Abstract
Objective
To estimate the effectiveness of physical activity monitor (PAM) based interventions among adults and explore reasons for the heterogeneity.
Design
Systematic review and meta-analysis.
Study selection
The electronic databases MEDLINE, Embase, SPORTDiscus, CINAHL, and the Cochrane Central Register of Controlled Trials (CENTRAL) were searched on 4 June 2021. Eligible randomised controlled trials compared interventions in which adults received feedback from PAMs with control interventions in which no feedback was provided. No restrictions on type of outcome measurement, publication date, or language were applied.
Data extraction and synthesis
Two reviewers independently extracted data and assessed risk of bias. Random effects meta-analyses were used to synthesise the results. The certainty of evidence was rated by the Grading of Recommendations Assessment and Evaluation (GRADE) approach.
Main outcome measures
The three primary outcomes of interest were physical activity, moderate to vigorous physical activity, and sedentary time.
Results
121 randomised controlled trials with 141 study comparisons, including 16 743 participants, were included. The PAM based interventions showed a moderate effect (standardised mean difference 0.42, 95% confidence interval 0.28 to 0.55) on physical activity, equivalent to 1235 daily steps; a small effect (0.23, 0.16 to 0.30) on moderate to vigorous physical activity, equivalent to 48.5 weekly minutes; and a small insignificant effect (−0.12, −0.25 to 0.01) on sedentary time, equal to 9.9 daily minutes. All outcomes favoured the PAM interventions.
Conclusions
The certainty of evidence was low for the effect of PAM based interventions on physical activity and moderate for moderate to vigorous physical activity and sedentary time. PAM based interventions are safe and effectively increase physical activity and moderate to vigorous physical activity. The effect on physical activity and moderate to vigorous physical activity is well established but might be overestimated owing to publication bias.
Study registration
PROSPERO CRD42018102719.
Introduction
Physical inactivity, an activity level insufficient to meet current recommendations, has a large impact on global public health, as it is one of the major risk factors for non-communicable diseases and is estimated to be responsible for 9% of all premature deaths globally.1 Physical activity, any bodily movement produced by skeletal muscles that requires energy expenditure,2 has been quantified with physical activity monitors (PAMs) for research purposes for decades.3 However, as well as tracking and measuring physical activity, modern PAMs hold the potential to be used as facilitators for behavioural change, providing direct feedback on physical activity to the user.4 A novel systematic review by Bravata and colleagues in 2007 reported that PAMs could be effectively used to increase physical activity levels among adults.5 However, the number of randomised controlled trials included was low, and the effect estimate was affected by imprecision. Furthermore, several randomised controlled trials have been published since 2007 with different conclusions about the effectiveness of the PAMs. Some trials have reported promising effect sizes,6 7 8 9 10 11 12 some have reported inconclusive results owing to a lack of power or intervention effects,13 14 15 16 17 18 19 and some have reported negative findings on intervention effects.20 21 22 23 24 Even though several systematic reviews have investigated the effectiveness of PAMs, they have all been focused on specific populations or specific types of PAM or have included a limited number of randomised controlled trials.5 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 On the basis of the published literature, PAMs are expected to be effectively increasing physical activity behaviour in general. Nevertheless, as no systematic review has included all available studies, the evidence on the effectiveness of PAM based interventions promoting physical activity among all adults needs to be systematically reviewed according to best practice recommendations from the Cochrane Collaboration to provide high quality guidelines for a diverse audience with an interest in general medicine and public health.47
The objective of this systematic review and meta-analysis was to estimate the effect on physical activity, moderate and vigorous physical activity, and sedentary time from PAM based interventions compared with control interventions in which the participants did not receive feedback from PAMs in participants aged 18-65 years. Subsequently, we examined whether the effectiveness was affected by characteristics of studies and participants.
Methods
This systematic review and meta-analysis was conducted according to the recommendations from Cochrane and is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.47 48 The study protocol holds a detailed description of the methods, has been registered in the PROSPERO database, and has previously been published.49
Eligibility criteria
We included randomised controlled trials and randomised crossover trials. For studies to be considered eligible for inclusion, more than 80% of the study participants had to be above 18 years of age and below 65 years of age. We calculated age distributions by following the methods used by Hall and colleagues.50 We included studies comparing any PAM based intervention in which the participants received feedback on their physical activity level from the PAMs. The PAMs may be portable or wearable, electronic or mechanical, and driven by accelerometers, pedometers, or global positioning systems. In all control interventions, the participants could not receive any feedback on their physical activity level from the PAMs
Outcomes
The three primary outcomes of interest were changes in physical activity, moderate to vigorous physical activity, and sedentary time. If more than one relevant outcome was reported in a study on physical activity, we favoured daily step counts followed by daily metres walked and daily energy expenditure. Finally, if no objective measure was available for physical activity, we used self-reported measures. If more than one relevant outcome was reported in a study on moderate to vigorous physical activity, we favoured objectively measured activity followed by self-reported activity. If more than one relevant outcome was reported in a study on sedentary time, we favoured objectively measured sedentary time followed by self-reported sedentary time. For all three primary outcomes, we used the individual study definitions of physical activity, moderate to vigorous physical activity, and sedentary time. If a study reported only either physical activity or moderate to vigorous physical activity, we included the study results in the specific analysis only for that outcome. We extracted reported adverse events and dropouts.
Search methods for identification of studies
We searched the electronic databases MEDLINE, Embase, SPORTDiscus, CINAHL, and the Cochrane Central Register of Controlled Trials (CENTRAL) on 4 June 2021. The search string combined relevant keywords and MeSH/thesaurus terms for PAMs and study design. The search matrix is reported in the study protocol along with the full search strings.49 We contacted the authors of all unobtainable studies or studies with missing data. We applied no restrictions on language or publication date. Two reviewers (CK and VW) independently used citation pearl growing to hand search references of eligible studies and reviews identified from the search. We searched the database ClinicalTrials.gov to identify ongoing trials. We contacted the study authors of trial protocols if the trial status was uncertain (for example, if the anticipated completion date was overdue but no published study could be identified).
Study selection, data extraction, and risk of bias
A combination of two reviewers (RTL, VW, CBK, CK, JC) independently screened all titles and abstracts of identified studies. At least one of the reviewers assessed the full text of articles judged to be eligible, and consensus on eligibility was reached by discussion. Two reviewers (RTL, VW, CBK, CK, CBJ, JC) independently extracted data and assessed risk of bias using the RoB 2.0 tool.51 Disagreements between reviewers were solved by consulting a third reviewer. To provide the most realistic comparisons, we used the most active control interventions as comparators if more than one control group was available in a study (for example, other non-PAM based behavioural change interventions over usual care interventions over wait list). We imputed median values as means and extracted the standard deviation; estimated it from the standard error, 95% confidence interval, P value, or interquartile range; or measured it on a graph, as recommended by the Cochrane Handbook.52 Studies without any quantification of variance for endpoint scores had standard deviations imputed from baseline measures.
Data synthesis
As described in a previous study protocol,49 we calculated the effect size as a standardised mean difference of the final scores and summarised it using a Hartung-Knapp-Sidik-Jonkman random effects meta-analysis after adjustment to Hedges’ g.53 54 We estimated the risk ratio for adverse events and dropouts, and studies with zero events were given 0.5 events for both the intervention and control group to be included.55 We extracted no follow-up data after the end of intervention scores.
We tested the heterogeneity of results by using the Cochrane Q test and quantified it as I2 values and the between study variance τ2. We assessed small study bias by calculating the Egger’s test score; if this was significant, we used a trim and fill method to adjust for small study bias by removing the studies that caused the small study bias and then imputing missing studies on the bias corrected estimate.56 57 Furthermore, we used a non-parametric Spearman’s rank correlation test to investigate the relation between standardised mean difference and standard error; as a non-protocol defined sensitivity analysis, we used a Copas selection model to investigate the possibility of unpublished trials.58 For all statistical analyses, we considered an α level of 0.05 to be statistically significant. We used RStudio version 1.3.1093, using R version 4.0.3, for all analyses and illustrations.
Subgroup analyses and analysis of heterogeneity
We investigated heterogeneity by doing subgroup analyses and stratified analyses on the following nominal variables: diagnoses, feedback frequency, and content of control intervention (active versus non-active control). The description of these analyses can be found in the study protocol. However, we did not do the protocol defined analyses on type of intervention other than feedback from PAMs (for example, different types of behavioural change intervention or medical interventions related to the specific patient population of individual studies) owing to the complexity of the prevailing classification. We did not do the protocol defined subgroup analyses on whether the participants received feedback on their disease risks according to their physical activity level owing to insufficient data. Two reviewers (JC and RTL) independently rated the certainty of evidence for each outcome by using the Grading of Recommendations Assessment and Evaluation (GRADE) approach (domains used to assess the certainty of the evidence were risk of bias, inconsistency, indirectness, imprecision, and publication bias).59 60 We used the Cochrane rule of thumb (<0.4 interpreted as a small effect, 0.4-0.7 interpreted as a moderate effect, >0.7 interpreted as a large effect) to re-express the standardised mean differences in the summary of findings.61 As a sensitivity approach, we did cumulative meta-analyses to investigate by which year the pooled estimates were positive with at least a clinically relevant small effect (standardised mean difference <0.2 with 95% confidence).62 Another deviation from the study protocol was the use of gross national income per capita as a measure of a country’s economy to explain the heterogeneity of the study results, over the protocol defined use of a country’s gross domestic product. We did this because the World Bank uses gross national income to classify low, lower middle, upper middle, and high income countries.63
Some studies used non-blinded or non-sealed PAMs to assess the study groups during baseline and endpoint weeks. To investigate whether the pooled effect estimates were affected directly by bias due to deviations from the intended control interventions, we did a non-protocol defined sensitivity analysis to analyse whether the control groups were considered to be exposed for feedback from the PAMs.
Patient and public involvement
Because this review did not focus on any specific patient population, no patients were directly involved in setting the research question or the outcome measures or in the design or implementation of the study. No patients were asked to advise on interpretation or writing up of results. However, the members of the research team have worked with physical activity behaviour among different patient populations, which have inspired this review. Patient representatives will be included in the dissemination of results, including the use of lay summaries describing the research and its results for non-scientific audiences.
Results
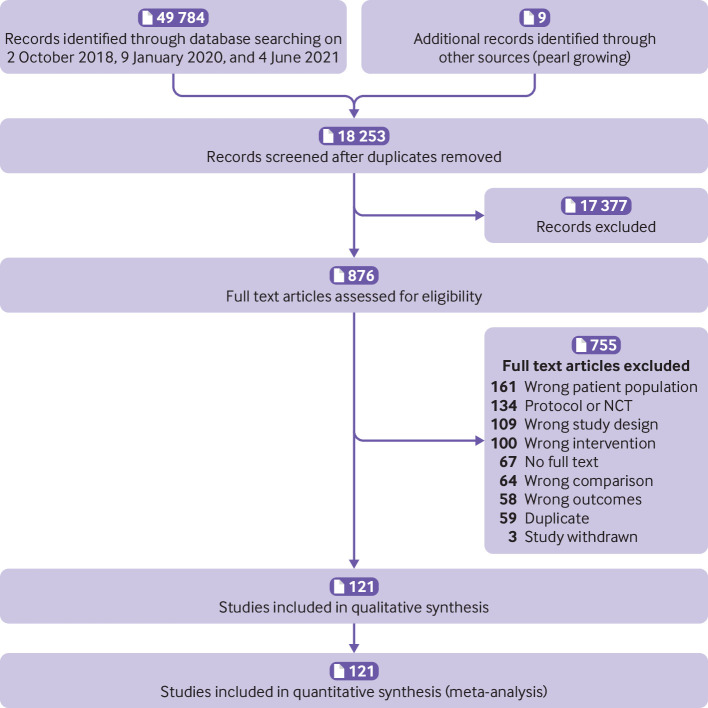
In total, we included 121 studies with 141 study comparisons and 16 743 participants.6 7 8 9 10 11 12 14 15 16 17 18 19 20 21 22 23 24 64 65 66 67 68 69 70 71 72 73 74 75 76 77 78 79 80 81 82 83 84 85 86 87 88 89 90 91 92 93 94 95 96 97 98 99 100 101 102 103 104 105 106 107 108 109 110 111 112 113 114 115 116 117 118 119 120 121 122 123 124 125 126 127 128 129 130 131 132 133 134 135 136 137 138 139 140 141 142 143 144 145 146 147 148 149 150 151 152 153 154 155 156 157 158 159 160 161 162 163 164 165 166 167 The search was conducted on 4 June 2021 and identified 18 253 unique study references. Hand searching of 59 relevant reviews identified five additional studies.71 75 93 106 110 We contacted 105 study authors for obtaining of full text or protocol details, confirmation of trial status, or sharing of preliminary or missing relevant data. The 67 unobtainable studies excluded as “no full text” were conference abstracts, inaccessible trials, or completed trial registrations for which the study report could not be found and the authors did not respond. Figure 1 shows the study selection process and reasons for exclusion in the full text screening.
