Abstract
Background:
The coronavirus disease 2019 (COVID-19) pandemic has led to increases in anxiety, depression, posttraumatic stress disorder, burnout, grief, and suicide, particularly for healthcare workers and vulnerable individuals. In some places, due to low vaccination rates and new variants of SARS-CoV-2 emerging, psychosocial strategies for remaining resilient during an ongoing multi-faceted stressor are still needed. Elsewhere, thanks to successful vaccination campaigns, some countries have begun reopening but questions remain regarding how to best recover, adjust, and grow following the collective stress and loss caused by the pandemic.
Method:
Here, we briefly describe three evidence-based strategies that can help foster individual and collective recovery, growth, and resilience: cultivating social belonging, practicing compassion, and engaging in kindness.
Results:
Social belonging involves a sense of interpersonal connectedness. Practicing compassion involves perceiving suffering as part of a larger shared human experience and directing kindness toward it. Finally, engaging in kindness involves prosocial acts toward others.
Conclusions:
Together, these strategies can promote social connectedness and help reduce anxiety, stress, and depression, which may help psychologists, policymakers, and the global community remain resilience in places where cases are still high while promoting adjustment and growth in communities that are now recovering and looking to the future.
Keywords: social safety, social belonging, empathy, prosocial behavior, Coronavirus, COVID-19
Coronavirus disease 2019, commonly known as COVID-19, has affected the lives of countless people worldwide. Because this illness spreads primarily through close contact with persons infected with SARS-CoV-2 (Li et al., 2020), the primary global strategy for reducing the impact of COVID-19 has involved enacting physical distancing measures, such as cancelling large gatherings, closing businesses, restricting travel, and sheltering in place (Hsiang et al., 2020). These policies have been vital for protecting public health, but they have also degraded the social fabric and financial stability that are integral for sustaining mental health (Pieh et al., 2020; Wilson et al., 2020). Black and marginalized communities have been particularly affected, given the fact that the chronic stress of the pandemic has been compounded by events involving racial injustice and inequity (Schad et al., 2021; Snowden & Graaf, 2020). As a result of experiencing these complex stressors, the global community has recently witnessed a notable rise in anxiety, depression, posttraumatic stress disorder, burnout, grief, and suicide (Bertuccio & Runion, 2020; d’Ettorre et al., 2021; Gruber & Rottenberg, 2020; Gruber et al., 2020), particularly among frontline workers, caregivers, vulnerable (e.g., low socioeconomic) populations, and BIPOC communities (Centers for Disease Control and Prevention, 2021; Gallagher & Wetherell, 2020; Snowden & Graaf, 2020; Valenzuela et al., 2020).
In countries such as India and Brazil that have distributed relatively few vaccines to date, COVID-19 is still widespread and shows few signs of waning. Here, the main psychosocial question involves what individuals can do to foster resilience (i.e., healthy adjustment despite chronically aversive circumstances) while experiencing the chronic, multi-faceted stressor that is the COVID-19 pandemic (Luthar & Cicchetti, 2000). In other areas of the world such as the United States, where new daily case rates have declined, society has begun reopening, raising the question of how individuals can best recovery from this chronic, life-altering stressor. As Dedoncker et al. (2021), Zaki (2021), and others have suggested, this transition also provides a unique opportunity to grow by identifying new techniques for bolstering resilience and reconsidering what life should look like in order to achieve a more healthy, sustainable, equitable, and enjoyable future. To help accomplish these goals, we briefly describe three key evidence-based strategies that psychologists, policymakers, and individuals can use to promote psychosocial resilience during the pandemic, as well as recovery, adjustment to a new normal, and growth after the pandemic subsides. These strategies involve cultivating social belonging, practicing compassion, and engaging in kindness.
Social Belonging
Social belonging involves a sense of deep connectedness, affiliation, and integration with a social group or community (Allen et al., 2021). The importance of connecting deeply with others and cultivating a sense of belonging has become even more apparent as the ability to do so has been greatly affected by shelter-in-place orders and isolating practices that have restricted or eliminated in-person interactions (Okruszek et al., 2020). Yet, social belonging remains one of the most important psychosocial strategies for promoting resilience and fostering recovery, adjustment, and growth.
