Supplemental Digital Content is available in the text.
Keywords: coronavirus disease, long-term care hospitals, mechanical ventilation, weaning
Abstract
OBJECTIVES:
To describe the clinical characteristics and outcomes of adult patients with coronavirus disease 2019 requiring weaning from prolonged mechanical ventilation.
DESIGN:
Observational cohort study of patients admitted to two long-term acute care hospitals from April 1, 2020, to March 31, 2021.
SETTING:
Two long-term acute care hospitals specialized in weaning from prolonged mechanical ventilation in the Chicagoland area, Illinois, United States.
PATIENTS:
Adult (≥ 18 yr old) ICU survivors of respiratory failure caused by severe acute respiratory syndrome coronavirus 2 pneumonia receiving prolonged mechanical ventilation.
INTERVENTIONS:
None.
MEASUREMENTS AND MAIN RESULTS:
During the study period, 158 consecutive patients were transferred to the long-term acute care hospitals for weaning from prolonged ventilation. Demographic, clinical, and laboratory data were collected and analyzed. Final date of follow-up was June 1, 2021. Prior to long-term acute care hospital transfer, median length of stay at the acute care hospital was 41.0 days and median number of ventilator days was 35. Median age was 60.0 years, 34.8% of patients were women, 91.8% had a least one comorbidity, most commonly hypertension (65.8%) and diabetes (53.2%). The percentage of weaning success was 70.9%. The median duration of successful weaning was 8 days. Mortality was 9.6%. As of June 1, 2021, 19.0% of patients had been discharged home, 70.3% had been discharged to other facilities, and 1.3% were still in the long-term acute care hospitals.
CONCLUSIONS:
Most patients with coronavirus disease 2019 transferred to two Chicago-area long-term acute care hospitals successfully weaned from prolonged mechanical ventilation.
As of June 1, 2021, more than 33 million laboratory-confirmed cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection have been recorded in the United States (1). The cumulative U.S. hospitalization rate for adults with coronavirus disease 2019 (COVID-19) is 709 per 100,000 population (2). Up to 30% of hospitalized patients with COVID-19 are started on invasive ventilation for severe pneumonia (3–7). Invasive ventilation in these patients (8–10) portend a poor prognosis as approximately 40% of them do not survive hospitalization (3, 5–7, 11–14). For those who survive, the duration of ventilatory support is prolonged (11, 13–15). When the clinical condition stabilizes, patients with COVID-19 receiving prolonged mechanical ventilation are commonly transferred to long-term acute care hospitals (LTACHs) for further care (16).
The clinical characteristics and outcomes of COVID-19 patients cared for in the ICU have been detailed in several reports (5, 6, 11, 12, 17–21). There is limited information pertaining to COVID-19 patients once they have been transferred to an LTACH (16). Accordingly, the goal of this study was to describe, for the first time, the clinical characteristics and outcomes of a cohort of mechanically ventilated patients with COVID-19 who survived acute care hospitalization and were then transferred to two Chicago-area LTACHs during the first 12 months of the city’s outbreak for weaning from prolonged mechanical ventilation.
MATERIALS AND METHODS
See the Electronic Supplementary Material (http://links.lww.com/CCM/G593) for additional details.
We conducted this study at RML Specialty Hospital-Hinsdale, a 115-bed free-standing LTACH located in a Chicago suburb, and RML Specialty Hospital-Chicago, a 69-bed free-standing LTACH in Chicago. The Institutional Review Board at RML Specialty Hospital approved the investigation (FXL 004).
All patients with respiratory failure caused by SARS-CoV-2 pneumonia admitted to the LTACHs between April 1, 2020, and March 31, 2021, for weaning from prolonged ventilation (≥ 4 d plus tracheostomy) (22, 23) were included in the investigation. We prospectively reviewed patients’ medical records. When data of interest were missing, we contacted the primary team caring for the patient to obtain the information (18). Postal codes were used to determine whether patients lived in areas where the percentage of low-income residents exceeds the Illinois benchmark of 29.4%, as defined by the Uniform Data System Mapper (24).
