Abstract
Background
The outbreak of Coronavirus disease (COVID-19) in 2019 and the resulting quarantine may have increased the prevalence of mental health problems in adolescents. The aim of this study was to explore the association between the effects of home-based learning during the pandemic and the risks of depression, anxiety, and suicidality among junior and senior high school students.
Methods
An online survey using Patient Health Questionnaire (PHQ-9) and Generalized Anxiety Disorder (GAD-7) was conducted between 12 to 30 April 2020, on a total of 39,751 students. Multivariable logistic regression analysis was used to analyze the risk factors of associated depression, anxiety and suicidality during the pandemic.
Results
Prevalence of depression, anxiety symptoms and suicidality found was 16.3% (95% CI: 16.0, 16.7), 10.3% (95% CI: 10.0, 10.6) and 20.3% (95% CI: 19.9, 20.7), respectively. Participants with female gender and in junior high school, with poor overall sleep quality and poor academic performance and very worried about being infected during COVID-19 were highly associated with the risk of depression, anxiety symptoms and suicidal ideation (all P<0.001).
Conclusions
Prevalence of self-reported mental health problems for adolescents using home-based distance learning was high. Implementing measures (e.g., wearing face masks) and spending only moderate time focusing on COVID-19-related information could be protective factors for mental health. These results provide suggestions for teachers and policy makers regarding adolescent improving sleep quality (sufficient sleep) and academic performance and reducing worry about pandemic during quarantine to prevent mental health problems.
Keywords: COVID-19, Adolescents, Depression Symptoms, Anxiety Symptoms, Suicidality
Introduction
Since the first outbreak of the Coronavirus disease (COVID-19) at the end of 2019, the COVID-19 pandemic was listed as a global public health emergency of international concern by the World Health Organization (WHO, 2020). In order to contain the spread of COVID-19, most recently, the Chinese Government issued a stay-at-home order, which meant that mass quarantine was mandatory during the initial outbreak of COVID-19 (Brooks et al., 2020). For example, only residents were allowed to enter residential communities, the wearing of face masks was made compulsorily, and non-essential community services were shut down (Leung et al., 2020). Meanwhile, 107 countries as estimated by the UN Educational, Scientific and Cultural Organization (UNESCO) on 18 March 2020, had implemented national school closures related to COVID-19, affecting 862 million children and adolescents (UNESCO, 2020). In particular, there were more than 220 million children and young people confined to their homes in China, according to the Ministry of Education of China (Ministry of Education of China, 2020). Normal daily life shifted for adolescents to home-based distance learning models, which has resulted in substantial disruption to the lives of students and their families and which may have longer-term consequences for adolescent health (Golberstein et al., 2020). There are obvious advantages to remote learning, e.g., accessibility and comfort during online learning, however, the limitations of inefficient learning, lack of eye contact and feedback from teachers, inattention and the difficulty in maintaining academic integrity are also of concern (Mukhtar et al., 2020). Although adolescence is a transitional and critical developmental period with brain and body maturation, students still faced further challenges in terms of losing structure and support, routine social connections, social distancing and loneliness, less physical activity, spending more time on screens, increased irregular sleep patterns, and less favorable diets, resulting collectively in weight gain and a loss of cardiorespiratory fitness (Brazendale et al., 2017; Loades et al., 2020). These challenges have been associated with increased mental health problems in adolescents, including an increase in anxiety, depression, loneliness and a loss of motivation and purpose (Caspi et al., 2006). Therefore, adolescent mental health needs to be prioritized during the COVID-19 pandemic.
Depression and suicide are significant global public health problems that occur across lifespans. According to the World Health Organization, depression is one of the leading causes of disability, suicide is the second leading cause of death among 15-29-year-olds (WHO, 2021a). One person dies of suicide every 40s (WHO, 2021b). The estimated lifetime and last-year prevalence rates of suicidal ideation in the Chinese adolescents were 17.6 and 10.7% in males, 23.5 and 14.7% in females (Liu et al., 2019). Symptoms of anxiety and depression often occur sequentially or concurrently in adolescents (Chavira et al., 2004; Garber and Weersing, 2010). A review in 2020 by Nearchou et al., (Nearchou et al., 2020) reported that the mental health consequences of COVID-19 were particularly associated with depression and anxiety in adolescent cohorts rather than with suicide. However, in the view of Reger et al., (Reger et al., 2020) the potential for adverse consequences in terms of suicide risk are high both during and following the COVID-19 outbreak as a result of isolation and quarantine. The interpersonal theory of suicide by Van Orden et al., (Van Orden et al., 2010) emphasized that the role of social connection is essential in suicide prevention. People experiencing suicidal thoughts may lack connection to others and often disconnect increasingly as the risk of suicide rises (Van Orden et al., 2010). Suicidal thoughts and behaviors are associated with social isolation and loneliness (Van Orden et al., 2010). Furthermore, there is a need to understand the increased risk of suicide and to address directly specific recommendations that can aid suicide prevention in adolescents (Klomek, 2020). Despite evidence of the negative impact of the virus and necessary quarantine on adults, media reports on suicidal behavior need to be cautious and research findings should be presented in a balanced way (Hawton et al., 2021), as research on the impact on children and adolescents is to date limited (Nearchou et al., 2020).
To fill the knowledge gap, the current study was conducted to investigate the prevalence and risk factors of depression, anxiety and suicidality among high school students using home-based learning models during the COVID-19 lockdown. This study may be useful for policy makers in dealing with Coronavirus outbreaks necessitating worldwide school closures.
Methods
Participants and Procedure
For this study an online cross-sectional investigation was designed during the COVID-19 pandemic and before the start of the Spring 2020 semester at Foshan City, in Guangdong Province. Because the aim of this study was to assess the mental health of students before they returned to school in 2020, and the time return to school was different for each level of student, the questionnaire was distributed to the junior high school and senior high school students between 12 and 30 April 2020. The students were asked to voluntarily complete an online questionnaire which was administered by their headteacher via a link to Wen Juan Xing (a professional online survey platform) sent to students’ WeChat or QQ class groups. A total of 47,614 students completed the questionnaire; 6,905 students were excluded due to answering the same choices in all scales and students who answered the same questionnaire more than one time, and 958 students using the same IP address were excluded. In total, 39,751 students were included in the study and all participants and their guardians signed the e-informed content statement before completing the questionnaire. This study was approved by the Southern Medical University, Guangzhou, China.
Measurements
Socio-demographic characteristics
Three main factors for examination in the study formed the questionnaire: demographic factors, pandemic-related factors, and daily routine and behavior factors. Demographic factors were associated with each participant’s age, grade, family type, single child or siblings, academic performance, health status and residence. The pandemic-related factors consisted of four questions about COVID-19: (i) time spent focusing on COVID-19 information; (ii) concern about being infected; (iii) psychological help sought due to COVID-19; (iv) implemented preventive measures during COVID-19. Further questions were included to examine participants’ daily sleep routine and how they had dealt with the COVID-19 pandemic. These questions gathered information on wake-up times, sleep duration, bedtime and overall sleep quality and were all related to daily sleeping routines, while questions about physical activity and time spent online surfing indicated their daily behaviors at home.
