Abstract
Objective:
To investigate the influence of caries infiltrant preconditioning on the shear bond strength of orthodontic resin cements on sound and demineralized enamel.
Materials and Methods:
Stainless-steel brackets were bonded to sound or artificially demineralized (14 d, acidic buffer, pH 5.0) bovine enamel specimens using a resin cement or a combination of caries infiltrant preconditioning (Icon, DMG) and the respective resin cement (light-curing composite: Heliosit Orthodontic, Transbond XT, using either Transbond XT Primer or Transbond Plus Self Etching Primer; light-curing resin-modified glass ionomer cement: Fuji Ortho; or self-curing composite: Concise Orthodontic Bonding System). Each group consisted of 15 specimens. Shear bond strength was evaluated after thermo-cycling (10,000×, 5°C to 55°C) at a crosshead speed of 1 mm/min, and data were statistically analyzed by analysis of variance, Mann-Whitney test, and Weibull statistics. Adhesive Remnant Index (ARI) scores and enamel fractures were determined at 25× magnification and were statistically analyzed by regression analyses (P < .05).
Results:
The caries infiltrant system significantly increased the shear bond strength of Transbond XT Primer, Transbond Plus Self Etching Primer, and Fuji Ortho in sound specimens, and of all resin cements except for the Concise Orthodontic Bonding System in demineralized enamel. Overall, caries infiltrant preconditioning decreased significantly the number of enamel fractures, but it did not affect ARI scores.
Conclusion:
Preconditioning of sound and demineralized enamel with the caries infiltrant system did not impair but rather increased the shear bond strength of most orthodontic resin cements while decreasing the risk of enamel fracture at debonding.
Keywords: Enamel, Orthodontic resin, Shear bond strength, Caries infiltrant
INTRODUCTION
The fixation of orthodontic brackets enhances plaque retention and thus favors the development of demineralization and initial caries around the brackets when the oral hygiene of the patient is poor. Different attempts have been made to increase the caries resistance of enamel prior to and during fixed orthodontic treatment (eg, application of fluoride or casein-phosphopeptide-amorphous calcium phosphate1–4). Schmidlin et al.5 suggested the use of an adhesive patch as an intermediate layer under metal brackets to prevent demineralization under and around the bracket and to relocate the bracket-patch margins to areas that are easier to access for oral hygiene. In addition, the use of different (fluoridated) bonding agents and sealants has been discussed4,6,7 as a means to protect the surrounding enamel from demineralization. However, enamel white spot lesions not only develop during orthodontic treatment but might be present even at the start of orthodontic treatment. Tufekci et al.8 and Gorelick et al.9 found 11% and 24% patients, respectively, with existing white spot lesions at the time of bracket fixation. Thus, preventive strategies in orthodontics also include, easires to remineralize previously demineralized enamel to allow for bracket fixation.10
In recent years, low-viscosity resins with a high capability for penetrating initial caries lesions have been increasingly studied. Clinical trials11,12 showed that the caries progression of infiltrated lesions is significantly reduced. Although originally developed for penetration into carious lesions and occlusion of diffusion pathways, the resin infiltrant also prevented enamel surface demineralization to some extent.13 Moreover, existing white spot lesions might be covered and provided with increased stability10,14; thus, bond strength of brackets might be increased compared to that of demineralized enamel without pretreatment.10
As a result of the sealing effect on sound enamel and the stabilization of demineralized enamel, it is conceivable that the caries infiltration technique may be beneficial as a form of pretreatment prior to bracket fixation. Therefore, the purpose of this study was to investigate the influence of caries infiltrant preconditioning on the shear bond strength of orthodontic resin cements on sound and demineralized enamel. The null hypothesis was that preconditioning with the caries infiltration system does not reduce the shear bond strength of orthodontic cements.
MATERIALS AND METHODS
Specimen Preparation
Three hundred cylindrical enamel specimens (6.6 mm in diameter) were prepared from the labial surface of freshly extracted bovine crowns, embedded in chemically cured acrylic resin (ScandiQuick, ScanDia, Hagen, Germany), and ground flat with P 180 silica-carbide (SiC) paper (Struers, Willich, Germany). The surfaces were polished under water cooling with 500 SiC paper (Struers).
