Abstract
Wireless epidermal devices (WEDs), based on UHF radio frequency identification (RFID), enable a contactless and noninvasive human body monitoring through sampling of health parameters directly on the skin. With reference to body temperature, this letter reports an experimental campaign aimed at assessing the degree of agreement of a battery-less plaster-like WED, placed in the armpit region, with a standard axilla thermocouple thermometer. A measurement campaign over 10 volunteers, for overall 120 temperature outcomes, revealed a good correlation among the instruments (Person's coefficient p = 0.78) and a difference of less than 0.6 °C in the 95% of the measured cases, provided that a user-calibration is applied. RFID-WED enables a noncontacting reading up to 20 cm and direct connectivity with a cloud architecture. Envisaged applications are the periodic monitoring in clinical and domestic scenarios, as well as the screening of restricted communities related to COVID-19 control and recovery.
Keywords: Sensor applications, body temperature, epidermal electronics, radio frequency identification (RFID)
I. Introduction
Body core temperature is a key wellness parameter related to many physio-pathological conditions. The COVID-19 emergency is currently focusing even more attention on body temperature [1], [2] since the reorganization of activities in safe conditions requires prompt identification of the onset of febrile states that are related to infections and virus outbreak. The gold standard for its measurement is invasive since it requires the insertion of a thermal probe into natural or surgical central body cavities. Less intrusive methods, that find practical and domestic application, estimate the core temperature through much easier on-skin measurements. They are typically performed on the forehead or in the ear canal with a thermal camera or infrared thermometers, under the armpit or in the oral cavity with expansion or thermocouple-based thermometers. These methodologies are fairly simple to implement, and the measurement times span from a few seconds in the first cases up to a few minutes [3].
The possibility to capture the skin temperature by means of wireless epidermal devices (WEDs) attached to the patient has been very recently explored in [5]–[8]. They are made of a thin conformable, bio-compatible, and breathable membrane hosting an antenna and an integrated circuit (IC) with additional system-oriented capabilities. IC simultaneously acts as a pn-junction temperature sensor as well as a communication transponder. When energized from remote, a WED transmits back the collected data by means of the radio frequency identification (RFID) standard, in either the NFC (13.56 MHz) [5] or UHF (860–960 MHz) [6]–[8] band. Once gently attached to the user's skin, it stays functional for several days and even weeks. As batteries are not required to get an instantaneous reading, the device can be low-profile, low-cost, and less harmful for the environment. Cattery-assisted-passive configurations can be adopted for continuous monitoring [6] without a reader. Preliminary tests in controlled conditions revealed that UHF WEDs can guarantee accuracy in the skin temperature measurement of 0.2 °C in comparison with a precise thermocouple [9]. Unlike the NFC devices [5] (see Table 2 for further details), UHF WEDs can be interrogated up to 1.5 m [8], provided that at least a 3 × 3 cm antenna is used. Accordingly, they are potential candidates to merge the accuracy and reliability of an axillary thermometer [10] with a noncontacting reading procedure.
Table 2. Comparison Between WED and Other Skin Thermometers.
| Cost [$] | Read range | User identif. | Precision /accuracy | Environ. effect | |
|---|---|---|---|---|---|
| WED | (scan) 200–500 | 20 cm | yes | 0.3/0.6 °C | Low |
| eWTS[5] | \ | 1-3 cm | yes | 0.08 °C | Low |
| Infrared | 100 | 10 cm | no | 0.2 °C | High |
| Th.Cam | 15,000 | 1–2 m | perhaps | ±1 °C | Medium |
In this letter, we experimentally evaluate the reliability of UHF WEDs to reproduce the measurements of a standard axilla electronic thermometer through tests over volunteers in realistic conditions. The goal is to derive the most appropriate sensor placement, the measurement procedure (see Section II), and the evaluation of the degree of accuracy with the axillary thermometer starting from rough data, as well by introducing a user-specific calibration (see Section III).