Assessed clinical outcomes included: 1) respiratory status (ventilator dependence, spontaneous breathing), 2) functional status (basic mobility and self-care functioning quantified using the Activity Measure for Post-Acute Care (AM-PAC) Inpatient Short Form) (25), 3) discharge location (home, nursing home, rehabilitation hospital, acute care hospital), 4) LTACH mortality, and 5) need for home mechanical ventilation. Clinical outcomes were monitored until LTACH discharge or no later than June 1, 2021, the final date of follow-up. Patients were considered weaning successes when they breathed without ventilator assistance for at least five consecutive days by day 45 of LTACH admission (26). All other patients were considered weaning failures.
Categorical variables were reported as percentages and continuous variables as medians and interquartile ranges (IQRs). Comparison of continuous variables was performed using the Mann-Whitney U test. chi-square or Fisher exact test were used for categorical variables as appropriate. Statistical significance was assumed at two-tailed p values of less than 0.05. Sample size and power calculations were not feasible owing to the lack of published data on LTACH outcomes for this illness (27). Accordingly, the sample size was equal to the number of COVID-19 patients transferred to the LTACHs during the study period (7, 11, 12, 18). All analyses were done using SPSS 23 (IBM SPSS, Armonk, NY).
RESULTS
Patient Characteristics
During the study period, 215 consecutive COVID-19 patients were transferred to the LTACHs. One-hundred fifty-eight of these patients had respiratory failure caused by SARS-CoV-2 pneumonia and required weaning from prolonged ventilation. The median age of these patients was 60.0 years (IQR, 53.0–70.0 yr); 55 (34.8%) were women (Table 1). Two-thirds had a history of hypertension, over half were diabetic, and more than one-third were obese (body mass index ≥ 30). Seventy-four patients (46.8%) were Hispanic, 36 (22.8%) were Black, and 39 (24.7%) were White non-Hispanics. Nearly two-thirds of all patients resided in low-income areas (e-Table 1, http://links.lww.com/CCM/G593). Hispanic and Black patients were about twice as likely to live in low-income areas as White patients (e-Table 1, http://links.lww.com/CCM/G593). The median length of stay in the acute care hospital of origin was 41.0 days (IQR, 33.0–54.0 d) and the median number of ventilator days prior to transfer was 35.0 days (IQR, 27.0–46.0 d).
LTACH Outcomes
The percentage of weaning success was 70.9%. The median duration of weaning (weaning success only) was 8.0 days (IQR, 4.0–15.0 d). During LTACH stay, the most common complications were healthcare-associated pneumonia (20.3% of patients) followed by septic shock (10.8% of patients), cardiac arrest (7.0% of patients), and gastrointestinal bleeding (6.3% of patients).
Overall, LTACH mortality was 9.6%. As expected (28), mortality in the success group was less than in the failure group (1.8% and 29.5%, respectively; p < 0.0001) Table 1). As of June 1, 2021, two patients (1.3%) were still in the LTACHs and 141 patients (89.2%) had been discharged alive: 30 (19.0%) home, 73 (46.2%) to a rehabilitation facility, 27 (17.1%) had been transferred to an acute care hospital, and 11 (7.0%) to a nursing home. No patient discharged home required mechanical ventilation.
Table 1.
Patient Demographics and Characteristics
| Characteristics | Total Participants (n = 158) | Weaning Success (n = 112) | Weaning Failure (n = 46) | p a |
|---|---|---|---|---|
| Age, yr | 60.0 (53.0–70.0) | 59.0 (51.0–69.8) | 63.5 (56.8–71.0) | 0.034 |
| Gender, female/male (%female) | 55/103 (34.8%) | 42/70 (37.5%) | 13/33 (28.3%) | 0.268 |