Half of the specimens were demineralized in an acidic buffer (pH 5.0, 37°C15) for 14 days to create artificial caries-like lesions. The buffer solution was renewed every second day to keep the pH constant. Sound and demineralized specimens were randomly allocated into 10 groups each (n = 15).
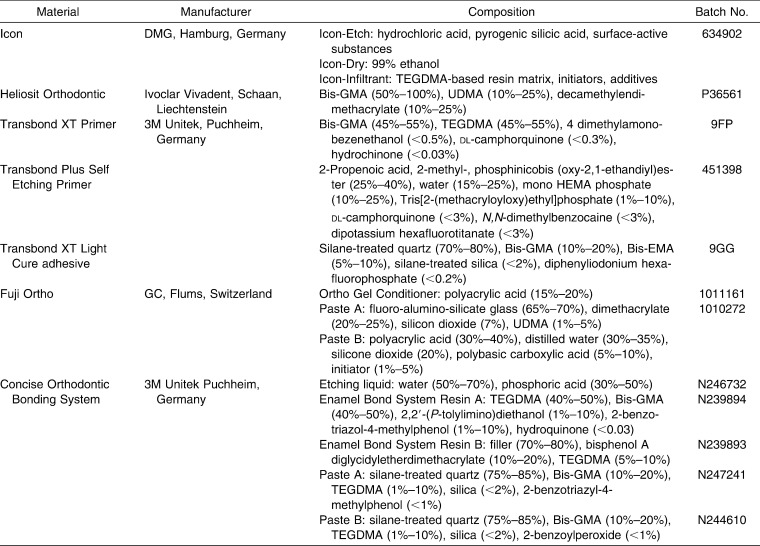
Bonding Procedure and Application of Brackets
Stainless-steel brackets for central lower incisors (Discovery, slot 0.56 × 0.76 mm/22 × 30, 8.71-mm2 surface area bracket base; Dentaurum, Ispringen, Germany) were bonded to the sound or demineralized specimens using either one of the resin cements or a combination of caries infiltrant (Icon, DMG, Hamburg, Germany) preconditioning and the respective resin cement. The resin cements comprised two light-curing composites (Heliosit Orthodontic, Ivoclar Vivadent, Schaan, Liechtenstein, Transbond XT, 3M Unitek, Puchheim, Germany), one light-curing resin-modified glass-ionomer cement (Fuji Ortho, GC, Flums, Switzerland) and one self-curing composite (Concise Orthodontic Bonding System). The resin cement Transbond XT was used either after conventional etching and application of Transbond XT primer or after applying a self-etching primer (Transbond Plus Self Etching Primer, 3M Unitek, Puchheim, Germany). The compositions of the materials are presented in Table 1.
Table 1. .
Composition of Materials Used
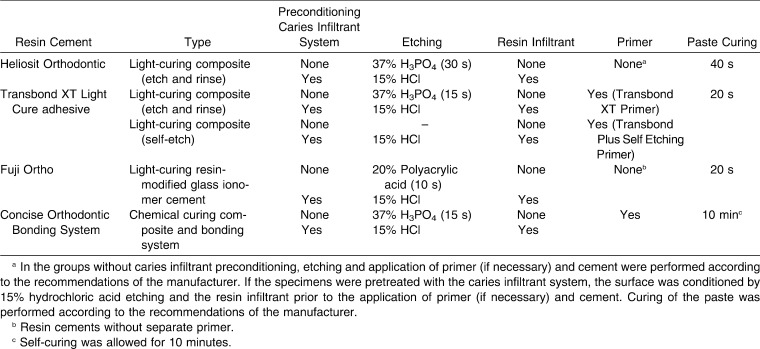
Preconditioning with the caries infiltrant included hydrochloric acid etching (15% HCl, 2 minutes; Icon Etch, DMG), water rinsing (30 seconds), surface drying by ethanol (30 seconds, Icon Dry, DMG), and application of a low-viscosity resin infiltrant (Icon Infiltrant, DMG). The resin infiltrant was applied twice (for 3 minutes and 1 minute); each application was followed by light-curing (800 W/cm2 bluephase; Ivoclar Vivadent, Schaan, Liechtenstein) for 40 seconds at 2-mm distance to the surface. In half of the sound or demineralized enamel groups, respectively, specimens were preconditioned with the caries infiltrant system prior to resin cement application, while in the remaining groups the brackets were bonded using the resin cements according to the manufacturers' recommendations (Table 2).
