Abstract
Objective:
The increasing focus on adolescent personality disorder has tended to ignore evidence of the developmental continuity of the period from puberty to young adulthood. This study aims to: (1) describe the characteristics of a sample of young people with borderline personality disorder (BPD) who had no previous history of evidence-based treatment for the disorder and (2) compare their characteristics by participant age group.
Methods:
One hundred and thirty-nine young people (15 to 25 years) with BPD, newly enrolled in the Monitoring Outcomes of BPD in Youth randomized controlled trial, completed semi-structured interview and self-report measures assessing demographic, clinical, and functional characteristics. Younger (aged 15 to 17 years; n = 64) and older (aged 18 to 25 years; n = 75) participants were compared on these same variables using t-tests, chi-square tests, and logistic regression.
Results:
Young outpatients with BPD had extensive and severe psychopathology and were functioning poorly. Adolescents and young adults with BPD showed substantial similarities on 20 key aspects of their presentation. Significant between-groups differences were observed in household makeup, treatment history, antisocial personality disorder, emotion dysregulation, substance use, age of commencement and extent of self-harm, and achievement of age-appropriate educational milestones. Adolescent BPD group membership was predicted by family composition and self-harm, whereas young adult BPD group membership was predicted by not achieving age-appropriate milestones, vocational disengagement, and emotion dysregulation. The final model explained 54% of the variance and correctly classified 80.2% of the sample by age.
Conclusions:
Both adolescents and young adults with early stage BPD present with severe and often similar problems to one another, supporting developmental continuity across this age range. However, there are also meaningful differences in presentation, suggesting that pathways to care might differ by age and/or developmental stage. Detection and intervention for personality disorder should not be delayed until individuals reach 18 years of age.
Keywords: early intervention, borderline personality disorder, randomized controlled trial, treatment, youth, adolescents, young adults, psychiatry
Abstract
Objectif:
L’attention croissante portée au trouble de la personnalité limite chez les adolescents a tendance à ignorer les données probantes de la continuité développementale pour la période de la puberté au jeune âge adulte. La présente étude vise à: (1) décrire les caractéristiques d’un échantillon de jeunes gens souffrant du trouble de la personnalité limite (TPL) qui n’avaient pas d’antécédents de traitement fondé sur des données probantes pour le trouble; et (2) comparer les caractéristiques des participants par groupe d’âge.
Méthode:
Cent trente-neuf jeunes gens (de 15 à 25 ans) souffrant du TPL, nouvellement inscrits dans l’essai randomisé contrôlé MOBY, ont répondu à une entrevue semi-structurée et à des mesures auto-administrées évaluant les caractéristiques démographiques, cliniques et fonctionnelles. Les participants plus jeunes (de 15 à 17 ans; n = 64) et plus âgés (de 18 à 25 ans; n = 75) ont été comparés selon ces mêmes variables à l’aide de t-tests, de tests chi-carré, et de la régression logistique.
Résultats:
Les jeunes patients ambulatoires souffrant du TPL avaient une psychopathologie développée et grave, et avaient un mauvais fonctionnement. Les adolescents et les jeunes adultes souffrant du TPL révélaient des similarités substantielles à 20 aspects clés de leur présentation. Des différences significatives ont été observées entre les groupes en ce qui concerne la composition du ménage, les antécédents de traitement, le trouble de la personnalité antisociale, la dérégulation des émotions, l’utilisation de substances, l’âge du commencement, et l’étendue de l’automutilation, et la réussite des étapes éducatives appropriées à leur âge. L’appartenance au groupe des adolescents souffrant du TPL était prédite par la composition familiale et l’automutilation, alors que l’appartenance au groupe des jeunes adultes souffrant du TPL était prédite par le fait de ne pas réussir les étapes appropriées à leur âge, le désengagement professionnel, et la dérégulation des émotions. Le modèle final expliquait 54% de la variance et classait correctement 80,2% de l’échantillon selon l’âge.
Conclusions:
Les adolescents et les jeunes adultes en première phase du TPL présentent de graves problèmes souvent semblables les uns aux autres, soutenant la continuité développementale dans cette tranche d’âge. Toutefois, il y a également des différences significatives dans la présentation, ce qui suggère que les trajectoires de soins pourraient différer selon l’âge et/ou le stade développemental. La détection du trouble de la personnalité et l’intervention ne devraient pas retarder avant que les personnes aient 18 ans.