II. Instrumentations and Methods
A. Armpit RFID Passive Sensor
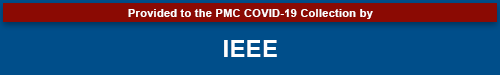
The considered WED thermometer (see Fig. 1) is derived from the antenna layout in [8] having removed the booster wire for purposes of miniaturization. It is a multilayer soft UHF RFID tag that comprises an 11 ×8 mm2 rectangular loop-antenna provided with a sensing-oriented RFID IC (Axzon Magnus-S3). The loop is a 10-μm aluminum trace etched on a 50-μm-thick polyethylene substrate [see Fig. 1(b)] that is sandwiched between two layers of 1-mm-thick biocompatible silicone. The entire device is encapsulated within a thin (220 μm) adhesive non-woven sterile medical-grade fabric plaster (BSN Medical - Fixomull Stretch) for a comfortable and robust bond with the skin. The WED is intended to be used only on healthy skin. Moreover, while the plaster is disposable, the core loop module can be removed and reused several times by the same user with new plasters, provided that cleaning and disinfection procedures are correctly performed. Finally, the absence of battery and other leaky components makes the WED extremely safe against skin injuries risk.
Fig. 1.
WED plaster for skin temperature sensing. (a) Exploded view, (b) RF module, and (c) encapsulated prototype within a sterile medical plaster.
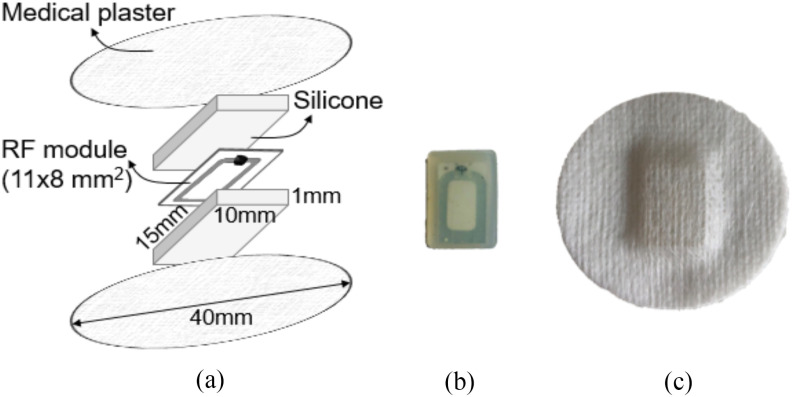
The reduced size with respect to [8] and the placement in the armpit region made the WED suitable to be read up to 20 cm [see Fig. 3(a)] by a circular polarized reader's antenna emitting 3.2 W EIRP. Such distance enabled comfortable reads in all the following tests, even when the tag was fully covered by the forearm. Longer distances would require a wire booster around the loop, as in [8], at the price of enlarging the size of the antenna. Accordingly, a different placement site, like the torso, should be considered.
Fig. 3.
(a) Example of the received signal strength indicator (RSSI) of the reader by varying the distance from the tag. RSSI considerably drops for d > 25 cm, thus, making the communication unstable. (b) Temperature profiles (RFID sensor and reference thermocouple probe) measured for 35 min in case of two positions of the arm (relaxed down and 45° tilted).
To get rid of manufacturing uncertainties, sensors were preliminarily calibrated at the same ambient temperature.