Table 2. .
Treatment of Sound or Demineralized Enamel with the Resin Cement or a Combination of Caries Infiltrant System and Resin Cementa
The brackets were fixed on the specimens with a standardized load of 500 g. Excess material was carefully removed with microbrushes at 2.5× magnification. Light-curing of the cements was performed according to the manufacturers' recommendations at a distance of 5 mm. The self-curing system Concise Orthodontic Bonding System (3M Unitek, Puchheim, Germany) was allowed to set for 10 minutes.
Shear Bond Strength Measurement
Prior to shear bond strength testing, the specimens were thermo-cycled 10,000 times between 5°C and 55°C (Willytec, Gräfelfing, Germany; dwell time: 20 seconds in each bath; transfer time: 10 seconds).
The shear bond test was performed with a universal testing machine (Z010, Zwick, Ulm, Germany). A shear force was applied through a chisel-shaped loading device at a crosshead speed of 1 mm/min parallel to the specimen's surface. Load at fracture was recorded, and shear bond strength was calculated according to the following equation: S = F/A, where S is shear bond strength, F is load at failure (N), and A represents the adhesive area (mm2) (TestXpert 11.02, Zwick).
The debonded area was examined with a stereomicroscope at 25× magnification (M3B, Wild, Heerbrugg, Switzerland) for assessment of the Adhesive Remnant Index (ARI) and enamel fractures.16 ARI scores ranged from 0 to 3, as follows: 0 = no adhesive was left on the enamel surface; 1 = less than half of the adhesive was left on the enamel; 2 = half or more of the adhesive was left on the enamel; and 3 = all of the adhesive was left on the enamel.
Statistical Analysis
Mean shear bond strength (±standard deviation) for each group was computed. Kolmogorov-Smirnov and Shapiro-Wilk tests were applied to check the assumption of normality. Although data were not normally distributed in two of 20 groups, data were analyzed by three-way analysis of variance (ANOVA)—the factors being the substrate (sound/demineralized enamel), the pretreatment mode, and the kind of primer/resin cement—to check for possible interactions. As all factors and interactions were found to be significant, two-way ANOVAs were further applied within sound and demineralized enamel groups, the factors being the pretreatment mode and the kind of primer/resin cement.
Mann-Whitney tests were applied to analyze differences between specimens with and without caries infiltrant preconditioning (separately for the primers/resin cements and the substrate). Differences between the primers/resin cements were analyzed by Kruskal-Wallis tests (separately for sound and demineralized specimens and specimens with and without caries infiltrant preconditioning) followed by pairwise Mann-Whitney tests and Bonferroni correction. Differences between shear bond strength values of sound and demineralized enamel groups were also analyzed by Mann-Whitney tests.
Weibull statistics (Weibull modulus m, characteristic bond strength σo) were calculated using the maximum likelihood estimation method at a 95% confidence level (MINITAB, State College, Penn).
To analyze the effect of the caries infiltrant preconditioning on ARI scores and enamel fractures, data were statistically analyzed by ordinal or linear regression analysis, respectively. For all tests, the level of significance was set at P < .05.
RESULTS
The shear bond strength values of sound and demineralized enamel groups are presented in Figure 1. Three- and two-way ANOVAs showed all factors and all interactions to be significant with respect to shear bond strength (P < .004).
Figure 1. .
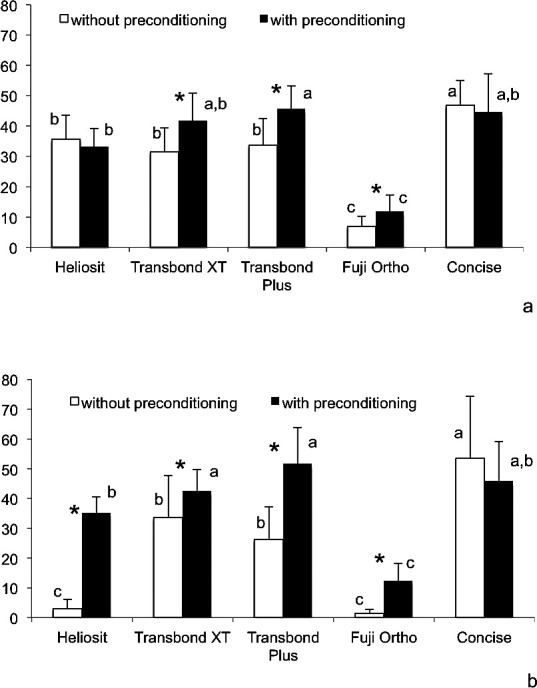
Shear bond strength (mean ± standard deviation, MPa) of sound (a) and demineralized (b) enamel. Within each primer/resin cement combination, significant differences between enamel with and without caries infiltrant preconditioning are marked by an asterisk. Significant differences between the primers/resin cements are marked with different small letters within sound and demineralized enamel separately for groups with and without caries infiltrant preconditioning.
