Included two face-to-face meetings and 8 weeks of biweekly 30–60 min support and coaching (chat sessions). Between chat sessions, participants could contact using e-mail | NA |
•Manchester Short Assessment of Quality of Life (MANSA; Priebe et al., 1999) •Hospital Anxiety and •Depression Scale (ADS; Zigmond & Snaith, 1983) •Sense of Coherence questionnaire (SOC-29; Antonovsky, 1979) •Rosenberg self-esteem scale (RSES; Rosenberg, 1989) •Patient perspective On Care and Rehabilitation process (Krevers & Oberg, 2002) |
Hardware: Computer with Internet connection Software: Chat and instant messaging (e-mail) |
Countries
Because hybrid telehealth interventions might be influenced by geographical environments, the country in which each study was conducted was examined. Most (six) studies were conducted in the United States, three in Sweden, and two in Australia.
Participants
Among the 11 studies, a total of 190 participants were enrolled in intervention groups and 95 in control groups. Most participants were between the ages of 12 through 25 years, as defined in the inclusion criteria. However, in studies that included younger or older participants, the mean age fell within the defined age range (i.e., Hepburn et al., 2016; Sehlin et al., 2020).
Intervention Goals
The intervention goals of the hybrid telehealth programs were reviewed. Some interventions focused on one area; others aimed to promote multiple areas. Most hybrid-intervention goals focused on reducing core ASD symptoms or cooccurring mental health conditions (Hepburn et al., 2016; Sehlin et al., 2020; Tang et al., 2021; Wentz et al., 2012) or promoting identity-related subjects, such as self-determination, self-esteem, sense of coherence, and knowledge of ASD (Backman et al., 2018; Hatfield et al., 2017; Sehlin et al., 2020; Wentz et al., 2012). Some intervention outcomes aimed at increasing quality of life (Hatfield et al., 2017; Sehlin et al., 2020; Wentz et al., 2012). Others focused on promoting social skills (Bross et al., 2020; Joseph et al., 2021; Tang et al., 2021) or acquiring or promoting employment/job skills (Hatfield et al., 2017; Hayes et al., 2015; Strickland et al., 2013). Only one study’s outcome measure focused on the promotion of daily living skills (Ford et al., 2020). Many studies included outcomes that spanned intervention goals (e.g., knowledge of ASD, as well as quality of life).
Intervention Outcome Measures
Analysis of intervention outcome measures showed that four studies did not include validated tools but used only tools developed specifically for the study (Bross et al., 2020; Ford et al., 2020; Hayes et al., 2015; Joseph et al., 2021). Another three studies combined validated tools and new tools developed for study purposes (Backman et al., 2018; Hatfield et al., 2017; Strickland et al., 2013). The last four used only validated and standardized tools to measure intervention outcomes (Hepburn et al., 2016; Sehlin et al., 2020; Tang et al., 2021; Wentz et al., 2012).
Intervention Efficacy Results by Goal Area
From the articles included in this review, it appeared that a variety of goals were set for promotion among adolescents with ASD, and some studies included multiple goals. As detailed in the following paragraphs, five studies addressed symptoms, four each addressed identity and social skills; three each for quality of life and employment skills, and one for daily living skills.
Symptoms of ASD and Cooccurring Mental Health Conditions
Only one of the four studies that addressed this category indicated the hybrid intervention efficacy as a reduction in ASD symptoms, anxiety, or depression symptoms (Hepburn et al., 2016). The remaining four studies presented partial results, insignificant trends, or no changes.
Identity-Related Subjects
Of the four studies aimed to promote participants' identity-related subjects (such as self-determination), three presented significant improvement in outcome measures following a hybrid intervention (Backman et al., 2018; Sehlin et al., 2020; Wentz et al., 2012).
Quality of Life
Only one of the three related studies presented a significant increase in quality of life following a hybrid intervention (Wentz et al., 2012). The remaining two studies presented partial results, insignificant trends, or no changes.
Social Skills
Inconsistent results for the efficacy of hybrid interventions in promoting social skills were found: Two of the three studies presented significant improvement among participants following the intervention (Joseph et al., 2021; Tang et al., 2021).
Employment and Job Interview Skills
All the three studies that aimed to promote job-interview skills reported a significant improvement in the intervention groups (Hatfield et al., 2017; Hayes et al., 2015; Strickland et al., 2013).
Daily Living Skills
The only study aimed to promote daily living skills also showed a significant improvement in the outcome measures (Ford et al., 2020).
Table 4 presents a summary of the interventions’ durations, goal areas, significant efficacy results, and technology evaluations, summarized according to outcome measures.
Table 4.