Introduction
Borderline personality disorder (BPD) is a severe mental disorder commonly emerging during adolescence (10 to 18 years) or early adulthood (19 to 25 years). 1,2 International consensus is that the diagnosis of BPD is reliable and valid in adolescence, and that BPD is both common and treatable. 3 However, the field has been slow to integrate contemporary, evidence-based developmental models of the transition from childhood to adulthood. 4
Reluctance to diagnose BPD in young people under the age of 18 years is often due to the belief that BPD features are reflective of normative developmental processes (“storm and stress”), rather than personality pathology. 5 Such beliefs appear to assume that the developmental processes underpinning personality development, identity formation, and executive functioning are in flux before 18 years of age and stabilize thereafter. However, these processes have been shown to extend into the third decade of life, with some aspects extending even further. 6 –9 Research has identified a distinct and developmentally continuous period in economically developed societies, extending from puberty (operationally defined as age 10 to 12 years) to around 25 years of age (collectively referred to as “young people”), which is believed to support enculturation. 6,7 This developmental period also represents a period of particular vulnerability and coincides with the peak period of clinical onset for major mental disorders, including BPD. 2,10
Recognition of this vulnerable period of development has led to the emergence of youth mental health as a construct to guide developmentally appropriate prevention and early intervention and care for those with enduring mental ill-health. 11,12 However, the personality disorder (PD) and youth mental health fields have been slow to engage with one another. 13 For example, in a recent systematic review and meta-analysis of psychotherapies for adolescents with BPD, 14 one study 15 that recruited participants aged 15 to 25 years (mean age 18.4 [standard deviation = 2.9]) was excluded because the review authors stated that it “…included a large number of adults…We felt that adolescents were not the primary patient population…” (p.1) 16
While this age group might be developmentally coherent, there might still be meaningful age-related differences. Nine publications from 5 studies have used structured diagnostic assessments to investigate the clinical presentation and functioning of adolescents and young adults with BPD. 17 –24 Only one of these compared adolescents (13- to 17-year-olds) with adults (18- to 35-year-old). 25 However, these 2 samples were not collected contemporaneously and the stage of illness was not reported, thereby confounding the findings with “duration of illness.” 26 No study has used contemporaneously collected data from individuals at a similar stage of illness (e.g., first presentation for evidence-based BPD care) to comprehensively investigate similarities or differences among the demographic, clinical, and functional characteristics of older versus younger people within this developmental period. The aims of the current study are to: (i) describe the clinical characteristics of young people with first presentation for evidence-based care for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR)/Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition BPD 27,28 and (ii) compare adolescent (15 to 17 years) with young adult (18 to 25 years) participants.
Methods
Design
Participants were enrolled in Monitoring Outcomes of BPD in Youth (MOBY), a parallel groups, single-blind randomized controlled trial (RCT) that was prospectively registered with the Australian New Zealand Clinical Trials Registry (ACTRN12610000100099). 29 The current study reports cross-sectional data from the baseline assessments.
Setting
Participants were recruited from Orygen, which manages both the State Government-funded specialist mental health service for 15- to 25-year-olds residing in western and northwestern metropolitan Melbourne, Victoria, Australia, and also a Federally funded headspace center within the same geographical area, which is part of the national network of primary care youth mental health centers for 12- to 25-year-olds.
Participants
The sample comprised 139 young people aged 15 to 25 years (inclusive), with a DSM-IV-TR diagnosis of BPD (≥5 criteria). Potential participants were excluded if they had: (i) a DSM-IV-TR psychotic disorder in the past 12 months; (ii) a lifetime diagnosis of a schizophrenia spectrum disorder or bipolar I or II disorder; (iii) a mental disorder due to a medical condition; or (iv) prior evidence-based psychosocial treatment for BPD. 30
Procedure
Potential participants were recruited between March 2011 and September 2015. All participants (and a parent or guardian for those under 18 years) gave written informed consent. Assessments were conducted by psychology graduates who were trained and supervised by the trial coordinator (JB), a psychologist, and the chief investigator (AC), a psychiatrist. Participants were reimbursed for their time and expenses. Ethical approval was granted by the Melbourne Health Human Research and Ethics Committee (HREC 2010.055).
Measures
Demographic, vocational, and treatment information were collected, consistent with Australian Bureau of Statistics variables. 31 –33 Participants were deemed to have achieved age-appropriate secondary school milestones if they had passed a year level at the age at which most school students in Victoria would pass that level (with a tolerance of 1 additional year).