In more typical (i.e., non-pandemic) times, social belonging has been found to be associated with decreases in loneliness, depression, anxiety, pain, sleep disruption, hypertension, fatigue, cognitive dysfunction, and suicide, as well as with a reduced likelihood of early mortality (Cacioppo & Patrick, 2008; Fisher et al., 2015; Holt-Lunstad et al., 2017; Taylor & Broffman, 2011). In response to adverse circumstances, belonging has been related to a lower likelihood of experiencing posttraumatic stress and greater resilience following traumas (Muldoon et al., 2019). In addition to fulfilling the human need for relatedness with others, social belonging can provide important coping resources (e.g., the availability of social support), which can help buffer against the negative effects of adversity and even foster social growth and strengthen relational bonds (Layous & Nelson, Coffey, 2020; Levine, 2003). Moreover, greater social belonging helps shift the body’s biological resources away from a threat-related pro-inflammatory state, which reduces risk for anxiety disorders, depression, cardiovascular disease, and autoimmune and neurodegenerative disorders, and toward a more anti-viral state, which decreases individuals’ susceptibility to viruses such as the common cold and, possibly, COVID-19 (Cohen, 2020; Furman et al., 2019; Shields et al., 2020; Slavich, 2020).
Social belonging can be pursued with others at home as well as outside the home. In the home, meaningfully connecting with family members by (for example) cooking together, engaging in activities and hobbies, and setting aside time for mindful conversations can all foster a sense of belonging within the family. In turn, fostering social belonging with others outside the home can be pursued by increasing social connection virtually using technologies and software platforms that promote collective resilience when in-person interactions are not possible (e.g., Marzouki et al., 2021). Virtual interactions such as these can occur while using social media and participating in virtual events like birthday parties, playdates, work meetings, religious ceremonies, book clubs, and exercise or yoga classes over live videoconference. When and where it is safe to do so, it will be important for recovery to prioritize the reintroduction of in-person interactions with others.
Additionally, research has found that interventions that target the subjective sense of group inclusion and cohesion by shifting focus to shared experiences may also increase social belonging and, by doing so, can reduce the gap in opportunity disparities experienced by marginalized groups (e.g., Walton & Cohen, 2011; Walton et al., 2012). These perceptions can be altered by individuals, psychologists, and even public health officials. For example, individuals can choose to reframe adverse situations to focus on common humanity and psychologists can encourage clients to do the same. Similarly, public health initiatives that focus on the shared experience of going through a challenging time—combined with the shared goal of safely resuming in-person gatherings—may increase perceptions of social belonging during the COVID-19 pandemic while also improving public health and wellness.
Compassion
A second evidence-based strategy for building psychosocial resilience during times of recurrent or chronic stress and recovering once a stressor has passed is the practice of compassion. Although physically separate and from varying backgrounds, people from all around the world are presently going through shared experiences of anxiety, fear, and uncertainty that, for many, will persist into the foreseeable future as a result of the COVID-19 pandemic (Pfefferbaum & North, 2020). This is where the practice of fostering compassion can be helpful, as it involves recognizing suffering, perceiving that suffering as part of a larger shared human experience (i.e., common humanity) and directing kindness toward it in an effort to alleviate suffering (Goetz et al., 2010; Strauss et al., 2016). By doing so, compassion can help reduce perceived stress and increase individuals’ positive affect and sense of connectedness (Hofmann et al., 2011).
Researchers have described two basic forms of compassion: compassion toward others (Gilbert, 2009) and compassion toward the self (i.e., self-compassion; Neff, 2003; Strauss et al., 2016). Compassion for others can act as a motivator for prosociality toward individuals who need emotional or practical support. In a pandemic, compassion can therefore promote a sense of social connectedness and help to ensure that individuals’ most basic medical needs will be met: that people, especially the vulnerable, have access to necessary resources like facemasks, healthcare, housing, and food. Without compassion for others, it is less likely that these fundamental requirements for humane living will be realized during the pandemic. Compassion for others also has the potential to enhance the ability for disadvantaged and disenfranchised groups to recover and adjust adaptively to the “new normal” upon re-entry. Compassion for the self, in turn, can reduce feelings of anxiety, fear, and aloneness by focusing the mind on shared struggles (Neff, 2003). Self-compassion has been shown to increase individuals’ ability to cope with major stressors, including chronic illness (Sirois et al., 2015; Zessin et al., 2015), and can aid in achieving both recovery and growth following trauma (e.g., Hiraoka et al., 2015; Wong & Yeung, 2017).