Summary of interventions’ duration, goal area, efficacy and technology evaluation
| Study | Duration range of intervention | Goal area | Intervention main efficacy finding | Evaluation of technology | Efficacy resultsa |
|---|---|---|---|---|---|
| Backman et al. (2018) | Eight ASD-themed modules, each worked on for 1 week | Identity-related issues | Participants reported significantly increased knowledge about ASD from pre- to postintervention; symptoms of anxiety, depression, and acceptance of diagnosis did not significantly change | An open feasibility study evaluated the internet-delivered intervention; 79% of participants completed the intervention. Participants’ experience of treatment credibility increased during the SCOPE web course, and overall satisfaction with treatment was high. Coaches reported high treatment credibility and good clinical feasibility of the internet-based delivered intervention | + |
| Bross et al. (2020) | Approximately 6 weeks for each group | Social skills | All participants increased their planning skills but presented no increased participation in weekly social activities | Participants reported they liked the technology-based components of the intervention. Participants use their personal devices; little to no technical assistance was required | ? |
| Ford et al. (2020) | Intervention sessions scheduled 1 to 2 times per week, each for 15–60 min. Intervention duration changed due to number of sessions required to complete the changing criterion hierarchy | Daily living skills | All participants performed target daily living skills independently and reached individualized criteria |
Evaluation of technology was not presented Overall, participants positively perceived the intervention as helpful for their everyday lives |
+ |
| Hatfield et al. (2017) | Approximately 12 months to complete intervention (including 2-month period in which participants completed online outcome measures at the T2 measurement point) | Job interview skills | Adolescents’ self-reported a significant increase in career awareness |
Feedback from the pilot studies was used to modify the BOOST-A™ to enhance usability Adherence to the intervention was monitored using website analytics (numbers of logins and modules completed) and feedback from participants about the number of times they met with the team |
+ |
| Quality of life | Both intervention and control groups experienced a decrease in quality of life and increase in happiness with life | ? | |||
| Identity-related issues | No change in self-reported total self-determination score; parent-reported increases in adolescents’ self-determination | – | |||
| Hayes et al. (2015) | Treatment group received technology for personal use for 1 month; before and after this month, both groups completed outcome measures | Job interview skills |
All participants reported feeling more relaxed and/or confident in their interview performance during posttest mock employment interviews, regardless of intervention or control condition Interviewers assessed intervention group participants significantly higher after the intervention |
Interviews provide general information related to potential feasibility and efficacy of a mobile videomodeling and prompting tool for teaching interview skills | + |
| Hepburn et al. (2016) | Twelve sessions of 1.5 h. each across 3–4-month period | Reducing symptoms of ASD, anxiety, or depression | The telehealth version of Facing Your Fears has the potential to affect anxiety and excessive fears | The technology was found acceptable and usable for intervention to parents and adolescents with ASD. Therapist fidelity to critical elements of the original intervention was presented. The mean satisfaction score for adolescents was 88.8% | + |
| Joseph et al. (2021) | Participants reached mastery criteria in 9 to 13 sessions | Social skills | All intervention group participants increased on-topic conversational exchanges and decreased off-topic conversational exchanges. Two of the three participants maintained these skills when the intervention was removed | Evaluation of technology was not presented | + |
| Sehlin et al. (2020) | Initial face-to-face meeting with appointed coach followed by 8 weeks of twice-weekly internet-based coaching scheduled chat-sessions for 30–60 min. Two sessions (intervention Weeks 3 and 6) were also face-to-face meetings | Identity-related issues | Intervention group reported significant increase in self-esteem postintervention | A total of six dropouts in the intervention group who had completed at least one chat session but did not finalize the full 8 weeks of participation, leaving 80% (24/30) of individuals who completed the intervention | + |
| Reducing symptoms of ASD, anxiety, or depression | Significant differences were found in anxiety and depression postintervention between intervention and control groups; findings were partially due to increased anxiety and depression in the control group | ? | |||
| Quality of life | There were no significant differences in quality of life between intervention and control groups postintervention | – | |||
| Strickland et al. (2013) | Between two assessing sessions (7-day period), each treatment group participant completed program of basic knowledge about interviewing; one 30-min virtual practice session with a staff member | Job interview skills | Treatment group showed significant increase in interview content; intervention was more effective in teaching content, because participants’ nonverbal skills during interview did not change | Evaluation of technology was not presented | + |
| Tang et al. (2021) | Ten sessions of 1 h. per week | Social skills | Intervention group participants demonstrated greater improvements on social cognition (i.e., rating others’ mental states) | After developing the program, the system was tested with two children and two youth with ASD and their parents. The feedback helped identify potential problems, which were addressed prior to launching the system and the release of the prototype program | + |
| Reducing symptoms of ASD, anxiety, or depression | Participants experienced a trend toward reduction in autistic traits postintervention. Depression, anxiety, and self-efficacy did not significantly change postintervention | ? | |||
| Wentz et al. (2012) | Two face-to-face meetings and 8 weeks of biweekly 30–60 min support and coaching (chat sessions) | Identity-related issues | Self-esteem and sense of coherence (i.e., ability to cope with stressful situations) significantly improved postintervention | Evaluation of technology was not presented | + |
| Quality of life | Adolescent self-reported global quality of life significantly improved postintervention | + | |||
| Reducing symptoms of ASD, anxiety, or depression | Participants reported no significant change in depression | – |
+ = significant improvement; ? = partial improvement or tendency; – = no significant improvement
Technology Types
The hybrid-delivered interventions necessitated the use of hardware and software to conduct the studies. Of the 11 studies, seven evaluated the technology or referred to the participants' ability to use and access the technology and indicated good feasibility, usability, and acceptability (Table 4). The following paragraphs address the hardware and software.