Mental state disorders and PDs were diagnosed using the Structured Clinical Interview for DSM-IV (SCID) Axis I Disorders—Patient Version 34 and the SCID Axis II Disorders (SCID-II). 35 For antisocial PD (ASPD), Criterion B, requiring individuals to be 18 years or over, was not applied. This is in keeping with the evidence regarding continuity of this disorder across the same developmental period. 36 Specific phobia was not assessed.
Severity of BPD: The Borderline PD Severity Index (BPDSI) 37,38 is a 70-item semistructured interview that assesses for each of the 9 DSM-IV BPD criteria over the previous 3 months. Inter-rater reliability was found to be high in the current study, (intraclass correlation coefficient (ICC) (2,1) = 0.993, P < .001).
Emotion dysregulation: The Difficulties in Emotion Regulation Scale (DERS) 39 is a 36-item, self-report scale. Higher total score indicates greater difficulties. 40
Depressive symptomatology: The Centre for Epidemiologic Studies Depression Scale—Revised comprises 20 self-report items. 41 Higher total score indicates greater depression severity. The Montgomery-Äsberg Depression Rating Scale (MADRS) 42 is a 10-item, observer-rated measure, administered using the Structured Interview Guide for the MADRS. 43 Higher total score indicates greater depression severity. Inter-rater reliability was found to be high in the current study; (ICC(2,1) = 0.969, P < 0.001).
Self-harm and suicidality: The Beck Scale for Suicide Ideation (BSS) 44 comprises between 6 and 21 self-report items. A higher score (sum of first 19 items) indicates greater severity. The Suicide Attempt and Self-Injury Interview (SASII) 45 is a structured interview with self-report questionnaires.
Substance use was assessed using the Opiate Treatment Index Section II (OTI) 46 and the Alcohol Use Disorders Identification Test (AUDIT). 47 The OTI is a semistructured interview that can be used to generate a Q-score, reflecting mean quantity used daily, by dividing the total quantity used in the previous 2 episodes of use by the total number of days between the last 3 episodes. 46 The AUDIT comprises 10 self-report items, with a score greater than 19 indicating alcohol dependence. 48
Functioning was captured using the Social Adjustment Scale Self-Report (SAS-SR), 49 the Inventory of Interpersonal Problems Circumplex Version (IIP-C), 50,51 and the Social and Occupational Functioning Assessment Scale (SOFAS). 52 The 54-item SAS-SR measures functioning over the previous 2 weeks, covering work/study, leisure activities, and relationships. Higher scores reflect poorer functioning. The IIP-C is a 64-item self-report questionnaire used to assess interpersonal functioning, which enables a total raw score to be calculated by summing all items. 51 The SOFAS was used to capture general social and occupational functioning.
Quality of life was measured using the 35-item self-report Assessment of Quality of Life—8 Dimensions. 53 This measure derives a utility score ranging from 0.00 (representing death) to 1.00 (representing the best health state within this measure).
Data Analysis
Statistical analyses were performed using the IBM SPSS Statistics, Version 22. Summary statistics were generated to characterize the sample, and independent samples t-tests, chi-square tests, and Fisher exact tests were conducted to compare the 2 age groups, with α set at 0.05 for all analyses. Multivariate forward stepwise logistic regression was used to determine which variables best discriminated between the age groups.
Results
Participant Flow
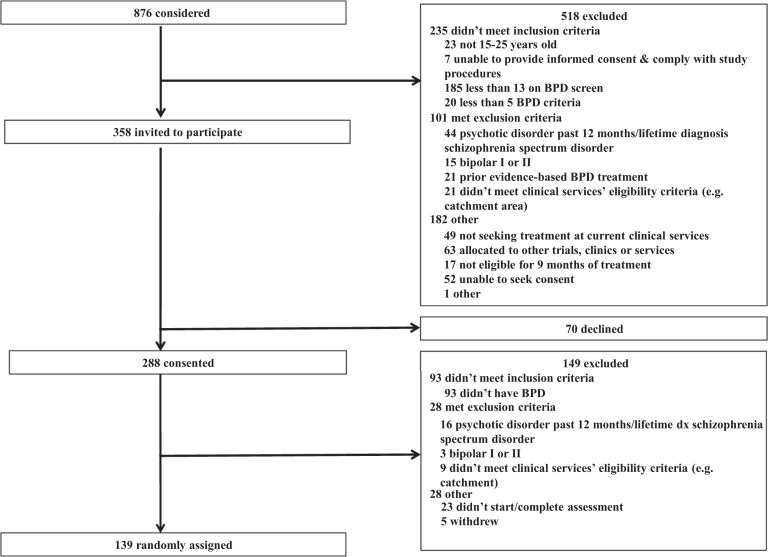
In total, 876 young people were considered for inclusion in the trial (Figure 1), with 288/358 (80%) consenting to participate. Of those, 139 were confirmed to be eligible and were randomized.