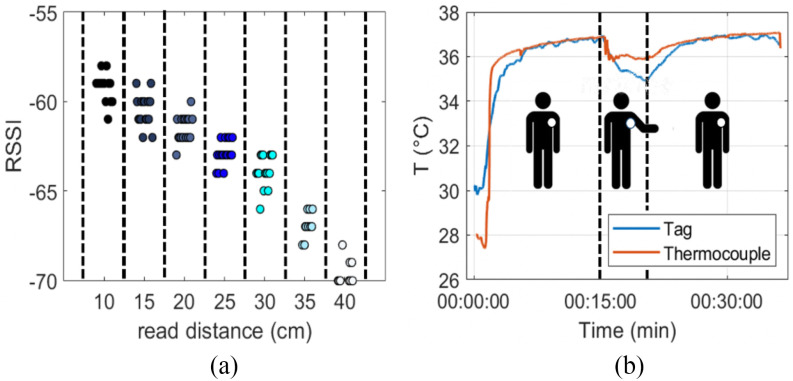
B. Measurement Set-Up
The interrogation system comprises a Jadak UsbPro reader connected to a circularly polarized patch antenna (radiated power EIRP = 3.2 W @ 867 MHz) that are both integrated into a totem-like stand (see Fig. 2). The reader is controlled by a personal computer running a custom software for data acquisition, processing, and visualization. Following a guided procedure, the user is asked 1) to be identified (inventory), 2) to take and insert the reference armpit temperature TA by means of a digital electronic thermometer (Chicco Digi Baby, Artsana SpA, range 32–42.9 °C, accuracy: ±0.1 °C within 35.5–42.0 °C and ±0.2 °C outside that range, precision: ±0.2 °C (experimentally retrieved over 20 measurements), and finally, 3) to collect the RFID tag temperature Ttag by means of interrogation of the WED thermometer. An audio feedback helps the user to stay close enough to the totem (< 20 cm) to get the data. The returned Ttag data are the average over 12 samples having drop out the lowest and the highest values. Then, a power-based correction as in [9] is applied to account for the nonlinearity of the pn-junction temperature sensor onboard the IC as a consequence of the user-specific relative position w.r.t. the reader. Five WED measurements are sequentially taken by the testbed for averaging during approximately 30 s.
Fig. 2.
WED placement in the armpit and measurement set-up.
C. Volunteers
The experimental campaign involved 10 healthy volunteers (four males, six females, 25≤age≤50, body mass index 17.7≤BMI ≤27.2) and was carried out in July 2020 in the Pervasive Electromagnetic Lab of the University of Rome “Tor Vergata.” Each volunteer wore the sensor under the armpit. No control over clothes was exerted. Overall, 120 measures have been recorded during 2–3 days of use.
D. Impact of Measurement Time
The time the RFID WED thermometer needs to achieve the thermal equilibrium with the armpit and accordingly to provide meaningful data was preliminarily estimated for one of the volunteers (age = 28 BMI = 19.8, in Fig. 2) by a transient measurement. A k-type probe thermocouple placed in the same body position and sampled by a 16-bit data acquisition device (MonoDAQ-U-X by DEWESoft) was used for comparison.
Measurement started immediately after the sensors had been attached in the armpit [see Fig. 3(b)]. After less than 5 min (IC time constant in [11]), the two temperatures converged to equilibrium. Lifting the arm at a  produced a decrease of
produced a decrease of  in 5 min, probably due to air flow in the armpit area. Once the arm was put back again, the temperature recovered the previous stable value in nearly 5 min. Hence, in order to obtain reliable data, the forearm must adhere to the body for at least 5 min before the RFID interrogation.
in 5 min, probably due to air flow in the armpit area. Once the arm was put back again, the temperature recovered the previous stable value in nearly 5 min. Hence, in order to obtain reliable data, the forearm must adhere to the body for at least 5 min before the RFID interrogation.