Hardware
Four of the described remote interventions could be applied on any available device equipped with a webcam and headsets or built-in microphones available to the participants (Bross et al., 2020; Ford et al., 2020; Hatfield et al., 2017; Hepburn et al., 2016). In addition, one intervention was designed for laptops or computers but could be used on a mobile device in a case of technical issues (Joseph et al., 2021); four could be applied only on a computer (desktop or laptop) with an Internet connection (Sehlin et al., 2020; Strickland et al., 2013; Tang et al., 2021; Wentz et al., 2012); and one lacked specificity but referred to the intervention as “computer-based” (Backman et al., 2018). One intervention could apply only on a mobile device with iOS (Hayes et al., 2015).
Software
The reviewed studies indicated the use of commercial software for remote communication, such as Zoom, Facebook, various chat and mail programs, or a national platform for Internet-delivered treatments (e.g., Backman et al., 2018). For seven of the presented interventions, the researchers had developed software specifically for the intervention goals, such as the BOOST-A™ online program (Hatfield et al., 2017) and MindChip™ (Tang et al., 2018).
Discussion
Adolescence is a period of transition to adult life in the community. Given that the literature indicated that adolescents with ASD exhibit less independence in daily living skills (Lamash & Josman, 2020; Späth & Jongsma, 2020) and poorer community participation (Lamash et al., 2020; Tint et al., 2017) than their typical peers, there is a strong rationale for interventions in this area. Surprisingly, only one intervention designed to promote these adolescents’ independence in daily activities and preparation for adult community life (Ford et al., 2020) was found in this review.
In the last decade, there has been growing interest in the use of telehealth among various populations. However, the COVID-19 pandemic and subsequent isolation and restrictions expedited the need to implement evidence-based remotely delivered services. The aim of this review was to examine hybrid delivery of interventions designed to promote health- and behavioral-related outcomes for adolescents with ASD. Although some evidence suggested that telehealth-service outcomes may be effective (Ellison et al., 2021), rigorous research is still needed to capture and evaluate feasibility, acceptability, and efficacy of telehealth interventions to this population.
Findings from the current systematic review demonstrate that research is still in the early stages of investigating the efficacy of hybrid-delivered interventions for adolescents with ASD. The reviewed studies had been conducted in a limited number of geographic areas; hence, their findings are limited for generalization to this population in wider geographical areas or from different cultural backgrounds. In addition, most of the reviewed studies included an array of individual subjects or small samples. The total number of participants who received hybrid interventions (in all included studies) was extremely low. Although the difficulty of recruiting participants with complex conditions, especially with ASD, is understandable and even supported by the literature (e.g., Ahmed et al., 2020; Lord et al., 2005; Vozenilek, 1999), further studies with larger samples and more robust designs are needed to provide strong evidence supporting the efficacy of hybrid interventions for adolescents with ASD.
There was great variability regarding intervention targets within and across the studies in this review. Although the studies’ targets were relevant and recommended for adolescents with ASD in nonremote formats (e.g., Tomchek et al., 2017), the inclusion of multiple outcomes within studies with relatively low sample sizes makes it challenging to draw conclusions. For example, some interventions aimed at promoting identity-related components (e.g., self-determination, sense of ability, and sense of coherence) and emotional–psychological components (e.g., reduction in depression and anxiety; increase in quality of life). Future research with increased sample sizes may illuminate the extent to which various remote interventions best suit various outcomes.
Across the studies, there appeared to be underlying assumptions related to how increased knowledge among adolescents would lead to increased performance in activities. Two studies that used outcome measures focused on advancing more functional-based interventions found significant improvements (e.g., Ford et al., 2020; Hayes et al., 2015). Other studies, which relied on self-report measures related to identity and mental health, found varying levels of change. This finding is consistent with literature indicating the need for and the efficacy of interventions that are more focused and task-oriented among adolescents with ASD (Hodgetts & Park, 2017; Lamash & Josman, 2020; Odom et al., 2015).