Figure 1.
CONSORT flow diagram detailing recruitment. BPD = borderline personality disorder; CONSORT = Consolidated Standards of Reporting Trials.
Characteristics of Young People with BPD
The sample primarily comprised single (59%), Australian-born (88.5%) females (80.6%) of medium-to-high socioeconomic disadvantage (82%) residing with siblings (51.8%) and/or biological parents (60.4%) who had received mental-health treatment in the previous 12 months (66.2% and 63.3% used mental health sessions and medications, respectively, Table 1). Participants had a mean of 2.6 concurrent mental state disorder diagnoses and 2.4 PDs (Table 2). In addition to a diagnosis of BPD, 95% (132/139) of participants met criteria for a DSM-IV-TR mental state disorder, and 68.4% (95/139) had another concurrent PD. Overall, 99.3% of participants reported self-harming behavior (Table 3). The most commonly used substances in the previous month were tobacco, alcohol, cannabis, and amphetamines. AUDIT scores indicated that 18.7% (26/139) of participants were dependent on alcohol. Forty percent of the sample were not engaged in education, employment, training, or homemaking (NEET, Table 4).
Table 1.
Demographic Characteristics and Treatment History.
| Characteristics | Descriptive statistic | Total sample N = 139 |
15 to 17 years N = 64 |
18 to 25 years N = 75 |
Test statistic |
|---|---|---|---|---|---|
| Age | M (SD) | 19.1 (2.8) | 16.6 (0.9) | 21.2 (1.9) | |
| Sex (%female) | % (n) | 80.6 (112) | 85.9 (55) | 76.0 (57) | χ2(1) = 2.18, P = 0.140 |
| Socioeconomic disadvantage | χ2(2) = 1.67, P = 0.434 | ||||
| Low | % (n) | 18.0 (25) | 14.0 (9) | 21.3 (16) | |
| Medium | % (n) | 49.6 (69) | 54.7 (35) | 45.3 (34) | |
| High | % (n) | 32.4 (45) | 31.3 (20) | 33.3 (25) | |
| Born in Australia | %(n) | 88.5 (123) | 90.6 (58) | 86.7 (65) | χ2(1) = 0.53, P = 0.466 |
| Indigenous | % (n) | 3.7 (5) | 3.2 (2) | 4.0 (3) | |
| Parent(s) born outside Australia | % (n) | 57.6 (80) | 39.0 (25) | 45.3 (34) | χ2(1) = 0.56, P = 0.456 |
| English as main language spoken at home | % (n) | 97.1 (135) | 95.3 (61) | 98.7 (74) | FET, P = 0.334 |
| Relationship status—single | % (n) | 59.0 (82) | 62.5 (40) | 56.0 (42) | χ2(1) = 0.60, P = 0.437 |
| Children | % (n) | 7.2 (10) | 0 (0) | 13.3 (10) | FET, P = 0.002 |
| Living with a: | |||||
| Siblings | % (n) | 51.8 (72) | 70.3 (45) | 36.0 (27) | χ2(1) = 16.28, P < 0.001 |
| Biological father and/or mother | % (n) | 60.4 (84) | 81.25 (52) | 42.7 (32) | χ2(1) = 21.50, P < 0.001 |
| Other nonrelatives, e.g., friends, flatmates | % (n) | 27.3 (38) | 20.3 (13) | 33.3 (25) | χ2(1) = 2.95, P = 0.086 |
| Other relatives, e.g., grandparent, aunty | % (n) | 15.8 (22) | 14.1 (9) | 17.3 (13) | χ2(1) = 0.28, P = 0.598 |
| Partner | % (n) | 10.8 (15) | 3.1 (2) | 17.3 (13) | χ2(1) = 7.24, P = 0.007 |
| Stepfather and/or stepmother | % (n) | 4.3 (6) | 3.1 (2) | 2.7 (2) | |
| Foster parents or a residential placement | % (n) | 2.9 (4) | 4.7 (3) | 1.4 (1) | |
| Alone | % (n) | 2.9 (4) | 1.6 (1) | 4.0 (3) | |
| Children | % (n) | 2.9 (4) | 0 (0) | 5.3 (4) | |
| Homeless | % (n) | 0.7 (1) | 0 (0) | 1.4 (1) | |
| Treatment history | |||||
| Medication use (current) | % (n) | 46.0 (64) | 39.1 (25) | 52.0 (39) | χ2(1) = 2.33, P=.127 |
| Medication use (past 12 months) | % (n) | 63.3 (88) | 50.0 (32) | 74.7 (56) | χ2(1) = 9.05, P = .003 |
| Mental health session use (past 12 months) | % (n) | 66.2 (92) | 75.0 (48) | 58.7 (44) | χ2(1) = 4.12, P = .042 |
| Number of sessions (past 12 months) | M (SD) | 13.6 (22.4) | 18.1 (25.8) | 9.8 (18.4) | t(111.6) = 2.14, P = .034b |
Note. M = mean; SD = standard deviation; FET = Fisher exact test.