| BMI | 28.6 (25.0–33.8) | 28.8 (25.6–34.2) | 27.7 (24.0–32.3) | 0.271 |
| Race | ||||
| Hispanic | 74 (46.8%) | 50 (44.6%) | 24 (52.2%) | 0.389 |
| Black | 36 (22.8%) | 26 (23.2%) | 10 (21.7%) | 0.841 |
| White non-Hispanic | 39 (24.7%) | 29 (25.9%) | 10 (21.7%) | 0.582 |
| Others | 9 (5.7%) | 7 (6.3%) | 2 (4.3%) | 0.805 |
| Acute Physiology and Chronic Health Evaluation II | 12.0 (8.0–17.0) | 10.0 (7.0–16.0) | 15 (11.8–18.3) | 0.001 |
| Do not resuscitate | 14 (8.9%) | 6 (5.4%) | 8 (17.4%) | 0.027 |
| Comorbidities | ||||
| Hypertension | 104 (65.8%) | 73 (65.2%) | 31 (67.4%) | 0.790 |
| Diabetes mellitus | 84 (53.2%) | 54 (48.2%) | 30 (65.2%) | 0.052 |
| Obesity (BMI ≥ 30) | 62 (39.2%) | 46 (41.1%) | 16 (34.8%) | 0.462 |
| Pulmonary disease | 29 (18.2%) | 23 (20.5%) | 6 (13.0%) | 0.269 |
| Cardiac disease | 27 (17.2%) | 16 (14.3%) | 11 (23.9%) | 0.151 |
| Malignancy | 10 (6.3%) | 7 (6.3%) | 3 (6.5%) | 0.949 |
| Hemodialysis | 6 (3.0%) | 3 (2.7%) | 3 (6.5%) | 0.358 |
| Clinical course in the acute care hospital of origin | ||||
| LOS, d | 41.0 (33.0–54.0) | 40.5 (32.0–51.0) | 43.0 (33.0–63.0) | 0.127 |
| MV, d | 35.0 (27.0–46.0) | 35.0 (27.3–45.8) | 35.5 (26.0–54.8) | 0.351 |
| LTACHs admission functional status | ||||
| Basic mobility (AM-PAC t Scale score) | 16.6 (16.6–19.4) | 16.6 (16.6–22.6) | 16.7 (16.7–16.7) | 0.0001 |
| Self-care functioning (AM-PAC t Scale score) | 17.1 (17.1–23.5) | 17.1 (17.1–23.3) | 17.1 (17.1–17.1) | 0.0003 |
| Course in the LTACHsb | ||||
| MV, d | 11.0 (5.8–26.0) | 9.5 (5.0–18.0) | 32 (6.8–63.5) | 0.0003 |
| LOS, d | 36.5 (26.3–60.0) | 39.0 (28.0–59.0) | 33.5 (8.8–73.0) | 0.118 |
| Mortality | 15 (9.6%) | 2 (1.8%) | 13 (29.5%) | < 0.0001 |
AM-PAC = Activity Measure for Post-Acute Care, BMI = body mass index, LOS = length of stay, LTACH = long-term acute care hospital, MV = mechanical ventilation.
aComparisons weaning success vs weaning failure only, Mann-Whitney U test was used for continuous variables, and χ2 test or Fisher exact test was used for categorical variables.
bData refers to patients discharged at the time of final assessment (Total n = 156, weaning successes n = 112, weaning failure n = 44).
Data are n (%) or median (interquartile range).
Median AM-PAC standardized scores (25) for basic mobility and self-care functioning at LTACH admission were 16.6 (IQR, 16.6–19.4) and 17.1 (IQR, 17.1–23.5), respectively (Table 1). These scores reflect a patient’s total need of assistance while performing basic mobility tasks such as rolling in bed and while performing daily activities such as toileting or brushing teeth (25). At LTACH discharge, basic mobility and daily activity scores had increased to 30.3 (IQR, 16.6–39.7) and 32.2 (IQR, 17.1–38.7) (p < 0.001 in both instances). In 55.1% and in 60.3% of patients, improvements in basic mobility and daily activity scores, respectively, were greater than the minimal detectable difference (29).
COVID-19 Testing During LTACH Stay
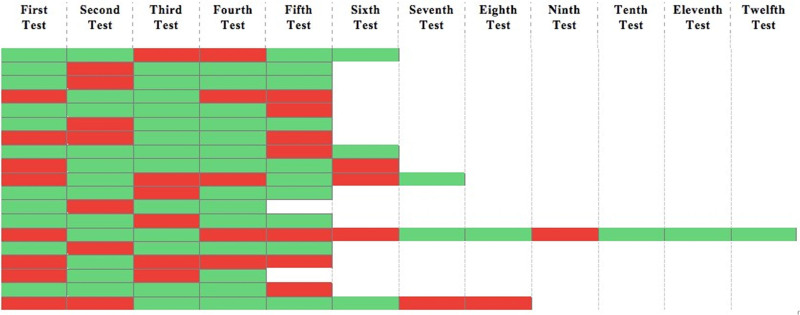
One-hundred nine patients (69.0%) underwent at least one target capture and transcription-mediated amplification assay SARS-CoV-2 test (nasopharyngeal swab) in the LTACH (see Electronic Supplementary Material, http://links.lww.com/CCM/G593, for details). Thirty-two (29.4%) of these tests were positive. In 78 patients, the test was repeated an average of four times at approximately 7-day intervals. In 45 of these patients (57.7%), repeated tests were either consistently positive (three patients, 3.8%) or consistently negative (42 patients, 53.8%). In 19 patients, the results of repeat tests were unstable—for example, test from negative became positive, and then again negative or vice versa (Fig. 1). The greatest number of LTACH days that a test was persistently positive was 28.