Further, knowledge did not necessary translate to changes in behavior across the reviewed studies. This may indicate that remote interventions may be able to capitalize on adolescents’ everyday environments to promote functional behavior, as opposed to only knowledge. For example, participants’ knowledge of the content of an employment interview did not result in increased performance at the interview (Strickland et al., 2013). Additionally, increased knowledge of ASD characteristics did not translate to an acceptance of the diagnosis or a decrease in anxiety and depression (Backman et al., 2018). Lastly, increased planning skills did not equate to increased weekly social outings (Bross et al., 2020). It seems that targets of hybrid interventions may benefit from a focus on directly promoting adolescents’ performance or engagement.
No significant changes in social-skills or quality-of-life indices or reductions in autism, depression, or anxiety symptoms were noted. Thus, the effectiveness of hybrid intervention programs was equivocal for those purposes. Some literature suggested that efficient interventions for clinical anxiety or depression of adolescents with ASD require standardized approaches to improve their outcomes (Vasa et al., 2016). Moreover, findings on the efficacy of social-cognitive and social-skills interventions were inconsistent, and the authors recommended further investigations of existing and novel interventions (Tseng et al., 2020). Because ASD represents heterogeneous characteristics and a wide variety of difficulties and strengths (Fuentes et al., 2021), interventions for adolescents with ASD should focus on their abilities and strengths, which can be important and positive bases for any intervention (Donaldson et al., 2017; Lee et al., 2020).
One area of need for hybrid interventions is evaluation of components related to access to telehealth (or hybrid) interventions. In the recent PACE Framework, which outlines domains of measurement needed within telehealth interventions specific to Population and Health Outcomes, Access to Care, Costs and Cost Effectiveness, Experiences of Practitioners and Clients, Little et al. (2021) presented nine subdomains specific to Access to Care issues that may influence participant outcomes. In the studies reviewed, the researchers did not formally evaluate participants for digital literacy, and they inconsistently described how the participants obtained the hardware for the study purpose. Given the rapid increase in the use of telehealth to serve individuals with ASD, future studies must consider how to ensure that participants can access the interventions. Access considerations may include (a) ensuring hardware is included in the study (e.g., provide hardware to participants), (b) addressing varying levels of digital literacy among adolescents and caregivers, and (c) applying interventions that use participants’ everyday materials and do not require specialized materials.
Hybrid interventions are of great value to adolescents with ASD due to the interventions’ potential to increase collaboration, expand the diversity and number of customers, and connect in the adolescents’ natural environments. Clinicians should intensively develop and implement hybrid interventions for adolescents with ASD to promote their transition processes to independent adult living in the community. Researchers should further expand and substantiate evidence among larger samples worldwide.
Limitations
Any systematic review includes a selection of articles from a wide variety, and the exclusion process may create a bias in the results. The authors of this review endeavored to reduce this bias by adhering to Cochrane guideline recommendations for teamwork. An additional limitation was the large heterogeneity of the reviewed studies’ designs, methodologies, and participant characteristics. Although such heterogeneity provided a full overview of the literature to date, it also affected the ability to collectively synthesize the data. Finally, the quality of the included studies' evidence and the high risk of bias for many of the studies greatly limited the ability to make definitive conclusions. Additionally, participants’ age ranges were variable and some studies in this review included a percentage of participants that fell outside the targeted ages. Although single-subject designs play an important role in autism research, they must be systematically replicated to contribute to understandings in this field.
Author contribution
All the authors initiated the study and completed the literature search, completed the screening of the articles and decided on the final set of articles to be included in the review, led the design and the implementation of data extraction, analysis, and interpretation. All the authors drafted the initial manuscript, edited and revised the manuscript, and reviewed and approved the final version of the manuscript.
Funding
No funds, grants, or other support were received.