E. Impact of Position
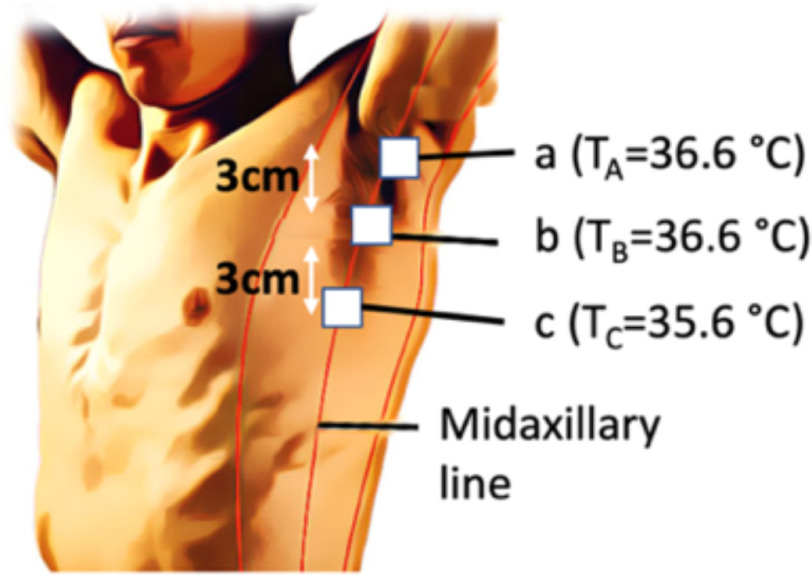
To assess the variability of the RFID sensor response with the placement on the axilla area, three different positions along the midaxillary line were considered for the same volunteer as above (see Fig. 4). The reference value provided by the electronic thermometer was collected in position a. When the sensor was placed too far from the axilla cavity (position c), up to 1 °C temperature difference was measured. Accordingly, the sensor must be attached in position a or b.
Fig. 4.
Temperatures from the WED thermometer placed at three different positions under the axilla. (a) Cavity (0 cm), b) middle (3 cm), and c) basis (6 cm). The reference temperature by the electronic thermometer in position a) was TA = 36.6 °C.
F. Impact of Clothing and External Temperature
The impact of the clothing on the measurement was evaluated with respect to position b (more susceptible than position a to airflow and external temperature). The volunteer was asked to wear a thick cotton coat and then, in a different test, a light undershirt. Measurements were taken indoor (TE = 28.7 °C) and outdoor (TE = 37.7 °C). Results in Table 1 demonstrate the repeatability of the measurements regardless of the clothing and the environmental conditions, with less than 0.2 °C discrepancy among data (comparable with the accuracy of the reference thermometer).
Table 1. Output of the RFID Sensor for Different Clothes and Environmental Temperatures.
| TE (°C) | 28.7 | 37.7 | |||
|---|---|---|---|---|---|
| Clothes | Shirt | Coat | Shirt | Coat | |
| Ttag (°C) | 35.9 ± 0.1 | 35.9 ± 0.1 | 36.0 ± 0.1 | 36.1 ± 0.1 | |
| Ref. (°C) | 36.2 | 36.2 | 36.2 | 36.4 | |
III. Campaign Results
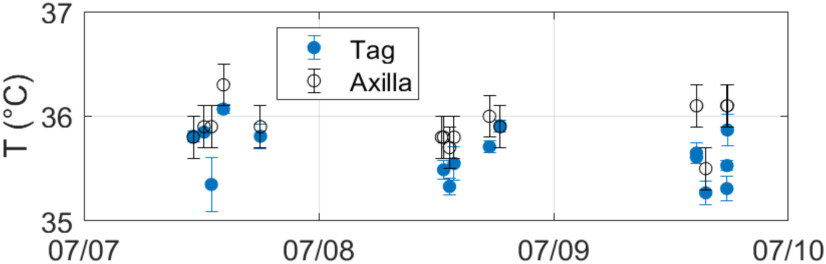
Fig. 5 shows an example of the temperature profile of the same volunteer as above, which was taken along a couple of days by the RFID system and compared with the electronic axilla thermometer. The two datasets are in reasonable agreement with an average difference value  and a standard deviation
and a standard deviation 
Fig. 5.
Examples of measured data from a volunteer taken along three days w.r.t. the digital axillary thermometer.
A. Data Processing
The whole dataset of the ten volunteers was then processed to derive the accuracy of the system with respect to the reference. Temperature samples lower than 35 °C were considered artifacts and discarded [12]. Accordingly, the collected useful data fall in the 35–37.5 °C range.
