In 30 cases, the differentiation of an aneurysm versus a vascular variant could be achieved. In 20 cases (66%), the initial suspected diagnosis was revised. The findings suggest that 7T MR imaging provides a clarification tool for the group of patients with suspected unruptured intracranial aneurysms and diagnostic ambiguity after standard 3T MR imaging.
SUMMARY:
Most unruptured intracranial aneurysms can be adequately characterized using 1.5T and 3T MR imaging. Findings in a subgroup of patients can remain unclear due to difficulties in distinguishing aneurysms from vascular anatomic variants. We retrospectively analyzed clinical data from 30 patients with suspected incidental aneurysms on 3T MR imaging who underwent 7T MR imaging. In all 30 cases, the differentiation of an aneurysm versus a vascular variant could be achieved. In 20 cases (66%), the initial suspected diagnosis was revised. Our findings suggest that 7T MR imaging provides a clarification tool for the group of patients with suspected unruptured intracranial aneurysms and diagnostic ambiguity after standard 3T MR imaging.
The prevalence of unruptured intracranial aneurysms (UIAs) in the general population is estimated to be about 3%–5%.1 Most UIAs can be sufficiently characterized and followed up using conventional 1.5T and 3T MR imaging. However, findings in a relevant subgroup of patients can remain ambiguous when using 1.5T and 3T MR imaging due to difficulties in distinguishing aneurysms from vascular anatomic variants such as vessel infundibula or loops. Especially, small findings (<5 mm) may remain ambiguous: Up to 18% of findings on 3T 3D-TOF may be unclear, and in the remaining 82%, they may be regarded as clear. False-positive and -negative rates of up to 6% and 2% can be observed.2-4 Diagnostic uncertainty may lead to potentially unnecessary follow-up examinations or even invasive diagnostic procedures (DSA). The consequence is patient anxiety, risk of co-morbidities, and considerable additional costs.
MR imaging at 7T may provide a definitive noninvasive diagnosis in this subgroup of patients because the higher magnetic field strength enables image acquisition with a higher signal-to-noise ratio, higher spatial resolution, and higher vessel contrast. MR imaging at 7T has recently received the CE mark and FDA clearance and can be implemented beyond research settings. Previous studies have suggested the superiority of 7T MR imaging over 1.5T or 3T MR imaging in the depiction and characterization of aneurysms.5 A strong correlation between 7T and DSA has also been shown previously, with some studies reporting sensitivity rates comparable with those of DSA.6 However, most of the existing evidence is derived from an experimental setting. We report our single-institution experience of integration of 7T MR imaging in a clinical routine work-up for the management of patients with ambiguous neurovascular findings on 3T MR imaging suspicious for small UIAs. We hypothesize that 7T MR imaging provides definitive, noninvasive discrimination of intracranial aneurysms versus normal vascular variants.
MATERIALS AND METHODS
Patients
We identified 30 patients with suspected incidental UIAs after routine 3T MR imaging who underwent additional 7T MR imaging. The interdisciplinary neurovascular board at Bern University Hospital screened and selected the patients during the clinical-management process. Approximately 800 patients with confirmed or suspected intracranial aneurysms are presented for evaluation annually to this board, representing all cases referred to our institution as a tertiary referral center. Patients with small, incidental ambiguous findings, ie, suspected UIAs, on recent routine 3T MR imaging were additionally examined with 7T MR imaging on the basis of the recommendation of the board. The findings were reviewed by the board, and a management recommendation was made. All patients were examined between October 2019 and March 2021. All patients signed the informed consent form, and the analysis was approved by the local ethics committee.
Imaging Protocol
All patients were scanned on a clinically approved 7T whole-body MR imaging scanner (Magnetom Terra, clinical mode; Siemens) equipped with a 1-channel transmit and 32-channel receive head coil (Nova Medical, Wilmington, MA, USA) and on a 3T Magnetom Prisma scanner (Siemens) equipped with a 32-channel head coil (Nova Medical, Wilmington, MA, USA).
The 7T imaging comprised the following sequences: sagittal T1 MPRAGE, 0.6 × 0.6 × 0.6 mm3; axial T2 spin-echo, 0.3 × 0.3 × 1.5 mm3; axial SWI, 0.2 × 0.2 × 1.2 mm3; axial arterial TOF angiography, 0.14 × 0.14 × 0.25 mm3 (interpolated, acquired: 0.36 × 0.28 × 0.50 mm3), and sagittal T1 sampling perfection with application optimized contrast by using different flip angle evolution (SPACE; Siemens), 0.5 × 0.5 × 0.5 mm3 (Online Supplemental Data). No intravenous contrast agent was administered. The 3T imaging was a standardized contrast-enhanced protocol (including arterial TOF angiography and contrast-enhanced angiography) (Online Supplemental Data).