Mental Health Problems
Patient Health Questionnaire (PHQ-9)
The Patient Health Questionnaire (PHQ-9) is the 9-item depression module taken from the full PHQ (Kroenke et al., 2001). The PHQ-9 is a reliable and valid instrument used for screening for depression in adolescents in primary care facilities in China. A score of 10 was used as the cut-off to indicate depression in the sample of Chinese adolescents (Xingchen et al., 2014). Cronbach’s alpha was 0.91 in the study. As a severity measure, the PHQ-9 score can range from 0-27, the higher the sum score, the more severe the depressive symptoms, and the cut-off points are easy to memorize: i.e., 5, 10, 15 and 20 representing thresholds for mild, moderate, moderately severe, and severe depressive symptoms, respectively(Kroenke, 2021).
Item 9 of the PHQ-9 was used to assess the presence of suicidal thoughts as follows: “Over the last two weeks, how often have you been bothered by thoughts that you would be better off dead, or of hurting yourself in some way?” The response options were “not at all” (0 points), “several days” (1 point), “more than half the days” (2 points), and “nearly every day” (3 points). Suicidal ideation was defined as positive if a participant’s option was “several days,” “more than half the days,” and “nearly every day” (Rossom et al., 2017; Rotenstein et al., 2016).
Generalized Anxiety Disorder (GAD-7)
The Generalized Anxiety Disorder (GAD-7) is a widely-used method used in mental health care settings in China to measure the frequency of emotions that may be related to anxiety and depression. Several research studies have been carried out to confirm the reliability and validity of GAD-7 in the Chinese population (Yang et al., 2017; Xu et al., 2018). The cut-off point for GAD-7 was 10 (Spitzer et al., 2006) and Cronbach’s alpha was 0.93 in the study. GAD-7 consisted of seven items, each question had four possible responses (ranging from 0 to 3), and the total score ranged from 0 to 21. The severity of anxiety symptoms was classified as none (0–4), mild (5–9), moderate (10–14), and severe (15–21).
Statistical Analysis
The data was analyzed using SPSS version 22.0 (IBM, SPSS, Armonk, NY). The demographic variables were described as numbers and percentages using Chi-squared tests comparing the difference of categorical variables between male and female groups. Binary multivariate logistic regression analyses were performed to explore potential factors associated with the prevalence and risk factors in mental health status. The mental health status of all respondents was divided by the cut off values; the presence of depression, anxiety and suicide risk were the dependent variables respectively, and the socio-demographic variables were the independent variables. Odds ratio (OR) values and adjusted odds ratio (AOR) values are all presented in Table 2 and the statistical significance level was set at P<0.05 (two sided).
Table 2.
Bivariate and multivariable analysis: association with pandemic-related, major demographic, daily routine and behavior factors with depression, anxiety symptoms and suicide risk (N=39751)
| Depression No. (%)[95%CI] |
Crude OR(95%CI) | AOR (95%CI) | Anxiety No. (%)[95%CI] |
Crude OR(95%CI) | AOR (95%CI) | Suicide risk No. (%)[95%CI] |
Crude OR(95%CI) | AOR (95%CI) | |
|---|---|---|---|---|---|---|---|---|---|
| Total | 6497(16.3)[16.0,16.7] | 4083(10.3)[10.0,10.6] | 8081(20.3)[19.9,20.7] | ||||||
| Pandemic-related factors | |||||||||
| Focusing on COVID-19 | |||||||||
| ≤1 h | 4090(17.4)[17.0,17.9] | Ref. | Ref. | 2521(10.8)[10.4,11.2] | Ref. | Ref. | 4978(21.2)[20.7,21.8] | Ref. | Ref. |
| 1-2 h | 1993(14.1)[13.5,14.6] | 0.77***(0.73,0.82) | 0.97(0.90,1.03) | 1267(8.9)[8.5,9.4] | 0.82***(0.76,0.88) | 0.99(0.91,1.07) | 2616(18.5)[17.8,19.1] | 0.84***(0.80,0.89) | 0.98(0.92,1.04) |
| ≥3 h | 414(19.4)[17.7,21.0] | 1.14*(1.02,1.27) | 1.37***(1.20,1.56) | 295(13.8)[12.3,15.3] | 1.33***(1.17,1.51) | 1.50***(1.30,1.74) | 487(22.8)[21.0,24.5] | 1.09(0.98,1.22) | 1.24***(1.11,1.39) |
| Worried about being infected | |||||||||
| Very worried | 515(23.1)[21.3,24.8] | 1.58***(1.42,1.75) | 1.73***(1.53,1.95) | 382(17.1)[15.6,18.7] | 2.05***(1.82,2.31) | 2.25***(1.97,2.57) | 552(24.8)[23.0,26.5] | 1.31***(1.18,1.45) | 1.29***(1.15,1.44) |
| Worried | 2660(15.9)[15.3,16.4] | 0.99(0.94,1.05) | 1.00(0.94,1.06) | 1797(10.7)[10.2,11.2] | 1.19***(1.11,1.27) | 1.25***(1.16,1.35) | 3363(20.1)[19.4,20.7] | 1.00(0.95,1.05) | 0.97(0.92,1.03) |
| Not worried | 3322(16.0)[15.5,16.5] | Ref. | Ref. | 1904(9.2)[8.8,9.6] | Ref. | Ref. | 4166(20.1)[19.5,20.6] | Ref. | Ref. |
| Implemented preventive measures during COVID-19 | |||||||||
| Yes | 6178(15.9)[15.5,16.3] | Ref. | Ref. | 3861(9.9)[9.6,10.2] | Ref. | Ref. | 7714(19.8)[19.5,20.2] | Ref. | Ref. |