Fig 1.
PRISMA flow diagram illustrating selection of studies. NCT=National Clinical Trial registry
Characteristics of included studies
All 121 included studies were conducted in high income countries except for eight studies that were conducted in upper middle income countries.12 80 87 104 123 129 150 156 Most of the included studies were European (31%) or North American (40%). Most of the studies were categorised as including mainly healthy participants (47%), followed by studies that reported including overweight participants (17%) and studies that reported including participants with cancer (12%). In total, 62% of the included studies used passive control comparisons, meaning that most of the control groups’ participants received no active intervention content; 81% of the included studies used goal setting for the intervention group participants; and almost all (97%) of the included studies provided daily feedback on physical activity for the intervention group participants. The median duration of intervention among the included studies was 12 weeks. The median baseline daily step count was 6994, and the median body mass index was 27.8. The median age of the participants was 47 years, and the median proportion of female participants was 77%. The median sample size of the included studies was 69. Table 1 summarises the characteristics of the included studies, with detailed summary statistics and references. Appendix 1 provides information about interventions, types of PAM used in the intervention and for measuring outcomes, and further study level characteristics.
Table 1.
Characteristics of included studies
| Characteristics | No (%) of studies (n=121) | No (%) of participants (n=16 743) |
|---|---|---|
| Continent | ||
| Africa123 129 | 2 (2) | 103 (0.6) |
| Asia6 10 79 86 90 102 103 115 131 141 150 154 162 | 14 (12) | 1681 (10.0) |
| Australia7 16 65 70 75 78 108 111 113 114 130 134 146 147 157 165 168 | 15 (12) | 1510 (9.0) |
| Europe8 13 15 18 20 21 23 64 66-69 72 83 88 89 92 97 107 112 116 117 119 121 127 128 135 145 148 149 152 155 158 163 164 166 167 169 170 | 37 (31) | 8047 (48.1) |
| North America9 11 14 17 19 22 24 71 73 74 76 82 84 85 91 94-96 98-101 105 106 109 110 118 120 122 124 125 132 133 136-140 142 143 152 153 159-161 171 172 | 48 (40) | 5071 (30.3) |
| South America12 80 87 104 156 | 5 (4) | 331 (2.0) |
| Population | ||
| Participants with cancer8 22 24 71 76 89 102 106 117 134 141 143 | 14 (12) | 1630 (9.7) |
| Participants with cardiovascular disease90 | 1 (1) | 37 (0.2) |
| Participants with diabetes15 16 78 101 118 122 140 155 162 163 | 10 (8) | 1177 (7.0) |
| Healthy participants6 7 9 10 12 14 19 21 23 64 66-70 75 78 83 85 86 88 93 96 97 100 103 104 107-112 114 119 121 123 128 131 132 136 139 145-148 151 152 154 157-159 172 | 57 (47) | 9103 (54.4) |
| Participants with musculoskeletal disorders72 105 153 161 | 4 (3) | 436 (2.6) |
| Participants with neurological disorders11 124 164 167 | 4 (3) | 399 (2.4) |
| Participants who are overweight18 73 74 82 84 91 92 94 95 98 99 113 115 120 125 127 135 137 138 142 | 20 (17) | 2754 (16.4) |
| Participants with psychiatric disorders130 149 | 2 (2) | 120 (0.7) |
| Participants with pulmonary disorders80 87 116 156 | 2 (2) | 375 (3.3) |
| Participants with other disorders65 129 133 150 166 | 5 (4) | 712 (2.2) |
| Methods | ||
| Active control interventions7 8 10 11 14 16-18 21-24 64 66-68 70 71 73 74 76 78 79 82-86 89 91 93 95 97 100-109 113-115 117 121 122 124 127-133 135-137 140 143 147 149 154 156-158 161 163-167 172 | 46 (38) | 5522 (33.0) |
| Passive control interventions6 9 12 15 19 22 65 69 72 75 80 87 88 90 92 94 96 98 99 110-112 116 118-120 123 125 134 138 139 141-143 145 146 148 150-153 155 158-160 162 168 171 | 75 (62) | 11 221 (67.0) |
| Goal setting7 8 10-12 15-18 21-24 64-67 69-76 78-80 82-89 92-97 99-102 104-108 110-114 118-122 124 125 127-133 135 137-143 145 147 148 150-156 158 160-167 172 | 98 (81) | 14 381 (85.9) |
| No goal setting6 9 14 17 19 22 67 79 90 91 98 103 109 115-117 123 134 136 146 149 158 159 | 23 (19) | 2362 (14.1) |
| Daily feedback6-12 14-24 64-124 126-167 | 117 (97) | 16 451 (98.3) |
| Weekly feedback19 127 | 2 (2) | 209 (1.2) |
| Monthly feedback87 125 | 2 (2) | 83 (0.5) |
| Other characteristics—median (interquartile range) | ||
| Country gross national income per capita (US$; No of studies=121) | 52 448* (42 300-65 118) | |
| Intervention length (weeks; No of studies=121) | 12 (8-12) | |
| Baseline step count (No of studies=59) | 6994 (5158-8230) | |
| Age of participants (years; No of studies=108) | 47.1 (39.0-52.5) | |
| Sex distribution (% of female participants; No of studies=116) | 76.8 (56.4-96.0) | |
| Mean body mass index (No of studies=102) | 27.8 (24.4-30.7) | |
| Median total No of participants (No of studies=121) | 69 (39-152) | |
Equivalent to £38 760 or €46 123
Risk of bias in individual studies
Risk of bias assessments in individual studies, including reasons, are listed in the characteristics of included studies in appendix 1. Figure 2 illustrates the risk of bias for the three outcomes.
Fig 2.
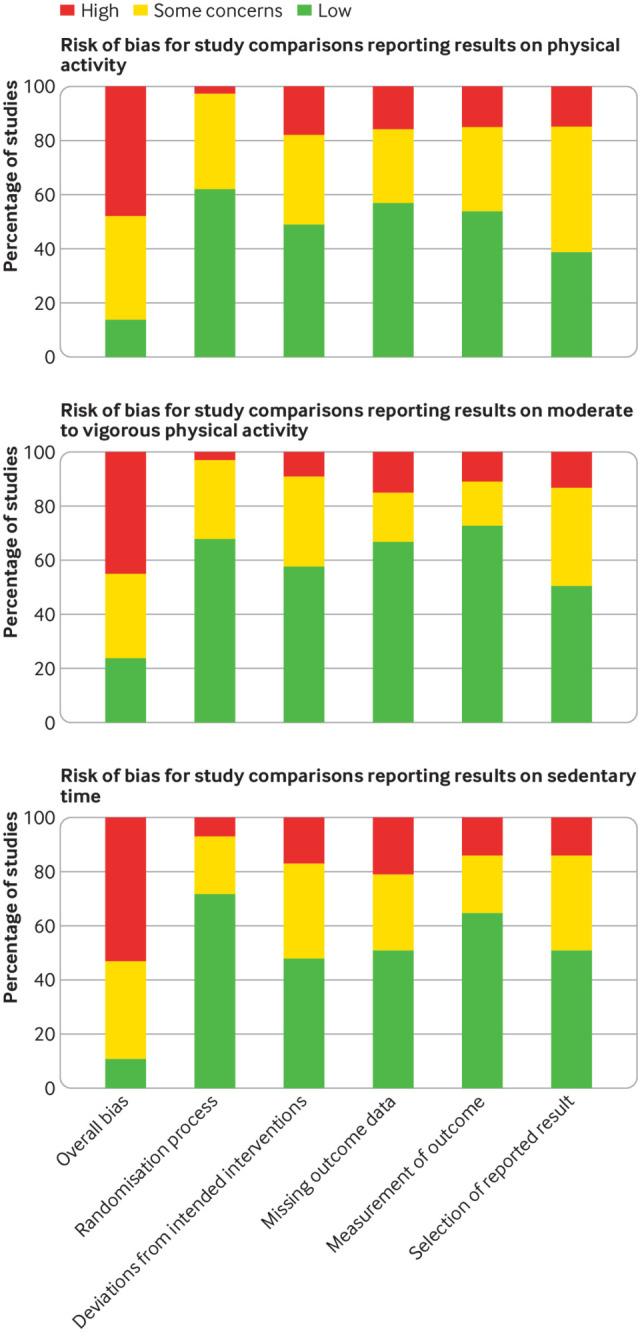
Risk of bias for three outcomes
Effects of interventions on physical activity
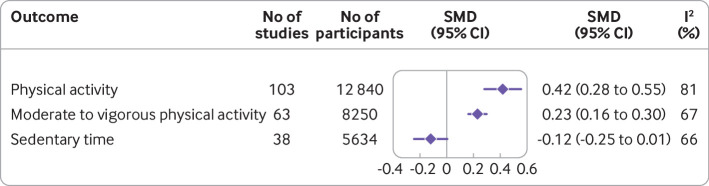
We included 103 studies including results for 12 840 participants in the meta-analysis on physical activity.6 7 8 9 10 11 12 14 15 16 18 19 20 21 22 23 24 64 65 66 67 68 69 73 74 75 76 78 79 80 82 83 85 86 87 88 89 90 91 92 93 94 96 97 98 99 100 101 103 104 106 107 108 109 110 111 112 113 114 115 116 117 118 119 120 121 122 123 124 125 126 128 129 130 131 132 133 134 135 136 137 139 140 141 143 145 146 147 148 150 151 152 153 154 156 158 159 161 162 163 164 167 The overall standardised mean difference was 0.42 (95% confidence interval 0.28 to 0.55; I2=81%) in favour of the PAM interventions. When we transformed the standardised mean difference to a weighted mean difference on daily steps using a median standard deviation of 2940 steps,145 the pooled effect equated to 1235 (95% confidence interval 823 to 1617) daily steps in favour of the intervention. No methodological heterogeneity (whether active or passive control interventions were used; whether objective or self-reported outcome instruments were used; whether goal setting was applied; whether the participants received feedback daily, weekly, or monthly; how long the interventions lasted; what gross national income the study country had; or how the studies were assessed in terms of risk of bias) or clinical heterogeneity (participant population, baseline step count, age of participants, sex distribution of participants, or body mass index of participants) explained the heterogeneity of the results significantly or relevantly. Because of funnel plot asymmetry (positive Eggers’ test, intercept 2.03 (95% confidence interval 1.32 to 2.75)) and, therefore, a risk of small study bias, we applied a trim and fill method in which 36 fictive studies were added, giving an adjusted standardised mean difference of 0.15 (−0.02 to 0.32). A Copas selection model suggested that 69 studies were left unpublished and gave an adjusted standardised mean difference of 0.15 (0.06 to 0.24). A cumulative meta-analysis showed that the standardised mean difference has been significantly larger than 0.25 since 2014. Two comparisons had standard deviations imputed for daily steps,110 165 as did one comparison for weekly walking minutes.91 Three comparisons reported only change scores and were included in the analysis after calculation of the end of treatment standardised mean difference.16 125 Three studies reported results from dichotomous outcomes and were included in the analysis after calculation of the odds ratio and estimation of the individual standardised mean difference.18 89 101
Effects of interventions on moderate to vigorous physical activity
We included 63 studies including results on 8250 participants in the meta-analysis on moderate to vigorous physical activity.7 11 12 15 20 22 23 24 67 69 70 71 72 73 74 76 82 83 84 85 86 87 90 92 93 94 95 97 98 99 100 102 105 106 108 111 114 115 116 117 119 124 126 127 128 132 134 138 142 143 145 146 149 153 155 157 162 163 164 166 167 172 The overall standardised mean difference was 0.23 (0.16 to 0.30; I2=67%) in favour of the PAM interventions. When we transformed the standardised mean difference to a weighted mean difference on weekly minutes of moderate to vigorous physical activity using a median standard deviation of 211 minutes,165 the pooled effect equated to 48.5 (33.8 to 63.3) minutes of moderate to vigorous physical activity in favour of the intervention. The following covariates and risk of bias items explained some of the heterogeneity of the results. Studies using objective outcome instruments for moderate to vigorous physical activity reported a lower standardised mean difference (0.14, 0.06 to 0.22) than did studies using self-reported measures (0.42, 0.22 to 0.62). Studies with low risk of bias arising from the randomisation process were found to have a larger standardised mean difference (0.28, 0.16 to 0.40) than studies with some concerns (0.04, 0.00 to 0.08) and those with high risk of bias (0.17, −3.10 to 3.44). Studies with high risk of bias in selection of the reported results were found to have a lower standardised mean difference (0.05, −0.04 to 0.14) than studies with some concerns (0.31, 0.20 to 0.42) and those with low risk of bias (0.24, 0.09 to 0.38). No other methodological heterogeneity (whether active or passive control interventions were used; whether goal setting was applied; whether the participants received feedback daily, weekly, or monthly; how long the interventions lasted; what gross national income the study country had; or how the studies were assessed in terms of other risk of bias domains) or clinical heterogeneity (participant population, baseline step count, age of participants, sex distribution of participants, or body mass index of participants) explained the heterogeneity of the results significantly or relevantly. Because of funnel plot asymmetry (positive Eggers’ test, intercept 1.00 (0.59 to 1.42)) and the consequent risk of small study bias, we applied a trim and fill method in which 22 fictive studies were added, giving an adjusted standardised mean difference of 0.06 (−0.01 to 0.13). A Copas selection model suggested that 21 studies were left unpublished and gave an adjusted standardised mean difference of 0.10 (0.03 to 0.17). A cumulative meta-analysis showed that the standardised mean difference has been significantly larger than 0.15 since 2016. One comparison had standard deviations imputed for weekly moderate to vigorous physical activity.67 Two comparisons reported only change scores and were included in the analysis after calculation of the end of treatment standardised mean difference.111 142 One study reported results from dichotomous outcomes and was included in the analysis after calculation of the odds ratio and estimation of the individual standardised mean difference.84
Effects of interventions on sedentary time