Figure 1.
Severe acute respiratory syndrome coronavirus 2 test results using target capture and transcription-mediated amplification in 19 patients who underwent nasal swabs more than once during long-term acute care hospital stay and in whom test results were unstable. Red = positive test. Green = negative test. Repeat tests were performed approximately 1 wk apart from each other.
DISCUSSION
This is the first study designed to describe clinical characteristics and outcomes of COVID-19 patients receiving prolonged mechanical ventilation from a large U.S. metropolitan area. All patients were transferred to two LTACHs during the initial 12 months of the COVID-19 outbreak. Most patients were Hispanic or Black men around 60 years old with hypertension and diabetes. Nearly 40% were obese. The 45-day weaning success rate was 70.9%. As of June 1, 2021, LTACH mortality was 9.6%.
Patient Characteristics
Over half of the cohort of patients had diabetes. The corresponding figure in the Chicago metropolitan area is estimated between 15.6% and 22.1% for middle age and older adults (30). The higher prevalence of diabetes in our patients than in the local population supports the association between diabetes and critical illness related to COVID-19 (5). Patients with diabetes were more likely to fail weaning from mechanical ventilation than those without diabetes (Table 1). This finding is consistent with previous reports documenting worse outcomes in patients with COVID-19 and diabetes (21, 31). The prevalence of obesity (39.2%) and hypertension (65.8%) in our patients is close to the range of the local prevalence of obesity (32.8–37.0%) and hypertension (40.8–63.3%) for middle age and older adults (30). This suggests that the high prevalence of these two conditions in our cohort of COVID-19 patients mostly reflects the population of origin.
The racial distribution in our cohort of patients was 46.8% Hispanic, 22.8% Black, and 24.7% White. The racial distribution in the Chicago metropolitan area consists of 29.9% Hispanic, 29.8% Black, and 32.9% White (30). Whether race per se is a risk factor for development of critical illness related to COVID-19 remains controversial (5, 7, 32). A key aspect to consider when deciphering the role of race on clinical outcomes includes income, living conditions (32), and access to healthcare of different racial groups (33). Most Hispanic and Black patients resided in low-income areas (68.9% and 75.0%, respectively, e-Table 1, http://links.lww.com/CCM/G593). Whether belonging to a specific racial group or having low income or a combination of the two portends higher likelihood of prolonged mechanical ventilation among survivors of critical illness related to COVID-19 remains to be determined.
LTACH Outcomes
Considering that this is the first investigation on LTACH weaning outcomes and mortality in COVID-19 patients, we cannot comment on how our results compare with the experience of other LTACHs both nationally and internationally. Similarly, it is difficult to assess how COVID-19 affects weaning outcome and mortality compared with patients without COVID-19 cared for in LTACH facilities. The rate of LTACH weaning success for non-COVID-19 patients reported in the last 24 years ranges from 38% to 87%, and LTACH mortality ranges from 7.6% to 50% (e-Table 2, http://links.lww.com/CCM/G593). This heterogeneity stems from several factors including varying definitions of weaning success across studies and systematic differences in patients’ selection for LTACH admission within a country (23) and among countries (34).
To explore the impact of COVID-19 on LTACH weaning outcome, we compared a subset of 56 COVID-19 patients and 56 non-COVID-19 patients with acute lung injury as the reason for intubation (acute lung injury being the presumed mechanism of respiratory failure caused by severe SARS-CoV-2 pneumonia) (35) (e-Table 3, http://links.lww.com/CCM/G593). Patients in the non-COVID-19 group had been admitted to our two LTACHs in the 12 months preceding the pandemic. The two groups were matched for age, gender, race group, and severity of disease at LTACH admission (Acute Physiology and Chronic Health Evaluation II scores). In this explorative subgroup analysis, COVID-19 patients had equivalent rates of LTACH weaning success and no difference in weaning duration or LTACH mortality compared with non-COVID-19 patients (e-Table 3, http://links.lww.com/CCM/G593). As it pertains to prognosis, the equivalent outcomes between COVID-19 and non-COVID-19 patients admitted to the two LTACHs suggest that the etiology of respiratory failure (i.e., acute lung injury) may be of more import than its upstream cause (i.e., SARS-CoV-2) (36, 37). This possibility is supported by the equivalent acute ICU mortality reported in a recent single-center U.K. investigation of ventilated patients with and without COVID-19 who fulfilled the Berlin criteria for acute respiratory distress syndrome (36).