Preconditioning with the caries infiltrant system increased the shear bond strength of Transbond XT Primer (P = .009), Transbond Plus Self Etching Primer (P = .001), and Fuji Ortho (P = .011) in sound specimens and the shear bond strength of all resin cements (P < .009) except for the Concise Orthodontic Bonding System (P = .265) in demineralized enamel. Generally, the lowest shear bond strength values were observed for Fuji Ortho, independent of the preconditioning and the substrate (sound or demineralized enamel). Without caries infiltrant preconditioning, the shear bond strength of Heliosit Orthodontic (P < .001) and Fuji Ortho (P < .001) was significantly reduced in demineralized compared to sound enamel. All other comparisons between sound and demineralized enamel were not significantly different.
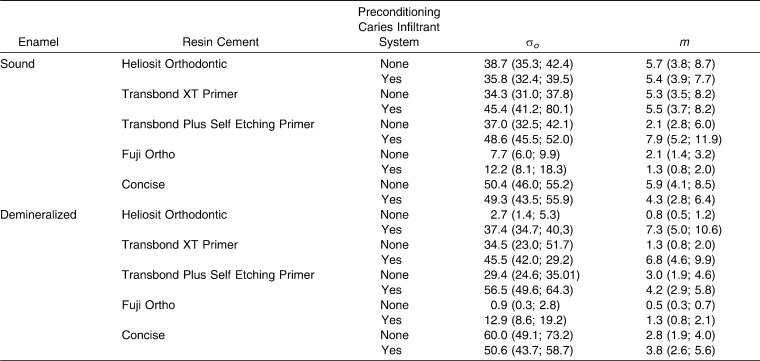
The Weibull parameters are presented in Table 3. In most groups, characteristic strength (σo values) increased when specimens were preconditioned with the caries infiltrant system. Weibull moduli m were remarkably low in groups in which brackets were bonded with Fuji Ortho and when Heliosit Orthodontic and Transbond XT Primer were used on demineralized enamel without Icon preconditioning.
Table 3. .
Weibull Parameters: Characteristic Strength σo (MPa) and Weibull Modulus m and their 95% Confidence Intervals in the Different Groups
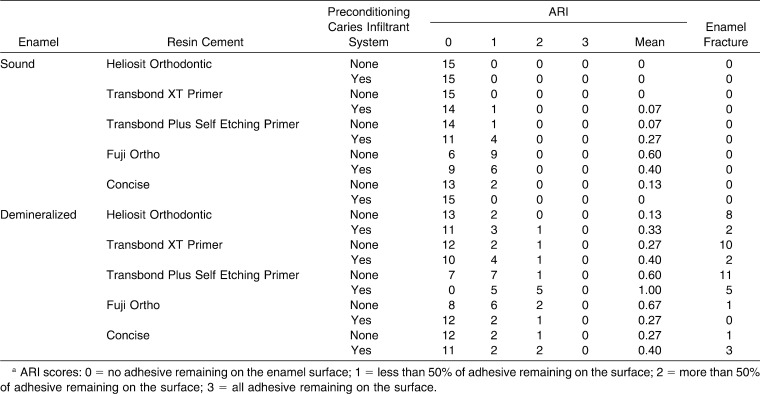
ARI scores and enamel fractures are presented in Table 4. Regression analyses revealed that preconditioning with the caries infiltrant system was significant with respect to enamel fractures but not with respect to the ARI scores. Enamel fractures occurred only in demineralized enamel but were significantly reduced when specimens were preconditioned with Icon. ARI scores with and without caries infiltrant preconditioning were not significantly different within each primer/resin cement combination.
Table 4. .