| No | 319(36.0)[32.8,39.2] | 2.98***(2.59,3.42) | 1.60***(1.35,1.90) | 222(25.1)[22.2,27.9] | 3.03***(2.59,3.54) | 1.68***(1.40,2.01) | 367(41.4)[38.2,44.7] | 2.86***(2.49,3.27) | 1.88***(1.62,2.19) |
| Major Demographic factors | |||||||||
| Gender | |||||||||
| Male | 2448(12.9)[12.4,13.4] | Ref. | Ref. | 1518(8.0)[7.6,8.4] | Ref. | Ref. | 3004(15.8)[15.3,16.4] | Ref. | Ref. |
| Female | 4049(19.5)[18.9,20.0] | 1.63***(1.55,1.72) | 1.64***(1.54,1.74) | 2565(12.3)[11.9,12.8] | 1.62***(1.51,1.73) | 1.59***(1.48,1.71) | 5077(24.4)[23.8,25.0] | 1.72***(1.63,1.81) | 1.72***(1.63,1.82) |
| Grade | |||||||||
| Junior high | 1596(15.1)[14.4,15.8] | 1.08**(1.02,1.14) | 1.49***(1.39,1.59) | 1006(9.5)[8.9,10.1] | 1.16***(1.08,1.24) | 1.46***(1.35,1.58) | 5766(22.1)[21.6,22.6] | 1.39***(1.32,1.47) | 1.82***(1.72,1.93) |
| Senior high | 1682(17.1)[16.3,17.8] | Ref. | Ref. | 1038(10.5)[9.9,11.1] | Ref. | Ref. | 2315(16.9)[16.3,17.6] | Ref. | Ref. |
| Academic performance | |||||||||
| Good | 1710(10.9)[10.4,11.4] | Ref. | Ref. | 1141(7.3)[6.9,7.7] | Ref. | Ref. | 2402(15.3)[14.8,15.9] | Ref. | Good |
| Medium | 2830(16.9)[16.3,17.5] | 1.66***(1.56,1.77) | 1.33***(1.23,1.42) | 1751(10.5)[10.0,10.9] | 1.49***(1.37,1.61) | 1.18***(1.08,1.28) | 3540(21.1)[20.5,21.8] | 1.48***(1.40,1.57) | 1.26***(1.19,1.34) |
| Poor | 1957(26.6)[25.6,27.6] | 2.96***(2.75,3.18) | 1.90***(1.74,2.06) | 1191(16.2)[15.4,17.0] | 2.46***(2.25,2.68) | 1.50***(1.36,1.65) | 2139(29.1)[28.0,30.1] | 2.26***(2.12,2.42) | 1.66***(1.54,1.79) |
| Health status | |||||||||
| Very healthy | 3183(11.6)[11.2,12.0] | Ref. | Ref. | 2002(7.3)[7.0,7.6] | Ref. | Ref. | 4427(16.1)[15.7,16.6] | Ref. | Ref. |
| Well | 2209(22.0)[21.2,22.8] | 2.15***(2.03,2.29) | 1.62***(1.52,1.74) | 1343(13.4)[12.7,14.1] | 1.96***(1.83,2.11) | 1.49***(1.37,1.61) | 2618(26.1)[25.2,27.0] | 1.84***(1.74,1.94) | 1.50***(1.41,1.59) |
| General or poor | 1105(48.5)[46.5,50.6] | 7.19***(6.57,7.86) | 2.77***(2.50,3.09) | 738(32.4)[30.5,34.3] | 6.09***(5.52,6.73) | 2.46***(2.19,2.76) | 1036(45.5)[43.5,47.5] | 4.34***(3.97,4.74) | 2.09***(1.89,2.31) |
| Daily routine and behavior factors | |||||||||
| Overall sleep quality* | |||||||||
| Good | 2458(8.4)[8.1,8.7] | Ref. | Ref. | 1531(5.2)[5.0,5.5] | Ref. | Ref. | 4078(13.9)[13.5,14.3] | Ref. | Ref. |
| Normal | 2730(32.3)[31.3,33.3] | 5.23***(4.92,5.56) | 3.99***(3.74,4.26) | 1630(19.3)[18.5,20.1] | 4.35***(4.04,4.69) | 3.39***(3.13,3.67) | 2888(34.2)[33.2,35.2] | 3.22***(3.05,3.41) | 2.61***(2.46,2.77) |
| Poor | 1309(67.5)[65.4,69.6] | 22.71***(20.47,25.19) | 15.60***(13.98,17.42) | 922(47.5)[45.3,49.7] | 16.47***(14.86,18.25) | 11.29***(10.11,12.62) | 1115(57.5)[55.3,59.7] | 8.38***(7.61,9.22) | 5.98***(5.40,6.63) |
|
Depression No. (%)[95%CI] |
Crude OR(95%CI) | AOR (95%CI) |
Anxiety No. (%)[95%CI] |
Crude OR(95%CI) | AOR (95%CI) |
Suicide risk No. (%)[95%CI] |
Crude OR(95%CI) | AOR (95%CI) | |
| Physical activity time* | |||||||||
| Never | 696(37.3)[35.1,39.5] | 3.88***(3.37,4.45) | 1.68***(1.42,1.98) | 433(23.2)[21.3,25.1] | 3.04***(2.58,3.58) | 1.31**(1.09,1.58) | 674(36.2)[34.0,38.3] | 2.64***(2.31,3.01) | 1.32***(1.14,1.53) |
| ≤30 mins | 3124(18.9)[18.3,19.5] | 1.51***(1.35,1.69) | 1.05(0.92,1.19) | 1911(11.5)[11.0,12.0] | 1.31***(1.15,1.49) | 0.94(0.81,1.08) | 3721(22.5)[21.8,23.1] | 1.35***(1.22,1.49) | 0.99(0.88,1.10) |
| 30-60 mins | 2259(12.4)[11.9,12.9] | 0.92(0.83,1.03) | 0.85**(0.75,0.96) | 1455(8.0)[7.6,8.4] | 0.87*(0.76,1.00) | 0.82**(0.71,0.95) | 3132(17.2)[16.7,17.8] | 0.97(0.88,1.07) | 0.85**(0.76,0.95) |
| ≥60 mins | 418(13.3)[12.1,14.5] | Ref. | Ref. | 284(9.1)[8.1,10.1] | Ref. | Ref. | 554(17.7)[16.3,19.0] | Ref. | Ref. |
| Online surfing time | |||||||||
| ≤1 h | 1235(11.8)[11.2,12.4] | Ref. | Ref. | 824(7.9)[7.3,8.4] | Ref. | Ref. | 1705(16.3)[15.5,17.0] | Ref. | Ref. |
| 1-2 h | 2969(14.9)[14.4,15.4] | 1.31***(1.22,1.41) | 1.27***(1.17,1.37) | 1814(9.1)[8.7,9.5] | 1.17***(1.08,1.28) | 1.12*(1.02,1.23) | 3853(19.3)[18.8,19.9] | 1.23***(1.16,1.31) | 1.22***(1.14,1.30) |
| 3-5 h | 1486(21.5)[20.5,22.5] | 2.05***(1.89,2.23) | 1.58***(1.44,1.74) | 917(13.3)[12.5,14.1] | 1.80***(1.63,1.98) | 1.37***(1.23,1.53) | 1705(24.7)[23.7,25.7] | 1.69***(1.57,1.82) | 1.44***(1.33,1.56) |
| ≥5 h | 807(33.8)[31.9,35.7] | 3.83***(3.45,4.25) | 2.10***(1.85,2.37) | 528(22.1)[20.5,23.8] | 3.33***(2.96,3.76) | 1.85***(1.61,2.12) | 818(34.3)[32.4,36.2] | 2.69***(2.44,2.97) | 1.70***(1.53,1.90) |
CI: confidence interval; OR: odds ratio; AOR: adjusted odds ratio; all independent variables were simultaneously entered into a logistic regression model; *: in last two weeks before the date the questionnaire was circulated. ***P<0.001; **P<0.01; *P<0.05
Results
Sample Characteristics (Table 1)
Table 1.