Moreover, both compassion for others and self-compassion are skills that can be developed using contemplative practices like mindfulness, loving-kindness, and compassion meditation (Neff et al., 2007). These practices, in turn, have been shown to increase positive emotions and social connectedness, and to decrease distress, depression, systemic inflammation and inflammatory responses to stress, and markers of biological aging (Black & Slavich, 2016; Galante al., 2014; Hutcherson et al., 2008; Pace et al., 2009). Following the pandemic, policymakers and psychologists can also help to aid recovery by framing COVID-19 as a collective experience and by describing it and the recovery process through an empathetic, mutually supportive lens. For example, following the September 11th attacks in the United States, an initiative arose to create the “9/11 National Day of Service” in an effort to highlight the spirit of togetherness and compassion observed in the immediate aftermath of the attacks, as well as to inspire unity and offer assistance to those in need. Something similar could be done for the COVID-19 pandemic.
Kindness
Finally, individual and collective resilience to COVID-19 can be developed by promoting kindness (Zaki, 2019). Kindness involves engaging in voluntary prosocial acts (e.g., acting friendly and generously) driven by compassion or concern for others (Peterson & Seligman, 2004), and involves activities such as donating time, money, expertise, or services to important causes, as well as helping care for vulnerable family members, friends, or neighbors. Adversity is known to inspire prosocial acts such as these (Vollhardt, 2009), and the COVID-19 pandemic appears to be one such case, with individuals engaging in widespread acts of kindness and prosocial behavior as evidenced by the recent creation of “mutual aid” spreadsheets in which people have offered to help their more vulnerable neighbors and others in need (Samuel, 2020). At first glance, prosocial acts like these seem like a transfer, whereby one person sacrifices so another can benefit. Well-being, however, is not a zero-sum exchange, and research has consistently demonstrated that when people help others, they experience greater happiness, satisfaction, and self-worth, as well as better health (Aknin et al., 2020; Dunn et al., 2008; Krause, 2016).
Likewise, studies have shown that prosocial behavior, especially when accompanied by a sense of emotional connection and when done out of concern for others, increases helpers’ happiness and self-efficacy, and can decrease feelings of stress and depression (Crocker, Canevello, & Brown, 2017), thus making kindness a powerful tool for maintaining well-being both during and after the COVID-19 pandemic. In addition, research has found that striving to support and not harm others reduces neuroendocrine responding to stress (Abelson et al., 2014) and elicits growth following collective trauma (Tingey et al., 2017). Acting kindly thus not only benefits others but also has the potential to reduce givers’ risk for stress-related health problems.
In addition, individuals should remember that physical distancing when public health officials deem it necessary is itself a prosocial act. Especially for relatively young, healthy individuals, keeping physically distant from others is an important way to protect members of the community who are at elevated risk for COVID-19, such as older adults and persons with preexisting chronic disease conditions (Rahman & Jahan Sathi, 2020; Zheng et al., 2020). Thinking of these actions as prosocial has been shown to increase individuals’ willingness to distance (Jordan et al., 2020); as such, public health officials reframing physical isolation as a necessary act of solidarity and togetherness may help promote perceptions of social integration and belonging in the face of the COVID-19 pandemic. Additionally, individuals can participate in home-based community volunteer efforts when doing so in person would present a risk. These home-based activities can include cooking meals for shelters, creating care packages, sending thoughtful cards to struggling friends or family members, donating to relief funds, and offering digital assistance (e.g., social media outreach, content sharing) for service organizations.