During the first wave of the pandemic, weaning success rates of patients with COVID-19 cared for in acute ICUs ranged broadly (11–65.0%), as did mortality (23.3–81%) (11, 13, 18, 37–39). A contributing factor to this variability is the timing of assessment: day-28 of admission in some studies (18, 37, 39) and a fixed day of follow-up in others (11, 13, 38) (e-Table 4, http://links.lww.com/CCM/G593).
Total duration of mechanical ventilation (ventilator days in the acute ICU plus LTACH) among COVID-19 LTACH survivors in the current investigation was 51.5 days (IQR, 39.3–66.8 d). In contrast, duration of mechanical ventilation in acute COVID-19 ICU survivors ranges from approximately 14.0 days to approximately 27.0 days (4, 11, 14, 36, 37, 39) (e-Table 4, http://links.lww.com/CCM/G593). This signifies that most of our patients were further away from the time of initial lung injury. Furthermore, our patients were, by definition, acute ICU survivors. These two factors introduce selection bias, limiting comparison between acute ICU and LTACH patients with COVID-19. The much lower LTACH mortality of our patients (9.6%) compared with acute ICU studies (23.3–81%) (11, 13, 18, 37–39) may reflect this bias. Despite these limitations, our data suggest that survival of COVID-19 patients beyond the acute ICU may portend a high likelihood of successful weaning from mechanical ventilation and of LTACH survival.
At LTACH admission, patient basic mobility, such as rolling in bed, and self-care functioning, such as toileting, were severely impaired (Table 1). Severe impairment in mobility and self-care functioning at LTACH admission are common (40–44) and are associated with worse clinical outcomes including lower probability to remain ventilator-free (40, 43) and higher mortality (43). All COVID-19 patients in our investigation underwent physical and occupational therapy according to LTACHs standard of care (see Electronic Supplementary Material, http://links.lww.com/CCM/G593, for details) and, as expected (40–44), their basic mobility and self-care functioning improved over LTACH stay. In more than half of patients, these improvements were greater than the AM-PAC standard minimal detectable difference (indicating a minimum change beyond measurement error) (29), yet, at LTACH discharge, patients still required in excess of 60% assistance to perform basic mobility and self-care functioning tasks. Not surprisingly, over 80% of COVID-19 patients discharged alive from the LTACH did not go home but were transferred to a rehabilitation center or a nursing home, or an acute care hospital. These figures are similar to those reported in non-COVID patients (28, 45, 46), emphasizing the protracted negative impact of critical illness.
The prominent physical impairment and the need for prolonged ventilatory support also highlight the important role of LTACHs during the ongoing pandemic especially during periods of high acute ICU occupancy. To increase the available ICU resources in the regional acute care hospitals, our LTACHs developed an organizational model similar to what was recently described by Grigonis et al (16). The two LTACHs, having served the Chicago metropolitan area for more than 30 years, relied on the already well-established working relationships with regional acute care hospitals. Second, the LTACHs maintain on-site high acuity units. This allowed for the ongoing care of COVID-19 patients who became unstable, minimizing the burden on acute-care ICUs. Third, via a series of organizational steps, the two LTACHs maximized capacity while maintaining patient and healthcare staff safety (see Electronic Supplementary Material, http://links.lww.com/CCM/G593, for details), resulting in two LTACHs operating at virtually full capacity for most of the last 12 months.
SARS-CoV-2 Testing During LTACH Admission
For infection-control purposes and to assist in the disposition of patients, the primary team obtained serial nasopharyngeal swabs for SARS-CoV-2 testing approximately once a week. In 57.7% of patients, the tests were either consistently negative or positive first and then negative. In contrast, in 24.4% patients test results were variable over time (Fig. 1). The mechanisms that might be responsible for such fluctuation include deficiency in sampling technique, reinfection, laboratory error, and prolonged nucleic acid conversion (47). It follows that a negative nasopharyngeal swab specimen cannot be considered as the sole indicator to inform decisions on isolation, recovery, discharge, and transferring of LTACH patients. It is unclear whether tracheal aspirates or mini bronchoalveolar lavage may have a greater diagnostic yield than nasopharyngeal or oropharyngeal swabs (48). Furthermore, it is unknown whether traces of virus detected by nucleic acid amplification tests equate to live virus capable of transmission (49).