a Categories are not mutually exclusive.
b Test statistic and degrees of freedom modified because equal variances not assumed.
Table 2.
Diagnostic Characteristics.
| Diagnoses | Descriptive statistic | Total sample N = 139 |
15 to 17 years N = 64 |
18 to 25 years N = 75 |
Test statistic |
|---|---|---|---|---|---|
| Mental state diagnoses | |||||
| Number of current diagnoses | M (SD) | 2.6 (1.5) | 2.5 (1.6) | 2.6 (1.4) | t(137) = −0.22, P = 0.830 |
| Any mood | % (n) | 82.0 (114) | 82.8 (53) | 81.3 (61) | χ2(1) = 0.05, P = 0.821 |
| Any anxiety disorder | % (n) | 71.9 (100) | 70.3 (45) | 73.3 (55) | χ2(1) = 0.16, P = 0.693 |
| Any eating disorder | % (n) | 7.2 (10) | 7.8 (5) | 6.7 (5) | FET, P = 1.000 |
| Any somatoform disorder | % (n) | 6.5 (9) | 3.1 (2) | 9.3 (7) | FET, P = 0.178 |
| Posttraumatic stress disorder | % (n) | 31.7 (44) | 31.3 (20) | 32.0 (24) | χ2(1) = 0.01, P = 0.925 |
| Personality disorders | |||||
| Number of current diagnoses | M (SD) | 2.4 (1.4) | 2.2 (1.4) | 2.5 (1.4) | t(137) = −1.10, P = 0.274 |
| Borderline | % (n) | 100 (139) | 100 (64) | 100 (75) | |
| Antisocial | % (n) | 33.1 (46) | 20.3 (13) | 44.0 (33) | χ2(1) = 8.75, P = 0.003 |
| Avoidant | % (n) | 24.5 (34) | 23.4 (15) | 25.3 (19) | χ2(1) = 0.07, P = 0.795 |
| Paranoid | % (n) | 24.5 (34) | 20.3 (13) | 28.0 (21) | χ2(1) = 1.10, P = 0.293 |
| Depressive | % (n) | 19.4 (27) | 18.8 (12) | 20.0 (15) | χ2(1) = 0.03, P = 0.853 |
| Passive aggressive | % (n) | 14.4 (20) | 17.2 (11) | 12.0 (9) | χ2(1) = 0.75, P = 0.385 |
| Obsessive compulsive | % (n) | 5.8 (8) | 6.3 (4) | 5.3 (4) | FET, P = 1.000 |
| Narcissistic | % (n) | 4.3 (6) | 4.7 (3) | 4.0 (3) | FET, P = 1.000 |
| Histrionic | % (n) | 4.3 (6) | 3.1 (2) | 5.3 (4) | FET, P = 0.687 |
| Dependent | % (n) | 3.6 (5) | 3.1 (2) | 4.0 (3) | FET, P = 1.000 |
| Schizotypal | % (n) | 2.2 (3) | 4.7 (3) | 0 (0) | FET, P = 0.095 |
| Schizoid | % (n) | 0.0 (0) | 0 (0) | 0 (0) | |
| Previously diagnosed BPD | % (n) | 18.7 (25)a | 14.5 (9)b | 22.2 (16)c | χ2(1) = 1.30, P = 0.254 |
Note. BPD = borderline personality disorder; FET = Fisher exact test; M = mean; SD = standard deviation.
a n = 134.
b n = 62.
c n = 72.