We included 38 studies including results on 5634 participants in the meta-analysis on sedentary time.13 22 23 64 66 67 70 73 82 87 92 93 94 98 99 103 105 113 114 116 117 119 121 126 127 128 130 143 146 149 152 153 155 157 160 162 163 172 The overall standardised mean difference was −0.12 (−0.25 to 0.01; I2=66%), favouring the PAM intervention as the intervention groups were less sedentary. When we transformed the standardised mean difference to a weighted mean difference of daily sedentary minutes using a median standard deviation of 87.2 minutes, the pooled effect equated to 9.9 (−0.8 to 21.8) daily minutes of sedentary time less in the intervention groups. Participant population groups were found to explain some heterogeneity (P<0.001), primarily driven by the results from studies with overweight participants having an effect size favouring the control interventions (0.11, −0.02 to 0.23) compared with the other participant populations. Country’s gross national income was correlated with the effect of the interventions (coefficient 0.01, 95% confidence interval 0.00 to 0.02) per US$10 000 (£7390; €8794) increase). No other methodological heterogeneity (whether active or passive control interventions were used; whether objective or self-reported outcome instruments were used; whether goal setting was applied; whether the participants received feedback daily, weekly, or monthly; how long the interventions lasted; or how the studies were assessed in terms of risk of bias) or clinical heterogeneity (baseline step count, age of participants, sex distribution of participants, or body mass index of participants) explained the heterogeneity of the results significantly or relevantly. No funnel plot asymmetry, and therefore no risk of small study bias, was found. A cumulative meta-analysis showed that the pooled estimate has been stable around a small effect since 2020. One comparison had standard deviations imputed for weekly sitting minutes.67
Fig 3.
Random effects meta-analysis adjusted to Hedges’ g on effect of interventions on physical activity, moderate to vigorous physical activity, and sedentary time. SMD=standardised mean difference
Appendix 2 shows the forest plots from the random effects meta-analyses. Appendix 3 gives the full results from the subgroup analyses and meta-regressions.
Adverse events and discontinued interventions
With 224 (6.4%) adverse events among 3501 intervention group participants and 186 (5.5%) adverse events among 3355 control group participants, we found no significant association between group allocation when summarising the risk of experiencing an adverse event in 34 studies (relative risk 1.1, 95% confidence interval 0.93 to 1.30; I2=0%). With 931 (10.1%) of 9201 intervention group participants discontinuing the interventions and 713 (8.5%) among 8374 control group participants discontinuing the interventions, we found no significant association between group allocation when summarising the risk of discontinuing interventions in 117 studies (relative risk 1.1, 0.96 to 1.20; I2=16%).
Non-protocol defined sensitivity analyses on whether control group participants were considered to receive feedback from PAMs
We found no effect from whether the control group participants were considered to be exposed for non-blinded PAMs in baseline and endpoint measurement weeks for physical activity and moderate to vigorous physical activity. For sedentary time, the studies in which the control group was considered to receive feedback had a less favourable effect size (0.06, −0.62 to 0.74) than the other studies (−0.14, −0.27 to −0.00).
Summary of findings and risk of bias across studies
The following includes a summary of findings, an effect size interpretation, and a grading of the certainty of evidence (table 2).59 61
Table 2.
Physical activity monitor interventions compared with control interventions—summary of findings
| Outcomes | Anticipated absolute effects* | SMD (95% CI) | No of study comparisons and participants | Certainty of evidence† | Comments |
|---|---|---|---|---|---|
| Physical activity | SMD translates to weighted mean difference of 1235 (95% CI 823 to 1617) daily steps, with more steps in intervention groups | 0.42 (0.28 to 0.55) in favour of intervention | 103 studies; 12 840 participants | Lowठ| None |
| Moderate to vigorous physical activity | SMD translates to weighted mean difference of 48.5 (33.8 to 63.3) minutes weekly MVPA, with more time in intervention groups | 0.23 (0.16 to 0.30) in favour of intervention | 63 studies; 8250 participants | Moderate§ | None |
| Sedentary time | SMD translates to weighted mean difference of 9.9 (−0.8 to 21.8) daily sedentary minutes, with less time in intervention groups | −0.12 (−0.25 to 0.01) | 38 studies; 5634 participants | Moderate | None |
| Adverse events | 224 (6.4%) adverse events among 3501 intervention group participants; 186 (5.5%) adverse events among 3355 control group participants | Relative risk 1.1 (0.93 to 1.30) | 34 studies; 6856 participants | High | No heterogeneity |
| Discontinued intervention (dropout) | 931 (10.2%) of 9201 intervention group participants discontinued interventions; 713 (8.5%) of 9201 control group participants discontinued interventions | Relative risk 1.1 (0.96 to 1.20) | 117 studies; 17 575 participants | High | No heterogeneity |
CI=confidence interval; MVPA=moderate to vigorous physical activity; SMD=standardised mean difference.
Absolute effects are calculated from SMDs and relevant standard deviation, as described in methods section.
Grading of Recommendations Assessment and Evaluation (GRADE) Working Group grades of evidence: high certainty (very confident that true effect lies close to estimate of effect); moderate certainty (moderately confident in effect estimate: true effect is likely to be close to estimate of effect, but possibility that it is substantially different exists); low certainty (confidence in effect estimate is limited: true effect may be substantially different from estimate of effect); very low certainty (very little confidence in effect estimate: true effect is likely to be substantially different from estimate of effect).
Downgraded by one level owing to inconsistency (unexplained heterogeneity).
Downgraded by one level owing to publication bias.
Downgraded by one level owing to imprecision of results.
Physical activity
The standardised mean difference for physical activity of 0.42 (0.28 to 0.55) equates to a moderate effect that translates to a weighted mean difference of 1235 (823 to 1617) daily steps, with more steps in the intervention groups. Certainty in the effect estimate was rated as low. The considerable amount of heterogeneity (I2=81%) could not be explained by any covariates or risk of bias items. Furthermore, the funnel plot asymmetry and findings from the trim and fill method and the Copas selection model suggest an overestimation of the effect, possibly due to publication and small study bias. Therefore, the certainty in the estimate was downgraded owing to inconsistency and the risk of small study bias due to funnel plot asymmetry.
Moderate to vigorous physical activity
The standardised mean difference for moderate to vigorous physical activity of 0.23 (0.16 to 0.30) equates to a small effect that translates to a weighted mean difference of 48.5 (33.8 to 63.3) minutes weekly moderate to vigorous physical activity time more in the intervention groups. Certainty in the effect estimate was rated as moderate. The substantial amount of heterogeneity (I2=67%) was partially explained by outcome instrument type and risk of bias items. As the risk of bias items were counterintuitively explaining heterogeneity (high risk of bias studies reported lower effects), no downgrading due to risk of bias was needed. Furthermore, the funnel plot asymmetry and findings from the trim and fill method and the Copas selection model suggest an overestimation of the effect, possibly due to publication and small study bias. In summary, the certainty was downgraded only owing to risk of small study bias due to funnel plot asymmetry.
Sedentary time
The standardised mean difference for sedentary time of −0.12 (−0.25 to 0.01) equates to a small effect that translates to a weighted mean difference of 9.9 (−0.8 to 21.8) daily sedentary minutes less in the intervention groups. Certainty in the effect estimate was rated as moderate. The overall effect estimate was affected by imprecision, as the upper and lower confidence interval limits represent a large effect and no effect, respectively. The substantial amount of heterogeneity (I2=66%) was partially explained by differences in participant population and country gross national income to a small extent. Thus, the certainty of evidence was downgraded owing to imprecision.
Adverse events and discontinued interventions
For both the risk of adverse events and risk of discontinuing the intervention, no heterogeneity was present. Thus, no downgrading was needed, and the certainty in the evidence was rated high for both outcomes.
Discussion
The finding that PAM based interventions effectively enhance physical activity levels was expected from previous systematic reviews on adult outpatients5; older adults25; overweight participants26; patients with chronic obstructive pulmonary disease,27 28 multiple sclerosis,29 rheumatic or musculoskeletal diseases,30 31 cardiometabolic conditions,32 173 or type 2 diabetes33 34 35; former healthcare patients36; patients in cardiac rehabilitation and with cardiovascular disease37 38; and sedentary adults.39 40 Previously, related systematic reviews have focused on more narrow modalities, such as step counting alone,41 electronic devices or other accelerometers but excluding pedometers,42 43 fitness trackers,44 or PAMs available to consumers.45 Finally, one systematic review has been published with overlapping but not similar aims, which included fewer randomised controlled trials.46 Therefore, this is the first systematic review to summarise the entire body of evidence across different patient populations and different types of PAM. Our finding of a moderate effect on physical activity, equivalent to 1235 (95% confidence interval 823 to 1617) daily steps, and the small effect on moderate to vigorous physical activity, equivalent to 48.5 (33.8 to 63.3) minutes weekly MVPA time, are both clinically relevant. An increase of 1000 daily steps has previously been reported to reduce all cause mortality by 6-36%.174 This association has a non-linear pattern, with the strongest association in people with fewer than 8000 daily steps.175 176 Recent results for moderate to vigorous physical activity show the maximal reduction in risk of mortality to be at around 20-25 minutes of daily moderate to vigorous physical activity.177 These findings support the conclusions of a systematic review investigating associations between mortality and physical activity levels and including individual data for 36 383 participants, in which any physical activity level was associated with a substantially lower risk of mortality compared with the least active group.177 Because of the above, the re-expression of the standardised mean difference for moderate to vigorous physical activity as a small effect might be misleading when the translated effect estimate is close to a third of the recommended level of weekly moderate to vigorous physical activity 2; hence, a small effect on the physical activity behaviour could still very well be highly relevant clinically.
