Figure 1.
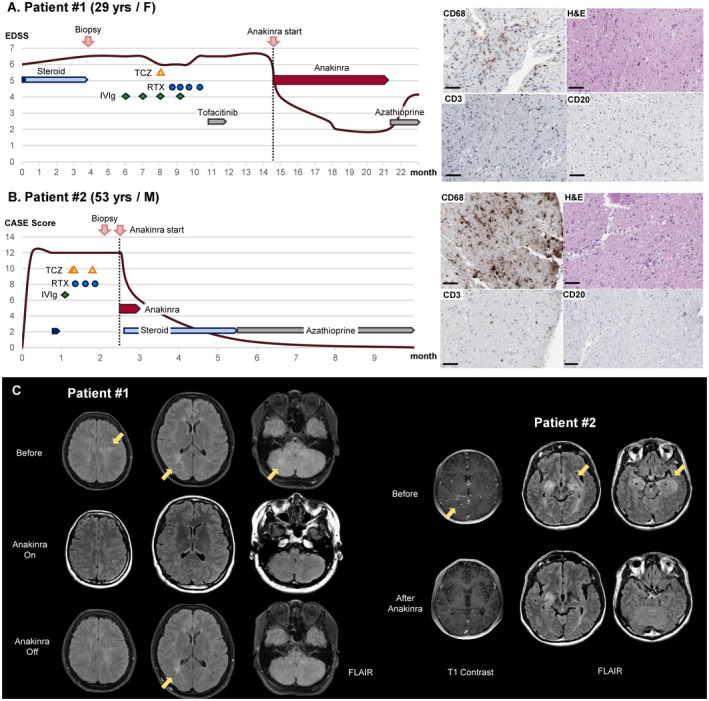
Clinical course, pathology, and brain images of Patients 1 and 2 who showed very good responses to the anakinra treatment. (A) A 29‐year‐old woman with primary progressive multiple sclerosis (PPMS) was pathologically identified as having a cerebral autoinflammatory response (CAIR), which is CD68‐positive macrophage infiltration. Anakinra treatment dramatically improved her symptoms from an expanded disability status scale (EDSS) score of 6.5 to 2.0, but after the discontinuation of anakinra, her symptoms aggravated again to an EDSS score of 4. (B) A 51‐year‐old man with refractory granulomatosis with polyangiitis (GPA) showed CD68‐positive microglia‐dominant pathology on brain biopsy. He responded very well to a 14‐day short‐term anakinra treatment followed by steroids and azathioprine, recovering from a Clinical Assessment Scale in Encephalitis (CASE) score of 12 to 0. All immunotherapies administered during the clinical courses are presented schematically. IVIg, intravenous immunoglobulin; RTX, rituximab; TCZ, tocilizumab. Scale bar = 100 μm. (C). In Patient 1, brain magnetic resonance imaging (MRI) identified T2 hyperintensity lesions in the bilateral subcortical and periventricular white matter, middle cerebellar peduncle, and cerebellum. During the anakinra treatment, the lesions disappeared but partially recurred after the discontinuation of anakinra. In Patient 2, brain MRI revealed improvement in T2 lesions in the bilateral medial temporal lobes and basal ganglia with leptomeningeal enhancement after the anakinra treatment.