Strengths and Limitations
We prospectively identified patients and collected data. Accordingly, our findings reflect the outbreak of COVID-19 in the Chicago metropolitan area, a region that has been very severely affected by the pandemic with 10,535 cases and 204.3 deaths per 100,000 residents to date (50). Data collection was concurrent with ongoing patient care. If we encountered missing or uncertain information in the medical records, we could contact the primary team for clarification (18). This minimized the number of missing data and enhanced the internal validity of the investigation.
The study was geographically confined to the Chicago metropolitan area. This limits the generalizability to LTACH settings elsewhere in the United States and abroad. Data on weaning outcome were complete by the final date of follow-up. In contrast, data anchored to LTACH discharge such as patient disposition and mortality were available in 98.7% of patients (two patients are still cared for in the LTACHs). Any comparison with weaning outcomes of non-COVID-19 patients cared for in the same LTACHs must be considered only hypothesis generating (51, 52). Finally, the analyses have not been adjusted for multiple comparisons (5, 12), and given the possibility of type I error, the findings should be interpreted as exploratory (12).
CONCLUSIONS
Most COVID-19 patients transferred to two Chicago-area LTACHs successfully weaned from prolonged mechanical ventilation.
Supplementary Material
Footnotes
*See also p. 341.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
Dr. Undevia received funding from Springer. The remaining authors have disclosed that they do not have any potential conflicts of interest.
Data collection was done at RML Specialty Hospitals. Data analysis and article preparation was performed at each of the above institutions.
REFERENCES
- 1.Centers for Disease Control and Prevention: Coronavirus Disease 2019 (COVID 19): Cases in the U.S. 2021. Available at: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html. Accessed June 1, 2021
- 2.Centers for Disease Control and Prevention: COVID-NET; A Weekly Summary of U.S. COVID-19 Hospitalization Data. 2020. Available at: https://covid.cdc.gov/covid-data-tracker/#covidnet-hospitalization-network. Accessed June 1, 2021
- 3.Richardson S, Hirsch JS, Narasimhan M, et al. ; the Northwell COVID-19 Research Consortium: Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020; 323:2052–2059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.King CS, Sahjwani D, Brown AW, et al. : Outcomes of mechanically ventilated patients with COVID-19 associated respiratory failure. PLoS One. 2020; 15:e0242651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Petrilli CM, Jones SA, Yang J, et al. : Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: Prospective cohort study. BMJ. 2020; 369:m1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Argenziano MG, Bruce SL, Slater CL, et al. : Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: Retrospective case series. BMJ. 2020; 369:m1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Suleyman G, Fadel RA, Malette KM, et al. : Clinical characteristics and morbidity associated with coronavirus disease 2019 in a series of patients in metropolitan detroit. JAMA Netw Open. 2020; 3:e2012270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tobin MJ, Laghi F, Jubran A: Caution about early intubation and mechanical ventilation in COVID-19. Ann Intensive Care. 2020; 10:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tobin MJ, Laghi F, Jubran A: P-SILI is not justification for intubation of COVID-19 patients. Ann Intensive Care. 2020; 10:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tobin MJ: The criteria used to justify endotracheal intubation of patients with COVID-19 are worrisome. Can J Anaesth. 2021; 68:258–259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cummings MJ, Baldwin MR, Abrams D, et al. : Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: A prospective cohort study. Lancet. 