Analysis
In clinical routine, all images were reviewed by 2 readers and subsequently presented to the referring board. We analyzed the following: 1) board decisions and recommendations before 7T MR imaging, 2) reports from 3T MR imaging and subsequent 7T MR imaging, and 3) board decisions and recommendations after 7T MR imaging to capture changes in diagnosis and management. We used a simple binomial test considering ambiguous-versus-nonambiguous diagnoses. P values < .05 were considered statistically significant.
RESULTS
Thirty patients with suspected incidental UIAs after routine 3T MR imaging were included (19 women and 11 men; median age, 56 years; mean age, 51 years; range, 16–71 [SD, 15.5] years) (Online Supplemental Data). All MR imaging examinations were performed without interruption or adverse effects. All images fulfilled the criteria of diagnostic quality within routine image reading. In all 30 cases, no ambiguous findings remained after 7T MR imaging, and a definitive diagnosis was made according to the analyzed reports (P < .001).
In 20 cases (66%), the initial suspected diagnosis was revised. In 18 of the 20 cases (60%), the initial diagnosis of suspected UIA was revised in favor of a normal vessel (infundibulum, Fig 1, or perforating artery, Fig 2, and Online Supplemental Data). As a result, because UIA was ruled out, no further follow-up was recommended by the interdisciplinary neurovascular board. In the 2 remaining cases (6.7%) (prominent tip of the basilar artery and vessel loop, but UIA could not be ruled out), the initial suspected diagnosis was revised in favor of a true aneurysm. In 1 of these 2 cases, a standard follow-up was recommended; in the remaining case, DSA was recommended due to a high-risk profile.
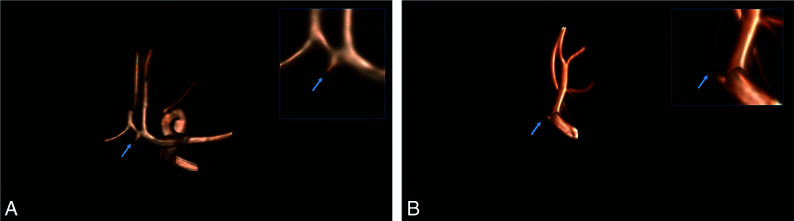
FIG 1.
A, A UIA was reported on the basis of 3T MR imaging (MIP reconstruction of the 3D-TOF angiography, zoom in the right upper corner). B, MIP reconstruction of the TOF acquired at 7T MR imaging depicts an infundibulum emerging from the anterior communicating artery (zoom in the right upper corner). The blue arrow is indicating the finding of interest.
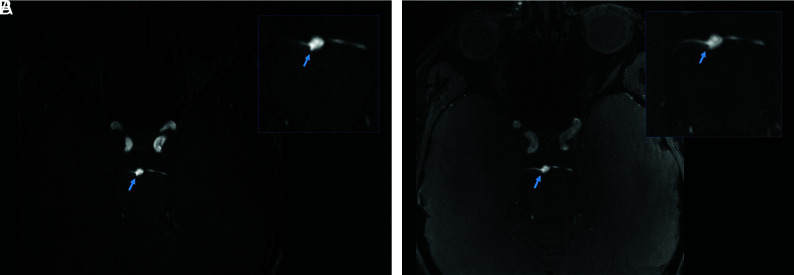
FIG 2.
A, A UIA was suspected on the basis of 3T MR imaging (axial 3D-TOF angiography, zoom in the right upper corner). B, MR imaging at 7T depicts a perforator artery parallel to the right superior cerebellar artery (axial 3D-TOF angiography, zoom in the right upper corner). The blue arrow is indicating the finding of interest.
In 10 cases (33%), the initial diagnosis was confirmed. Therefore, in 8 cases (26.7%), a definitive diagnosis of an UIA was confirmed, and as a consequence, the interdisciplinary board recommended annual MR imaging follow-up according to the institutional guidelines for small UIAs. In 2 cases (6.7%), 7T MR imaging confirmed the presence of an infundibulum and ruled out the presence of a UIA; therefore, no further follow-up was recommended.
DISCUSSION
Our findings suggest that 7T MR imaging provides a clarification tool for the group of patients with suspected UIAs and diagnostic ambiguity after standard 3T MR imaging. DSA as the criterion standard is not available for this cohort, a potential limitation; however, performing an invasive procedure would not necessarily be justifiable. The higher diagnostic confidence7 may enable avoiding unnecessary follow-up examinations or invasive DSA. Similarly, revision of an UIA diagnosis toward a normal vascular variant reduces the number of unnecessary follow-up imaging procedures, which would be otherwise performed according to our institutional and national standards.
