Abstract
While severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection primarily causes inflammation in the respiratory system, there is growing evidence of extrapulmonary tissue damage mediated by the host innate immune system in children and adults. A cytokine storm can manifest as a viral‐induced haemophagocytic lymphohistiocytosis (HLH). Here, we present a previously healthy 8‐year‐old boy with newly diagnosed cardiac injury and COVID‐19‐related HLH syndrome with haemophagocytosis in bone marrow biopsy. After remission of inflammation, the patient underwent a heart transplant due to persistent cardiac failure. The histology of the explanted heart showed only a focal subtle subendocardial inflammation. Three days after transplant, he developed progressive acute respiratory distress syndrome (ARDS) with the rise of inflammatory markers. He unfortunately died after 20 days because of disseminated intravascular coagulation (DIC). For the first time, we described a child with COVID‐19‐related HLH and severe cardiac failure, which had a poor prognosis despite a heart transplant.
Keywords: Acute heart failure, COVID‐19, Haemophagocytic lymphohistiocytosis syndrome, MIS‐C, Heart transplant, Haemophagocytosis
Introduction
Extrapulmonary involvement has been commonly documented since the outbreak of severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) in December 2019. 1 Symptoms in children are generally milder than in adults. 2 However, in the spectrum of cytokine storm, a variety of multisystem inflammatory syndromes in children (MIS‐C) overlapping with Kawasaki, macrophage activated syndrome (MAS), and haemophagocytic lymphohistiocytosis (HLH) have been identified from various centres in which usually occurred after a few weeks of acute infection. 3 , 4 , 5 , 6 Although most of the children with MIS recovered, some showed multi end‐organ failure with poor outcomes. 7 , 8
Case report
A previously healthy 8‐year‐old boy was referred to our heart tertiary centre for further workup because of severe heart failure and the rise of inflammatory markers. He'd been admitted to a local hospital 2 weeks prior with a fever and heart failure, where he was treated with supportive therapy and a suspected diagnosis of myocarditis. The polymerase chain reaction (PCR) for SARS‐CoV‐2 was negative, but the serology IgG was positive. He was afebrile with a heart rate of 135 beats/min, respiratory 26 breaths/min, and blood pressure 95/55 mmHg on his referral. He had hepatomegaly. Upon admission to our centre, the blood count showed leucocytosis and lymphopenia white blood count 13.4 × 103/μL (lymphocyte 2.5%), anaemia Hg 8.5 g/dL, and mild thrombocytopenia 140 × 103/μL. Troponin was weakly positive (0.56 ng/mL, normal range < 0.03 ng/mL). The laboratory findings showed evidence of liver and cardiac injury, coagulopathy, and elevated inflammatory markers. Detailed laboratory finding during admission in our centre is available in Table 1 .
Table 1.
Laboratory findings
| During admission | Pre‐transplant | 10 days post‐transplant | |
|---|---|---|---|
| White blood cells (× 103/μL) | 13.4 | 9900 | 23 |
| Lymphocytes (%) | 2.5% | 10% | 2% |
| Haemoglobin (g/dL) | 8.5 | 10 | 9 |