The small effect on sedentary time (−0.12, −0.25 to 0.01), which translates to a weighted mean difference of 9.9 (−0.8 to 21.8) daily sedentary minutes less in the intervention groups, might be found owing to the imprecision of the results. However, even if the estimated effect is close to the true effect size, the result lacks the clinical relevance of physical activity and moderate to vigorous physical activity, as larger effects are probably needed to reduce clinically relevant outcomes significantly.177 178 However, as the strongest inverse correlation between physical activity and sedentary time has been found between light physical activity and sedentary time,179 the lack of effect might be explained by participants increasing their moderate to vigorous physical activity, and thus also their physical activity, when receiving feedback from PAMs. This explanation remains theoretical, as it is outside the aim of this systematic review and meta-analysis. The lack of a clinically relevant effect on sedentary time is still noteworthy, however, as this systematic review cannot support the use of PAMs to reduce sedentary time alone.
Factors affecting expected effect of physical activity monitoring
As seen in the subgroup analyses on physical activity, the standardised mean differences for different methodological factors and across participant populations are somewhat comparable. Thus, no clinical or methodological heterogeneity explained the heterogeneity of the results on physical activity sufficiently, and the moderate effect should be expected in most settings, no matter the population of interest.
For moderate to vigorous physical activity, some heterogeneity was explained by studies using self-reported outcome instruments reporting a larger effect than studies using objective outcome instruments. This could be explained by the questionable validity of commonly used physical activity questionnaires for assessing moderate to vigorous physical activity180; however, as the randomisation should handle any validity imbalances between groups, and thus the endpoint effect size, this explanation remains theoretical and outside the primary aim of this study. Future studies investigating moderate to vigorous physical activity should include objective outcome instruments, as self-reported outcome instruments might overestimate the effects of the intervention. Other explanations for heterogeneity of the results on moderate to vigorous physical activity include risk of bias items. However, as these explanations remain counterintuitive, with low risk of bias studies having larger effects, they are not discussed any further.
For sedentary time, the heterogeneity of the results was explained to a very small degree by studies with higher gross national income having a greater effect; however, as this result is clinically irrelevant (correlation coefficient 0.01 (0.00 to 0.02) per US$10 000 increase), the finding is not discussed any further. Lastly, the heterogeneity of the results on sedentary time was also explained by differences in participant populations, with studies including overweight participants reporting a result favouring the control interventions (0.11, −0.02 to 0.23). This could be due to overweight participants experiencing an ambiguous and even counterproductive influence from feedback from PAMs similar to the findings identified in a small study with young adults with depression or anxiety.181 However, as no explanation was found from the baseline body mass index reported in the included studies, the above finding could also be due to chance alone. For the present, the use of PAMs to reduce sedentary time among overweight participants cannot be supported, and the results should be investigated further in future studies. Finally, however, all of these findings are secondary to the aim of this systematic review and meta-analyses and could, therefore, be due to chance alone.
Publication bias
The effect sizes on physical activity and moderate to vigorous physical activity might both be affected by publication bias and small study bias. The protocol defined trim and fill adjustment added 36 and 22 fictive studies for physical activity and moderate to vigorous physical activity, respectively, and the effect sizes were adjusted to small and clinically irrelevant for physical activity and moderate to vigorous physical activity, respectively. However, an empirical evaluation of the trim and fill adjustment concludes that it might lead to an excessively conservative estimate.58 Because of this, we used the non-protocol defined Copas selection model as an alternative sensitivity analysis and adjustment method to the trim and fill method.182 183 The Copas selection model supported the trim and fill method for both outcomes, but it was not as conservative on moderate to vigorous physical activity as the former alternative. Statistical evaluation and especially correction of small study bias are complex; even though the expected true effect sizes for physical activity and moderate to vigorous physical activity might be overestimated, the results still suggest and support the use of PAM interventions.
Strengths and limitations of study
With its 121 included studies, this study stands as the largest available systematic review and meta-analysis investigating the effect of PAMs on physical activity behaviour. Furthermore, it includes all populations (healthy individuals and patients) and provides precise estimates of the effect sizes for physical activity and moderate to vigorous physical activity. The following limitations should, however, be considered when interpreting the results. Firstly, a substantial amount of heterogeneity was found for all outcomes and explained to some degree only for moderate to vigorous physical activity and sedentary time. Secondly, studies conducted in high income countries are overrepresented, as only eight studies were conducted in non-high income countries, all upper middle income countries.12 80 87 104 123 129 150 156 Consequently, the external validity of our results is limited to high income countries. Thirdly, studies with a high female participation rate are overrepresented, limiting the external validity to female populations. However, as the percentage of female participants in the studies did not explain any heterogeneity, the influence of gender seems to be low. Fourthly, the studies all used objective PAMs as intervention tools but included a variety of physical activity outcome instruments, including self-reported measures (according to appendix 3, 42% of comparisons for physical activity, 45% for moderate to vigorous physical activity, and 48% for sedentary time), which also explained some heterogeneity for moderate to vigorous physical activity. As previously discussed, self-reported outcome measures have a low validity for moderate to vigorous physical activity, which might explain the finding. The inclusion of studies using self-reported measures might limit our results; however, as self-reported measures seem to affect the effect estimate only for moderate to vigorous physical activity, the inclusion could also be seen as a strength for physical activity and sedentary time. Finally, some patient populations appear in only a few studies and thus few participants (cardiovascular, musculoskeletal, neurological, psychiatric, and pulmonary patient populations). This limits the generalisability to these populations, as the effect sizes might be driven by other populations. But as no evidence indicates that these populations will react differently to feedback from PAMs or suggests that they will have negative or unexpected effects, the results should apply equally.
Implications for practice and research
The certainty of the evidence for a moderate effect on physical activity was rated low and could very well be changed by future studies. The effect estimate might also be overestimated owing to publication bias and small study bias. The certainty of the evidence for a small effect on moderate to vigorous physical activity was rated moderate, and it is likely to be close to the true effect. However, the effect estimate might also be overestimated owing to publication bias and small study bias and affected by studies with self-reported instruments reporting larger effects. However, according to the cumulative meta-analysis, the effect estimates on physical activity have been stable for some years, which should inform future studies and encourage comparisons only where needed (for example, large scale studies on physical activity and moderate to vigorous physical activity to avoid small study bias and studies on sedentary time in general and especially among overweight adults).
Even though the effects might be overestimated, clinically relevant effects on physical activity and moderate to vigorous physical activity should be expected when implementing PAMs among healthy or patient populations. These perspectives and recommendations, however, do not apply to studies investigating the effects on sedentary time, as we provide an imprecise effect estimate with low clinical relevance on sedentary time. Because of this, future investigations on sedentary time are encouraged.
In summary, this systematic review and meta-analysis summarises the results of 121 randomised controlled trials and is the first large summary to conclude that although individual studies might show different results, this is most likely due to the expected heterogeneity of the effects among individuals and not because one type of PAM intervention is superior to others. In the future, researchers should investigate how PAMs can be used in combination with other behavioural change contents or how PAMs might affect sedentary time.
Conclusions
This systematic review and meta-analysis identified 121 studies with 141 comparisons investigating the effect of PAMs. We summarise the results from 16 743 unique participants and provide low certainty of evidence for a moderate effect on physical activity equal to 1235 daily steps more, moderate certainty of evidence for a small effect on moderate to vigorous physical activity equal to 48.5 minutes weekly moderate to vigorous physical activity time more, and moderate certainty of evidence for a small but insignificant effect on sedentary time equal to 9.9 daily sedentary minutes less in the intervention groups. Because of the certainty of evidence, future studies could change the overall estimates and are encouraged to investigate how PAMs can be used in combination with other interventions or how PAMs can be used to reduce sedentary time.
What is already known on this topic
Modern physical activity monitors have the potential to be used as facilitators for behavioural change, providing direct feedback on activity to the user
In 2007 a systematic review reported that use of physical activity monitors could increase physical activity, but few studies were included and the effect estimate was affected by imprecision
Since 2007 several studies have been published with different conclusions about the effectiveness of physical activity monitors
What this study adds
This comprehensive and methodologically sound systematic review and meta-analysis summarises the existing body of evidence covering 121 studies, including 16 743 participants
This study provides evidence for using physical activity monitors for enhancing physical activity and moderate to vigorous physical activity
Large scale studies and studies investigating sedentary time in general, especially among overweight participants, are needed to clarify evidence gaps identified here
Acknowledgments
We thank Andreas Lund Hessner for the help with data collection.
Web extra.
Extra material supplied by authors
Web appendix: Appendix 1-3
Contributors: RTL and JC conceived the project. CBJ and HL supervised the work. RTL, JC, and CBJ discussed and planned the analysis. RTL collected the data from online sources, and JC checked this work. VW, CBK, CK, RTL, and JC independently reviewed trials for meeting of inclusion criteria and extracted data. VW contacted corresponding authors by email to request additional data. RTL did the analysis. RTL, JC, and CBJ contributed to the interpretation of results and writing of the discussion section. All authors discussed the results and contributed to the writing and editing of the manuscript. RTL and JC are the guarantors. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: The content presented in this paper was produced as part of the project REACH, which has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement number 690425 (reach2020.eu). The funders had no role in considering the study design, in the collection, analysis, or interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: support from the European Union’s Horizon 2020 research and innovation programme for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
The lead authors (the manuscript’s guarantors) affirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: Results will be disseminated using social media such as LinkedIn, at international conferences such as the Scandinavian Sports Medicine Congress, and to relevant stakeholders at non-profit organisations and within healthcare.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Ethical approval
No individual level data are included in this manuscript. All data are aggregated data from clinical trials.
Data availability statement
The statistical analysis plan and dataset can be available from the corresponding author on reasonable request.