Table 3.
Clinical Features.
| Characteristics | Descriptive statistic | Total sample N = 139 |
15 to 17 years N = 64 |
18 to 25 years N = 75 |
Test statistic | |
|---|---|---|---|---|---|---|
| Symptomatology | ||||||
| BPDSI | M (SD) | 40.2 (12.8)a | 39.3 (12.2)b | 40.9 (13.4)c | t(134) = −0.72, P = 0.473 | |
| DERS– | M (SD) | 132.2 (20.1)d | 128.0 (19.0)b | 135.7 (20.5)e | t(135) = −2.28, P = 0.024 | |
| CESD-R | M (SD) | 43.2 (12.8) | 41.8 (13.2) | 44.5 (12.5) | t(137) = −1.21, P = 0.230 | |
| MADRS | M (SD) | 28.3 (9.3) | 27.8 (10.1) | 28.7 (8.7) | t(137) = −0.58, P = 0.562 | |
| Substance use | ||||||
| AUDIT | M (SD) | 10.5 (9.0) | 7.1 (6.3) | 13.5 (9.9) | t(137) = −4.44, P < 0.001 | |
| OTI—Tobacco use in past month | % (n) | 74.6 (100)f | 67.7 (42)g | 80.6 (58)h | χ2(1) = 2.89, P = 0.089 | |
| OTI—Alcohol use in past month | % (n) | 69.4 (93)f | 58.1 (36)g | 79.2 (57)h | χ2(1) = 6.99, P = 0.008 | |
| OTI—Cannabis use in past month | % (n) | 42.5 (57)f | 37.1 (23)g | 47.2 (34)h | χ2(1) = 1.40, P = 0.237 | |
| OTI—Amphetamines use in past month | % (n) | 16.4 (22)f | 6.5 (4)g | 25.0 (18)h | χ2(1) = 8.35, P = 0.004 | |
| OTI—Polysubstance use in past month | % (n) | 68.7 (92)f | 56.5 (35)g | 79.2 (57)h | χ2(1) = 7.99, P = 0.005 | |
| OTI—Number of substance classes (past month) | M (SD) | 2.4 (1.6)f | 1.9 (1.6)g | 2.7 (1.6)h | t(132) = −2.89, P = 0.005 | |
| OTI Q score—Tobacco use, cigarettes | M (SD) | 7.0 (8.4)i | 6.2 (8.9)g | 7.7 (7.9)j | t(132) = −1.05, P = 0.295 | |
| OTI Q score—Alcohol, standard drinks | M (SD) | 1.7 (3.4)f | 0.9 (2.1)g | 2.3 (4.2)h | t(109.1) = −2.38, P = 0.019 | |
| OTI Q score—Cannabis, joints/bongs | M (SD) | 0.4 (1.6)i | 0.4 (2.0)g | 0.5 (1.1)j | t(131) = −0.18, P = 0.861 | |
| OTI Q score—Amphetamines, tablets/hits | M (SD) | 0.06 (0.2)i | 0.02 (0.1)l | 0.1 (0.2)h | t(102.3) = −1.99, P = 0.049 | |
| Self-harm | ||||||
| SASII—Any lifetime self-harm | % (n) | 99.3 (134)m | 100.0 (63)b | 98.6 (71)h | χ2(1) = 0.88, P = 0.348 | |
| SASII—Age of onset (years) | M (SD) | 13.2 (2.8)f | 12.3 (2.2)b | 14.0 (3.1)j | t(132) = −3.50, P = 0.001 | |
| SASII—NSSI (past 12 months) | % (n) | 77.0 (104)m | 88.9 (56)b | 66.7 (48)h | χ2(1) = 9.38, P = 0.002 | |
| SASII—NSSI number of acts (past 12 months) | M (SD) | 42.4 (95.3)m | 61.3 (125.5)b | 25.8 (52.7)h | t(80.9) = 2.09, P = 0.039 | |
| SASII—Suicide attempts (past 12 months) | % (n) | 62.2 (84)m | 63.5 (40)b | 61.1 (44)h | χ2(1) = 0.08, P = 0.776 | |
| SASII—Number of suicide attempts (past 12 months) | M (SD) | 1.9 (2.6)m | 1.9 (2.4)b | 1.8 (2.7)h | t(133) = 0.19, P = 0.847 | |
| BSS | M (SD) | 11.3 (8.5)n | 13.0 (9.0)o | 10.0 (7.8)p | t(116) = 2.0, P = 0.051 | |
Note. AUDIT = Alcohol Use Disorders Identification Test; BPDSI = Borderline Personality Disorder Severity Index; BSS = Beck Scale for Suicide Ideation; CESD-R = Centre for Epidemiologic Studies Depression Scale; DERS = Difficulties in Emotion Regulation Scale; M = mean; MADRS = Montgomery-Äsberg Depression Rating Scale; NSSI = nonsuicidal self-injury; OTI = Opiate Treatment Index Section II; Polysubstances = 2 or more classes of substance; SASII = Suicide Attempt and Self-Injury Interview; SD = standard deviation.