| Platelets (× 103/μL) | 140 | 196 | 61 |
| Aspartate aminotransferase (U/L) | 57 | 34 | 196 |
| Alanine aminotransferase (U/L) | 83 | 31 | 50 |
| Total bilirubin (mg/dL) | 10.2 | 3 | 8.4 |
| Direct bilirubin (mg/dL) | 6.6 | 1.5 | 6.2 |
| Prothrombin time (s) | 19 | 19 | 19 |
| International normalized ratio | 1.3 | 1.37 | 1.5 |
| Partial thromboplastin time (s) | 50 | 39 | 40 |
| C‐reactive protein (mg/L) | 15 | 3 | 36 |
| Erythrocyte sedimentation rate (ESR) (mm) | 17 | 6 | 17 |
| Lactate dehydrogenase (U/L) | 962 | 1208 | |
| Ferritin (ng/mL) | 750 | 280 | 922 |
| Triglycerides (mg/dL) | 300 | ||
| Troponin‐I (ng/mL) | 0.56 | 0.096 | 1.4 |
| N‐terminal pro‐B‐type natriuretic peptide (pg/mL) | 4800 | 4347 | >5000 |
| Lactate (mmol/L) | 4.3 | 2.1 | |
| D‐dimer, μ/mL | 10.9 | 2.08 | 1.9 |
| CD25 (soluble IL2 receptor α) (U/mL) | 3200 |
Chest computed tomography (CT) on admission showed only pulmonary congestion with no evidence of COVID‐19 lung features (Figure 1 A ). On Day 3 of admission to our centre, the cardiac magnetic resonance imaging (MRI) showed enlarged left ventricle (LV) size and severe biventricular dysfunction (Supporting Information, Video S1 ). There was an increased signal intensity in the mid septum in T2 weighted fat‐saturated sequences (Figure 1 B ) and focal nearly transmural enhancement in the late gadolinium sequences (Figure 1 C ) suggestive of dilated cardiomyopathy with oedema and possible focal fibrosis. There is also a large thrombus in the LV (Figure 1 C , Supporting Information, Video S2 ). PCR tests on blood for other viral aetiologies, including cytomegalovirus and Epstein bar virus, were negative. Regarding the presence of high total and direct bilirubin levels (10.2 and 6.6 mg/dL, respectively), a liver biopsy was performed showed diffuse sinusoidal dilation and patchy haemorrhage and necrosis which could be attributed to cardiomyopathy. He undertook bone marrow aspiration in approach to the bi‐cytopenia, which showed haemophagocytosis (Figure 2 A ). There is also markedly elevated CD25 (soluble IL‐2 receptor‐α). Antinuclear antibodies were negative; the workup for metabolic and underlying cancer was negative. According to clinical and laboratory findings, the diagnosis of haemophagocytic lymphohistiocytosis was made, fulfilling 2004 HLH Criteria. 9
Figure 1.
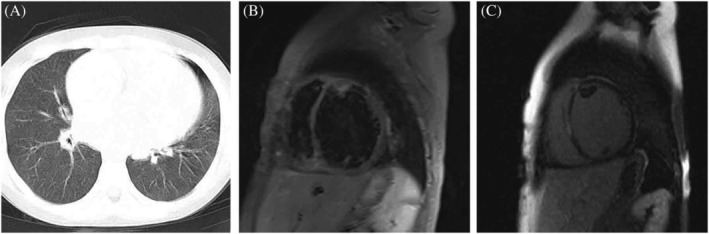
(A) Axial lung CT on admission showing enlarged cardiac margins and pulmonary congestion with no evidence of COVID‐19 features. (B) Cardiac MRI T2 weighted fat suppression images showing inflammation in the anterior and septal wall. (C) Late gadolinium enhancement images demonstrating nearly transmural foci of fibrosis in the septal wall with a large thrombus attached to the anterior wall.
Figure 2.
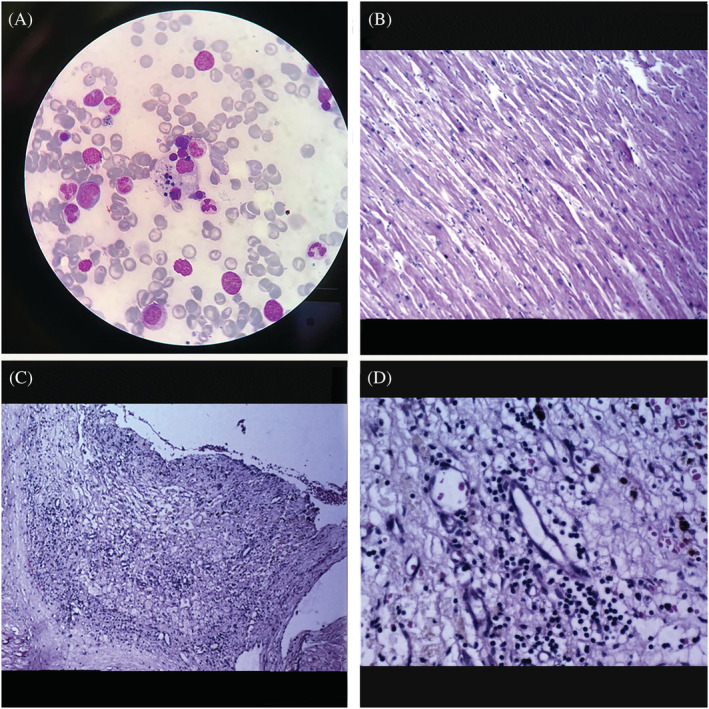
(A) Bone marrow aspirates showing erythrocytes and lymphocytes engulfed by bizarrely shaped macrophage. (B) Microscopic examination shows cardiac myocytes with mild to moderate hypertrophy and delicate interstitial fibrosis. (C and D) Focus of mural granulation tissue formation and scattered chronic inflammatory cells—lymphocytic infiltration restricted to endocardium—is seen.
