Recent evidence has shown that COVID-19 immunity and vaccine effectiveness wanes over time.1 Together with the emergence of the omicron (B.1.1.529) variant with substantial antibody escape,2 this resulted in widespread implementation of booster vaccinations to optimise immunity and protection. With increasing availability of vaccines and evidence towards improved immunogenicity of heterologous vaccine regimens,3 knowledge on the immunogenicity of different vaccine combinations and how to best induce booster immunity is of paramount importance to guide vaccination policies. A homologous third dose of CoronaVac (Sinovac) given 8 months after the second dose was shown to be associated with an increase in detectable antibodies,4 whereas immunogenicity data for heterologous boosting was unknown.
In The Lancet, Sue Costa Clemens and colleagues provide timely results of a randomised trial on the reactogenicity and immunogenicity of a homologous and three different heterologous booster vaccines among individuals who had received two doses of the CoronaVac vaccine.5 A total of 1240 individuals from São Paulo and Salvador, Brazil, without history of SARS-CoV-2 infection were randomly assigned to receive a third dose with either CoronaVac, the mRNA vaccine BNT162b2 (Pfizer–BioNTech), or one of the vector vaccines ChAdOx nCov-19 (AstraZeneca), or AD25.COV2-S (Janssen). Adult study participants were recruited to include two equally sized age groups: younger than 60 years and 61 years and older. 1205 individuals, of whom 729 (60·5%) were women and 814 (67·6%) were White, were available for analysis of primary outcomes, which included reactogenicity and immunogenicity of IgG antibodies and neutralising activity before the boost and 28 days after.5
Three serious adverse events possibly related to the vaccine occurred, which resolved completely. Otherwise, all booster doses were well tolerated with commonly observed local and systemic reactions predominantly found after heterologous boosting. Local pain at the injection site was most frequent among recipients of BNT162b2, whereas systemic adverse events predominated among vector recipients. This safety profile is reassuring and will likely not influence the choice of booster vaccine in clinical practice. Antibody concentrations were remarkably low 6 months after the primary vaccine doses (20·4% [95% CI 12·8–30·1] in adults younger than 60 years and 8·9% [4·2–16·2] in older individuals), and were induced in all study groups by day 28 after boosting. Another recent study from Hong Kong confirmed low median antibody titres in individuals vaccinated with CoronaVac 4 months after primary vaccination.6 Although CoronaVac recipients in the present study had the most favourable safety profile, the magnitude of the antibody boost was significantly lower compared with all heterologous regimens. As exemplified for IgG titres, the increase from baseline to 28 days was 12-fold for CoronaVac, 152-fold for BNT162b2, 90-fold for ChAdOx, and 77-fold for AD25.COV2-S. This effect held true for all immunological parameters including neutralising activity, where the booster effect was most pronounced in recipients of BNT162b2, followed by the two vector vaccines where immunogenicity was largely similar. Neutralising capacity towards the delta and omicron variants were well induced after heterologous boosting in more than 90% of individuals. By contrast, only 80% and 35% of individuals after CoronaVac boosting had neutralising activity towards delta and omicron, respectively. Across all vaccines, responses after boosting were lower in the older age group than in the younger group.5
Although the COV-BOOST study with different vaccine combinations has shown a similar advantage of mRNA and vector vaccines over adjuvanted protein-based vaccines,7 the rapidly spreading omicron variant underscores the need for large cohort studies to determine whether the differences in immunogenicity after booster vaccination observed with age and vaccine regimens will correlate with different susceptibility towards infection or disease. Additionally, with increasing immune escape, there is a need for diagnostic assays adapted to characterise vaccine-induced humoral and cellular immunity towards specific SARS-CoV-2 variants, which should also include determination of meaningful correlates for protection.8, 9 Of note, the present study did not assess T-cell immunity, which could inform on the ability to protect from severe disease and which was shown to be markedly induced after heterologous vector or mRNA vaccination in healthy and immunocompromised individuals.3, 10
Among approximately 10 billion vaccine doses administered globally, CoronaVac accounts for more than 2 billion doses, making it the world's most frequently used SARS-CoV-2 vaccine.11 It is noteworthy to mention that there are considerable price differences between the SARS-CoV-2 vaccines, which could influence the choice of booster vaccines in low-income and middle-income countries. However, as a result of WHO's endorsement of heterologous vaccine schedules12 and Costa Clemens' study, we strongly believe that heterologous boosting with mRNA or vector vaccines after primary CoronaVac vaccination should be advised to rapidly regain protective antibody concentrations.