Declarations
Conflict of interest
The authors have no financial or proprietary interests in any material discussed in this article. The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Ahmed KL, Simon AR, Dempsey JR, Samaco RC, Goin-Kochel RP. Evaluating two common strategies for research participant recruitment into autism studies: Observational study. Journal of Medical Internet Research. 2020;22(9):e16752. doi: 10.2196/16752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4. American Psychiatric Press; 1994. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental health disorders. 5. American Psychiatric Association; 2013. [Google Scholar]
- Antonovsky A. Health, stress, and coping. Jossey-Bass; 1979. [Google Scholar]
- AutismSpeaks. (2021). Autism statistics and facts. https://www.autismspeaks.org/autism-statistics-asd
- Backman A, Mellblom A, Norman-Claesson E, Keith-Bodros G, Frostvittra M, Bölte S, Hirvikoski T. Internet-delivered psychoeducation for older adolescents and young adults with autism spectrum disorder (SCOPE): An open feasibility study. Research in Autism Spectrum Disorders. 2018;54:51–64. doi: 10.1016/j.rasd.2018.07.001. [DOI] [Google Scholar]
- Baron-Cohen S, Golan O, Wheelwright S, Hill JJ. Mind reading: The interactive guide to emotions. Jessica Kingsley; 2004. [Google Scholar]
- Baweja R, Brown SL, Edwards EM, Murray MJ. COVID-19 pandemic and impact on patients with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2021 doi: 10.1007/s10803-021-04950-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benevides TW, Shore SM, Andresen ML, Caplan R, Cook B, Gassner DL, Erves JM, Hazelwood TM, King MC, Morgan L, Murphy LE, Purkis Y, Rankowski B, Rutledge SM, Welch SP, Wittig K. Interventions to address health outcomes among autistic adults: A systematic review. Autism. 2020;24(6):1345–1359. doi: 10.1177/1362361320913664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(10):1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Bölte S, Fleck S, Dziobek I. Double movie for the assessment of social cognition-multiple choice (DMASC-MC) Hogrefe; 2014. [Google Scholar]
- Borkovec TD, Nau SD. Credibility of analogue therapy rationales. Journal of Behavior Therapy and Experimental Psychiatry. 1972;3(4):257–260. doi: 10.1016/0005-7916(72)90045-6. [DOI] [Google Scholar]
- Bradford N, Caffery L, Smith A. Telehealth services in rural and remote Australia: A systematic review of models of care and factors influencing success and sustainability. Rural and Remote Health. 2016 doi: 10.22605/RRH3808. [DOI] [PubMed] [Google Scholar]
- Bramham J, Young S, Bickerdike A, Spain D, McCartan D, Xenitidis K. Evaluation of group cognitive behavioral therapy for adults with ADHD. Journal of Attention Disorders. 2009;12(5):434–441. doi: 10.1177/1087054708314596. [DOI] [PubMed] [Google Scholar]
- Bross LA, Huffman JM, Watson EK, Wills HP, Mason RA. Social skills instruction, online modules, and telecoaching to develop planning skills of young adults with autism. Journal of Special Education Technology. 2020 doi: 10.1177/0162643420924188. [DOI] [Google Scholar]
- Clarke, M., & Oxman, A. D. (2002). Cochrane reviewers’ handbook 4.1. 5 [updated April 2002]. The Cochrane Library, 2
- Constantino JN, Gruber CP. Social Responsiveness Scale (SRS) Western Psychological Services; 2005. [Google Scholar]
- Constantino JN, Gruber CP. Social Responsiveness Scale-second edition (SRS-2): Manual. Western Psychological Services; 2012. [Google Scholar]
- Cooper K, Smith LG, Russell A. Social identity, self-esteem, and mental health in autism. European Journal of Social Psychology. 2017;47(7):844–854. doi: 10.1002/ejsp.2297. [DOI] [Google Scholar]
- Curtis AC. Defining adolescence. Journal of Adolescent and Family Health. 2015;7(2):2. [Google Scholar]
- Donaldson AL, Krejcha K, McMillin A. A strengths-based approach to autism: Neurodiversity and partnering with the autism community. Perspectives of the ASHA Special Interest Groups. 2017;2(1):56–68. doi: 10.1044/persp2.SIG1.56. [DOI] [Google Scholar]
- Dziobek I, Fleck S, Kalbe E, Rogers K, Hassenstab J, Brand M, Kessler J, Woike JK, Wolf OT, Convit A. Introducing MASC: A movie for the assessment of social cognition. Journal of Autism and Developmental Disorders. 2006;36:623–636. doi: 10.1007/s10803-006-0107-0. [DOI] [PubMed] [Google Scholar]
- Ellison KS, Guidry J, Picou P, Adenuga P, Davis TE., III Telehealth and autism prior to and in the age of COVID-19: A systematic and critical review of the last decade. Clinical Child and Family Psychology Review. 2021;24:599–630. doi: 10.1007/s10567-021-00358-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford K, Wang M, Koegel LK, Koegel RL, Fedders A. Use of a videoconferencing intervention and systematic hierarchy to teach daily living skills to young adults with autism spectrum disorder. Journal of Positive Behavior Interventions. 2020;23:81–92. doi: 10.1177/1098300720921214. [DOI] [Google Scholar]