Adhesive Remnant Index (ARI; Distribution and Mean) and Frequency of Enamel Fractures in the Different Groupsa
DISCUSSION
For the first time a caries infiltrant system was used for preconditioning of sound and artificially demineralized enamel prior to bracket fixation. The null hypothesis cannot be rejected, as Icon preconditioning did not reduce, but rather even increased, the shear bond strength of some of the resin cements.
The results of the present study are promising, as the preconditioning with the caries infiltrant system enhanced shear bond strength in most groups and reduced the frequency of enamel fractures in demineralized enamel at bracket debonding. In light of previous studies showing that the caries infiltrant system reduced the progression of initial caries lesions and protected both sound and demineralized enamel from acid dissolution, this indicates that the range of application of the caries infiltrant system might be extended to the preconditioning of enamel prior to fixed orthodontic treatment.
Shear bond strength was tested on bovine enamel, which has been proposed as a suitable alternative for human enamel in shear bond strength testing, although slightly different values between human and bovine enamel have been shown.17 Artificial carious lesions were created according to the methods of previous studies18,19 and exhibit the typical histological structure of initial enamel caries (intact surface layer, lesion body, demineralization front).20 Moreover, they have the advantage of a higher homogeneity, allowing for a better standardization than is associated with natural lesions in human teeth. Preconditioning with the caries infiltrant system followed the recommendations of the manufacturers; thus, enamel was etched with hydrochloric acid for 120 seconds. As the surface layer of artificial caries lesions is slightly thinner compared to that of natural lesions, it might be assumed that extensive etching with hydrochloric acid not only removes the surface layer but also induces a breakdown of the lesion. However, in fact it was shown14 that hydrochloric acid etching for 120 seconds does remove the surface layer of artificial lesions without destroying the underlying structure. Complete removal of the surface layer was shown21 to be essential for the penetration of the TEGDMA-based resin infiltrant (triethylene glycol dimethacrylate).
Preconditioning with the caries infiltrant system increased the shear bond strength of the resin cements on artificial enamel lesions, most likely as a result of a deeper penetration of the resin infiltrant into the body of the lesion, compared to the primer or paste, respectively, of the orthodontic cements. The frequency of fractures in demineralized enamel was significantly reduced compared to that of specimens without Icon preconditioning, indicating a stabilizing effect of the resin infiltrant.
Monomer formulations with an increased TEGDMA content have a high penetration capability22 and were shown to induce the formation of a thick oxygen-inhibited layer,23 which probably allows a chemical connection of the resin infiltrant to the monomers of the primer or paste. Conventional adhesives are able to penetrate carious lesions to some extent; thus, it is assumed that the primers of the tested systems also might partly penetrate demineralized enamel and strengthen the outermost part of the infiltrated enamel when applied after Icon preconditioning. However, Concise was shown to exhibit a relatively high penetration coefficient,24 which might explain why this material did not benefit from the preconditioning with the caries infiltrant system.
From the results of this study it becomes evident that, in particular, resin cements without an additional primer (Heliosit Orthodontic and Fuji Ortho) benefit from preconditioning with the caries infiltration system, as their penetration capability is limited,24 probably as a result of the significant amount of bisphenol-A glycol dimethacrylate (Bis-GMA) and urethane dimethacrylate (UDMA22) (Heliosit Orthodontic) and the high filler content (Fuji Ortho),25 respectively. In the case of Fuji Ortho, penetration into demineralized enamel is further hampered, as etching with polyacrylic acid is less efficient compared to phosphoric acid,26 likely resulting in incomplete removal of the intact surface layer. In addition, the acidic monomers of self-etching adhesives were shown27 to be unable to erode the surface layer of artificial enamel lesions adequately to allow for penetration of the adhesive.
For these reasons, the penetration of Transbond Plus Self Etching Primer might be distinctly increased by etching with hydrochloric acid during Icon preconditioning, resulting in significantly higher shear bond strength values. Even on sound enamel, preconditioning with the caries infiltrant system had a slightly positive effect on shear bond strength, probably as a result of the high wettability of the TEGDMA resin.22
The results were confirmed by the Weibull statistics, which mostly showed higher characteristic strength σo values when specimens were preconditioned with the caries infiltrant system. As lower Weibull moduli indicate larger variation in measured strengths and poorer reliability of a material, the shear bond strength data in specimens bonded with Fuji Ortho and in demineralized enamel bonded with Heliosit Orthodontic and Transbond XT Primer without Icon preconditioning should be interpreted with caution.