Conclusion
In conclusion, the COVID-19 pandemic has caused unprecedented disruptions to peoples’ social routines and economic security that may endure for some time, especially as outbreaks of different variants of SARS-CoV-2 occur (Kissler et al., 2020). These disruptions have already led to notable increases in psychiatric symptoms (Gruber & Rottenberg, 2020; Gruber et al., 2020; Torales et al., 2020), highlighting the need to identify evidence-based strategies that can be used to foster resilience in countries that are still in the throes of the pandemic, as well as recovery and growth in places that are now recovering. By promoting social belonging and practicing compassion and kindness, psychologists, policymakers, and individual citizens can not only decrease peoples’ risk for this terrible disease but also increase the global community’s collective sense of togetherness, efficacy, and resilience while enhancing adjustment to the “new normal” and promoting psychosocial growth from this multi-faceted life stressor.
Figure 1.
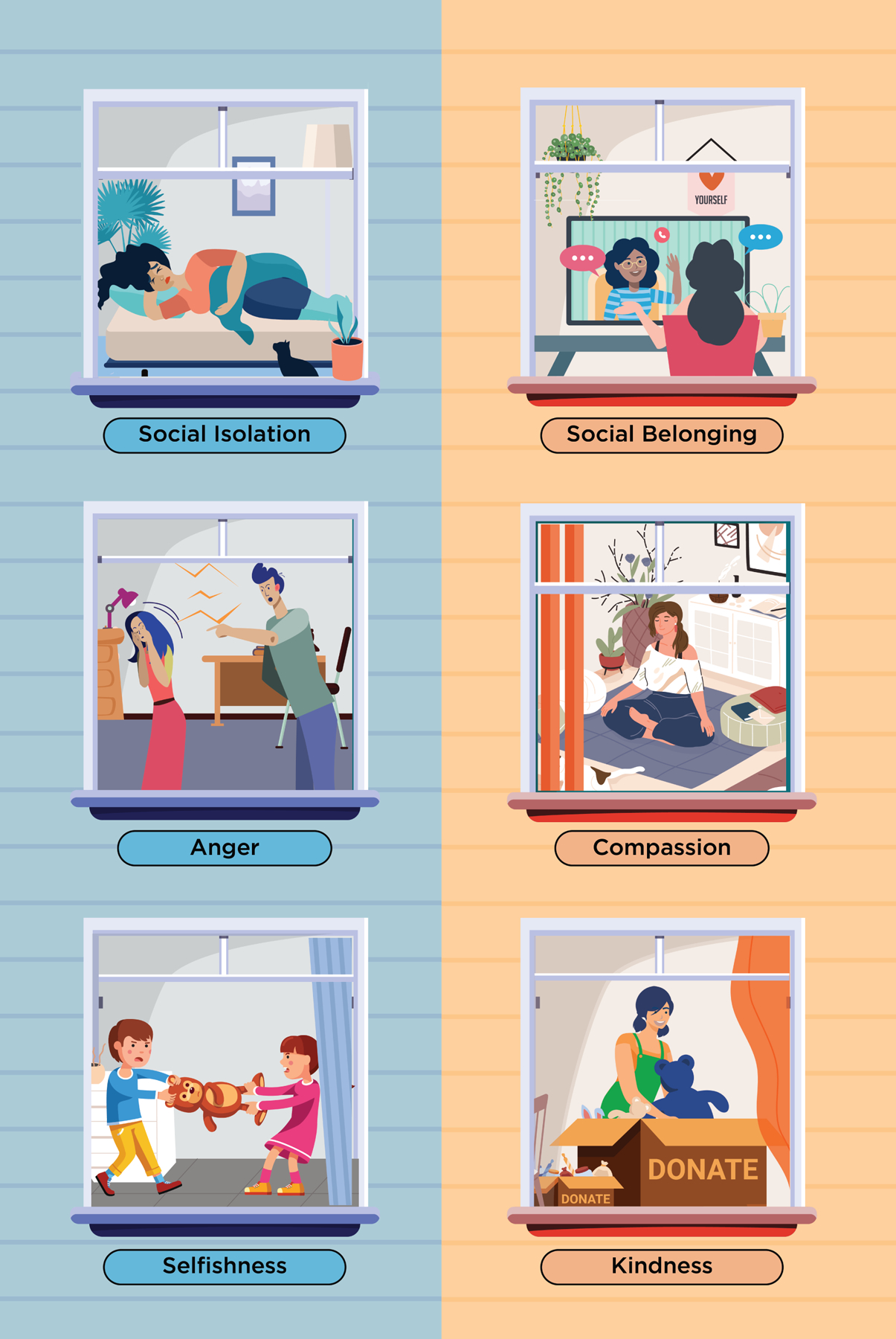
Evidence-based strategies for promoting individual and collective resilience during the COVID-19 pandemic, as well as recovery and growth following the pandemic. They include fostering social belonging, compassion, and kindness.