- Fuentes J, Hervás A, Howlin P. ESCAP practice guidance for autism: A summary of evidence-based recommendations for diagnosis and treatment. European Child & Adolescent Psychiatry. 2021;30(6):961–984. doi: 10.1007/s00787-020-01587-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grynszpan O, Weiss PL, Perez-Diaz F, Gal E. Innovative technology-based interventions for autism spectrum disorders: A meta-analysis. Autism. 2014;18(4):346–361. doi: 10.1177/1362361313476767. [DOI] [PubMed] [Google Scholar]
- Hatfield M, Falkmer M, Falkmer T, Ciccarelli M. Effectiveness of the BOOST-A™ online transition planning program for adolescents on the autism spectrum: A quasi-randomized controlled trial. Child and Adolescent Psychiatry and Mental Health. 2017;11:1–12. doi: 10.1186/s13034-017-0191-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes GR, Custodio VE, Haimson OL, Nguyen K, Ringland KE, Ulgado RR, Waterhouse A, Weiner R. Mobile video modeling for employment interviews for individuals with autism. Journal of Vocational Rehabilitation. 2015;43:275–287. doi: 10.3233/JVR-150775. [DOI] [Google Scholar]
- Hepburn SL, Blakeley-Smith A, Wolff B, Reaven JA. Telehealth delivery of cognitive-behavioral intervention to youth with autism spectrum disorder and anxiety: A pilot study. Autism. 2016;20:207–218. doi: 10.1177/1362361315575164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savović J, Schulz KF, Weeks L, Sterne JAC. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011 doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirvikoski T, Waaler E, Alfredsson J, Pihlgren C, Holmstrom A, Johnson A, Rück J, Wiwe C, Bothn P, Nordstrom AL. Reduced ADHD symptoms in adults with ADHD after structured skills training group: Results from a randomized controlled trial. Behaviour Research and Therapy. 2011;49:175–185. doi: 10.1016/j.brat.2011.01.001. [DOI] [PubMed] [Google Scholar]
- Hodgetts S, Park E. Preparing for the future: A review of tools and strategies to support autonomous goal setting for children and youth with autism spectrum disorders. Disability and Rehabilitation. 2017;39(6):535–543. doi: 10.3109/09638288.2016.1161084. [DOI] [PubMed] [Google Scholar]
- Hume K, Boyd BA, Hamm JV, Kucharczyk S. Supporting independence in adolescents on the autism spectrum. Remedial and Special Education. 2014;35:102–113. doi: 10.1177/0741932513514617. [DOI] [Google Scholar]
- Jaworska N, MacQueen G. Adolescence as a unique developmental period. Journal of Psychiatry & Neuroscience. 2015;40:291–293. doi: 10.1503/jpn.150268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston C, Mash EJ. A measure of parenting satisfaction and efficacy. Journal of Clinical Child Psychology. 1989;18:167–175. doi: 10.1207/s15374424jccp1802_8. [DOI] [Google Scholar]
- Joseph B, Kearney KB, Brady MP, Downey A, Torres A. Teaching small talk: Increasing on-topic conversational exchanges in college students with intellectual and developmental disabilities using remote audio coaching. Behavior Modification. 2021;45:251–271. doi: 10.1177/0145445520975174. [DOI] [PubMed] [Google Scholar]
- Krevers B, Oberg B. Development of the patient perspective on care and rehabilitation process’ instrument (POCR) Aging Clinical and Experimental Research. 2002;14:402–411. doi: 10.1007/BF03324469. [DOI] [PubMed] [Google Scholar]
- Lamash L, Bedell G, Josman N. Participation patterns of adolescents with autism spectrum disorder compared to their peers: Parents’ perspectives. British Journal of Occupational Therapy. 2020;83:78–87. doi: 10.1177/0308022619853518. [DOI] [Google Scholar]
- Lamash L, Josman N. Full-information factor analysis of the daily routine and autonomy (DRA) questionnaire among adolescents with autism spectrum disorder. Journal of Adolescence. 2020;79:221–231. doi: 10.1016/j.adolescence.2020.01.011. [DOI] [PubMed] [Google Scholar]
- Lee EAL, Black MH, Falkmer M, Tan T, Sheehy L, Bölte S, Girdler S. “We can see a bright future”: Parents’ perceptions of the outcomes of participating in a strengths-based program for adolescents with autism spectrum disorder. Journal of Autism & Developmental Disorders. 2020;50(9):3179–3194. doi: 10.1007/s10803-020-04411-9. [DOI] [PubMed] [Google Scholar]
- Liebowitz MR. Social phobia. Modern Problems in Pharmacopsychiatry. 1987;22:141–173. doi: 10.1159/000414022. [DOI] [PubMed] [Google Scholar]
- Lindgren S, Wacker D, Suess A, Schieltz K, Pelzel K, Kopelman T, Lee J, Romani P, Waldron D. Telehealth and autism: Treating challenging behavior at lower cost. Pediatrics. 2016;137(Supp 2):S167–S175. doi: 10.1542/peds.2015-2851O. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little, L. M., Pickett, K. A., Proffitt, R., & Cason, J. (2021). Keeping PACE with 21st century healthcare: A framework for telehealth research, practice, and program evaluation in occupational therapy. International Journal of Telerehabilitation, 13(1). 10.5195/ijt.2021.6379 [DOI] [PMC free article] [PubMed]