a n = 136.
b n = 63.
c n = 73.
d n = 137.
e n = 74.
f n = 134.
g n = 62.
h n = 72.
i n = 133.
j n = 71.
l n = 61.
m n = 135.
n n = 118.
o n = 53.
p n = 65.
Table 4.
Functioning, Vocational Engagement, Academic Achievement, and Quality of Life.
| Characteristics | Descriptive statistic | Total sample N = 139 | 15 to 17 years N = 64 | 18 to 25 years N = 75 | Test statistic |
|---|---|---|---|---|---|
| Functioning and quality of life | |||||
| SOFAS | M (SD) | 58.1 (0.5) | 59.2 (8.2) | 57.1 (7.8) | t(137) = 1.54, P = 0.125 |
| IIPC | M (SD) | 121.5 (33.3) | 118.6 (31.8) | 123.9 (34.5) | t(137) = −0.94, P = 0.348 |
| SAS-SR | M (SD) | 2.8 (0.5) | 2.8 (0.5) | 2.9 (0.5) | t(137) = −0.43, P = 0.666 |
| AQoL-8D | M (SD) | 0.32 (0.13) | 0.33 (0.1) | 0.31 (0.1) | t(137) = 0.98, P = 0.329 |
| Achieved age-appropriate secondary school milestones a | % (n) | 65.5 (91) | 87.5 (56) | 46.7 (35) | χ2(1) = 25.5, P < 0.001 |
| Qualifications postsecondary school | |||||
| Nil | % (n) | 73.4 (102) | 93.8 (60) | 56.0 (42) | |
| Certificate | % (n) | 83.8 (31) | 6.3 (4) | 36.0 (27) | |
| Advanced diploma | % (n) | 10.8 (4) | 0 (0) | 5.3 (4) | |
| Bachelor degree | % (n) | 5.4 (2) | 0 (0) | 2.7 (2) | |
| Current work status | |||||
| Unemployed | % (n) | 38.1 (53) | 25.0 (16) | 49.3 (37) | |
| Homemaker or student | % (n) | 30.2 (42) | 43.8 (28) | 18.7 (14) | |
| Part-time employment (<11 hrs/week) | % (n) | 10.8 (15) | 15.6 (10) | 6.7 (5) | |
| Part-time employment (11 to 30 hrs/week) | % (n) | 11.5 (16) | 10.9 (7) | 12.0 (9) | |
| Full-time employment (>30 hrs/week) | % (n) | 7.2 (10) | 1.6 (1) | 12.0 (9) | |
| Medical or psychiatric leave | % (n) | 2.2 (3) | 3.1 (2) | 1.3 (1) | |
| NEET | M (SD) | 40.2 (56) | 28.1 (18) | 50.7 (38) | χ2(1) = 7.29, P = 0.007 |
| Current occupational classification | |||||
| Sales workers | % (n) | 64.3 (27)b | 94.7 (18)c | 39.1 (9)d | |
| Technicians and trades | % (n) | 11.9 (5)b | 0 (0)c | 21.7 (5)d | |
| Laborers | % (n) | 7.1 (3)b | 0 (0)c | 13.0 (3)d | |
| Community and personal service workers | % (n) | 7.1 (3)b | 0 (0)c | 13.0 (3)d | |
| Clerical and administrative workers | % (n) | 4.8 (2)b | 5.3 (1)c | 4.3 (1)d | |
| Managers | % (n) | 4.8 (2)b | 0 (0)c | 8.7 (2)d | |
| Main source of financial support | |||||
| Parents | % (n) | 33.1 (45)e | 57.4 (35)f | 13.3 (10)g | |
| Income through employment | % (n) | 25.0 (34)e | 21.3 (13)f | 28.0 (21)g | |
| Government (studying) | % (n) | 18.4 (25)e | 16.4 (10)f | 20.0 (15)g | |
| Government (unemployment) | % (n) | 14.7 (20)e | 1.6 (1)f | 25.3 (19)g | |
| Government (parenting) | % (n) | 2.9 (4)e | 0 (0)f | 5.3 (4)g | |
| Partner | % (n) | 2.2 (3)e | 0 (0)f | 4.0 (3)g | |
| Other family or friends | % (n) | 2.2 (3)e | 3.3 (2)f | 1.3 (1)g | |
| Government (disability) | % (n) | 1.5 (2)e | 0 (0)f | 2.7 (2)g | |
Note. AQoL-8D = Assessment of Quality of Life-8 Dimensions; IIPC = Inventory of Interpersonal Problems Circumplex Version; M = mean; NEET = not in education, employment, training or homemaking; SAS-SR = Social Adjustment Scale Self-Report; SD = standard deviation; SOFAS = Social and Occupational Functioning Assessment Scale.