Funding source:
George Slavich was supported by a Society in Science—Branco Weiss Fellowship, NARSAD Young Investigator Grant #23958 from the Brain & Behavior Research Foundation, and National Institutes of Health grant K08 MH103443. Jamil Zaki was supported by National Science Foundation CAREER Award BCS-1454518 and National Institute of Mental Health R01 MH112560. These organizations had no role in the preparation, review, or approval of the manuscript, or the decision to submit the manuscript for publication.
Footnotes
Declaration of interests: The authors report no conflicts of interest with regard to this article.
References
- Abelson JL, Erickson TM, Mayer SE, Crocker J, Briggs H, Lopez-Duran NL, & Liberzon I (2014). Brief cognitive intervention can modulate neuroendocrine stress responses to the Trier Social Stress Test: Buffering effects of a compassionate goal orientation. Psychoneuroendocrinology, 44, 60–70. 10.1016/j.psyneuen.2014.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aknin L, Dunn E, Proulx J, Lok I, & Norton MI (2020). Does spending money on others promote happiness?: A registered replication report. Journal of Personality and Social Psychology, 119, e15–e26. 10.1037/pspa0000191 [DOI] [PubMed] [Google Scholar]
- Allen KA, Kern ML, Rozek CS, McInerney DM, & Slavich GM (2021). Belonging: A review of conceptual issues, an integrative framework, and directions for future research. Australian Journal of Psychology, 73, 87–102. 10.1080/00049530.2021.1883409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertuccio RF & Runion MC (2020). Considering grief in mental health outcomes of COVID-19. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S87–S89. 10.1037/tra0000723 [DOI] [PubMed] [Google Scholar]
- Black DS, & Slavich GM (2016). Mindfulness meditation and the immune system: A systematic review of randomized controlled trials. Annals of the New York Academy of Sciences, 1373, 13–24. 10.1111/nyas.12998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, & Patrick W (2008). Loneliness: Human nature and the need for social connection. WW Norton & Company. [Google Scholar]
- Centers for Disease Control and Prevention. (2021, April 19). Health equity considerations and racial and ethnic minority groups. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html
- Cohen S (2020). Psychosocial vulnerabilities to upper respiratory infectious illness: Implications for susceptibility to coronavirus disease 2019 (COVID-19). Perspectives on Psychological Science, 16, 161–174. 10.1177/1745691620942516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crocker J, Canevello A, & Brown AA (2017). Social motivation: Costs and benefits of selfishness and otherishness. Annual Review of Psychology, 68, 299–325. 10.1146/annurev-psych-010416-044145 [DOI] [PubMed] [Google Scholar]
- Dedoncker J, Vanderhasselt MA, Ottaviani C, & Slavich GM (2021). Mental health during the COVID-19 pandemic and beyond: The importance of the vagus nerve for biopsychosocial resilience. Neuroscience and Biobehavioral Reviews, 125, 1–10. 10.1016/j.neubiorev.2021.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Ettorre G, Ceccarelli G, Santinelli L, Vassalini P, Innocenti GP, Alessandri F, Koukopoulos AE, Russo A, d’Ettorre G, & Tarsitani L (2021). Post-traumatic stress symptoms in healthcare workers dealing with the COVID-19 pandemic: A systematic review. International Journal of Environmental Research and Public Health, 18, 601. 10.3390/ijerph18020601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn EW, Aknin LB, & Norton MI (2008). Spending money on others promotes happiness. Science, 319, 1687–1688. 10.1126/science.1150952 [DOI] [PubMed] [Google Scholar]
- Fisher LB, Overholser JC, Ridley J, Braden A, & Rosoff C (2015). From the outside looking in: Sense of belonging, depression, and suicide risk. Psychiatry, 78(1), 29–41. 10.1080/00332747.2015.1015867 [DOI] [PubMed] [Google Scholar]