- Little LM, Wallisch A, Pope E, Dunn W. Acceptability and cost comparison of a telehealth intervention for families of children with autism. Infants & Young Children. 2018;31:275–286. doi: 10.1097/IYC.0000000000000126. [DOI] [Google Scholar]
- Lord C, Wagner A, Rogers S, Szatmari P, Aman M, Charman T, Dawson G, Durand VM, Grossman L, Guthrie D, Harris S, Kasari C, Marcus L, Murphy S, Odom S, Pickles A, Scahill L, Shaw E, Siegel B, Yoder P. Challenges in evaluating psychosocial interventions for autistic spectrum disorders. Journal of Autism and Developmental Disorders. 2005;35:695–708. doi: 10.1007/s10803-005-0017-6. [DOI] [PubMed] [Google Scholar]
- Lorig K, Stewart A, Ritter P, Gonzalez V, Lynch J, Laurent D. Outcome measures for health education and other health care interventions. Sage; 1996. [Google Scholar]
- Lovibond SH, Lovibond PF. Manual for the depression anxiety & stress scales. 2. Psychology Foundation; 1995. [Google Scholar]
- Mazon C, Fage C, Sauzéon H. Effectiveness and usability of technology-based interventions for children and adolescents with ASD: A systematic review of reliability, consistency, generalization, and durability related to the effects of intervention. Computers in Human Behavior. 2019;93:235251. doi: 10.1016/j.chb.2018.12.001. [DOI] [Google Scholar]
- Meeus W. Adolescent psychosocial development: A review of longitudinal models and research. Developmental Psychology. 2016;52(12):1969–1993. doi: 10.1037/dev0000243. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, Prisma Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odom SL, Thompson JL, Hedges S, Boyd BA, Dykstra JR, Duda MA, Szidon KL, Smith LE, Bord A. Technology-aided interventions and instruction for adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2015;45(12):3805–3819. doi: 10.1007/s10803-014-2320-6. [DOI] [PubMed] [Google Scholar]
- Priebe S, Huxley P, Knight S, Evans S. Application and results of the manchester short assessment of quality of life (MANSA) International Journal of Social Psychiatry. 1999;45:7–12. doi: 10.1177/002076409904500102. [DOI] [PubMed] [Google Scholar]
- Rispoli M, Machalicek W. Advances in telehealth and behavioral assessment and intervention in education: Introduction to the special issue. Journal of Behavioral Education. 2020;29:189–194. doi: 10.1007/s10864-020-09383-5. [DOI] [Google Scholar]
- Rodriguez K. Maintaining treatment integrity in the face of crisis: A treatment selection model for transitioning direct ABA services to telehealth. Behavior Analysis in Practice. 2020;13:291–298. doi: 10.1007/s40617-020-00429-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg M. Society and the adolescent self-image. rev. Wesleyan University Press; 1989. [Google Scholar]
- Roux AM. National autism indicators report: Transition into young adulthood. A. J. Drexel Autism Institute; 2015. [Google Scholar]
- Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child & Adolescent Health. 2018;2:223–228. doi: 10.1016/S2352-4642(18)30022-1. [DOI] [PubMed] [Google Scholar]
- Sehlin H, Ahlström BH, Bertilsson I, Andersson G, Wentz E. Internet-based support and coaching with complementary clinic visits for young people with attention-deficit/hyperactivity disorder and autism: Controlled feasibility study. Journal of Medical Internet Research. 2020;22(12):e19658. doi: 10.2196/19658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seltzer MM, Krauss MW, Shattuck PT, Orsmond G, Swe A, Lord C. The symptoms of autism spectrum disorders in adolescence and adulthood. Journal of Autism and Developmental Disorders. 2003;33:565–581. doi: 10.1023/B:JADD.0000005995.02453.0b. [DOI] [PubMed] [Google Scholar]
- Shulver W, Killington M, Crotty M. “Massive potential” or “safety risk?” Health worker views on telehealth in the care of older people and implications for successful normalization. BMC Medical Informatics and Decision Making. 2016;16(1):1–15. doi: 10.1186/s12911-016-0373-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simacek J, Dimian AF, McComas JJ. Communication intervention for young children with severe neurodevelopmental disabilities via telehealth. Journal of Autism and Developmental Disorders. 2017;47(3):744–767. doi: 10.1007/s10803-016-3006-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith LE, Anderson KA. The roles and needs of families of adolescents with ASD. Remedial and Special Education. 2014;35(2):114–122. doi: 10.1177/0741932513514616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Späth EM, Jongsma KR. Autism, autonomy, and authenticity. Medicine, Health Care and Philosophy. 2020;23:73–80. doi: 10.1007/s11019-019-09909-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L. Age of opportunity: Lessons from the new science of adolescence. Houghton Mifflin Harcourt; 2014. [Google Scholar]
