Figure 1.
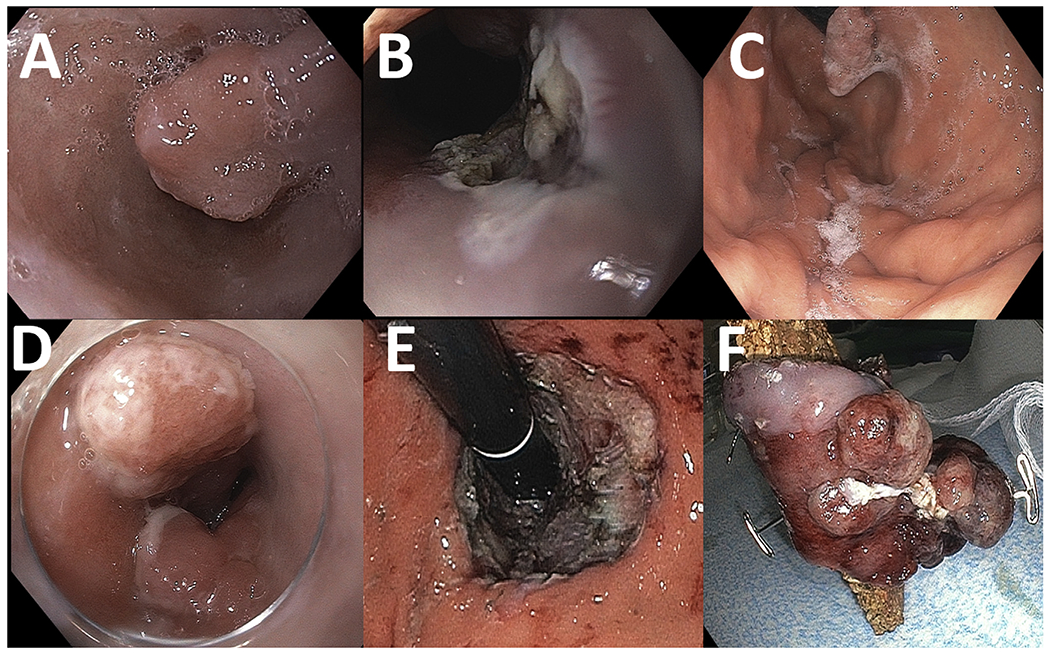
An 84-year-old patient with a 12-mm protruding lesion (Paris Is) in the background of Barrett’s esophagus is referred for endoscopy (A). The lesion is resected with EMR (B), with pathology confirming this to be a well-differentiated invasive adenocarcinoma with positive deep margins. The patient is deemed not a surgical candidate. He undergoes 4 sessions of cryotherapy and a second EMR due to recurrence of the nodule (C), with pathology demonstrating at least intramucosal adenocarcinoma with no lymphovascular invasion. The patient is subsequently referred for ESD. Two adjacent 10- to 15-mm nodules (Paris Is) were identified at the gastroesophageal junction on retroflexion (D). Successful circumferential ESD (E) with en bloc resection of a 60 × 30 mm tubular specimen (F). Pathology: Focal intramucosal adenocarcinoma with negative lateral and deep resection margins.