The basic characteristics of study population
| Variables | Category | Total (N=39751) |
Male (n=18966) |
Female (n=20785) |
p-value |
|---|---|---|---|---|---|
| Age, mean (SD), year | 14.79(1.7) | 14.8(1.7) | 14.78(1.7) | 0.130 | |
| Grades, n (%) | Junior high | 26090(65.6) | 12669(48.6) | 13421(51.4) | < 0.001 |
| Senior high | 13661(34.4) | 6297(46.1) | 7364(53.9) | ||
| Academic performance, n (%) | Good | 15653(39.4) | 7555(39.8) | 8098(39.0) | < 0.001 |
| Medium | 16744(42.1) | 7532(39.7) | 9212(44.3) | ||
| Poor | 7354(18.5) | 3879(20.5) | 3475(16.7) | ||
| Health status, n (%) | Very healthy | 27443(69.0) | 13505(71.2) | 13938(67.1) | < 0.001 |
| Well | 10031(25.2) | 4452(23.5) | 5579(26.8) | ||
| poor | 2277(5.7) | 1009(5.3) | 1268(6.1) | ||
| Overall sleep quality,* n (%) | Good | 29365(73.9) | 14614(77.1) | 14751(71.0) | < 0.001 |
| Normal | 8446(21.2) | 3493(18.4) | 4953(23.8) | ||
| Poor | 1940(4.9) | 859(4.5) | 1081(5.2) | ||
| Physical activity time,* n (%) | Never | 1864(4.7) | 893(4.7) | 971(4.7) | < 0.001 |
| ≤30 mins | 16567(41.7) | 6942(36.6) | 9625(46.3) | ||
| 30-60 mins | 18184(45.7) | 8801(46.4) | 9383(45.1) | ||
| ≥60 mins | 3136(7.9) | 2330(12.3) | 806(3.9) | ||
| Online surfing time, n (%) | ≤1 h | 10492(26.4) | 5185(27.3) | 5307(25.5) | < 0.001 |
| 1-2 h | 19961(50.2) | 9479(50.0) | 10482(50.4) | ||
| 3-5 h | 6912(17.4) | 3204(16.9) | 3708(17.8) | ||
| ≥5 h | 2386(6.0) | 1098(5.8) | 1288(6.2) | ||
| Time spent focusing on COVID-19, n (%) | ≤1 h | 23442(59.0) | 10936(57.7) | 12506(60.2) | < 0.001 |
| 1-2 h | 14170(35.6) | 6792(35.8) | 7378(35.5) | ||
| ≥3 h | 2139(5.4) | 1238(6.5) | 901(4.3) | ||
| Concern about being infected, n (%) | Very worried | 2230(5.6) | 1266(6.7) | 964(4.6) | < 0.001 |
| Worried | 16768(42.2) | 7584(40.0) | 9184(44.2) | ||
| Not worried | 20753(52.2) | 10116(53.3) | 10637(51.2) | ||
| Implement preventive measures during COVID-19, n (%) | Yes | 38865(97.8) | 18493(97.5) | 20372(98.0) | < 0.001 |
| No | 886(2.20) | 473(2.5) | 413(2.0) |
Abbreviation: SD, standard deviation; COVID-19, Coronavirus Disease 2019; *: in last two weeks before the date the questionnaire was circulated.
The socio-demographic characteristics of participants are summarized in Table 1. In total, 39,751 participants enrolled in the study with 18,966 (47.7%) male and 20,785 (52.3%) female. The mean age of participants was 14.79 years (SD 1.7). Table 1 data shows three types of characteristics, including major demographic, daily routine behavior, and pandemic-related factors. All factors identified in Table 2 were statistically different in terms of gender (P<0.001). Female high school students showed higher proportions of poor overall sleep quality and more than five hours online surfing time during the COVID-19 pandemic (P<0.001). With regard to time spent in physical activity, female respondents spent a lower proportion of time exercising (60 minutes less than males) (P<0.001). The majority of students implemented learned preventive measures during the outbreak of COVID-19 (97.8%) and half of those were not worried about being infected (52.2%).
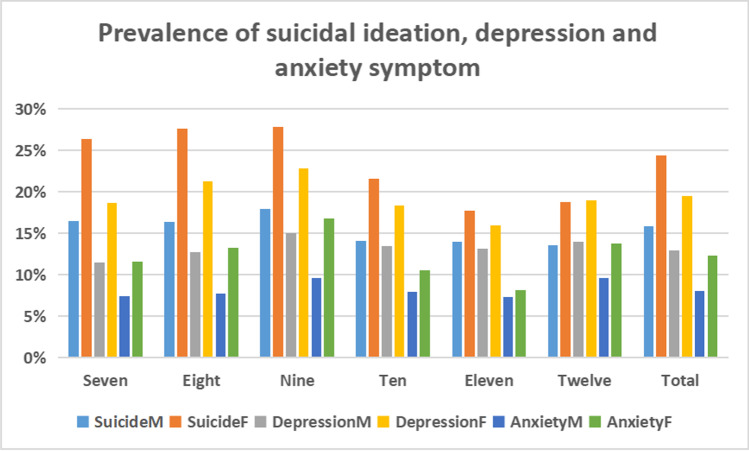
Prevalence of Suicidal Ideation, Depression and Anxiety Symptom by Gender and Grade (Fig. 1)
Fig. 1.
Percentage prevalence of suicidal ideation, depression and anxiety symptoms by gender and grade. Seven represents junior grade one, Eight represents junior grade two, Nine represents junior grade three; Ten represents senior grade one, Eleven represents senior grade two and Twelve represents senior grade three. SuicideM represents the prevalence of male suicidal ideation, SuicideF represents the prevalence of female suicidal ideation. DepressionM represents the prevalence of male suicidal ideation, DepressionF represents the prevalence of female suicidal ideation. AnxietyM represents the prevalence of male suicidal ideation, AnxietyF represents the prevalence of female suicidal ideation
Of the sample measured, 15.8% of males and 24.4% of females had suicidal ideation within the previous last two weeks before the date the study questionnaire was circulated; 12.9% and 19.5% had symptoms of depression respectively; and 8.0% and 12.3% had anxiety symptoms during the COVID-19 pandemic. The rates of prevalence of suicidal ideation, depression and anxiety symptoms were significantly higher in females than in males (all P<0.001). As shown in Fig. 1, there was a clear trend of increased suicidal thoughts, depression and anxiety symptoms in students up to grade nine (Mean age = 14.95). In contrast, suicidal ideation in males tended to decrease from grade ten (Mean age = 15.88) (14.1%) to twelve (Mean age = 17.86) (13.5%), while in females suicidal ideation showed a rebound from grade eleven (Mean age = 16.81) (17.7%) to grade twelve (18.7%).