References
- 1. Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT, Lancet Physical Activity Series Working Group . Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012;380:219-29. 10.1016/S0140-6736(12)61031-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. WHO guidelines on physical activity and sedentary behaviour. 2020. https://apps.who.int/iris/handle/10665/336656 [PubMed]
- 3. Stunkard A. A Method of Studying Physical Activity in Man. Am J Clin Nutr 1960;8:595-601. 10.1093/ajcn/8.5.595 [DOI] [Google Scholar]
- 4. Patel MS, Asch DA, Volpp KG. Wearable devices as facilitators, not drivers, of health behavior change. JAMA 2015;313:459-60. 10.1001/jama.2014.14781 [DOI] [PubMed] [Google Scholar]
- 5. Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA 2007;298:2296-304. 10.1001/jama.298.19.2296 [DOI] [PubMed] [Google Scholar]
- 6. Al-Anqodi N, McCullough F, Salter AM. Feasibility of smartphone application to promote physical activity in healthy Omani female adults. Proc Nutr Soc 2018;77. 10.1017/S0029665118001556 [DOI] [Google Scholar]
- 7. Ashton LM, Morgan PJ, Hutchesson MJ, Rollo ME, Collins CE. Feasibility and preliminary efficacy of the ‘HEYMAN’ healthy lifestyle program for young men: a pilot randomised controlled trial. Nutr J 2017;16:2. 10.1186/s12937-017-0227-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Backman M, Wengström Y, Johansson B, et al. A randomized pilot study with daily walking during adjuvant chemotherapy for patients with breast and colorectal cancer. Acta Oncol 2014;53:510-20. 10.3109/0284186X.2013.873820 [DOI] [PubMed] [Google Scholar]
- 9. Eisenberg MH, Phillips LA, Fowler L, Moore PJ. The Impact of E-diaries and Accelerometers on Young Adults’ Perceived and Objectively Assessed Physical Activity. Psychol Sport Exerc 2017;30:55-63. 10.1016/j.psychsport.2017.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kim KA, Hwang SY. [Effects of a Daily Life-Based Physical Activity Enhancement Program for Middle-Aged Women at Risk for Cardiovascular Disease]. J Korean Acad Nurs 2019;49:113-25. 10.4040/jkan.2019.49.2.113 [DOI] [PubMed] [Google Scholar]
- 11. Motl RW, Dlugonski D, Pilutti LA, Klaren RE. Does the effect of a physical activity behavioral intervention vary by characteristics of people with multiple sclerosis? Int J MS Care 2015;17:65-72. 10.7224/1537-2073.2014-016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ribeiro MA, Martins MA, Carvalho CRF. Interventions to increase physical activity in middle-age women at the workplace: a randomized controlled trial. Med Sci Sports Exerc 2014;46:1008-15. 10.1249/MSS.0000000000000190 [DOI] [PubMed] [Google Scholar]
- 13. Ryan JM, Fortune J, Stennett A, et al. Changing physical activity behaviour for people with multiple sclerosis: protocol of a randomised controlled feasibility trial (iStep-MS). BMJ Open 2017;7:e018875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Thompson WG, Koepp GA, Levine JA. Increasing physician activity with treadmill desks. Work 2014;48:47-51. 10.3233/WOR-131708 [DOI] [PubMed] [Google Scholar]
- 15. Whelan ME, Orme MW, Kingsnorth AP, Sherar LB, Denton FL, Esliger DW. Examining the Use of Glucose and Physical Activity Self-Monitoring Technologies in Individuals at Moderate to High Risk of Developing Type 2 Diabetes: Randomized Trial. JMIR Mhealth Uhealth 2019;7:e14195. 10.2196/14195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Peacock AS, Bogossian FE, Wilkinson SA, Gibbons KS, Kim C, McIntyre HD. A Randomised Controlled Trial to Delay or Prevent Type 2 Diabetes after Gestational Diabetes: Walking for Exercise and Nutrition to Prevent Diabetes for You. Int J Endocrinol 2015;2015:423717. 10.1155/2015/423717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Martin SS, Feldman DI, Blumenthal RS, et al. mActive: A Randomized Clinical Trial of an Automated mHealth Intervention for Physical Activity Promotion. J Am Heart Assoc 2015;4:e002239. 10.1161/JAHA.115.002239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Holmes VA, Draffin CR, Patterson CC, et al. PAIGE Study Group . Postnatal Lifestyle Intervention for Overweight Women With Previous Gestational Diabetes: A Randomized Controlled Trial. J Clin Endocrinol Metab 2018;103:2478-87. 10.1210/jc.2017-02654 [DOI] [PubMed] [Google Scholar]
- 19. Eastep E, Beveridge S, Eisenman P, Ransdell L, Shultz B. Does augmented feedback from pedometers increase adults’ walking behavior? Percept Mot Skills 2004;99:392-402. 10.2466/pms.99.2.392-402 [DOI] [PubMed] [Google Scholar]
- 20. Maselli M, Gobbi E, Carraro A. Effectiveness of individual counseling and activity monitors to promote physical activity among university students. J Sports Med Phys Fitness 2019;59:132-40. [DOI] [PubMed] [Google Scholar]
- 21. Reijonsaari K, Vehtari A, Kahilakoski OP, van Mechelen W, Aro T, Taimela S. The effectiveness of physical activity monitoring and distance counseling in an occupational setting - results from a randomized controlled trial (CoAct). BMC Public Health 2012;12:344. 10.1186/1471-2458-12-344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pope ZC, Barr-Anderson DJ, Lewis BA, Pereira MA, Gao Z. Use of wearable technology and social media to improve physical activity and dietary behaviors among college students: A 12-week randomized pilot study. Int J Environ Res Public Health 2019;16:3579. 10.3390/ijerph16193579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Slootmaker SM, Chinapaw MJ, Schuit AJ, Seidell JC, Van Mechelen W. Feasibility and effectiveness of online physical activity advice based on a personal activity monitor: randomized controlled trial. J Med Internet Res 2009;11:e27. 10.2196/jmir.1139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Van Blarigan EL, Chan H, Van Loon K, et al. Self-monitoring and reminder text messages to increase physical activity in colorectal cancer survivors (Smart Pace): a pilot randomized controlled trial. BMC Cancer 2019;19:218. 10.1186/s12885-019-5427-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Larsen RT, Christensen J, Juhl CB, Andersen HB, Langberg H. Physical activity monitors to enhance amount of physical activity in older adults - a systematic review and meta-analysis. Eur Rev Aging Phys Act 2019;16:7. 10.1186/s11556-019-0213-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. de Vries HJ, Kooiman TJM, van Ittersum MW, van Brussel M, de Groot M. Do activity monitors increase physical activity in adults with overweight or obesity? A systematic review and meta-analysis. Obesity (Silver Spring) 2016;24:2078-91. 10.1002/oby.21619 [DOI] [PubMed] [Google Scholar]
- 27. Qiu S, Cai X, Wang X, et al. Using step counters to promote physical activity and exercise capacity in patients with chronic obstructive pulmonary disease: a meta-analysis. Ther Adv Respir Dis 2018;12:1753466618787386. 10.1177/1753466618787386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Armstrong M, Winnard A, Chynkiamis N, Boyle S, Burtin C, Vogiatzis I. Use of pedometers as a tool to promote daily physical activity levels in patients with COPD: a systematic review and meta-analysis. Eur Respir Rev 2019;28:190039. 10.1183/16000617.0039-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rintala A, Hakala S, Paltamaa J, Heinonen A, Karvanen J, Sjögren T. Effectiveness of technology-based distance physical rehabilitation interventions on physical activity and walking in multiple sclerosis: a systematic review and meta-analysis of randomized controlled trials. Disabil Rehabil 2018;40:373-87. 10.1080/09638288.2016.1260649 [DOI] [PubMed] [Google Scholar]
- 30. Mansi S, Milosavljevic S, Baxter GD, Tumilty S, Hendrick P. A systematic review of studies using pedometers as an intervention for musculoskeletal diseases. BMC Musculoskelet Disord 2014;15:231. 10.1186/1471-2474-15-231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Davergne T, Pallot A, Dechartres A, Fautrel B, Gossec L. Use of Wearable Activity Trackers to Improve Physical Activity Behavior in Patients With Rheumatic and Musculoskeletal Diseases: A Systematic Review and Meta-Analysis. Arthritis Care Res (Hoboken) 2019;71:758-67. 10.1002/acr.23752 [DOI] [PubMed] [Google Scholar]
- 32. Kirk MA, Amiri M, Pirbaglou M, Ritvo P. Wearable Technology and Physical Activity Behavior Change in Adults With Chronic Cardiometabolic Disease: A Systematic Review and Meta-Analysis. Am J Health Promot 2019;33:778-91. 10.1177/0890117118816278 [DOI] [PubMed] [Google Scholar]
- 33. Vaes AW, Cheung A, Atakhorrami M, et al. Effect of ‘activity monitor-based’ counseling on physical activity and health-related outcomes in patients with chronic diseases: A systematic review and meta-analysis. Ann Med 2013;45:397-412. 10.3109/07853890.2013.810891 [DOI] [PubMed] [Google Scholar]
- 34. Funk M, Taylor EL. Pedometer-based walking interventions for free-living adults with type 2 diabetes: a systematic review. Curr Diabetes Rev 2013;9:462-71. 10.2174/15733998113096660084 [DOI] [PubMed] [Google Scholar]
- 35. Baskerville R, Ricci-Cabello I, Roberts N, Farmer A. Impact of accelerometer and pedometer use on physical activity and glycaemic control in people with Type 2 diabetes: a systematic review and meta-analysis. Diabet Med 2017;34:612-20. 10.1111/dme.13331 [DOI] [PubMed] [Google Scholar]
- 36. Braakhuis HEM, Berger MAM, Bussmann JBJ. Effectiveness of healthcare interventions using objective feedback on physical activity: A systematic review and meta-analysis. J Rehabil Med 2019;51:151-9. 10.2340/16501977-2522 [DOI] [PubMed] [Google Scholar]
- 37. Hannan AL, Harders MP, Hing W, Climstein M, Coombes JS, Furness J. Impact of wearable physical activity monitoring devices with exercise prescription or advice in the maintenance phase of cardiac rehabilitation: systematic review and meta-analysis. BMC Sports Sci Med Rehabil 2019;11:14. 10.1186/s13102-019-0126-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kanejima Y, Kitamura M, Izawa KP. Self-monitoring to increase physical activity in patients with cardiovascular disease: a systematic review and meta-analysis. Aging Clin Exp Res 2019;31:163-73. 10.1007/s40520-018-0960-7 [DOI] [PubMed] [Google Scholar]
- 39. Qiu S, Cai X, Ju C, et al. Step Counter Use and Sedentary Time in Adults: A Meta-Analysis. Medicine (Baltimore) 2015;94:e1412. 10.1097/MD.0000000000001412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Stephenson A, McDonough SM, Murphy MH, Nugent CD, Mair JL. Using computer, mobile and wearable technology enhanced interventions to reduce sedentary behaviour: a systematic review and meta-analysis. Int J Behav Nutr Phys Act 2017;14:105. 10.1186/s12966-017-0561-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Chaudhry UAR, Wahlich C, Fortescue R, Cook DG, Knightly R, Harris T. The effects of step-count monitoring interventions on physical activity: systematic review and meta-analysis of community-based randomised controlled trials in adults. Int J Behav Nutr Phys Act 2020;17:129. 10.1186/s12966-020-01020-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lewis ZH, Lyons EJ, Jarvis JM, Baillargeon J. Using an electronic activity monitor system as an intervention modality: A systematic review. BMC Public Health 2015;15:585. 10.1186/s12889-015-1947-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Goode AD, Reeves MM, Eakin EG. Telephone-delivered interventions for physical activity and dietary behavior change: an updated systematic review. Am J Prev Med 2012;42:81-8. 10.1016/j.amepre.2011.08.025 [DOI] [PubMed] [Google Scholar]
- 44. Lynch C, Bird S, Lythgo N, Selva-Raj I. Changing the Physical Activity Behavior of Adults With Fitness Trackers: A Systematic Review and Meta-Analysis. Am J Health Promot 2020;34:418-30. 10.1177/0890117119895204 [DOI] [PubMed] [Google Scholar]
- 45. Brickwood K-J, Watson G, O’Brien J, Williams AD. Consumer-Based Wearable Activity Trackers Increase Physical Activity Participation: Systematic Review and Meta-Analysis. JMIR Mhealth Uhealth 2019;7:e11819. 10.2196/11819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hakala S, Rintala A, Immonen J, Karvanen J, Heinonen A, Sjögren T. Effectiveness of physical activity promoting technology-based distance interventions compared to usual care. Systematic review, meta-analysis and meta-regression. Eur J Phys Rehabil Med 2017;53:953-67. 10.23736/S1973-9087.17.04585-3 [DOI] [PubMed] [Google Scholar]
- 47.Higgins JPT, Thomas J, Chandler J, et al, eds. Cochrane Handbook for Systematic Reviews of Interventions. 2021. https://training.cochrane.org/handbook/current.
- 48. Shamseer L, Moher D, Clarke M, et al. PRISMA-P Group . Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;350:g7647. 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- 49. Larsen RT, Wagner V, Keller C, Juhl CB, Langberg H, Christensen J. Feedback from physical activity monitors to enhance amount of physical activity in adults-a protocol for a systematic review and meta-analysis. Syst Rev 2019;8:53. 10.1186/s13643-019-0970-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hall M, Juhl CB, Lund H, Thorlund JB. Knee Extensor Muscle Strength in Middle-Aged and Older Individuals Undergoing Arthroscopic Partial Meniscectomy: A Systematic Review and Meta-Analysis. Arthritis Care Res (Hoboken) 2015;67:1289-96. 10.1002/acr.22581 [DOI] [PubMed] [Google Scholar]
- 51. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 52.Higgins JPT, Thomas J, Chandler J, et al, eds. Cochrane Handbook for Systematic Reviews of Interventions: Chapter 5: Collecting data. 2021. https://training.cochrane.org/handbook/current/chapter-05.