Data points are distributed [see Fig. 6(a)] along the ideal diagonal line with a Pearson correlation coefficient p = 0.48 between RFID measurements and reference. The relative cumulative distribution function [see Fig. 6(b)] of the difference  among the two datasets shows that there is better than 0.5 °C agreement in 60% of the cases. The Bland–Altman diagram [12] [see Fig. 6(c)] returns a bias
among the two datasets shows that there is better than 0.5 °C agreement in 60% of the cases. The Bland–Altman diagram [12] [see Fig. 6(c)] returns a bias  and a standard deviation
and a standard deviation  so that there is a ±1 °C degree of agreement within a 95% limit of confidence in the whole considered temperature range. The regression line is nearly horizontal so that the bias can be considered almost stable in the explored range.
so that there is a ±1 °C degree of agreement within a 95% limit of confidence in the whole considered temperature range. The regression line is nearly horizontal so that the bias can be considered almost stable in the explored range.
Fig. 6.
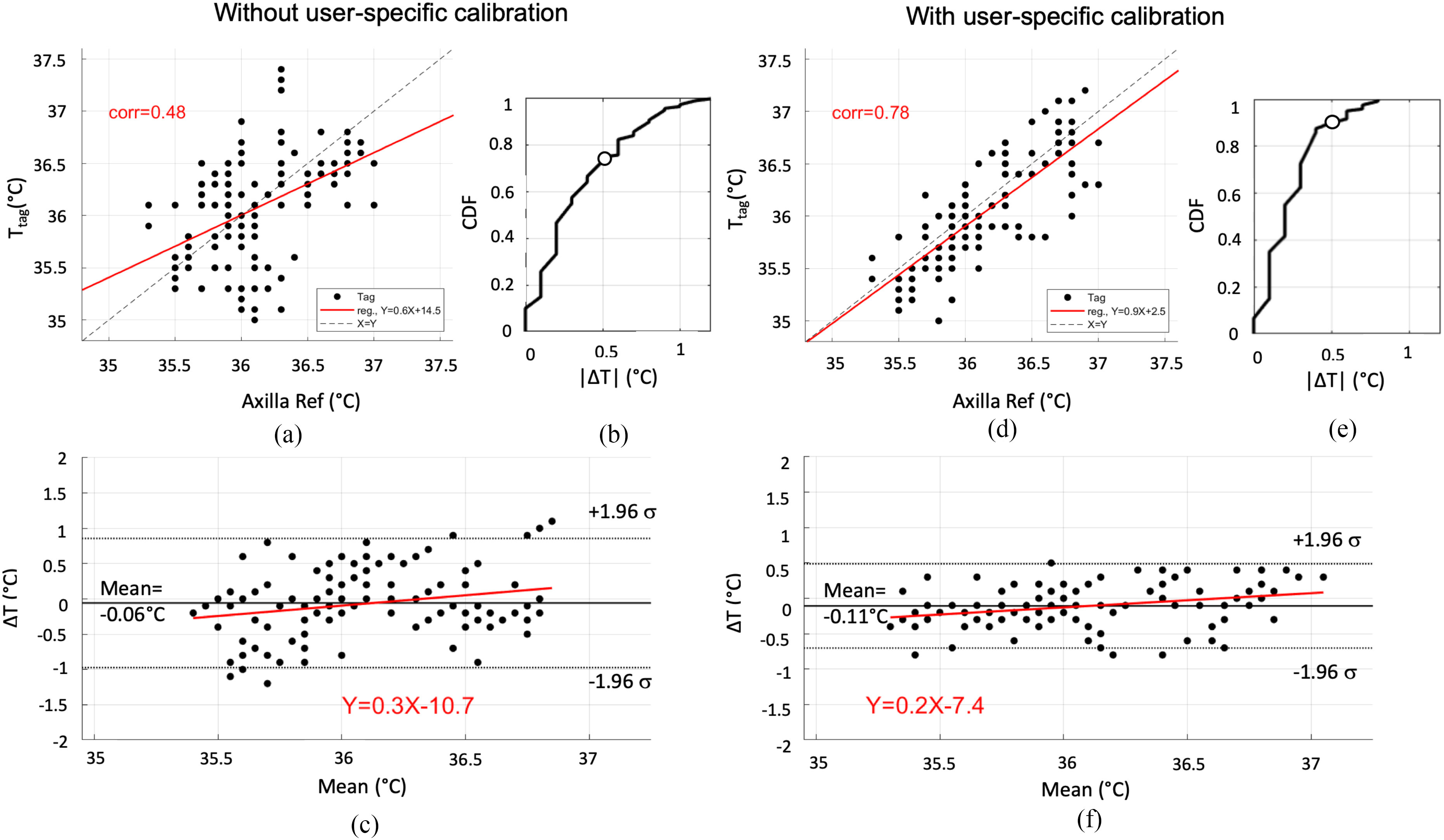
Numerical processing of degree of agreement between the two datasets  without and user-specific calibration. (a) and (d) RFID data versus reference thermometer. (b) and (e) Cumulative distribution of differences
without and user-specific calibration. (a) and (d) RFID data versus reference thermometer. (b) and (e) Cumulative distribution of differences  . (c) and (f) Bland–Altman diagrams with an indication of 95% limit of agreement, bias, and linear regression.
. (c) and (f) Bland–Altman diagrams with an indication of 95% limit of agreement, bias, and linear regression.
B. User-Specific Calibration
The same dataset was then reprocessed by introducing a user-specific calibration that can be computed once and for all just after the WED has been attached under the axilla. Namely, the temperature reading of the electronic thermometer in the first measurement round (n = 1) on the kth volunteer ( ) is used to calibrate all the following nth RFID data (
) is used to calibrate all the following nth RFID data ( ) in order to get rid of possible user-variability due to the plaster placement and the skin adhesion. In formulas, the calibrated tag temperature