Bivariable and Multivariable Analysis: Association of Pandemic-Related, Major Demographic and Daily Routine BehaviorFactors with Depression, Anxiety Symptom and Suicidal Ideation (Table 2)
In general, 16.3% respondents self-reported depression symptoms in the study, there were 25% respondents with mild depression, 9.4% with moderate depression and 6.9% with severe depression; while 10.3% participants self-reported anxiety symptoms, ranging from 20.9% mild to 6.9% moderate, and 3.4% were severe. As for suicidal ideation, 953 (2.4%) participants ticked the option of “nearly every day”, 1,420 (3.6%) chose “more than half the days”, and 5,708 (14.4%) ticked “several days”.
Table 2 summarizes the association of risk factors with depression, anxiety symptoms and suicidal ideation by using binary and multivariable logistic regression analysis, and odds ratio (ORs) and 95% CIs were calculated. The analysis showed the overall prevalence of depression, anxiety symptoms and suicide risk in the study respondents was 16.3% (95% CI: 16.0, 16.7), 10.3% (95% CI: 10.0, 10.6) and 20.3% (95% CI: 19.9, 20.7), respectively. Socio-demographic factors such as academic performance and physical activity time were statistically associated with the prevalence of depression, anxiety symptoms and suicidal ideation (P<0.05).
As for demographic characteristics, students who were females had potential risk higher than males (OR=1.64; 95% CI: 1.54, 1.74 for depression; OR=1.59; 95% CI: 1.48, 1.71; OR=1.72 for anxiety; 95% CI: 1.63, 1.82 for suicidal ideation; all P<0.001), students who were in junior high school had worsen mental health status than senior high school (OR=1.49; 95% CI: 1.39, 1.59 for depression; OR=1.46; 95% CI: 1.35, 1.58 for anxiety; OR=1.82; 95% CI: 1.72, 1.93 for suicidal ideation; all P<0.001), with poor academic performance had a higher risk of depression, anxiety symptoms and suicidal ideation (OR=1.9; 95% CI: 1.74, 2.06; OR=2.46; 95% CI: 2.25, 2.68; OR=1.66; 95% CI: 1.54, 1.79; all P<0.001, respectively) than good academic performance. General or poor health (P<0.001) was more likely to be associated with a higher risk of depression, anxiety symptoms and suicide risk (OR=2.77; 95% CI: 2.50, 3.09; OR=2.46; 95% CI: 2.19, 2.76; OR=2.09; 95% CI: 1.89, 2.31; all P<0.001, respectively). In particular, the risk of depression, anxiety symptoms and suicidal ideation for adolescents who were in general or poor in health was 1.77, 1.46 and 1.09 times (respectively) higher than those who were very healthy.
Note must be made of the pandemic-related factors: time spent focusing on COVID-19 information for more than three hours (OR=1.37; 95% CI: 1.20, 1.56; OR=1.50; 95% CI: 1.30, 1.74; OR=1.24; 95% CI: 1.11, 1.39; all P<0.001, respectively) and those who did not implement learned preventive measures during COVID-19 (OR=1.60; 95% CI:1.35, 1.90; OR=1.68; 95% CI: 1.40, 2.01; OR=1.88; 95% CI: 1.62, 2.19; all P<0.001, respectively) were highly associated with the risk of depression, anxiety symptoms and suicidal ideation. Furthermore, those very worried about being infected had a higher possibility of anxiety, depression symptoms and suicidal ideation (OR=2.25; 95% CI: 1.97, 2.57; OR=1.73; 95% CI: 1.53, 1.95; OR=1.29; 95% CI: 1.15, 1.44; all P<0.001, respectively) than those not worried about being infected.
In terms of daily routine behavioral factors, respondents with poor overall sleep quality had the highest risk of depression, anxiety symptoms and suicidal ideation (OR=15.6; 95% CI: 13.98, 17.42; OR=11.29; 95% CI: 10.11, 12.62; OR=5.98; 95% CI: 5.40, 6.63; all P<0.001, respectively) over all factors, which means that compared with good sleep quality, poor sleep quality was 14.6, 10.3 and 6.0 times (respectively) more highly associated with the risk of mental health problems. Lack of physical activity was significantly associated with the risk of depression, anxiety symptoms and suicidal ideation (OR=1.68; 95% CI: 1.42, 1.98; OR=1.31; 95% CI: 1.09, 1.58; OR=1.32; 95% CI: 1.14, 1.53; all P<0.001, respectively). Online surfing time of more than five hours was highly associated with mental health problems. The odds ratios of depression, anxiety symptoms and suicidal ideation were 2.1 (95% CI: 1.85, 2.37; P<0.001), 1.85 (95% CI: 1.61, 2.12; P<0.001) and 1.7 (95% CI: 1.53, 1.90; P<0.001, respectively), for online surfing time of more than five hours when compared with online surfing time of less than an hour.
Discussion
This cross-sectional study aimed to investigate the prevalence and risk factors associated with self-reported mental health problems such as depression, anxiety and suicidal ideation among junior and senior high school students during the COVID-19 pandemic in China. To our knowledge, few studies have reported prevalence and risk factors of suicidal ideation during the COVID-19 pandemic in high school students. This study found that the overall prevalence of depression, anxiety and suicidal ideation in the sample studied was relatively high (16.3%, 10.3% and 20.3%, respectively). We also found that grade nine students had the highest proportion of mental health problems among high school grades during the outbreak of COVID-19.
According to this study data, the prevalence of depression and anxiety symptoms was 16.3% and 10.3%, respectively, in junior high school and senior high school during the COVID-19 pandemic. Zhou et al., have reported that the prevalence of depression during COVID-19 pandemic between 8 and 15 March 2020 was 17.3% in junior high school students and senior high school students (N=8079) with the same scale and cut-off point (Zhou et al., 2020). The difference between these two study results is significant (χ2 =4.489, P=0.034), except for the prevalence of anxiety (both are 10.3%). Moreover, the prevalence of depression and anxiety was 13.76% and 6.73%, respectively in the study by Liu et al., where data was collected from 3,836 students at junior and senior high school after lockdown between 9 and 28 June 2020 (Liu et al., 2021b). The difference between these two study results in terms of depression and anxiety was statistically significant (χ2 =17.223 and χ2 =49.045, P<0.001, respectively). In a word, these two studies with this current study indicates that the prevalence of depression and anxiety might gradually decline by time during the COVID-19 lockdown. An UK Household Longitudinal study showed levels of mental health problems subsequently declined between April and June 2020 but significantly remained above pre-COVID-19 levels (Daly et al., 2020). The downward trend observed across March and April and June is consistent with a pattern of ‘recovery’ that is commonly observed in response to stressful or traumatic life events (Infurna & Luthar, 2018).