2020; 395:1763–1770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grasselli G, Zangrillo A, Zanella A, et al. ; COVID-19 Lombardy ICU Network: Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020; 323:1574–1581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Auld SC, Caridi-Scheible M, Blum JM, et al. : ICU and ventilator mortality among critically ill adults with coronavirus disease 2019. Crit Care Med. 2020; 48:e799–e804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doidge JC, Gould DW, Ferrando-Vivas P, et al. : Trends in intensive care for patients with COVID-19 in England, Wales, and Northern Ireland. Am J Respir Crit Care Med. 2021; 203:565–574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hamilton NJI, Jacob T, Schilder AGM, et al. ; COVIDTrach collaborative: COVIDTrach; the outcomes of mechanically ventilated COVID-19 patients undergoing tracheostomy in the UK: Interim Report. Br J Surg. 2020; 107:e583–e584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grigonis AM, Mathews KS, Benka-Coker WO, et al. : Long-term acute care hospitals extend ICU capacity for COVID-19 response and recovery. Chest. 2021; 159:1894–1901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guan WJ, Ni ZY, Hu Y, et al. ; China Medical Treatment Expert Group for Covid-19: Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382:1708–1720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang X, Yu Y, Xu J, et al. : Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med. 2020; 8:475–481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhou F, Yu T, Du R, et al. : Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020; 395:1054–1062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Docherty AB, Harrison EM, Green CA, et al. ; ISARIC4C investigators: Features of 20 133 UK patients in hospital with Covid-19 using the ISARIC WHO Clinical Characterisation Protocol: Prospective observational cohort study. BMJ. 2020; 369:m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu Z, McGoogan JM: Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020; 323:1239–1242 [DOI] [PubMed] [Google Scholar]
- 22.MacIntyre NR, Epstein SK, Carson S, et al. ; National Association for Medical Direction of Respiratory Care: Management of patients requiring prolonged mechanical ventilation: Report of a NAMDRC consensus conference. Chest. 2005; 128:3937–3954 [DOI] [PubMed] [Google Scholar]
- 23.Unroe M, Kahn JM, Carson SS, et al. : One-year trajectories of care and resource utilization for recipients of prolonged mechanical ventilation: A cohort study. Ann Intern Med. 2010; 153:167–175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.American Academy of Family Practice: Uniform Data System Mapper. 2020. Available at: https://www.udsmapper.org/. Accessed December 2, 2020
- 25.Jette A, Haley SM, Coster W, et al. : AM-PAC Boston University Activity Measure for Post-Acute Care. AM-PAC® Short Form Manual 3.0. Boston University School of Public Health, Health and Disability Research Institute. Copyright © 2021 AM-PAC – OnePress theme, FameThemes [Google Scholar]
- 26.Jubran A, Grant BJ, Duffner LA, et al. : Effect of pressure support vs unassisted breathing through a tracheostomy collar on weaning duration in patients requiring prolonged mechanical ventilation: A randomized trial. JAMA. 2013; 309:671–677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tansey CM, Louie M, Loeb M, et al. : One-year outcomes and health care utilization in survivors of severe acute respiratory syndrome. Arch Intern Med. 2007; 167:1312–1320 [DOI] [PubMed] [Google Scholar]
- 28.Sansone GR, Frengley JD, Vecchione JJ, et al. : Relationship of the duration of ventilator support to successful weaning and other clinical outcomes in 437 prolonged mechanical ventilation patients . J Intensive Care Med. 2017; 32:283–291 [DOI] [PubMed] [Google Scholar]
- 29.Jette DU, Stilphen M, Ranganathan VK, et al. : Validity of the AM-PAC “6-Clicks” inpatient daily activity and basic mobility short forms. Phys Ther. 2014; 94:379–391 [DOI] [PubMed] [Google Scholar]
- 30.Chicago Department of Public Health: Chicago Health Atlas. 2020. Available at: https://www.chicagohealthatlas.org/indicators. Accessed April 20, 2021
- 31.Zhou Y, Chi J, Lv W, et al. : Obesity and diabetes as high-risk factors for severe coronavirus disease 2019 (Covid-19). Diabetes Metab Res Rev. 2021; 37:e3377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Price-Haywood EG, Burton J, Fort D, et al. : Hospitalization and mortality among black patients and white patients with COVID-19. N Engl J Med. 2020; 382:2534–2543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rentsch CT, Kidwai-Khan F, Tate JP, et al. : Patterns of COVID-19 testing and mortality by race and ethnicity among United States veterans: A nationwide cohort study. PLoS Med. 2020; 17:e1003379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Damuth E, Mitchell JA, Bartock JL, et al. : Long-term survival of critically ill patients treated with prolonged mechanical ventilation: A systematic review and meta-analysis. Lancet Respir Med. 2015; 3:544–553 [DOI] [PubMed] [Google Scholar]