- 53. IntHout J, Ioannidis JP, Borm GF. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med Res Methodol 2014;14:25. 10.1186/1471-2288-14-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Lin L, Aloe AM. Evaluation of various estimators for standardized mean difference in meta-analysis. Stat Med 2021;40:403-26. 10.1002/sim.8781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Friedrich JO, Adhikari NKJ, Beyene J. Inclusion of zero total event trials in meta-analyses maintains analytic consistency and incorporates all available data. BMC Med Res Methodol 2007;7:5. 10.1186/1471-2288-7-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000;56:455-63. 10.1111/j.0006-341X.2000.00455.x [DOI] [PubMed] [Google Scholar]
- 57.Higgins JPT, Thomas J, Chandler J, et al, eds. Cochrane Handbook for Systematic Reviews of Interventions: Chapter 10: Addressing reporting biases. 2011. https://handbook-5-1.cochrane.org/chapter_10/10_4_4_2_trim_and_fill.htm.
- 58. Schwarzer G, Carpenter J, Rücker G. Empirical evaluation suggests Copas selection model preferable to trim-and-fill method for selection bias in meta-analysis. J Clin Epidemiol 2010;63:282-8. 10.1016/j.jclinepi.2009.05.008 [DOI] [PubMed] [Google Scholar]
- 59. Guyatt GH, Oxman AD, Vist GE, et al. GRADE Working Group . GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924-6. 10.1136/bmj.39489.470347.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schünemann H, Brożek J, Guyatt G, Oxman A. GRADE Handbook. 2013. http://gdt.guidelinedevelopment.org/central_prod/_design/client/handbook/handbook.html#h.1i2bwkm8zpjo.
- 61.Higgins JPT, Thomas J, Chandler J, et al, eds. Cochrane Handbook for Systematic Reviews of Interventions: Chapter 12: Interpreting results and drawing conclusions. 2011. https://handbook-5-1.cochrane.org/chapter_12/12_6_2_re_expressing_smds_using_rules_of_thumb_for_effect_sizes.htm.
- 62.Higgins JPT, Thomas J, Chandler J, et al, eds. Cochrane Handbook for Systematic Reviews of Interventions: Chapter 22: Prospective approaches to accumulating evidence. 2021. https://training.cochrane.org/handbook/current/chapter-22#section-22-4-2.
- 63.World Bank. World Bank Country and Lending Groups. 2020. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
- 64. Aittasalo M, Rinne M, Pasanen M, Kukkonen-Harjula K, Vasankari T. Promoting walking among office employees - evaluation of a randomized controlled intervention with pedometers and e-mail messages. BMC Public Health 2012;12:403. 10.1186/1471-2458-12-403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Armit CM, Brown WJ, Marshall AL, et al. Randomized trial of three strategies to promote physical activity in general practice. Prev Med 2009;48:156-63. 10.1016/j.ypmed.2008.11.009 [DOI] [PubMed] [Google Scholar]
- 66. Arrogi A, Bogaerts A, Seghers J, et al. Evaluation of stAPP: a smartphone-based intervention to reduce prolonged sitting among Belgian adults. Health Promot Int 2019;34:16-27. 10.1093/heapro/dax046 [DOI] [PubMed] [Google Scholar]
- 67. Baker G, Gray SR, Wright A, et al. Scottish Physical Activity Research Collaboration (SPARColl) . The effect of a pedometer-based community walking intervention “Walking for Wellbeing in the West” on physical activity levels and health outcomes: a 12-week randomized controlled trial. Int J Behav Nutr Phys Act 2010;7:51. 10.1186/1479-5868-7-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Baker G, Mutrie N, Lowry R. A comparison of goals set in steps using a pedometer and goals set in minutes: a randomized controlled trial. Int J Health Promot Educ 2011;49:60-8. 10.1080/14635240.2011.10708210 . [DOI] [Google Scholar]
- 69. Baker G, Mutrie N, Lowry R. Using pedometers as motivational tools: Are goals set in steps more effective than goals set in minutes for increasing walking? Int J Health Promot Educ 2008;46:21-6. 10.1080/14635240.2008.10708123 . [DOI] [Google Scholar]
- 70. Barwais FA, Cuddihy TF, Tomson LM. Physical activity, sedentary behavior and total wellness changes among sedentary adults: a 4-week randomized controlled trial. Health Qual Life Outcomes 2013;11:183. 10.1186/1477-7525-11-183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Basen-Engquist K, Taylor CLC, Rosenblum C, et al. Randomized pilot test of a lifestyle physical activity intervention for breast cancer survivors. Patient Educ Couns 2006;64:225-34. 10.1016/j.pec.2006.02.006 [DOI] [PubMed] [Google Scholar]
- 72. Berglind D, Yacaman-Mendez D, Lavebratt C, Forsell Y. The Effect of Smartphone Apps Versus Supervised Exercise on Physical Activity, Cardiorespiratory Fitness, and Body Composition Among Individuals With Mild-to-Moderate Mobility Disability: Randomized Controlled Trial. JMIR Mhealth Uhealth 2020;8:e14615. 10.2196/14615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Biddle SJH, Edwardson CL, Wilmot EG, et al. A Randomised Controlled Trial to Reduce Sedentary Time in Young Adults at Risk of Type 2 Diabetes Mellitus: Project STAND (Sedentary Time ANd Diabetes). PLoS One 2015;10:e0143398. 10.1371/journal.pone.0143398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Bond DS, Vithiananthan S, Thomas JG, et al. Bari-Active: a randomized controlled trial of a preoperative intervention to increase physical activity in bariatric surgery patients. Surg Obes Relat Dis 2015;11:169-77. 10.1016/j.soard.2014.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Butler L, Dwyer D. Pedometers may not provide a positive effect on walking activity. Health Promot J Austr 2004;2004:134-6. 10.1071/HE04134 [DOI] [Google Scholar]
- 76. Cadmus-Bertram L, Tevaarwerk AJ, Sesto ME, Gangnon R, Van Remortel B, Date P. Building a physical activity intervention into clinical care for breast and colorectal cancer survivors in Wisconsin: a randomized controlled pilot trial. J Cancer Surviv 2019;13:593-602. 10.1007/s11764-019-00778-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Carr LJ, Karvinen K, Peavler M, Smith R, Cangelosi K. Multicomponent intervention to reduce daily sedentary time: a randomised controlled trial. BMJ Open 2013;3:e003261. 10.1136/bmjopen-2013-003261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Cheung NW, Blumenthal C, Smith BJ, et al. A Pilot Randomised Controlled Trial of a Text Messaging Intervention with Customisation Using Linked Data from Wireless Wearable Activity Monitors to Improve Risk Factors Following Gestational Diabetes. Nutrients 2019;11:E590. 10.3390/nu11030590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Cheung P, Chen S. Emmy Man Yee Wong. Using Mobile Phone Messages in Pedometer-Based Intervention for Working Adults in Hong Kong. Asian J Exerc Sports Sci 2012;9:76-85. [Google Scholar]
- 80. Coelho CM, Reboredo MM, Valle FM, et al. Effects of an unsupervised pedometer-based physical activity program on daily steps of adults with moderate to severe asthma: a randomized controlled trial. J Sports Sci 2018;36:1186-93. 10.1080/02640414.2017.1364402 [DOI] [PubMed] [Google Scholar]
- 81. Cooper AJ, Dearnley K, Williams KM, et al. Protocol for Get Moving: a randomised controlled trial to assess the effectiveness of three minimal contact interventions to promote fitness and physical activity in working adults. BMC Public Health 2015;15:296. 10.1186/s12889-015-1654-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Creel DB, Schuh LM, Reed CA, et al. A randomized trial comparing two interventions to increase physical activity among patients undergoing bariatric surgery. Obesity (Silver Spring) 2016;24:1660-8. 10.1002/oby.21548 [DOI] [PubMed] [Google Scholar]
- 83. Dadaczynski K, Schiemann S, Backhaus O. Promoting physical activity in worksite settings: results of a German pilot study of the online intervention Healingo fit. BMC Public Health 2017;17:696. 10.1186/s12889-017-4697-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Dicken-Kano R, Bell MM. Pedometers as a means to increase walking and achieve weight loss. J Am Board Fam Med 2006;19:524-5. 10.3122/jabfm.19.5.524 [DOI] [PubMed] [Google Scholar]
- 85. DuVall C, Dinger MK, Taylor EL, Bemben D. Minimal-contact physical activity interventions in women: a pilot study. Am J Health Behav 2004;28:280-6. 10.5993/AJHB.28.3.9 [DOI] [PubMed] [Google Scholar]
- 86. Finkelstein EA, Haaland BA, Bilger M, et al. Effectiveness of activity trackers with and without incentives to increase physical activity (TRIPPA): a randomised controlled trial. Lancet Diabetes Endocrinol 2016;4:983-95. 10.1016/S2213-8587(16)30284-4 [DOI] [PubMed] [Google Scholar]
- 87. Freitas PD, Silva AG, Ferreira PG, et al. Exercise Improves Physical Activity and Comorbidities in Obese Adults with Asthma. Med Sci Sports Exerc 2018;50:1367-76. 10.1249/MSS.0000000000001574 [DOI] [PubMed] [Google Scholar]
- 88. Glynn LG, Hayes PS, Casey M, et al. Effectiveness of a smartphone application to promote physical activity in primary care: the SMART MOVE randomised controlled trial. Br J Gen Pract 2014;64:e384-9 . 10.3399/bjgp14X680461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Gokal K, Wallis D, Ahmed S, Boiangiu I, Kancherla K, Munir F. Effects of a self-managed home-based walking intervention on psychosocial health outcomes for breast cancer patients receiving chemotherapy: a randomised controlled trial. Support Care Cancer 2016;24:1139-66. 10.1007/s00520-015-2884-5 [DOI] [PubMed] [Google Scholar]
- 90. Goto M, Takedani H, Haga N, et al. Self-monitoring has potential for home exercise programmes in patients with haemophilia. Haemophilia 2014;20:e121-7. 10.1111/hae.12355 [DOI] [PubMed] [Google Scholar]
- 91. Greene J, Sacks R, Piniewski B, Kil D, Hahn JS. The impact of an online social network with wireless monitoring devices on physical activity and weight loss. J Prim Care Community Health 2013;4:189-94. 10.1177/2150131912469546 [DOI] [PubMed] [Google Scholar]
- 92. Grey EB, Thompson D, Gillison FB. Effects of a Web-Based, Evolutionary Mismatch-Framed Intervention Targeting Physical Activity and Diet: a Randomised Controlled Trial. Int J Behav Med 2019;26:645-57. 10.1007/s12529-019-09821-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Hardeman W, Mitchell J, Pears S, et al. VBI Research Team . Evaluation of a very brief pedometer-based physical activity intervention delivered in NHS Health Checks in England: The VBI randomised controlled trial. PLoS Med 2020;17:e1003046. 10.1371/journal.pmed.1003046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Harrington DM, Champagne CM, Broyles ST, Johnson WD, Tudor-Locke C, Katzmarzyk PT. Steps ahead: a randomized trial to reduce unhealthy weight gain in the Lower Mississippi Delta. Obesity (Silver Spring) 2014;22:E21-8. 10.1002/oby.20684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Hartman SJ, Nelson SH, Cadmus-Bertram LA, Patterson RE, Parker BA, Pierce JP. Technology- and Phone-Based Weight Loss Intervention: Pilot RCT in Women at Elevated Breast Cancer Risk. Am J Prev Med 2016;51:714-21. 10.1016/j.amepre.2016.06.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Hultquist CN, Albright C, Thompson DL. Comparison of walking recommendations in previously inactive women. Med Sci Sports Exerc 2005;37:676-83. 10.1249/01.MSS.0000158993.39760.1B [DOI] [PubMed] [Google Scholar]
- 97. Hurling R, Catt M, Boni MD, et al. Using internet and mobile phone technology to deliver an automated physical activity program: randomized controlled trial. J Med Internet Res 2007;9:e7. 10.2196/jmir.9.2.e7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Jakicic JM, Davis KK, Rogers RJ, et al. Effect of Wearable Technology Combined With a Lifestyle Intervention on Long-term Weight Loss: The IDEA Randomized Clinical Trial. JAMA 2016;316:1161-71. 10.1001/jama.2016.12858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Katzmarzyk PT, Champagne CM, Tudor-Locke C, et al. A short-term physical activity randomized trial in the Lower Mississippi Delta. PLoS One 2011;6:e26667. 10.1371/journal.pone.0026667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Kendzor DE, Allicock M, Businelle MS, Sandon LF, Gabriel KP, Frank SG. Evaluation of a Shelter-Based Diet and Physical Activity Intervention for Homeless Adults. J Phys Act Health 2017;14:88-97. 10.1123/jpah.2016-0343 [DOI] [PubMed] [Google Scholar]