Other studies undertaken during COVID-19 reported various rates of suicidality, for example, a study by Hou et al., reported 31.3% of suicidal ideation among senior high school students in rural China (Hou et al., 2020). Shi et al., reported an overall prevalence of suicidal ideation of 16.4% among the general population in China (Shi et al., 2021), and a study by Hill et al., reported a suicidal ideation rate of 21.1% in March 2020 in an American Pediatric Emergency Department (Hill et al., 2021). Previous evidence has shown that approximately 10–20% of Ebola survivors had thoughts of suicide or self-harm during the outbreak (Secor et al., 2020). In the current study, the prevalence of suicidal ideation is 20.3%, which is lower than the study by Hou et al. One possible reason for this could be that Hou et al., investigated only senior high school students, so the sample contribution was not the same, the district was restricted to a rural one, whereas, our study included students in both rural and urban locations, and the assessments and time periods used were very different. Although the prevalence of suicidal ideation in this current study was higher than that found by Shi et al., the results could expand on the study by Shi et al., which investigated the general Chinese population over 18 years of age (Shi et al., 2021). As older people are more mature and perhaps capable in terms of facing such challenges, while 12–20-year-old adolescents will never have experienced an epidemic in their lifetime. Therefore, facing the spread of this worldwide disease and the consequences caused by COVID-19, it is likely that respondents in that age group would be confused at the loss of control of their life schedule and would not know how to cope, which could in turn lead to impulsive behaviors such as suicide. Moreover, adolescents need to know how to cope, to whom they can turn for help, who they can talk to, and how to express their worries when facing sudden life events. Meanwhile, the prevalence of suicidal ideation in the current study is relatively high, which indicates that adolescents have been suffering severe psychological distress during the COVID-19 period. So the government, society, school and family should be urged to pay more attention to targeting suicide prevention in adolescents. Meanwhile, this study could be useful as a supplemental one to add to the existing study of suicidal ideation in the general population by Shi et al.
As shown in the results of this study, females in Grade nine had the highest overall suicidal ideation (17.9% for male, 27.8% for female), depression (15.0% for male, 22.8% for female) and anxiety symptoms (9.6% for male, 16.8% for female) in all grades. Noticeably, female gender was positively associated with mental health problems, as well as higher levels of depression, anxiety and suicidal ideation during the COVID-19 pandemic, which is consistent with previous studies that found that female gender was at a higher risk of depression (Zhou et al., 2020; Lim et al., 2018) and anxiety symptoms (Zhou et al., 2020; Putwain, 2007). According to the demographic factors related to the COVID-19 pandemic, the results indicated that grade nine students (around 15 years old) had the highest prevalence of depression, anxiety symptoms and suicidal ideation among junior and senior high school respondents, this was especially the case for female adolescents. One possible reason for this could be that the age of 15 corresponds to the transition from junior to senior high school in China, which could be particularly stressful due to graduation exams, concerns about the future, struggling to adapt to a new environment and the added psychosocial pressure. Apart from the results of gender and grade which were different, poor academic performance and physical health were strongly associated with the risk of depression, anxiety symptoms and suicidal ideation in line with previous studies on the subject. Another previous study suggested that the detrimental impacts of COVID-19 on adolescents worried about their academic progress, might aggravate mental health issues generally (Hou et al., 2020). Self-reported unhealthy physical condition was associated strongly with the risk of depression and anxiety symptoms and is consistent with the study by Wang et al., conducted with Chinese college students during the outbreak of COVID-19 (Wang et al., 2020b) and also with Hawke et al (Hawke et al., 2020).
Apart from the demographic factors, the pandemic-related factors observed by the current study show that implementing learned preventive measures during COVID-19 and spending less time (i.e. less than an hour) focusing on COVID-19-related information may have a protective psychological effect for adolescents, which shows consistency with the study cited above by Zhou et al (Zhou et al., 2020). Implementing preventive measures such as wearing a face mask and practicing hand hygiene could reduce the level of anxiety and depression during the epidemic (Wang et al., 2020a). In addition, accurate information and reporting on the pandemic situation by authorities such as the Government and the Health Commission would help to allay fears. Access to accurate information would mean that there is no need to spend time on false information about COVID-19. The results show that the risk of anxiety symptoms for those “very worried about being infected” was 1.25 times higher than those “not worried about being infected”, 0.73 times higher in terms of depression symptoms, and 0.29 times higher for suicidal ideation. A review by Finiki et al., offers an insight into the association between COVID-19-related emotional reactions and mental health outcomes in young people, such as worry, fear about contracting the virus and stressor outcomes such as depression, anxiety, OCD symptoms, somatic symptoms and intensified behavior problems (Nearchou et al., 2020).
With regard to the daily routine behavioral factors, the study found that poor overall sleep quality had the highest association with the risk of depression, anxiety and suicidal ideation consistent with previous studies before and during the COVID-19 pandemic (Gong et al., 2020; Liu et al., 2021a). Overall sleep quality was the most important factor associated with mental health problems during COVID-19 among high school students. In addition, the study also found that time spent in moderate physical activity was associated with lower levels of depression, anxiety symptoms and suicidal ideation, also in line with previous studies by Lu et al. (Lu et al., 2020) and Chi et al. (Chi et al., 2020). Furthermore, the results indicated that adolescents spending more than five hours per day surfing online had higher odds of developing mental health problems, in line with the Li et al., study. Spending more time online, increases the feeling of anxiety, which could mean potential risk factors of addiction to the internet and to smartphones (Duan et al., 2020). Therefore, spending less time online, taking enough physical exercise (30–60 minutes per day), and improving sleep quality (for example, taking sufficient sleep, keeping exercise) are the main protective measures recommended for adolescents using e-learning models during the COVID-19 quarantine.
Limitations
This study concludes with some limitations. First, these results are based on self-reporting by the adolescents themselves, which might lead to misunderstanding of their actual status. Reports from parents and teachers could also be included in any future study. In addition, evaluation by professional psychiatrists where severe mental health problems are reported should be carried out. Secondly, the current study is a cross-sectional survey, so clarifying the causes of some of these mental health problems is difficult to ascertain. Thirdly, item 9 of the PHQ-9 was widely used to evaluate suicidal thoughts (Rossom et al., 2017; Uebelacker et al., 2011), however using a single item to assess this may bias the results, and it was limited to explore other domains of suicidality, such as suicidal plans and attempts. Finally, although we included many psychosocial factors, other associated factors such as students whose family members were infected or had succumbed to COVID-19 pandemic, students’ previous mental health problems and family psychiatry history, which may affect the study findings were not investigated.