- Furman D, Campisi J, Verdin E, Carrera-Bastos P, Targ S, Franceschi C, … & Slavich GM (2019). Chronic inflammation in the etiology of disease across the life span. Nature Medicine, 25, 1822–1832. 10.1038/s41591-019-0675-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galante J, Galante I, Bekkers M-J, & Gallacher J (2014). Effect of kindness-based meditation on health and well-being: A systematic review and meta-analysis. Journal of Consulting and Clinical Psychology, 82, 1101–1114. 10.1037/a0037249 [DOI] [PubMed] [Google Scholar]
- Gallagher S, & Wetherell MA (2020). Risk of depression in family caregivers: Unintended consequences of COVID-19. BJPsych Open, 6(6): 3119. 10.1192/bjo.2020.99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert P (2009). The compassionate mind. London: Constable & Robinson. [Google Scholar]
- Goetz JL, Keltner D, & Simon-Thomas E (2010). Compassion: An evolutionary analysis and empirical review. Psychological Bulletin, 136, 351–374. 10.1037/a0018807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber J, Prinstein MJ, Clark LA, Rottenberg J, Abramowitz JS, Albano AM, … & Weinstock LM (2020). Mental health and clinical psychological science in the time of COVID-19: Challenges, opportunities, and a call to action. American Psychologist. 10.1037/amp0000707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber J, & Rottenberg J (2020). Flattening the mental health curvey is the next big coronavirus challenge. Retrieved September 8, 2020, from: https://theconversation.com/flattening-the-mental-health-curve-is-the-next-big-coronavirus-challenge-139066
- Hiraoka R, Meyer EC, Kimbrel NA, DeBeer BB, Gulliver SB, & Morissette SB (2015). Self-compassion as a prospective predictor of PTSD symptom severity among trauma-exposed U.S. Iraq and Afghanistan war veterans. Journal of Traumatic Stress, 28, 127–133. 10.1002/jts.21995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Grossman P, & Hinton DE (2011). Loving-kindness and compassion meditation: Potential for psychological interventions. Clinical Psychology Review, 31, 1126–1132. 10.1016/j.cpr.2011.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Robles TF, & Sbarra DA (2017). Advancing social connection as a public health priority in the United States. American Psychologist, 72, 517–530. 10.1037/amp0000103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsiang S, Allen D, Annan-Phan S, Bollinger I, Chong T, Druckenmiller H, … & Wu T (2020). The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature 584, 262–267. 10.1038/s41586-020-2404-8 [DOI] [PubMed] [Google Scholar]
- Hutcherson CA, Seppala EM, & Gross JJ (2008). Loving-kindness meditation increases social connectedness. Emotion, 8, 720–724. 10.1037/a0013237 [DOI] [PubMed] [Google Scholar]
- Jordan J, Yoeli E, & Rand DG (2020, April 3). Don’t get it or don’t spread it? Comparing self-interested versus prosocially framed COVID-19 prevention messaging. 10.31234/osf.io/yuq7x [DOI] [PMC free article] [PubMed]
- Kissler S, Tedijanto C, Goldstein E, Grad Y, & Lipsitch M (2020). Projecting the transmission dynamics of SARS-CoV-2 through the post-pandemic period. Science, 368, 860–868. 10.1126/science.abb5793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause N (2016). Providing emotional support to others, self-esteem, and self-rated health. Archives of Gerontology and Geriatrics, 65, 183–191. 10.1016/j.archger.2016.03.014 [DOI] [PubMed] [Google Scholar]
- Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, … & Xing X (2020). Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. New England Journal of Medicine, 382, 1199–1207. 10.1056/NEJMoa2001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Layous K, & Nelson-Coffey SK (2020). The effect of perceived social support on personal resources following minor adversity: An experimental investigation of belonging affirmation. Personality and Social Psychology Bulletin. 10.1177/0146167220961270 [DOI] [PubMed] [Google Scholar]
- Levine S (2003). Psychological and social aspects of resilience: a synthesis of risks and resources. Dialogues in Clinical Neuroscience, 5, 273–280. 10.31887/DCNS.2003.5.3/slevine [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS & Cicchetti D (2000). The construct of resilience: Implications for interventions and social policies. Developmental Psychopathology, 12, 857–885. 10.1017/s0954579400004156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marzouki Y, Aldossari FS & Veltri GA (2021). Understanding the buffering effect of social media use on anxiety during the COVID-19 pandemic lockdown. Humanities & Social Sciences Communications 8, 47. 10.1057/s41599-021-00724-x [DOI] [Google Scholar]
- Muldoon OT, Haslam SA, Haslam C, Cruwys T, Kearns M & Jetten J (2019). The social psychology of responses to trauma: Social identity pathways associated with divergent traumatic responses. European Review of Social Psychology, 30, 311–348. 10.1080/10463283.2020.1711628 [DOI] [Google Scholar]
- Neff KD (2003). Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity, 2, 85–101. 10.1080/15298860309032 [DOI] [Google Scholar]
- Neff KD, Kirkpatrick KL, & Rude SS (2007). Self-compassion and adaptive psychological functioning. Journal of Research in Personality, 41, 139–154. 10.1016/j.jrp.2006.03.004 [DOI] [Google Scholar]
- Okruszek Ł, Aniszewska-Stańczuk A, Piejka A, Wiśniewska M, & Żurek K (2020). Safe but lonely? Loneliness, anxiety, and depression symptoms and COVID-19. Frontiers in Psychology, 11, 579181. 10.3389/fpsyg.2020.579181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace TW, Negi LT, Adame DD, Cole SP, Sivilli TI, Brown TD, Issa MJ, & Raison CL (2009). Effect of compassion meditation on neuroendocrine, innate immune and behavioral responses to psychosocial stress. Psychoneuroendocrinology, 34, 87–98. 10.1016/j.psyneuen.2008.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson C, & Seligman MEP (2004). Character strengths and virtues: A handbook and classification. Washington, DC: American Psychological Assocaition/Oxford University Press. [Google Scholar]
- Pfefferbaum B, & North CS (2020). Mental health and the Covid-19 pandemic. New England Journal of Medicine, 383, 510–512. 10.1056/NEJMp2008017 [DOI] [PubMed] [Google Scholar]
- Pieh C, O’Rourke T, Budimir S, & Probst T (2020). Relationship quality and mental health during COVID-19 lockdown. PLOS One, 15(9):e0238906. 10.1371/journal.pone.0238906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A, & Jahan Sathi N (2020). Risk factors of the severity of COVID-19: A meta-analysis. medRxiv 2020.04.30.20086744. 10.1101/2020.04.30.20086744 [DOI] [PubMed] [Google Scholar]
- Samuel S (2020, April 16). How to help people during the pandemic, one Google spreadsheet at a time. Vox. Retrieved September 8, 2020, from https://www.vox.com/future-perfect/2020/3/24/21188779/mutual-aid-coronavirus-covid-19-volunteering
- Schad A, Layton RL, Ragland D, & Cook JG (2021). Uncovering the compounding effects of COVID-19 and racism on mental health disparities among biomedical PhD and MD students. medRxiv 2021.04.29.21251164. 10.1101/2021.04.29.21251164 [DOI] [Google Scholar]
- Shields GS, Spahr CM, & Slavich GM (2020). Psychosocial interventions and immune system function: A systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry, 77, 1031–1043. 10.1001/jamapsychiatry.2020.0431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirois FM, Molnar DS, & Hirsch JK (2015). Self-compassion, stress, and coping in the context of chronic illness. Self and Identity, 14, 334–347. 10.1080/15298868.2014.996249 [DOI] [Google Scholar]