- 101. Kim C, Draska M, Hess ML, Wilson EJ, Richardson CR. A web-based pedometer programme in women with a recent history of gestational diabetes. Diabet Med 2012;29:278-83. 10.1111/j.1464-5491.2011.03415.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Kim JY, Lee MK, Lee DH, et al. Effects of a 12-week home-based exercise program on quality of life, psychological health, and the level of physical activity in colorectal cancer survivors: a randomized controlled trial. Support Care Cancer 2019;27:2933-40. 10.1007/s00520-018-4588-0 [DOI] [PubMed] [Google Scholar]
- 103. Kitagawa T, Higuchi Y, Todo E, Ueda T, Ando S, Murakami T. Tailored feedback reduced prolonged sitting time and improved the health of housewives: a single-blind randomized controlled pilot study. Women Health 2020;60:212-2 . 10.1080/03630242.2019.1616043 [DOI] [PubMed] [Google Scholar]
- 104. Kovelis D, Zabatiero J, Furlanetto KC, Mantoani LC, Proença M, Pitta F. Short-term effects of using pedometers to increase daily physical activity in smokers: a randomized trial. Respir Care 2012;57:1089-97. 10.4187/respcare.01458 [DOI] [PubMed] [Google Scholar]
- 105. Li LC, Sayre EC, Xie H, Clayton C, Feehan LM. A Community-Based Physical Activity Counselling Program for People With Knee Osteoarthritis: Feasibility and Preliminary Efficacy of the Track-OA Study. JMIR Mhealth Uhealth 2017;5:e86. 10.2196/mhealth.7863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Ligibel JA, Meyerhardt J, Pierce JP, et al. Impact of a telephone-based physical activity intervention upon exercise behaviors and fitness in cancer survivors enrolled in a cooperative group setting. Breast Cancer Res Treat 2012;132:205-13. 10.1007/s10549-011-1882-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Long JE, Ring C, Bosch JA, et al. A life-style physical activity intervention and the antibody response to pneumococcal vaccination in women. Psychosom Med 2013;75:774-82. 10.1097/PSY.0b013e3182a0b664 [DOI] [PubMed] [Google Scholar]
- 108. Mansi S, Milosavljevic S, Tumilty S, Hendrick P, Higgs C, Baxter DG. Investigating the effect of a 3-month workplace-based pedometer-driven walking programme on health-related quality of life in meat processing workers: a feasibility study within a randomized controlled trial. BMC Public Health 2015;15:410. 10.1186/s12889-015-1736-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Matevey C, Rogers LQ, Dawson E, et al. Lack of Reactivity During Pedometer Self-Monitoring in Adults. Meas Phys Educ Exerc Sci 2006;10:1-11. 10.1207/s15327841mpee1001_1 [DOI] [Google Scholar]
- 110. Melton BF, Buman MP, Vogel RL, et al. Wearable Devices to Improve Physical Activity and Sleep: A Randomized Controlled Trial of College-Aged African American Women. J Black Stud 2016;47:610-25. 10.1177/0021934716653349 [DOI] [Google Scholar]
- 111. Merom D, Rissel C, Phongsavan P, et al. Promoting walking with pedometers in the community: the step-by-step trial. Am J Prev Med 2007;32:290-7. 10.1016/j.amepre.2006.12.007 [DOI] [PubMed] [Google Scholar]
- 112. Miragall M, Domínguez-Rodríguez A, Navarro J, Cebolla A, Baños RM. Increasing physical activity through an Internet-based motivational intervention supported by pedometers in a sample of sedentary students: A randomised controlled trial. Psychol Health 2018;33:465-82. 10.1080/08870446.2017.1368511 [DOI] [PubMed] [Google Scholar]
- 113. Morgan PJ, Callister R, Collins CE, et al. The SHED-IT community trial: a randomized controlled trial of internet- and paper-based weight loss programs tailored for overweight and obese men. Ann Behav Med 2013;45:139-52. 10.1007/s12160-012-9424-z [DOI] [PubMed] [Google Scholar]
- 114. Murawski B, Plotnikoff RC, Rayward AT, et al. Efficacy of an m-Health Physical Activity and Sleep Health Intervention for Adults: A Randomized Waitlist-Controlled Trial. Am J Prev Med 2019;57:503-14. 10.1016/j.amepre.2019.05.009 [DOI] [PubMed] [Google Scholar]
- 115. Nakata Y, Sasai H, Tsujimoto T, Hashimoto K, Kobayashi H. Web-based intervention to promote weight-loss maintenance using an activity monitor: A randomized controlled trial. Prev Med Rep 2019;14:100839. 10.1016/j.pmedr.2019.100839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Obling KH, Overgaard K, Juul L, Maindal HT. Effects of a motivational, individual and locally anchored exercise intervention (MILE) on cardiorespiratory fitness: a community-based randomised controlled trial. BMC Public Health 2019;19:239. 10.1186/s12889-019-6556-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Ormel HL, van der Schoot GGF, Westerink NL, Sluiter WJ, Gietema JA, Walenkamp AME. Self-monitoring physical activity with a smartphone application in cancer patients: a randomized feasibility study (SMART-trial). Support Care Cancer 2018;26:3915-23. 10.1007/s00520-018-4263-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Paschali AA, Goodrick GK, Kalantzi-Azizi A, Papadatou D, Balasubramanyam A. Accelerometer feedback to promote physical activity in adults with type 2 diabetes: a pilot study. Percept Mot Skills 2005;100:61-8. 10.2466/pms.100.1.61-68 [DOI] [PubMed] [Google Scholar]
- 119. Pears S, Bijker M, Morton K, et al. VBI Programme Team . A randomised controlled trial of three very brief interventions for physical activity in primary care. BMC Public Health 2016;16:1033. 10.1186/s12889-016-3684-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Pellegrini CA, Verba SD, Otto AD, Helsel DL, Davis KK, Jakicic JM. The comparison of a technology-based system and an in-person behavioral weight loss intervention. Obesity (Silver Spring) 2012;20:356-63. 10.1038/oby.2011.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Petersen CB, Severin M, Hansen AW, Curtis T, Grønbæk M, Tolstrup JS. A population-based randomized controlled trial of the effect of combining a pedometer with an intervention toolkit on physical activity among individuals with low levels of physical activity or fitness. Prev Med 2012;54:125-30. 10.1016/j.ypmed.2011.12.012 [DOI] [PubMed] [Google Scholar]
- 122. Piette JD, Richardson C, Himle J, et al. A randomized trial of telephonic counseling plus walking for depressed diabetes patients. Med Care 2011;49:641-8. 10.1097/MLR.0b013e318215d0c9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Pillay JD, Kolbe-Alexander TL, Proper KI, et al. Steps that count! A feasibility study of a pedometer-based, health-promotion intervention in an employed, South African population. South Afr Sports Med Assoc 2014;26:15-19. 10.7196/SAJSM.500 [DOI] [Google Scholar]
- 124. Plow M, Finlayson M, Liu J, Motl RW, Bethoux F, Sattar A. Randomized Controlled Trial of a Telephone-Delivered Physical Activity and Fatigue Self-management Interventions in Adults With Multiple Sclerosis. Arch Phys Med Rehabil 2019;100:2006-14. . 10.1016/j.apmr.2019.04.022 [DOI] [PubMed] [Google Scholar]
- 125. Polzien KM, Jakicic JM, Tate DF, Otto AD. The efficacy of a technology-based system in a short-term behavioral weight loss intervention. Obesity (Silver Spring) 2007;15:825-30. 10.1038/oby.2007.584 [DOI] [PubMed] [Google Scholar]
- 126. Pope ZC, Zeng N, Zhang R, Lee HY, Gao Z. Effectiveness of Combined Smartwatch and Social Media Intervention on Breast Cancer Survivor Health Outcomes: A 10-Week Pilot Randomized Trial. J Clin Med 2018;7:E140. 10.3390/jcm7060140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Poston L, Briley AL, Barr S, et al. Developing a complex intervention for diet and activity behaviour change in obese pregnant women (the UPBEAT trial); assessment of behavioural change and process evaluation in a pilot randomised controlled trial. BMC Pregnancy Childbirth 2013;13:148. 10.1186/1471-2393-13-148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Recio-Rodriguez JI, Agudo-Conde C, Martin-Cantera C, et al. EVIDENT Investigators . Short-Term Effectiveness of a Mobile Phone App for Increasing Physical Activity and Adherence to the Mediterranean Diet in Primary Care: A Randomized Controlled Trial (EVIDENT II Study). J Med Internet Res 2016;18:e331. 10.2196/jmir.6814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Roos R, Myezwa H, van Aswegen H, Musenge E. Effects of an education and home-based pedometer walking program on ischemic heart disease risk factors in people infected with HIV: a randomized trial. J Acquir Immune Defic Syndr 2014;67:268-76. 10.1097/QAI.0000000000000299 [DOI] [PubMed] [Google Scholar]
- 130. Rosenbaum S, Sherrington C, Tiedemann A. Exercise augmentation compared with usual care for post-traumatic stress disorder: a randomized controlled trial. Acta Psychiatr Scand 2015;131:350-9. 10.1111/acps.12371 [DOI] [PubMed] [Google Scholar]
- 131. Alshahrani A, Siddiqui A, Khalil S, et al. WhatsApp-based intervention for promoting physical activity among female college students, Saudi Arabia: a randomized controlled trial. East Mediterr Health J 2021;27:782-9. 10.26719/emhj.21.012 [DOI] [PubMed] [Google Scholar]
- 132. Sharp P, Caperchione C. The effects of a pedometer-based intervention on first-year university students: A randomized control trial. J Am Coll Health 2016;64:630-8. 10.1080/07448481.2016.1217538 [DOI] [PubMed] [Google Scholar]
- 133. Sheshadri A, Kittiskulnam P, Lazar AA, Johansen KL. A Walking Intervention to Increase Weekly Steps in Dialysis Patients: A Pilot Randomized Controlled Trial. Am J Kidney Dis 2020;75:488-96. 10.1053/j.ajkd.2019.07.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Singh B, Spence RR, Sandler CX, Tanner J, Hayes SC. Feasibility and effect of a physical activity counselling session with or without provision of an activity tracker on maintenance of physical activity in women with breast cancer - A randomised controlled trial. J Sci Med Sport 2020;23:283-90. 10.1016/j.jsams.2019.09.019 [DOI] [PubMed] [Google Scholar]
- 135. Sniehotta FF, Evans EH, Sainsbury K, et al. Behavioural intervention for weight loss maintenance versus standard weight advice in adults with obesity: A randomised controlled trial in the UK (NULevel Trial). PLoS Med 2019;16:e1002793. 10.1371/journal.pmed.1002793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Spence JC, Burgess J, Rodgers W, Murray T. Effect of pretesting on intentions and behaviour: a pedometer and walking intervention. Psychol Health 2009;24:777-89. 10.1080/08870440801989938 [DOI] [PubMed] [Google Scholar]
- 137. Staudter M, Dramiga S, Webb L, Hernandez D, Cole R. Effectiveness of pedometer use in motivating active duty and other military healthcare beneficiaries to walk more. US Army Med Dep J 2011;108-19. [PubMed] [Google Scholar]
- 138. Thomas JG, Raynor HA, Bond DS, et al. Weight loss in Weight Watchers Online with and without an activity tracking device compared to control: A randomized trial. Obesity (Silver Spring) 2017;25:1014-21. 10.1002/oby.21846 [DOI] [PubMed] [Google Scholar]
- 139. Thorndike AN, Mills S, Sonnenberg L, et al. Activity monitor intervention to promote physical activity of physicians-in-training: randomized controlled trial. PLoS One 2014;9:e100251. 10.1371/journal.pone.0100251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Tudor-Locke C, Bell RC, Myers AM, et al. Controlled outcome evaluation of the First Step Program: a daily physical activity intervention for individuals with type II diabetes. Int J Obes Relat Metab Disord 2004;28:113-9. 10.1038/sj.ijo.0802485 [DOI] [PubMed] [Google Scholar]
- 141. Uhm KE, Yoo JS, Chung SH, et al. Effects of exercise intervention in breast cancer patients: is mobile health (mHealth) with pedometer more effective than conventional program using brochure? Breast Cancer Res Treat 2017;161:443-52. 10.1007/s10549-016-4065-8 [DOI] [PubMed] [Google Scholar]