Conclusions
The current findings indicate that the prevalence of depression, anxiety symptoms and suicidal ideation is relatively high, particularly for respondents who are female and in junior high school, with poor academic performance and negative health status, spending more than three hours focusing on COVID-19 information, very worried about being infected and those who did not implement preventive measures. Additionally, high risk of mental health problems is indicated in students who had poor overall sleep quality, little or no physical activity and who were spending more than five hours on the internet. These study findings contribute to a greater understanding of mental health problems during pandemics in both junior and high school students, especially in terms of suicidal ideation. The research will help to identify risk factors in the mental health of adolescents and provides some suggestions to prevent and manage according to the above factors, such as spending less time online, taking enough physical exercise (30–60 minutes per day), and improving sleep quality (for example, taking sufficient sleep, keeping exercise). Further longitudinal studies of the long-term effects of the COVID-19 pandemic and quarantine on adolescents are needed to expand on this research.
Acknowledgments
The authors want to express their sincere gratitude to all participants and the schools for their participating in the study. We would also like to thank the headteachers for their assistance during the study.
Author Contribution
Each author contributed substantially to the paper. Jingbo Zhao and Xiaodan Peng, Shunwei Liang designed the study. Lili Liu, Jianbin Chen and Chengcheng Cai made contributions to the conception and design of the work. Shunwei Liang and Xiaodan Peng collected data. Xiaodan Peng performed statistical analyses and drafted the manuscript. Lili Liu made contributions to the data analyses. Jianbin Chen, Andi Huang and Xiayong Wang contributed to reviewing the literature. Jingbo Zhao revised it critically for important intellectual content, and supervised the writing of the manuscript. All authors approved the final version of the manuscript.
Funding
This study was funded by the Key Projects for Research on Youth Development of Central Committee of the Communist Youth League (Grant No. 19ZD030) and the National Social Science Fund of China (Grant No. 16BSH105).
Data Availability
The datasets generated during and/or analyzed during the current study are available from the author on reasonable request.
Declarations
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Competing Interest
The authors declare that they have no competing interests. We declare that we do not have any commercial or associative interest that represents a conflict of interest in connection with the work submitted.
Ethical Statement
All procedures conducted were approved by the Southern Medical University.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Brazendale, K., Beets, M.W., Weaver, R.G., Pate, R.R., Turner-McGrievy, G.M., Kaczynski, A.T., Chandler, J.L., Bohnert, A., von Hippel, P.T. (2017). Understanding differences between summer vs. school obesogenic behaviors of children: The structured days hypothesis. International Journal of Behavioral Nutrition and Physical Activity, 14, 100. 10.1186/s12966-017-0555-2. [DOI] [PMC free article] [PubMed]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet, London. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Harrington HL, Moffitt TE, Milne BJ, Poulton R. Socially isolated children 20 years later: Risk of cardiovascular disease. Archives of Pediatrics and Adolescent Medicine. 2006;160:805–811. doi: 10.1001/archpedi.160.8.805. [DOI] [PubMed] [Google Scholar]
- Chavira DA, Stein MB, Bailey K, Stein MT. Comorbidity of generalized social anxiety disorder and depression in a pediatric primary care sample. Journal of Affective Disorders. 2004;80:163–171. doi: 10.1016/S0165-0327(03)00103-4. [DOI] [PubMed] [Google Scholar]
- Chi X, Liang K, Chen ST, Huang Q, Huang L, Yu Q, Jiao C, Guo T, Stubbs B, Hossain MM, Yeung A, Kong Z, Zou L. Mental health problems among Chinese adolescents during the COVID-19: The importance of nutrition and physical activity. IJCHP. 2020 doi: 10.1016/j.ijchp.2020.100218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly, M., Sutin, A. R., & Robinson, E. (2020). Longitudinal changes in mental health and the COVID-19 pandemic: evidence from the UK Household Longitudinal Study. Psychological Medicine, 1–10. Advance online publication. 10.1017/S0033291720004432. [DOI] [PMC free article] [PubMed]
- Duan L, Shao X, Wang Y, Huang Y, Miao J, Yang X, Zhu G. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. Journal of Affective Disorders. 2020;275:112–118. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber, J., Weersing, V.R. (2010). Comorbidity of Anxiety and Depression in Youth: Implications for Treatment and Prevention. Clinical Psychology, 17, 293–306. New York. [DOI] [PMC free article] [PubMed]
- Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatrics. 2020;174(9):819–820. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- Gong, Q., Li, S., Wang, S., Li, H., & Han, L. (2020). Sleep and suicidality in school-aged adolescents: A prospective study with 2-year follow-up. Psychiatry Research, 287. 10.1016/j.psychres.2020.112918 [DOI] [PubMed]
- Hawke LD, Monga S, Korczak D, Hayes E, Relihan J, Darnay K, Cleverley K, Lunsky Y, Szatmari P, Henderson J. Impacts of the COVID-19 pandemic on youth mental health among youth with physical health challenges. Early Intervention in Psychiatry. 2020 doi: 10.1111/eip.13052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K, Marzano L, Fraser L, Hawley M, Harris-Skillman E, Lainez YX. Reporting on suicidal behaviour and COVID-19-need for caution. The Lancet Psychiatry. 2021;8(1):15–17. doi: 10.1016/S2215-0366(20)30484-3. [DOI] [PubMed] [Google Scholar]
- Hill, R.M., Rufino, K., Kurian, S., Saxena, J., Saxena, K., Williams, L. (2021). Suicide ideation and attempts in a pediatric emergency department before and during COVID-19. Pediatrics, 147(3). 10.1542/peds.2020-029280. [DOI] [PubMed]
- Hou TY, Mao XF, Dong W, Cai WP, Deng GH. Prevalence of and factors associated with mental health problems and suicidality among senior high school students in rural China during the COVID-19 outbreak. Asian journal of psychiatry. 2020;54:102305. doi: 10.1016/j.ajp.2020.102305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Infurna FJ, Luthar SS. Re-evaluating the notion that resilience is commonplace: A review and distillation of directions for future research, practice, and policy. Clinical psychology review. 2018;65:43–56. doi: 10.1016/j.cpr.2018.07.003. [DOI] [PubMed] [Google Scholar]
- Klomek AB. Suicide prevention during the COVID-19 outbreak. The Lancet Psychiatry. 2020;7(5):390. doi: 10.1016/S2215-0366(20)30142-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K. (2021). PHQ-9: global uptake of a depression scale. World Psychiatry, 20(1)., 135-136. 10.1002/wps.20821. [DOI] [PMC free article] [PubMed]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung K, Wu JT, Liu D, Leung GM. First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: a modelling impact assessment. Lancet, London. 2020;395(10233):1382–1393. doi: 10.1016/S0140-6736(20)30746-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep. 2018;8(1):2861. doi: 10.1038/s41598-018-21243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu R, Chen X, Qi H, Feng Y, Xiao L, Yuan XF, Li YQ, Huang HH, Pao C, Zheng Y, Wang G. The proportion and associated factors of anxiety in Chinese adolescents with depression during the COVID-19 outbreak. Journal of Affective Disorders. 2021;284:114–119. doi: 10.1016/j.jad.2021.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu XC, Chen H, Liu ZZ, Wang JY, Jia CX. Prevalence of suicidal behaviour and associated factors in a large sample of Chinese adolescents. Epidemiology and psychiatric sciences. 2019;28(3):280–289. doi: 10.1017/S2045796017000488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Yue S, Hu X, Zhu J, Wu Z, Wang J, Wu Y. Associations between feelings/behaviors during COVID-19 pandemic lockdown and depression/anxiety after lockdown in a sample of Chinese children and adolescents. Journal of Affective Disorders. 2021;284:98–103. doi: 10.1016/j.jad.2021.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loades, M. E., Chatburn, E., Higson-Sweeney, N., Reynolds, S., Shafran, R., Brigden, A., Linney, C., McManus, M.N., Borwick, C., Crawley, E. (2020.) Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. Journal of the American Academy of Child Adolescent Psychiatry, 59(11), 1218-1239 e1213. 10.1016/j.jaac.2020.05.009 [DOI] [PMC free article] [PubMed]
- Lu C, Chi X, Liang K, Chen ST, Huang L, Guo T, Jiao C, Yu Q, Veronese N, Soares FC, Grabovac I, Yeung A, Zou L. Moving more and sitting less as healthy lifestyle behaviors are protective factors for insomnia, depression, and anxiety among adolescents during the COVID-19 pandemic. Psychology Research and Behavior Management. 2020;13:1223–1233. doi: 10.2147/PRBM.S284103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Education of China, Ministry of Industry and Information Technology of China (2020) Notice of arrangement for “suspension of school does not stop learning” during the postponement for the opening of primary and secondary schools. 2020. http://www.moe.gov.cn/srcsite/A06/s3321/202002/t20200212_420435.html (accessed 29 Feb. 2020 [in Chinese]).