- Slavich GM (2020). Social safety theory: A biologically based evolutionary perspective on life stress, health, and behavior. Annual Review of Clinical Psychology, 16, 265–295. 10.1146/annurev-clinpsy-032816-045159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snowden LR, & Graaf G (2020). COVID-19, social determinants past, present, and future, and African Americans’ health. Journal of Racial and Ethnic Health Disparities, 8, 12–20. 10.1007/s40615-020-00923-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss C, Lever Taylor B, Gu J, Kuyken W, Baer R, Jones F, & Cavanagh K (2016). What is compassion and how can we measure it? A review of definitions and measures. Clinical Psychology Review, 47, 15–27. 10.1016/j.cpr.2016.05.004 [DOI] [PubMed] [Google Scholar]
- Taylor SE. & Broffman JI (2011). Psychosocial resources: Functions, origins, and links to mental and physical health. Advances in Experimental Social Psychology, 44, 1–57. 10.1016/B978-0-12-385522-0.00001-9 [DOI] [Google Scholar]
- Tingey JL, McGuire AP, Stebbins OL, & Erickson TM (2017). Moral elevation and compassionate goals predict posttraumatic growth in the context of a college shooting. The Journal of Positive Psychology, 14, 261–270. 10.1080/17439760.2017.1402077 [DOI] [Google Scholar]
- Torales J, O’Higgins M, Castaldelli-Maia JM, & Ventriglio A (2020). The outbreak of COVID-19 coronavirus and its impact on global mental health. International Journal of Social Psychiatry, 66, 317–320. 10.1177/0020764020915212 [DOI] [PubMed] [Google Scholar]
- Walton GM, & Cohen GL (2011). A brief social-belonging intervention improves academic and health outcomes of minority students. Science, 331(6023), 1447–1451. 10.1126/science.1198364 [DOI] [PubMed] [Google Scholar]
- Walton GM, Cohen GL, Cwir D, & Spencer SJ (2012). Mere belonging: The power of social connections. Journal of Personality and Social Psychology, 102, 513–532. 10.1037/a0025731 [DOI] [PubMed] [Google Scholar]
- Wilson JM, Lee J, Fitzgerald HN, Oosterhoff B, Sevi B, & Shook NJ (2020). Job insecurity and financial concern during the COVID-19 pandemic are associated with worse mental health. Journal of Occupational and Environmental Medicine, 62, 686–691 10.1097/JOM.0000000000001962 [DOI] [PubMed] [Google Scholar]
- Wong CCY, & Yeung NCY (2017). Self-compassion and posttraumatic growth: Cognitive processes as mediators. Mindfulness, 8, 1078–1087. 10.1007/s12671-017-0683-4 [DOI] [Google Scholar]
- Valenzuela J, Crosby LE, & Harrison RR (2020). Reflections on the COVID-19 pandemic and health disparities in pediatric psychology. Journal of Pediatric Psychology, 45, 839–841. 10.1093/jpepsy/jsaa063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vollhardt JR (2009). Altruism born of suffering and prosocial behavior following adverse life events: A review and conceptualization. Social Justice Research, 22, 53–97. 10.1007/s11211-009-0088-1 [DOI] [Google Scholar]
- Zaki J (2019). The war for kindness: Building empathy in a fractured world. New York: Crown. [Google Scholar]
- Zaki J (2021). Habits of kindness that will endure: Disasters shock us into remembering our shared humanity. The Wall Street Journal. Retrieved May 21, 2021 from https://www.wsj.com/articles/habits-of-kindness-that-will-endure-11585368061 [Google Scholar]
- Zessin U, Dickhäuser O, & Garbade S (2015). The relationship between self‐compassion and well‐being: A meta‐analysis. Applied Psychology: Health and Well‐Being, 7, 340–364. 10.1111/aphw.12051 [DOI] [PubMed] [Google Scholar]
- Zheng Z, Peng F, Xu B, Zhao J, Liu H, Peng J, … & Ye C (2020). Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. Journal of Infection, 81, e16–e25. 10.1016/j.jinf.2020.04.021 [DOI] [PMC free article] [PubMed] [Google Scholar]


