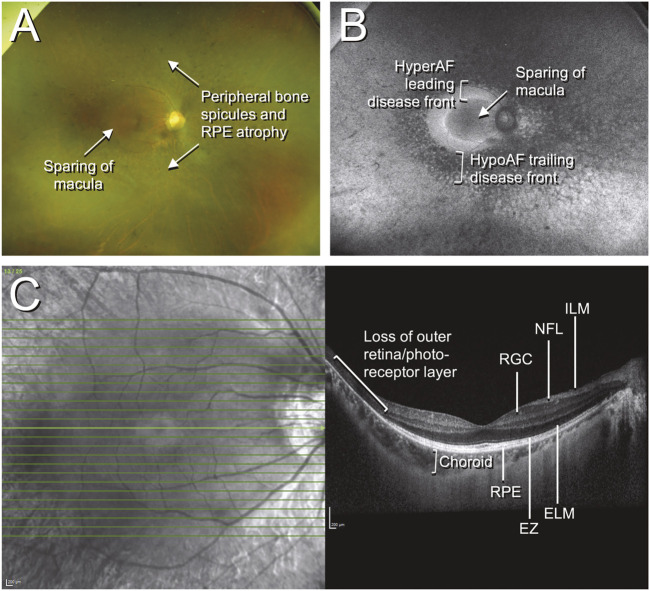
FIGURE 1.
Color fundus photographs, autofluorescence, and optical coherence tomography (OCT) of retinitis pigmentosa. The patient was a 42-year-old Chinese male who presented with an incidental finding of peripheral field loss during an inpatient admission for migraine headache. A long-standing history of nyctalopia was elicited but there was no evidence of neurosensory hearing loss. Whole exome sequencing (WES) uncovered the presence of biallelic pathogenic EYS mutations. (A) Fundus imaging shows peripheral bone spicule-like pigmentary retinopathy with outer retinal atrophy and sparing of the macula; (B) fundus autofluorescence highlights the areas of disease, with the hypoautofluorescent (hypoAF) trailing disease front appearing as dark areas and the hyperautofluorescent (hyperAF) leading disease front appearing as brighter areas; (C) horizontal cross-sectional OCT at the level of the fovea shows intact retinal layers at the fovea with loss of the outer retina and photoreceptor layers in the periphery. Selected retinal layers relevant to gene-based therapy are shown: ILM, internal limiting membrane; NFL, nerve fiber layer; RGC, retinal ganglion cell layer; RPE, retinal pigment epithelium; EZ, ellipsoid zone (photoreceptor inner/outer segments); ELM, external limiting membrane.