) in order to get rid of possible user-variability due to the plaster placement and the skin adhesion. In formulas, the calibrated tag temperature  is
is
 |
This calibration was then applied to the whole dataset of that volunteer and the systematic errors were sensibly reduced. Indeed, correlation considerably improves [see Fig. 6(d)], with a Pearson index p = 0.78. Even though the new bias ( ) is comparable with the calibration-less one, the standard deviation is now smaller (
) is comparable with the calibration-less one, the standard deviation is now smaller ( ) leading to approximately ±0.58 °C difference between the two thermometers (95% degree of agreement) in almost the whole considered measurement range [see Fig. 6(e) and (f)]. It is worth mentioning that the authors were able to reuse the same calibration data while having detached and attached again the WED several times on the same volunteer for up to 5–7 days by preserving the above degree of agreement with the electronics thermometer.
) leading to approximately ±0.58 °C difference between the two thermometers (95% degree of agreement) in almost the whole considered measurement range [see Fig. 6(e) and (f)]. It is worth mentioning that the authors were able to reuse the same calibration data while having detached and attached again the WED several times on the same volunteer for up to 5–7 days by preserving the above degree of agreement with the electronics thermometer.
IV. Conclusion
Even in a realistic scenario, data from the UHF RFID skin sensor thermometer are comparable with the ones provided by a conventional electronic placed in the same region. If correctly used (i.e., by placing the sensor close to axillary fossa and by keeping the arm closed for 5 min before collecting data), the average bias is negligible, and the degree of agreement is ±1 °C, independently on the environmental and clothing conditions. Furthermore, a sensible improvement can be achieved by means of user-specific calibration, to be set only at the time of the first measurement (±0.5 °C degree of agreement, correlation index 0.78). The time needed for calibration duration is mostly due to the time required to collect the reference temperature (1–3 min). Such initial extra-complexity could be acceptable when the user has to be periodically monitored.