Overall, bond strength was not impaired but rather was enhanced by caries infiltrant preconditioning, confirming the results of previous studies,18,19 which showed that caries infiltrant application increased shear bond strength values of etch-and-rinse and self-etching adhesives. From a clinical point of view it is of relevance that the frequency of enamel fractures at debonding was decreased by the preconditioning, while at the same time the ARI scores were not significantly changed, indicating that the amount of residual resin to be removed at debonding is not affected by this technique.
CONCLUSION
Preconditioning with the caries infiltrant system increased the shear bond strength of most orthodontic resins to sound and demineralized enamel; at the same time, the risk of enamel fractures at debonding was reduced and the amount of residual resin remained unchanged.
Acknowledgment
The study was supported by DMG, Germany.
REFERENCES
- 1.Uysal T, Amasyali M, Koyuturk AE, Ozcan S. Effects of different topical agents on enamel demineralization around orthodontic brackets: an in vivo and in vitro study. Aust Dent J. 2010;55:268–274. doi: 10.1111/j.1834-7819.2010.01233.x. [DOI] [PubMed] [Google Scholar]
- 2.Farhadian N, Miresmaeili A, Eslami B, Mehrabi S. Effect of fluoride varnish on enamel demineralization around brackets: an in-vivo study. Am J Orthod Dentofacial Orthop. 2008;133:S95–S98. doi: 10.1016/j.ajodo.2006.09.050. [DOI] [PubMed] [Google Scholar]
- 3.Stecksen-Blicks C, Renfors G, Oscarson ND, Bergstrand F, Twetman S. Caries-preventive effectiveness of a fluoride varnish: a randomized controlled trial in adolescents with fixed orthodontic appliances. Caries Res. 2007;41:455–459. doi: 10.1159/000107932. [DOI] [PubMed] [Google Scholar]
- 4.Benson PE, Parkin N, Millett DT, Dyer FE, Vine S, Shah A. Fluorides for the prevention of white spots on teeth during fixed brace treatment. Cochrane Database Syst Rev. 2004;3:CD003809. doi: 10.1002/14651858.CD003809.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Schmidlin PR, Schatzle M, Fischer J, Attin T. Bonding of brackets using a caries-protective adhesive patch. J Dent. 2008;36:125–129. doi: 10.1016/j.jdent.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Paschos E, Kleinschrodt T, Clementino-Luedemann T, et al. Effect of different bonding agents on prevention of enamel demineralization around orthodontic brackets. Am J Orthod Dentofacial Orthop. 2009;135:603–612. doi: 10.1016/j.ajodo.2007.11.028. [DOI] [PubMed] [Google Scholar]
- 7.Sudjalim TR, Woods MG, Manton DJ, Reynolds EC. Prevention of demineralization around orthodontic brackets in vitro. Am J Orthod Dentofacial Orthop. 2007;131:e1–e9. doi: 10.1016/j.ajodo.2006.09.043. [DOI] [PubMed] [Google Scholar]
- 8.Tufekci E, Dixon JS, Gunsolley JC, Lindauer SJ. Prevalence of white spot lesions during orthodontic treatment with fixed appliances. Angle Orthod. 2011;81:206–210. doi: 10.2319/051710-262.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gorelick L, Geiger AM, Gwinnett AJ. Incidence of white spot formation after bonding and banding. Am J Orthod Dentofacial Orthop. 1982;81:93–98. doi: 10.1016/0002-9416(82)90032-x. [DOI] [PubMed] [Google Scholar]
- 10.Attin R, Stawarczyk B, Kecik D, Knosel M, Wiechmann D, Attin T. Shear bond strength of brackets to demineralize enamel after different pretreatment methods. Angle Orthod. 2012;82:56–61. doi: 10.2319/012311-48.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martignon S, Ekstrand KR, Gomez J, Lara JS, Cortes A. Infiltrating/sealing proximal caries lesions: a 3-year randomized clinical trial. J Dent Res. 2012;91:288–292. doi: 10.1177/0022034511435328. [DOI] [PubMed] [Google Scholar]
- 12.Paris S, Hopfenmuller W, Meyer-Lueckel H. Resin infiltration of caries lesions: an efficacy randomized trial. J Dent Res. 2010;89:823–826. doi: 10.1177/0022034510369289. [DOI] [PubMed] [Google Scholar]