- Strickland DC, Coles CD, Southern LB. JobTIPS: A transition to employment program for individuals with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2013;43:2472–2483. doi: 10.1007/s10803-013-1800-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutherland R, Trembath D, Hodge MA, Rose V, Roberts J. Telehealth and autism: Are telehealth language assessments reliable and feasible for children with autism? International Journal of Language & Communication Disorders. 2019;54:281–291. doi: 10.1111/1460-6984.12440. [DOI] [PubMed] [Google Scholar]
- Tang J, Falkmer M, Chen NTM, Bӧlte S, Girdler S. Designing a serious game for youth on the autism spectrum: Perspectives from end-users and professionals. Journal of Autism and Developmental Disorders. 2018;49(3):978–995. doi: 10.1007/s10803-018-3801-9. [DOI] [PubMed] [Google Scholar]
- Tang JS, Falkmer M, Chen NT, Bӧlte S, Girdler S. Development and feasibility of MindChip™: A social emotional telehealth intervention for autistic adults. Journal of Autism and Developmental Disorders. 2021;51:1107–1130. doi: 10.1007/s10803-020-04592-3. [DOI] [PubMed] [Google Scholar]
- Tawfik GM, Dila KAS, Mohamed MYF, Tam DNH, Kien ND, Ahmed AM, Huy NT. A step by step guide for conducting a systematic review and meta-analysis with simulation data. Tropical Medicine and Health. 2019;47(1):1–9. doi: 10.1186/s41182-019-0165-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tint A, Maughan AL, Weiss JA. Community participation of youth with intellectual disability and autism spectrum disorder. Journal of Intellectual Disability Research. 2017;61:168–180. doi: 10.1111/jir.12311. [DOI] [PubMed] [Google Scholar]
- Tomchek S, Koenig KP. Occupational therapy practice guidelines for individuals with autism spectrum disorder. AOTA Press; 2016. [Google Scholar]
- Tomchek S, Koenig KP, Arbesman M, Lieberman D. Occupational therapy interventions for adolescents with autism spectrum disorder. American Journal of Occupational ThErapy. 2017;71:7101395010p1–7101395010p3. doi: 10.5014/ajot.2017.711003. [DOI] [PubMed] [Google Scholar]
- Tseng A, Biagianti B, Francis SM, Conelea CA, Jacob S. Social cognitive interventions for adolescents with autism spectrum disorders: A systematic review. Journal of Affective Disorders. 2020;274:199–204. doi: 10.1016/j.jad.2020.05.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasa RA, Mazurek MO, Mahajan R, Bennett AE, Bernal MP, Nozzolillo AA, Arnold LE, Coury DL. Assessment and treatment of anxiety in youth with autism spectrum disorders. Pediatrics. 2016;137:S115–S123. doi: 10.1542/peds.2015-2851J. [DOI] [PubMed] [Google Scholar]
- Veritas Health Innovation. (n.d.). Covidence systematic review software [Computer software]. www.covidence.org
- Vozenilek GP. Meeting the challenges of recruiting and retaining participants in clinical trials. Journal of the American Dietetic Association. 1999;99:1192. doi: 10.1016/S0002-8223(99)00288-6. [DOI] [PubMed] [Google Scholar]
- Wallisch A, Little L, Pope E, Dunn W. Parent perspectives of an occupational therapy telehealth intervention. International Journal of Telerehabilitation. 2019;11(1):15–22. doi: 10.5195/ijt.2019.6274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wehmeyer, M. L. (1995). The Arc’s self-determination scale: Procedural guidelines (ED441322). ERIC. https://eric.ed.gov/?id=ED441322
- Wentz E, Nydén A, Krevers B. Development of an internet-based support and coaching model for adolescents and young adults with ADHD and autism spectrum disorders: A pilot study. European Child & Adolescent Psychiatry. 2012;21:611–622. doi: 10.1007/s00787-012-0297-2. [DOI] [PubMed] [Google Scholar]
- White SW, Stoppelbein L, Scott H, Spain D. It took a pandemic: Perspectives on impact, stress, and telehealth from caregivers of people with autism. Research in Developmental Disabilities. 2021 doi: 10.1016/j.ridd.2021.103938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2007). International classification of functioning, disability, and health: Children & youth version; ICF-CY. https://apps.who.int/iris/handle/10665/43737
- World Health Organization. (2010). Telemedicine: Opportunities and developments in member states. https://apps.who.int/iris/handle/10665/44497
- World Health Organization. (2013). Adolescent health. https://www.who.int/health-topics/adolescent-health#tab=tab_1
- World Health Organization. (2020). Adolescent health and development. https://www.who.int/westernpacific/news/q-a-detail/adolescent-health-and-development
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]