According to the guidelines 9 and the availability of drugs, we initiated immunomodulatory treatment in addition to anticoagulation therapy. Intravenous immunoglobulin (IVIG) 1 g/kg was given for 2 days plus methylprednisolone intravenous pulse 30 mg/kg for 3 days in addition to intravenous heparin. We continued methylprednisolone 2–3 mg/kg for 5 days. During the 3 weeks, the laboratory inflammatory markers reduced (Table 1 ); however, the cardiac condition deteriorated. After a multidisciplinary team discussion regarding persistent severe heart failure, the patient was scheduled for heart transplantation (HT). HT was performed 5 weeks after admission to our centre. The macroscopic examination of the explanted heart showed increased heart weight and enlarged ventricular cavities. Histological features revealed nuclear enlargement, anisonucleosis, and focal myocyte vacuolation due to myofibrils loss and delicate interstitial fibrosis. One focus of mural granulation tissue formation containing scattered chronic inflammatory cells with lymphocytic infiltration restricted to subendocardium in the mid septum was detected (Figure 2B‐D ). No overt inflammation is seen. No overt necrosis is seen. The PCR for Parvovirus B19, enterovirus, human herpesvirus, and adenovirus was negative. Unfortunately, the tissue PCR on myocardium for SARS‐CoV‐2 was not available at the time of heart explantation in our centre; however, it became available recently, so it was checked on the available samples according to previously taken consent, and it was negative.
After the transplant, immunosuppression protocol was initiated with mycophenolate mofetil, everolimus, methylprednisolone intravenous pulse, and anti‐thymocyte globulin for 2 days. Three days after transplant, he experienced respiratory distress and hypoxia. The inflammatory markers were increased, and the blood test showed lymphopenia and low platelet count (Table 1 ). The lung CT showed bilateral ground‐glass opacities and progressed to acute respiratory distress syndrome (ARDS) (Supporting Information, Figure S1 ). The left ventricular ejection fraction (LVEF) was 50%. We sent multiple blood cultures. We held mycophenolate mofetil with the suspicion of infection and started a broad‐spectrum antibiotic, lopinavir/ritonavir, and azithromycin. After ruling out infection and graft rejection, Rituximab, steroid, and IVIG were added to the treatment in response to the relapse of inflammatory condition. The blood cultures were sterile, Rituximaband the repeated PCR test for SARS‐CoV‐2 returned negative. Unfortunately, after 20 days of supportive care, the patient eventually developed disseminated intravascular coagulation (DIC) and died. Despite the troponin rise after the heart transplant, which remained high throughout the course, the LV function was preserved during the post‐transplant period.
Discussion
Secondary HLH and macrophage activating syndrome are overlapping phenotypes of hyperinflammatory conditions such as cancers, viral infection, and autoimmune disorders. The high ferritin, liver injury, coagulopathy, and hypertriglyceridaemia are features of secondary HLH. 9 , 10 There is no clear data on the prevalence of COVID‐related HLH. This is because the bone marrow biopsy, and CD25 were not evaluated in most cases reported as possible COVID‐19‐related HLH, but it is generally a rare condition. 11 To our knowledge, this is the first case of a child with COVID‐19‐related HLH with severe myocardial dysfunction. Our patient met the HLH 2004 Criteria with proven haemophagocytosis in bone marrow aspiration and elevated CD25 level. The heart transplant was unsuccessful due to a relapse of inflammatory status, suggesting the poor prognosis of this condition. 2 , 9
