Figure 5.
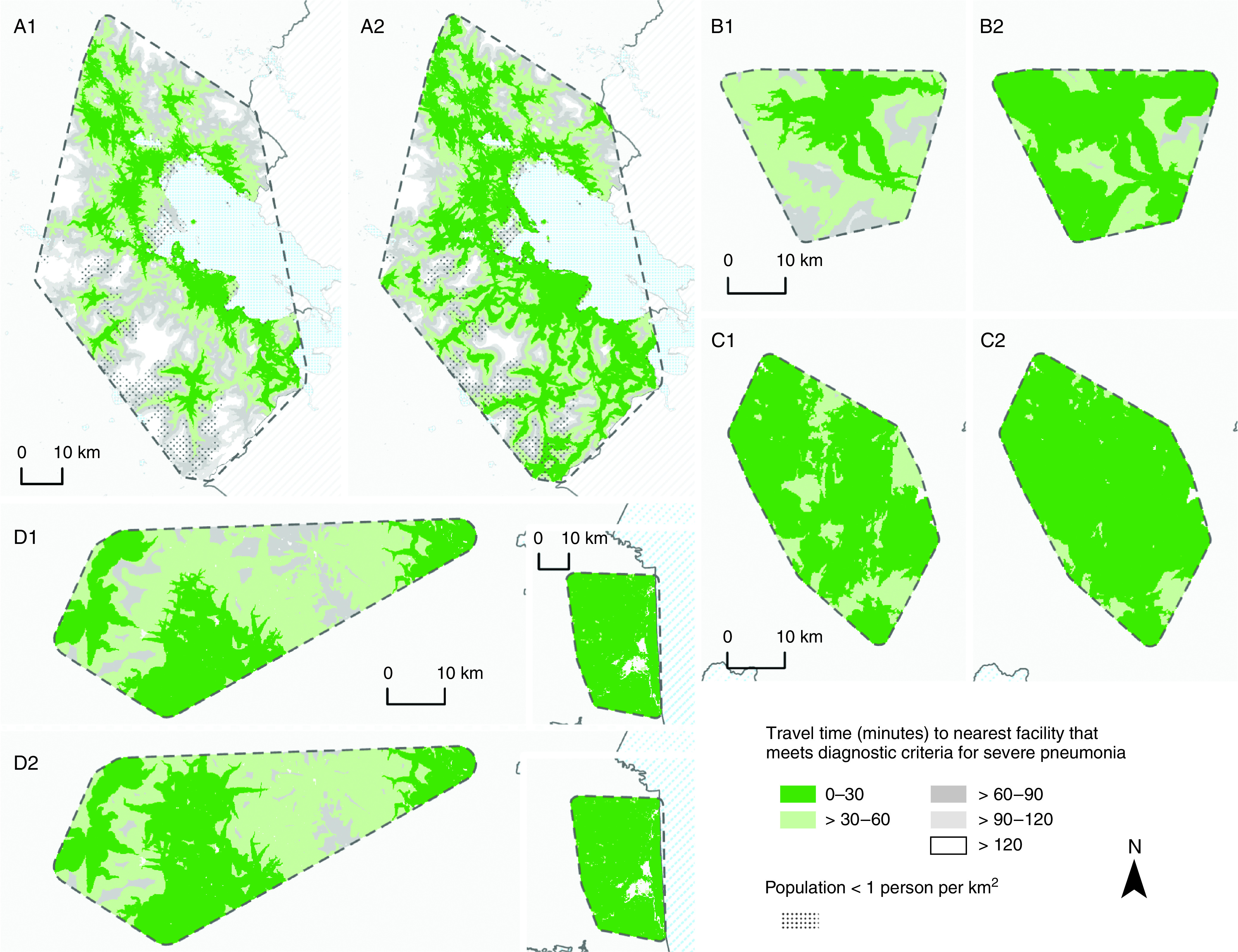
Geographic access to health facilities adequately resourced to diagnose and refer cases of severe pneumonia before and after the implementation of universal pulse oximetry coverage. (A1, B1, C1, and D1) Shading indicates the study areas in Puno, Peru; Kayonza, Rwanda; Jalapa, Guatemala; and Tamil Nadu, India (T-IND), respectively, that were within 10, 30, 60, 90, or 120 minutes of a facility with pulse oximetry (at the time of survey administration) for the diagnosis and referral of severe pneumonia; by default, this included facilities that were adequately resourced to treat severe pneumonia. (A2, B2, C2, and D2) Shading indicates regions in Puno, Peru; Kayonza, Rwanda; Jalapa, Guatemala; and T-IND, respectively, that would be within 30, 60, 90, or 120 minutes of a facility meeting the same diagnostic criteria if pulse oximetry were universally available in all facilities. Study area boundaries were estimated by using buffers equaling the average distance between each health facility and its closest neighboring health facility. Road networks were constructed by using OpenStreetMap roads where motorized travel was possible. Each study area was divided into a gridded matrix of 0.1 × 0.1-km cells, and the origin–destination cost matrix solver from ArcGIS Pro Network Analyst was used to estimate the least-cost pathway in minutes from every cell to the nearest facility with pulse oximetry before and after the hypothetical pulse oximetry intervention. Travel time accounted for road attributes, such as speed limits and directional limitations, and incorporated multiple modes of travel (i.e., walking to the road at 5 km/h and driving at half of the speed limit thereafter). Maps were not drawn to scale. The T-IND study site comprises two separate sites in Villupuram (left) and Nagapattinam (right).