- Mukhtar, K., Javed, K., Arooj, M., Sethi, A. (2020). Advantages, limitations and recommendations for online learning during COVID-19 pandemic era. Pakistan Journal of Medical Sciences, 36, S27–S31. 10.12669/pjms.36.COVID19-S4.2785. [DOI] [PMC free article] [PubMed]
- Nearchou, F., Flinn, C., Niland, R., Subramaniam, S.S., Hennessy, E. (2020). Exploring the impact of COVID-19 on mental health outcomes in children and adolescents: A systematic review. International Journal of Environmental Research and Public Health, 17(22). 10.3390/ijerph17228479. [DOI] [PMC free article] [PubMed]
- Putwain DW. Test anxiety in UK schoolchildren: prevalence and demographic patterns. Br J Educ Psychol. 2007;77(Pt 3):579–593. doi: 10.1348/000709906x161704. [DOI] [PubMed] [Google Scholar]
- Reger, M.A., Stanley, I.H., Joiner, T.E. (2020). Suicide Mortality and Coronavirus Disease 2019-A Perfect Storm? JAMA Psychiatry. 10.1001/jamapsychiatry.2020.1060. Advance online publication. 10.1001/jamapsychiatry.2020.1060. [DOI] [PubMed]
- Rossom RC, Coleman KJ, Ahmedani BK, Beck A, Johnson E, Oliver M, Simon GE. Suicidal ideation reported on the PHQ9 and risk of suicidal behavior across age groups. Journal of Affective Disorders Affect. 2017;215:77–84. doi: 10.1016/j.jad.2017.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, Segal JB, Peluso MJ, Guille C, Sen S, Mata DA. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016;316:2214–2236. doi: 10.1001/jama.2016.17324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Secor, A., Macauley, R., Stan, L., Kagone, M., Sidikiba, S., Sow, S., Dana Aronovich, D., Litvin, K., Davis, N., Alva, S., Sanderson, Jeff. (2020). Mental health among Ebola survivors in Liberia, Sierra Leone and Guinea: results from a cross-sectional study. BMJ Open. 10.1136/bmjopen-2019-035217. [DOI] [PMC free article] [PubMed]
- Shi L, Que JY, Lu ZA, Gong YM, Liu L, Wang YH, Ran MS, Ravindran N, Ravindran AV, Fazel S, Bao YP, Shi J, Lu L. Prevalence and correlates of suicidal ideation among the general population in China during the COVID-19 pandemic. European psychiatry. 2021;64(1):e18. doi: 10.1192/j.eurpsy.2021.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Uebelacker, L.A., German, N.M., Gaudiano, B.A., Miller, I.W. (2011). Patient health questionnaire depression scale as a suicide screening instrument in depressed primary care patients: a cross-sectional study. The Prim. Care Compan CNS Disord. 10.4088/PCC.10m01027. [DOI] [PMC free article] [PubMed]
- United Nations Educational, Scientific and Cultural Organization. (2020) COVID-19 educational disruption and response. 2020. https://en.unesco.org/themes/education-emergencies/coronavirus-school- closures (accessed 19 March 2020).
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr The interpersonal theory of suicide. Psychological Review. 2010;117(2):575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C.S., Ho, R.C. (2020a). Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 10.3390/ijerp h1705 1729. [DOI] [PMC free article] [PubMed]
- Wang ZH, Yang HL, Yang YQ, Liu D, Li ZH, Zhang XR, Zhang YJ, Shen D, Chen PL, Song WQ, Wang XM, Wu XB, Yang XF, Mao C. Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: A large cross-sectional study. Journal of Affective Disorders. 2020;275:188–193. doi: 10.1016/j.jad.2020.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2021b). Suicide data, https://www.who.int/news/item/09-09-2019-suicide-one-person-dies-every-40-seconds; 2021b [accessed13 October 2021].
- World Health Organization (2021a) Timeline: WHO’s COVID-19 response. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline#event-6 (accessed 11 March 2021).
- Xingchen, H., Yingli, Z., Wei, L., Hongmei Z., Shichang Y. (2014). Reliability and validity of the patient health questionnaire-9 in Chinese adolescents. Sichuan Mental Health, 27, No. 4. (in Chinese). 10.3969/j.issn.1007-3256.2014.04.021
- Xu WF, Peng Y, Chen BQ, Peng ZY, Zhao JL, Yu GL. Assessment of anxiety and depression by self-rating scales of GAD-7 and PHQ-9 in cardiovascular outpatients. World Latest Med. Inf. 2018;18(16):12–14. [Google Scholar]
- Yang, L., Z.W., Cai, J. (2017). Relation of anxiety and depression to lifestyle in junior high school students. Journal of Chinese Mental Health, 31(3), 235–240 (In Chinese).
- Zhou SJ, Zhang LG, Wang LL, Guo ZC, Wang JQ, Chen JC, Liu M, Chen X, Chen JX. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. European Child & Adolescent Psychiatry. 2020;29(6):749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the author on reasonable request.