- 13.Schmidlin PR, Sener B, Attin T, Wiegand A. Protection of sound enamel and artificial enamel lesions against demineralisation: caries infiltrant versus adhesive. J Dent. In press doi: 10.1016/j.jdent.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 14.Belli R, Rahiotis C, Schubert EW, Baratieri LN, Petschelt A, Lohbauer U. Wear and morphology of infiltrated white spot lesions. J Dent. 2011;39:376–385. doi: 10.1016/j.jdent.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 15.Buskes JAKM, Christoffersen J, Arends J. Lesion formation and lesion remineralization in enamel under constant composition conditions—a new technique with applications. Caries Res. 1985;19:490–496. doi: 10.1159/000260887. [DOI] [PubMed] [Google Scholar]
- 16.Lalani N, Foley TF, Voth R, Banting D, Mamandras A. Polymerization with the argon laser: curing time and shear bond strength. Angle Orthod. 2000;70:28–33. doi: 10.1043/0003-3219(2000)070<0028:PWTALC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Yassen GH, Platt JA, Hara AT. Bovine teeth as substitute for human teeth in dental research: a review of literature. J Oral Sci. 2011;53:273–282. doi: 10.2334/josnusd.53.273. [DOI] [PubMed] [Google Scholar]
- 18.Jia L, Stawarczyk B, Schmidlin PR, Attin T, Wiegand A. Effect of caries infiltrant application on shear bond strength of different adhesive systems to sound and demineralized enamel. J Adhes Dent. In press doi: 10.3290/j.jad.a25685. [DOI] [PubMed] [Google Scholar]
- 19.Wiegand A, Stawarczyk B, Kolakovic M, Hammerle CH, Attin T, Schmidlin PR. Adhesive performance of a caries infiltrant on sound and demineralised enamel. J Dent. 2011;39:117–121. doi: 10.1016/j.jdent.2010.10.010. [DOI] [PubMed] [Google Scholar]
- 20.Magalhaes AC, Moron BM, Comar LP, Wiegand A, Buchalla W, Buzalaf MAR. Comparison of cross-sectional hardness and transverse microradiography of artificial carious enamel lesions induced by different demineralising solutions and gels. Caries Res. 2009;43:474–483. doi: 10.1159/000264685. [DOI] [PubMed] [Google Scholar]
- 21.Meyer-Lueckel H, Paris S, Kielbassa AM. Surface layer erosion of natural caries lesions with phosphoric and hydrochloric acid gels in preparation for resin infiltration. Caries Res. 2007;41:223–230. doi: 10.1159/000099323. [DOI] [PubMed] [Google Scholar]
- 22.Paris S, Meyer-Lueckel H, Colfen H, Kielbassa AM. Penetration coefficients of commercially available and experimental composites intended to infiltrate enamel carious lesions. Dent Mater. 2007;23:742–748. doi: 10.1016/j.dental.2006.06.029. [DOI] [PubMed] [Google Scholar]
- 23.Shawkat ES, Shortall AC, Addison O, Palin WM. Oxygen inhibition and incremental layer bond strengths of resin composites. Dent Mater. 2009;25:1338–1346. doi: 10.1016/j.dental.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 24.Knox J, Jones ML, Hubsch P, Middleton J. The influence of orthodontic adhesive properties on the quality of orthodontic attachment. Angle Orthod. 2000;70:241–246. doi: 10.1043/0003-3219(2000)070<0241:TIOOAP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 25.Moszner N, Salz U, Zimmermann J. Chemical aspects of self-etching enamel-dentin adhesives: a systematic review. Dent Mater. 2005;21:895–910. doi: 10.1016/j.dental.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 26.Shinya M, Shinya A, Lassila LVJ, et al. Treated enamel surface patterns associated with five orthodontic adhesive systems—surface morphology and shear bond strength. Dent Mater J. 2008;27:1–6. doi: 10.4012/dmj.27.1. [DOI] [PubMed] [Google Scholar]
- 27.Mueller J, Meyer-Lueckel H, Paris S, Hopfenmuller W, Kielbassa AM. Inhibition of lesion progression by the penetration of resins in vitro: influence of the application procedure. Oper Dent. 2006;31:338–345. doi: 10.2341/05-39. [DOI] [PubMed] [Google Scholar]