Multisystem inflammatory syndrome in children is usually seen as a delayed consequence of COVID‐19. Most children with this condition had negative PCR but positive SARS‐CoV‐2 serology tests like our case. The factors such as dysregulation of innate immunity, cytokine storm, macrophage activation, and endothelial damage play roles in developing multi‐organ injury, coagulopathy, and immunopathogenesis of COVID‐19‐associated MIS and HLH. 7 , 8 , 11 Cardiac dysfunction is reported commonly in MIS; however, it usually improves over time. In a limited number of patients, the problem has continued or intensified after the first week of treatment. 7 , 12 The aetiology of cardiovascular involvement in the spectrum of MIS‐C can be multifactorial. Overt COVID‐19‐related myocarditis is not as frequent as previously thought, according to histologic studies in adults. 13 There is no histologic data regarding the pattern of cardiac involvement in children with COVID‐19 related to HLH syndrome. In our case, the cardiac magnetic resonance (CMR) showed inflammatory dilated cardiomyopathy with possible focal fibrosis. Histological features were compatible with dilated cardiomyopathy with focal lymphocytic infiltration restricted to the subendocardium. In our patient, the heart transplant took place after a period of immunomodulatory treatment and around 40 days after the onset of the disease, so we assume that the inflammation was subsided. The pathologic feature is more consistent with dilated cardiomyopathy caused by post‐immune‐mediated myocarditis as PCR for the viruse genomes were negative in the myocardium. This is in line with immunopathogenesis of the other organ damages in COVID‐19‐related HLH syndrome. 7 , 10 , 11 LV thrombus formation in our patient could also be result of endothelial disruption combined with hypercoagulation in this scenario. 11 , 14 In a study on paediatric patients with COVID‐19‐related MIS, Theocharis et al. showed common cardiovascular involvement. However, most patients exhibited mild forms of LV dysfunction with no fibrosis in CMR, and some showed a degree of oedema. 15 Latimer et al. reported a 16‐year‐old with COVID‐related thrombocytopenia‐associated multiple organ failure (TAMOF) with moderately reduced LV dysfunction in whom the ejection fraction normalized. 16
There is no established treatment to approach COVID‐related HLH in children. Steroid, IVIG, and anti‐cytokine agents showed some beneficial effects in secondary HLH and COVID‐19‐related MIS‐C. 9 , 17 , 18 There is not sufficient data on the therapeutic approach of persistent cardiac failure following COVID‐19. Whether these patients benefit from heart transplants or not is unknown. Our patient deteriorated early post‐operation due to the heightened systemic inflammation, ARDS, and eventual DIC. Whether the immunosuppressive treatment, including anti‐thymocyte globulin, triggers the recurrence of HLH is not evident. Overall, our experience suggests that COVID‐19‐related HLH with cardiac injury have a poor prognosis.
Conflict of interests
We declare no competing interests.
Funding
No funding to declare.
Supporting information
Figure S1. A) Axial lung CT in a few days post‐transplant with bilateral ground‐glass opacity and consolidation B) developing into bilateral infiltration.
Video S1. Cine 4 chamber showing enlarged ventricles and severely reduced systolic function.
Video S2. Short axis rest perfusion sequenced showing large LV thrombus attached to the mid anterior wall.
Mahdavi, M. , Hejri, G. M. , Pouraliakbar, H. , Shahzadi, H. , Hesami, M. , and Houshmand, G. (2022) Cytokine storm after heart transplantation in COVID‐19‐related haemophagocytic lymphohistiocytosis (HLH). ESC Heart Failure, 9: 219–223. 10.1002/ehf2.13728.
References
- 1. Bansal M. Cardiovascular disease and COVID‐19. Diabetes Metab Syndr Clin Res Rev 2020; 14: 247–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Guo C‐X, He L, Yin J‐Y, Meng X‐G, Tan W, Yang G‐P, Bo T, Liu JP, Lin XJ, Chen X. Epidemiological and clinical features of pediatric COVID‐19. BMC Med 2020; 18: 250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Riphagen S, Gomez X, Gonzalez‐Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID‐19 pandemic. Lancet 2020; 395: 1607–1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Whittaker E, Bamford A, Kenny J, Kaforou M, Jones CE, Shah P, Ramnarayan P, Fraisse A, Miller O, Davies P, Kucera F, Brierley J, McDougall M, Carter M, Tremoulet A, Shimizu C, Herberg J, Burns JC, Lyall H, Levin M, for the PIMS‐TS Study Group and EUCLIDS and PERFORM Consortia . Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS‐CoV‐2. JAMA 2020; 324: 259–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Verdoni L, Mazza A, Gervasoni A, Martelli L, Ruggeri M, Ciuffreda M, Bonanomi E, D'Antiga L. An outbreak of severe Kawasaki‐like disease at the Italian epicentre of the SARS‐CoV‐2 epidemic: an observational cohort study. Lancet 2020. 