- 142. Unick JL, O’Leary KC, Bond DS, Wing RR. Physical activity enhancement to a behavioral weight loss program for severely obese individuals: A preliminary investigation. ISRN Obes 2012;2012. 10.5402/2012/465158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Vallance JK, Courneya KS, Plotnikoff RC, Yasui Y, Mackey JR. Randomized controlled trial of the effects of print materials and step pedometers on physical activity and quality of life in breast cancer survivors. J Clin Oncol 2007;25:2352-9. 10.1200/JCO.2006.07.9988 [DOI] [PubMed] [Google Scholar]
- 144. Vallance JK, Friedenreich CM, Lavallee CM, et al. Exploring the Feasibility of a Broad-Reach Physical Activity Behavior Change Intervention for Women Receiving Chemotherapy for Breast Cancer: A Randomized Trial. Cancer Epidemiol Biomarkers Prev 2016;25:391-8. 10.1158/1055-9965.EPI-15-0812 [DOI] [PubMed] [Google Scholar]
- 145. Van Hoye K, Wijtzes AI, Lefevre J, De Baere S, Boen F. Year-round effects of a four-week randomized controlled trial using different types of feedback on employees’ physical activity. BMC Public Health 2018;18:492. 10.1186/s12889-018-5402-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Vandelanotte C, Duncan MJ, Maher CA, et al. The Effectiveness of a Web-Based Computer-Tailored Physical Activity Intervention Using Fitbit Activity Trackers: Randomized Trial. J Med Internet Res 2018;20:e11321. 10.2196/11321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Wallbank G, Sherrington C, Canning CG, et al. Active women over 50: study protocol for RCT of a low-dose information and support program to promote physical activity behaviour change. BMC Public Health 2019;19:1225. 10.1186/s12889-019-7514-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Walsh JC, Corbett T, Hogan M, Duggan J, McNamara A. An mHealth Intervention Using a Smartphone App to Increase Walking Behavior in Young Adults: A Pilot Study. JMIR Mhealth Uhealth 2016;4:e109. 10.2196/mhealth.5227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Williams J, Stubbs B, Richardson S, et al. ‘Walk this way’: results from a pilot randomised controlled trial of a health coaching intervention to reduce sedentary behaviour and increase physical activity in people with serious mental illness. BMC Psychiatry 2019;19:287. 10.1186/s12888-019-2274-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Omar NO, Ahmad RA, Mohd Shah MS, Aminuddin AA, Chellappan KC. Amelioration of inflammation in young men with cardiovascular risks participating pedometer-based walking programme. Med J Malaysia 2021;76:375-81. [PubMed] [Google Scholar]
- 151. Poirier J, Bennett WL, Jerome GJ, et al. Effectiveness of an Activity Tracker- and Internet-Based Adaptive Walking Program for Adults: A Randomized Controlled Trial. J Med Internet Res 2016;18:e34. 10.2196/jmir.5295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Anderson AS, Chong HY, Craigie AM, et al. A novel approach to increasing community capacity for weight management a volunteer-delivered programme (ActWELL) initiated within breast screening clinics: a randomised controlled trial. Int J Behav Nutr Phys Act 2021;18:34. 10.1186/s12966-021-01099-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Li LC, Feehan LM, Xie H, et al. Efficacy of a Physical Activity Counseling Program With Use of a Wearable Tracker in People With Inflammatory Arthritis: A Randomized Controlled Trial. Arthritis Care Res (Hoboken) 2020;72:1755-65. 10.1002/acr.24199 [DOI] [PubMed] [Google Scholar]
- 154. Kong S, Lee JK, Kang D, et al. Comparing the Effectiveness of a Wearable Activity Tracker in Addition to Counseling and Counseling Only to Reinforce Leisure-Time Physical Activity among Breast Cancer Patients: A Randomized Controlled Trial. Cancers (Basel) 2021;13:2692. 10.3390/cancers13112692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Haufe S, Kahl KG, Kerling A, et al. Employers With Metabolic Syndrome and Increased Depression/Anxiety Severity Profit Most From Structured Exercise Intervention for Work Ability and Quality of Life. Front Psychiatry 2020;11:562. 10.3389/fpsyt.2020.00562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Freitas PD, Passos NFP, Carvalho-Pinto RM, et al. A Behavior Change Intervention Aimed at Increasing Physical Activity Improves Clinical Control in Adults With Asthma: A Randomized Controlled Trial. Chest 2021;159:46-57. 10.1016/j.chest.2020.08.2113 [DOI] [PubMed] [Google Scholar]
- 157. Rayward AT, Murawski B, Duncan MJ, et al. Efficacy of an m-Health Physical Activity and Sleep Intervention to Improve Sleep Quality in Middle-Aged Adults: The Refresh Study Randomized Controlled Trial. Ann Behav Med 2020;54:470-83. 10.1093/abm/kaz064 [DOI] [PubMed] [Google Scholar]
- 158. Hajna S, Sharp SJ, Cooper AJM, et al. Effectiveness of Minimal Contact Interventions: An RCT. Am J Prev Med 2021;60:e111-21. 10.1016/j.amepre.2020.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Farnell G, Barkley J. The effect of a wearable physical activity monitor (Fitbit One) on physical activity behaviour in women: A pilot study. J Hum Sport Exerc 2017;12. 10.14198/jhse.2017.124.09 [DOI] [Google Scholar]
- 160. Kim H, Kang M. A Tailored Domain-specific Intervention Using Contextual Information about Sedentary Behavior to Reduce Sedentary Time: A Bayesian Approach. Meas Phys Educ Exerc Sci 2021;25:171-9. 10.1080/1091367X.2020.1862123 [DOI] [Google Scholar]
- 161. Lang AE, Hendrick PA, Clay L, et al. A randomized controlled trial investigating effects of an individualized pedometer driven walking program on chronic low back pain. BMC Musculoskelet Disord 2021;22:206. 10.1186/s12891-021-04060-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Yang Y-P, Wang C-J, Wang J-J, et al. The Effects of an Activity Promotion System on active living in overweight subjects with metabolic abnormalities. Obes Res Clin Pract 2017;11:718-27. 10.1016/j.orcp.2017.06.002 [DOI] [PubMed] [Google Scholar]
- 163. Peacock OJ, Western MJ, Batterham AM, et al. Effect of novel technology-enabled multidimensional physical activity feedback in primary care patients at risk of chronic disease - the MIPACT study: a randomised controlled trial. Int J Behav Nutr Phys Act 2020;17:99. 10.1186/s12966-020-00998-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Ryan JM, Fortune J, Stennett A, et al. Safety, feasibility, acceptability and effects of a behaviour-change intervention to change physical activity behaviour among people with multiple sclerosis: Results from the iStep-MS randomised controlled trial. Mult Scler 2020;26:1907-18. 10.1177/1352458519886231 [DOI] [PubMed] [Google Scholar]
- 165. Singh B, Spence RR, Sandler CX, Tanner J, Hayes SC. Feasibility and effect of a physical activity counselling session with or without provision of an activity tracker on maintenance of physical activity in women with breast cancer - A randomised controlled trial. J Sci Med Sport 2020;23:283-90. 10.1016/j.jsams.2019.09.019 [DOI] [PubMed] [Google Scholar]
- 166. Taylor A, Taylor RS, Ingram W, et al. Randomised controlled trial of an augmented exercise referral scheme using web-based behavioural support for inactive adults with chronic health conditions: the e-coachER trial. Br J Sports Med 2021;55:444-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Nasseri NN, Ghezelbash E, Zhai Y, et al. Feasibility of a smartphone app to enhance physical activity in progressive MS: a pilot randomized controlled pilot trial over three months. PeerJ 2020;8:e9303. 10.7717/peerj.9303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Teychenne M, Abbott G, Stephens LD, et al. Mums on the Move: A pilot randomised controlled trial of a home-based physical activity intervention for mothers at risk of postnatal depression. Midwifery 2021;93:102898. 10.1016/j.midw.2020.102898 [DOI] [PubMed] [Google Scholar]
- 169. Sandborg J, Söderström E, Henriksson P, et al. Effectiveness of a Smartphone App to Promote Healthy Weight Gain, Diet, and Physical Activity During Pregnancy (HealthyMoms): Randomized Controlled Trial. JMIR Mhealth Uhealth 2021;9:e26091. 10.2196/26091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Herman HG, Kleiner I, Tairy D, et al. 623: Improving post-Cesarean mobility with personalized feedback using digital step counters - a randomized controlled trial. Am J Obstet Gynecol 2020;222:S397-8. 10.1016/j.ajog.2019.11.639 [DOI] [PubMed] [Google Scholar]
- 171. Levin ME, Krafft J, Seifert S, Lillis J. Tracking Valued and Avoidant Functions with Health Behaviors: A Randomized Controlled Trial of the Acceptance and Commitment Therapy Matrix Mobile App. Behav Modif 2022;46:63-89. 10.1177/0145445520913987 [DOI] [PubMed] [Google Scholar]
- 172. Carr LJ, Karvinen K, Peavler M, Smith R, Cangelosi K. Multicomponent intervention to reduce daily sedentary time: a randomised controlled trial. BMJ Open 2013;3:e003261. 10.1136/bmjopen-2013-003261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Hodkinson A, Kontopantelis E, Adeniji C, et al. Accelerometer- and Pedometer-Based Physical Activity Interventions Among Adults With Cardiometabolic Conditions: A Systematic Review and Meta-analysis. JAMA Netw Open 2019;2:e1912895. 10.1001/jamanetworkopen.2019.12895 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 174. Hall KS, Hyde ET, Bassett DR, et al. Systematic review of the prospective association of daily step counts with risk of mortality, cardiovascular disease, and dysglycemia. Int J Behav Nutr Phys Act 2020;17:78. 10.1186/s12966-020-00978-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Hansen BH, Dalene KE, Ekelund U, et al. Step by step: Association of device-measured daily steps with all-cause mortality-A prospective cohort Study. Scand J Med Sci Sports 2020;30:1705-11. 10.1111/sms.13726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Saint-Maurice PF, Troiano RP, Bassett DR, Jr, et al. Association of Daily Step Count and Step Intensity With Mortality Among US Adults. JAMA 2020;323:1151-60. 10.1001/jama.2020.1382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Ekelund U, Tarp J, Steene-Johannessen J, et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: systematic review and harmonised meta-analysis. BMJ 2019;366:l4570. 10.1136/bmj.l4570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Rees-Punia E, Evans EM, Schmidt MD, et al. Mortality Risk Reductions for Replacing Sedentary Time With Physical Activities. Am J Prev Med 2019;56:736-41. 10.1016/j.amepre.2018.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179. Mansoubi M, Pearson N, Biddle SJH, Clemes S. The relationship between sedentary behaviour and physical activity in adults: a systematic review. Prev Med 2014;69:28-35. 10.1016/j.ypmed.2014.08.028 [DOI] [PubMed] [Google Scholar]
- 180. Lee PH, Macfarlane DJ, Lam TH, Stewart SM. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act 2011;8:115. 10.1186/1479-5868-8-115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Kanstrup AM, Bertelsen P, Jensen MB. Contradictions in digital health engagement: An activity tracker’s ambiguous influence on vulnerable young adults’ engagement in own health. Digit Health 2018;4:2055207618775192. 10.1177/2055207618775192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Copas J. What works?: selectivity models and meta-analysis. J R Stat Soc Ser A Stat Soc 1999;162:95-109. 10.1111/1467-985X.00123 [DOI] [Google Scholar]
- 183. Copas JB, Shi JQ. A sensitivity analysis for publication bias in systematic reviews. Stat Methods Med Res 2001;10:251-65. 10.1177/096228020101000402 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Appendix 1-3
Data Availability Statement
The statistical analysis plan and dataset can be available from the corresponding author on reasonable request.