WED thermometers could be low cost (<1 $ each), while the reader's cost spans between $200 (mobile keyfob) and $500 (fixed reader with an embedded computer). Since WEDs naturally enable the identification of patients by means of the Unique Identification Code of the IC, they could have an advantage over the more complex infrared and thermal cameras (see Table 2) in the epidemic control and screening, within scenarios where a community of people regularly share spaces and activities (nursing homes, hospitals, barracks) and, hence, can wear the device for several days.
Acknowledgment
This work was supported in part by Lazio Innova within “Programma Gruppi di Ricerca – SECOND SKIN,” under Grant 85-2017-14774 and in part by the University of Rome Tor Vergata within “Beyond Borders – Epidermal Sensor Networks for Emerging 5G systems,” under Grant E84I19002410005.
Contributor Information
Francesca Camera, Email: frncamera@gmail.com.
Carolina Miozzi, Email: carolina.miozzi@uniroma2.it.
Francesco Amato, Email: f.amato@gatech.edu.
Cecilia Occhiuzzi, Email: cecilia.occhiuzzi@uniroma2.it.
Gaetano Marrocco, Email: gaetano.marrocco@uniroma2.it.
References
- [1].Aw J., “The non-contact handheld cutaneous infrared thermometer for fever screening during the COVID-19 global emergency,” J. Hospital Infection, vol. 104, no. 4, p. 451, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Hsiao S.-H. et al. , “Measurement of body temperature to prevent pandemic COVID-19 in hospitals in taiwan: Repeated measurement is necessary,” J. Hospital Infection, vol. 105, no. 2, pp. 360–361, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Werner J., “Measurement of temperatures of the human body,” Brahme A. (Ed.), Comprehensive Biomedical Physics, vol. 5. Amsterdam, The Netherlands: Elsevier, 2014, pp. 107–126. [Google Scholar]
- [4].Kim D. H. et al. , “Epidermal electronics,” Science, vol. 333, no. 6044, pp. 838–843, 2011. [DOI] [PubMed] [Google Scholar]
- [5].Krishnan S. R. et al. , “Wireless, battery-free epidermal electronics for continuous, quantitative, multimodal thermal characterization of skin,” Small, vol. 14, no. 47, 2018, Art. no. 1803192. [DOI] [PubMed] [Google Scholar]
- [6].Miozzi C., Nappi S., Amendola S., Occhiuzzi C., and Marrocco G., “A general-purpose configurable RFID epidermal board with a two-way discrete impedance tuning,” IEEE Antennas Wireless Propag. Lett., vol. 18, no. 4, pp. 684–687, Apr. 2019. [Google Scholar]
- [7].Miozzi C., Amendola S., Bergamini A., and Marrocco G., “Clinical trial of wireless epidermal temperature sensors: Preliminary results,” in Proc. Eur. Med. Biol. Engin. Conf., 2017, pp. 1041–1044. [Google Scholar]
- [8].Miozzi C., Amato F., and Marrocco G., “Performance and durability of thread antennas as stretchable epidermal UHF RFID tags,” IEEE J. Radio Freq. Identification, to be published, doi: 10.1109/JRFID.2020.3001692. [DOI]
- [9].Camera F. and Marrocco G., “Electromagnetic-based correction of bio-integrated RFID sensors for reliable skin temperature monitoring,” IEEE Sens. J., to be published, doi: 10.1109/JSEN.2020.3014404. [DOI]
- [10].Chaturvedi D., Vilhekar K. Y., Chaturvedi P., and Bharambe M. S., “Comparison of axillary temperature with rectal or oral temperature and determination of optimum placement time in children,” Indian Pediatrics, vol. 41, pp. 600–603, 2004. [PubMed] [Google Scholar]
- [11].Amendola S., Bovesecchi G., Palombi A., Coppa P., and Marrocco G., “Design, calibration and experimentation of an epidermal RFID sensor for remote temperature monitoring,” IEEE Sens, J., vol. 16, no. 19, pp. 7250–7257, Oct. 2016. [Google Scholar]
- [12].Giavarina D., “Understanding bland altman analysis,” Biochemia Medica, vol. 25, no. 2, pp. 141–151, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]