06; 395: 1771–1778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Davies P, Evans C, Kanthimathinathan HK, Lillie J, Brierley J, Waters G, Johnson M, Griffiths B, du Pré P, Mohammad Z, Deep A, Playfor S, Singh D, Inwald D, Jardine M, Ross O, Shetty N, Worrall M, Sinha R, Koul A, Whittaker E, Vyas H, Scholefield BR, Ramnarayan P. Intensive care admissions of children with paediatric inflammatory multisystem syndrome temporally associated with SARS‐CoV‐2 (PIMS‐TS) in the UK: a multicentre observational study. Lancet Child Adolesc Health 2020; 4: 669–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Alsaied T, Tremoulet AH, Burns JC, Saidi A, Dionne A, Lang SM, Newburger JW, de Ferranti S, Friedman KG. Review of cardiac involvement in multisystem inflammatory syndrome in children. Circulation 2021; 143: 78–88. [DOI] [PubMed] [Google Scholar]
- 8. Jiang L, Tang K, Levin M, Irfan O, Morris SK, Wilson K, Klein JD, Bhutta ZA. COVID‐19 and multisystem inflammatory syndrome in children and adolescents. Lancet Infect Dis 2020; 20: e276–e288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Henter J‐I, Horne A, Aricó M, Egeler RM, Filipovich AH, Imashuku S, Ladisch S, McClain K, Webb D, Winiarski J, Janka G, for the Histiocyte Society . HLH‐2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer 2007; 48: 124–131. [DOI] [PubMed] [Google Scholar]
- 10. Fardet L, Galicier L, Lambotte O, Marzac C, Aumont C, Chahwan D, Coppo P, Hejblum G. Development and validation of the HScore, a score for the diagnosis of reactive hemophagocytic syndrome. Arthritis Rheumatol 2014; 66: 2613–2620. [DOI] [PubMed] [Google Scholar]
- 11. Retamozo S, Brito‐Zerón P, Sisó‐Almirall A, Flores‐Chávez A, Soto‐Cárdenas M‐J, Ramos‐Casals M. Haemophagocytic syndrome and COVID‐19. Clin Rheumatol 2021; 40: 1233–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mahdavi M, Houshmand G, Pouraliakbar H, Mortaz Hejri G. Delayed diffuse inflammatory myocardial damage in a child with a history of systemic inflammatory syndrome related to COVID‐19. Eur Heart J 2021; 42: 1639–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Basso C, Leone O, Rizzo S, De Gaspari M, van der Wal AC, Aubry M‐C, Bois MC, Lin PT, Maleszewski JJ, Stone JR. Pathological features of COVID‐19‐associated myocardial injury: a multicentre cardiovascular pathology study. Eur Heart J 2020; 41: 3827–3835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka F, Moch H. Endothelial cell infection and endotheliitis in COVID‐19. Lancet 2020; 395: 1417–1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Theocharis P, Wong J, Pushparajah K, Mathur SK, Simpson JM, Pascall E, Cleary A, Stewart K, Adhvaryu K, Savis A, Kabir SR. Multimodality cardiac evaluation in children and young adults with multisystem inflammation associated with COVID‐19. Eur Heart J Cardiovasc Imaging [Internet]; 22: 896–903 [cited 2020 Aug 8] Available from: https://academic.oup.com/ehjcimaging/advance‐article/doi/10.1093/ehjci/jeaa212/5882094. Accessed 8 Aug 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Latimer G, Corriveau C, DeBiasi RL, Jantausch B, Delaney M, Jacquot C, Bell M, Dean T. Cardiac dysfunction and thrombocytopenia‐associated multiple organ failure inflammation phenotype in a severe paediatric case of COVID‐19. Lancet Child Adolesc Health 2020; 4: 552–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Belhadjer Z, Auriau J, Méot M, Oualha M, Renolleau S, Houyel L, Bonnet D. Addition of corticosteroids to immunoglobulins is associated with recovery of cardiac function in multi‐inflammatory syndrome in children. Circulation 2020; 142: 2282–2284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Felsenstein S, Willis E, Lythgoe H, McCann L, Cleary A, Mahmood K, Porter D, Jones J, McDonagh J, Chieng A, Varnier G, Hughes S, Boullier M, Ryan F, Awogbemi O, Soda G, Duong P, Pain C, Riley P, Hedrich CM. Presentation, treatment response and short‐term outcomes in paediatric multisystem inflammatory syndrome temporally associated with SARS‐CoV‐2 (PIMS‐TS). JCM 2020; 9: 3293. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. A) Axial lung CT in a few days post‐transplant with bilateral ground‐glass opacity and consolidation B) developing into bilateral infiltration.
Video S1. Cine 4 chamber showing enlarged ventricles and severely reduced systolic function.
Video S2. Short axis rest perfusion sequenced showing large LV thrombus attached to the mid anterior wall.