Most important, socioeconomic factors of suspected, incidental aneurysms and ambiguous vascular findings on 1.5T and 3T MR imaging should be taken into consideration. In this context, resolving diagnostic ambiguities can be especially impactful for young patients with long life expectancies. In our cohort, 26% of patients were younger than 40 years of age. Several studies evaluated the psychological aspects of the UIA diagnosis, suggesting a relevant decrease in quality of life, depression, and anxiety.8,9 The impact of ambiguous findings is less explored10,11 and depends largely on the case-specific communication; however, a similar effect could be expected. Increased diagnostic accuracy, diagnostic confidence, and, as a consequence, reduction of ambiguity due to 7T imaging could potentially improve the quality of life and reduce a patient’s anxiety.
Financial savings due to avoided unnecessary noninvasive or even invasive diagnostic procedures and outpatient consultations in ambiguous findings are expected; however, this expectation is specific to each national reimbursement system. Thus, a dedicated analysis is not within the scope of this study.
We hypothesized that 7T MR imaging allowed us to resolve the ambiguity, first, due to improvement of the signal-to-noise ratio, resulting in better contrast between the vessel and the surrounding tissue and, second, due to the improved spatial resolution resulting in precise assessment of the shape of the vessels. Finally, the maximum-intensity-projection reconstruction of TOF acquired at 7T allows superior visual 3D analysis. As expected, we observed pulsation artifacts and field inhomogeneity in all patients under investigation. However, these artifacts did not influence the diagnostic confidence within the routine use of 7T MR imaging using dedicated vascular imaging sequences.
CONCLUSIONS
Clinical implementation of 7T MR imaging in patients with suspected small incidental UIAs has the potential to reduce the number of ambiguous vascular findings and to secure a definitive diagnosis and has, therefore, an impact on patient management as well as quality of life and cost of health services.
ABBREVIATION:
- UIA
unruptured intracranial aneurysm
Footnotes
Disclosure forms provided by the authors are available with the full text and PDF of this article at www.ajnr.org.
References
- 1.Seibert B, Tummala RP, Chow R, et al. Intracranial aneurysms: review of current treatment options and outcomes. Front Neurol 2011;2:45 10.3389/fneur.2011.00045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li MH, Li YD, Gu BX, et al. Accurate diagnosis of small cerebral aneurysms ≤5 mm in diameter with 3.0-T MR angiography. Radiology 2014;271:553–60 10.1148/radiol.14122770 [DOI] [PubMed] [Google Scholar]
- 3.White PM, Teasdale EM, Wardlaw JM, et al. Intracranial aneurysms: CT angiography and MR angiography for detection prospective blinded comparison in a large patient cohort. Radiology 2001;219:739–49 10.1148/radiology.219.3.r01ma16739 [DOI] [PubMed] [Google Scholar]
- 4.Okahara M, Kiyosue H, Yamashita M, et al. Diagnostic accuracy of magnetic resonance angiography for cerebral aneurysms in correlation with 3D-digital subtraction angiographic images: a study of 133 aneurysms. Stroke 2002;33:1803–08 10.1161/01.STR.0000019510.32145.A9 [DOI] [PubMed] [Google Scholar]
- 5.Wrede KH, Dammann P, Monninghoff C, et al. Non-enhanced MR imaging of cerebral aneurysms: 7 Tesla versus 1.5 Tesla. PLoS One 2014;9:e84562 10.1371/journal.pone.0084562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wrede KH, Matsushige T, Goericke SL, et al. Non-enhanced magnetic resonance imaging of unruptured intracranial aneurysms at 7 Tesla: comparison with digital subtraction angiography. Eur Radiol 2017;27:354–64 10.1007/s00330-016-4323-5 [DOI] [PubMed] [Google Scholar]
- 7.Springer E, Dymerska B, Cardoso PL, et al. Comparison of routine brain imaging at 3 T and 7T. Invest Radiol 2016;51:469–82 10.1097/RLI.0000000000000256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Su SH, Xu W, Hai J, et al. Cognitive function, depression, anxiety and quality of life in Chinese patients with untreated unruptured intracranial aneurysms. J Clin Neurosci 2014;21:1734–39 10.1016/j.jocn.2013.12.032 [DOI] [PubMed] [Google Scholar]
- 9.Towgood K, Ogden JA, Mee E. Psychosocial effects of harboring an untreated unruptured intracranial aneurysm. Neurosurgery 2005;57:858–60; discussion 858–60 10.1227/01.neu.0000179917.47904.d8 [DOI] [PubMed] [Google Scholar]
- 10.Kumbhar SS, Baheti AD, Itani M, et al. Ambiguous findings on radiographs. Curr Probl Diagn Radiol 2021;50:4–10 10.1067/j.cpradiol.2019.10.003 [DOI] [PubMed] [Google Scholar]
- 11.Domen RE. The ethics of ambiguity: rethinking the role and importance of uncertainty in medical education and practice. Acad Pathol 2016;3:2374289516654712 10.1177/2374289516654712 [DOI] [PMC free article] [PubMed] [Google Scholar]