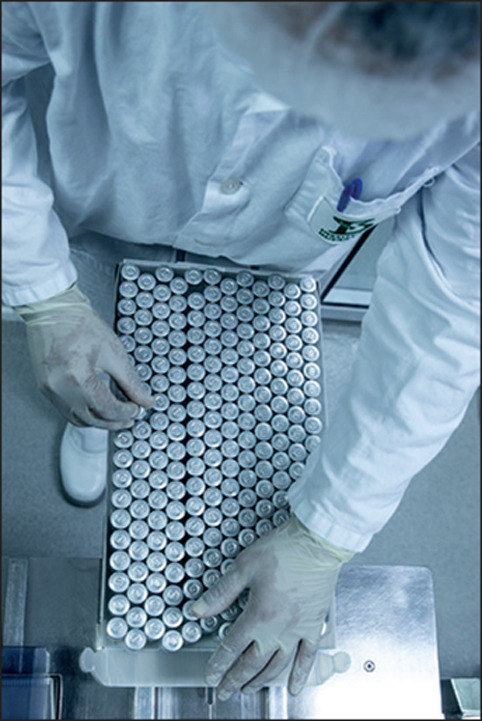
© 2022 Alexandre Schneider/Stringer/Getty Images
MS has received grant support from Astellas Pharmaceuticals and Biotest to her institution, Saarland University, outside the area of work commented on here, and honoraria for lectures from Biotest and Novartis. SLB has received travel grants and speaker fees from Astellas Pharmaceuticals, Becton Dickinson, Novartis, Pfizer, and Shionogi outside the area of work commented on here, and participated on advisory boards of Pfizer (pertaining to ceftazidime/avibactam) and Shionogi (pertaining to cefiderocol).
References
- 1.Chemaitelly H, Tang P, Hasan MR, et al. Waning of BNT162b2 vaccine protection against SARS-CoV-2 infection in Qatar. N Engl J Med. 2021;385:e83. doi: 10.1056/NEJMoa2114114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu L, Iketani S, Guo Y, et al. Striking antibody evasion manifested by the omicron variant of SARS-CoV-2. Nature. 2021 doi: 10.1038/s41586-021-04388-0. published online Dec 23. [DOI] [PubMed] [Google Scholar]
- 3.Schmidt T, Klemis V, Schub D, et al. Immunogenicity and reactogenicity of heterologous ChAdOx1 nCoV-19/mRNA vaccination. Nat Med. 2021;27:1530–1535. doi: 10.1038/s41591-021-01464-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zeng G, Wu Q, Pan H, et al. Immunogenicity and safety of a third dose of CoronaVac, and immune persistence of a two-dose schedule, in healthy adults: interim results from two single-centre, double-blind, randomised, placebo-controlled phase 2 clinical trials. Lancet Infect Dis. 2021 doi: 10.1016/S1473-3099(21)00681-2. published online Dec 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Costa Clemens SA, Weckx L, Clemens R, et al. Heterologous versus homologous COVID-19 booster vaccination in previous recipients of two doses of CoronaVac COVID-19 vaccine in Brazil (RHH-001): a phase 4, non-inferiority, single blind, randomised study. Lancet. 2022 doi: 10.1016/S0140-6736(22)00094-0. published online Jan 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kwok SL, Cheng SMS, Leung JNS, et al. Waning antibody levels after COVID-19 vaccination with mRNA Comirnaty and inactivated CoronaVac vaccines in blood donors, Hong Kong, April 2020 to October 2021. Euro Surveill. 2022 doi: 10.2807/1560-7917. published online Jan 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Munro APS, Janani L, Cornelius V, et al. Safety and immunogenicity of seven COVID-19 vaccines as a third dose (booster) following two doses of ChAdOx1 nCov-19 or BNT162b2 in the UK (COV-BOOST): a blinded, multicentre, randomised, controlled, phase 2 trial. Lancet. 2021;398:2258–2276. doi: 10.1016/S0140-6736(21)02717-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu J, Chandrashekar A, Sellers D, et al. Vaccines elicit highly cross-reactive cellular immunity to the SARS-CoV-2 omicron variant. medRxiv. 2022 doi: 10.1101/2022.01.02.22268634. published online Jan 3. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dejnirattisai W, Shaw RH, Supasa P, et al. Reduced neutralisation of SARS-CoV-2 omicron B.1.1.529 variant by post-immunisation serum. Lancet. 2022;399:234–236. doi: 10.1016/S0140-6736(21)02844-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schmidt T, Klemis V, Schub D, et al. Cellular immunity predominates over humoral immunity after homologous and heterologous mRNA and vector-based COVID-19 vaccine regimens in solid organ transplant recipients. Am J Transplant. 2021;21:3990–4002. doi: 10.1111/ajt.16818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mathieu E, Ritchie H, Ortiz-Ospina E, et al. A global database of COVID-19 vaccinations. Nat Hum Behav. 2021;5:947–953. doi: 10.1038/s41562-021-01122-8. [DOI] [PubMed] [Google Scholar]
- 12.WHO Interim recommendations for heterologous COVID-19 vaccine schedules. 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-vaccines-SAGE-recommendation-heterologous-schedules