- 35.Leist SR, Dinnon KH, 3rd, Schäfer A, et al. : A mouse-adapted SARS-CoV-2 induces acute lung injury and mortality in standard laboratory mice. Cell. 2020; 183:1070–1085.e12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Camporota L, Sanderson B, Dixon A, et al. : Outcomes in mechanically ventilated patients with hypoxaemic respiratory failure caused by COVID-19. Br J Anaesth. 2020; 125:e480–e483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ferrando C, Suarez-Sipmann F, Mellado-Artigas R, et al. ; COVID-19 Spanish ICU Network: Clinical features, ventilator management, and outcome of ARDS caused by COVID-19 are similar to other causes of ARDS. Intensive Care Med. 2020; 46:2200–2211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zangrillo A, Beretta L, Scandroglio AM, et al. ; COVID-BioB Study Group: Characteristics, treatment, outcomes and cause of death of invasively ventilated patients with COVID-19 ARDS in Milan, Italy. Crit Care Resusc. 2020; 22:200–211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Botta M, Tsonas AM, Pillay J, et al. ; PRoVENT-COVID Collaborative Group: Ventilation management and clinical outcomes in invasively ventilated patients with COVID-19 (PRoVENT-COVID): A national, multicentre, observational cohort study. Lancet Respir Med. 2021; 9:139–148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chiang LL, Wang LY, Wu CP, et al. : Effects of physical training on functional status in patients with prolonged mechanical ventilation. Phys Ther. 2006; 86:1271–1281 [DOI] [PubMed] [Google Scholar]
- 41.Chen YH, Lin HL, Hsiao HF, et al. : Effects of exercise training on pulmonary mechanics and functional status in patients with prolonged mechanical ventilation. Respir Care. 2012; 57:727–734 [DOI] [PubMed] [Google Scholar]
- 42.Yang PH, Wang CS, Wang YC, et al. : Outcome of physical therapy intervention on ventilator weaning and functional status. Kaohsiung J Med Sci. 2010; 26:366–372 [DOI] [PubMed] [Google Scholar]
- 43.Clini EM, Crisafulli E, Antoni FD, et al. : Functional recovery following physical training in tracheotomized and chronically ventilated patients. Respir Care. 2011; 56:306–313 [DOI] [PubMed] [Google Scholar]
- 44.Martin UJ, Hincapie L, Nimchuk M, et al. : Impact of whole-body rehabilitation in patients receiving chronic mechanical ventilation. Crit Care Med. 2005; 33:2259–2265 [DOI] [PubMed] [Google Scholar]
- 45.Scheinhorn DJ, Hassenpflug MS, Votto JJ, et al. ; Ventilation Outcomes Study Group: Post-ICU mechanical ventilation at 23 long-term care hospitals: A multicenter outcomes study. Chest. 2007; 131:85–93 [DOI] [PubMed] [Google Scholar]
- 46.Polverino E, Nava S, Ferrer M, et al. : Patients’ characterization, hospital course and clinical outcomes in five Italian respiratory intensive care units. Intensive Care Med. 2010; 36:137–142 [DOI] [PubMed] [Google Scholar]
- 47.Sethuraman N, Jeremiah SS, Ryo A: Interpreting diagnostic tests for SARS-CoV-2. JAMA. 2020; 323:2249–2251 [DOI] [PubMed] [Google Scholar]
- 48.Winichakoon P, Chaiwarith R, Liwsrisakun C, et al. : Negative nasopharyngeal and oropharyngeal swabs do not rule out COVID-19. J Clin Microbiol. 2020; 58:e00297-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Patel R, Babady E, Theel ES, et al. : Report from the American Society for Microbiology COVID-19 International Summit, 23 March 2020: Value of diagnostic testing for SARS-CoV-2/COVID-19. mBio. 2020; 11:e00722–e00720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.City of Chicago COVID-19 data. 2021. . Available at: https://www.chicago.gov/city/en/sites/covid-19/home/latest-data.html. Accessed June 1, 2021.
- 51.Vitacca M, Vianello A, Colombo D, et al. : Comparison of two methods for weaning patients with chronic obstructive pulmonary disease requiring mechanical ventilation for more than 15 days. Am J Respir Crit Care Med. 2001; 164:225–230 [DOI] [PubMed] [Google Scholar]
- 52.Windisch W, Dellweg D, Geiseler J, et al. : Prolonged weaning from mechanical ventilation. Dtsch Arztebl Int. 2020; 117:197–204 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.