aAge-appropriate milestone = Year 12 if 19 years or older, Year 11 if 18 years, Year 10 if 17 years old, Year 9 if 16 years old, Year 8 or below if 15 years old
b n = 42.
c n = 19.
d n = 23.
e n = 136.
f n = 61.
g n = 75.
Characteristics of Young People with BPD by Age
Comparisons between the adolescent (15- to 17-year-olds, n = 64) and young adult (18- to 25-year-olds, n = 75) groups are presented in Tables 1 to 4. The adolescents were significantly more likely to be living with siblings and/or biological parent(s). The young adults were significantly more likely to be living with a partner and to have children. More of the adolescents utilized psychosocial treatment (mental health sessions) while more of the young adults used medications. The young adults evidenced greater emotion regulation difficulties, and a significantly higher number of the young adults were diagnosed with ASPD compared with adolescents. The young adults evidenced greater alcohol, amphetamine, and polysubstance use than the adolescents. The adolescents commenced self-harming at a younger age and reported higher levels of nonsuicidal self-injury (NSSI). A higher number of the young adults had not achieved age-appropriate secondary school milestones and were NEET. All variables with a P < 0.10 were entered into a multivariable forward stepwise logistic regression analysis (specifically sex, living with siblings [yes/no], living with biological father and/or mother [yes/no], NEET [yes/no], achieved age-appropriate secondary school milestones [yes/no], medication use past 12 months [yes/no], mental health session use past 12 months [yes/no], number of mental health sessions past 12 months, SASII—NSSI [past 12 months; yes/no], BSS, BPDSI, ASPD [yes/no], DERS, OTI tobacco use in past month [yes/no], OTI alcohol use in past month [yes/no]). The final model had a Nagelkerke R 2 of 0.54, with 5 variables discriminating between the age groups: not achieving age-appropriate secondary school milestones (odds ratio [OR] = 9.34; 95% confidence interval [95% CI], 2.79 to 31.27), not living with birth parents (OR = 8.43; 95% CI, 2.85 to 24.94), NSSI (OR = 0.24; 95% CI, 0.06 to 0.95), NEET status (OR = 2.89; 95% CI, 1.01 to 8.23), and DERS total score (1.03; 95% CI, 1.01 to 8.28). Overall correct classification with this model was 80.2%, with 76.9% of 15- to 17-year-olds and 82.8% of 18 to 25-year-olds correctly classified.
Discussion
To the authors’ knowledge, this is the first study to compare the characteristics of adolescent (15 to 17 years) with young adult (18 to 25 years) outpatients with BPD who were at a similar stage of illness, that is, accessing evidence-based BPD treatment for the first time. Four key findings emerge from this study. First, young outpatients with BPD were severely unwell and were functioning poorly. Second, adolescent and young adult outpatients with BPD were more notable for their similarities than for any differences. Third, there were significant differences between the 2 age groups in household makeup, treatment history, presence of ASPD, degree of emotion dysregulation, pattern of substance use, age of onset and extent of self-harm, and achievement of age-appropriate vocational milestones. Fourth, membership of the adolescent group was predicted by living with one or both birth parents and a higher proportion of participants engaging in NSSI, whereas membership of the young adult group was predicted by not achieving age-appropriate educational milestones, NEET status, and emotion dysregulation.
With regard to the first aim of this study, the young people (n = 139) with BPD were characterized by acute, severe, and complex presentations. Consistent with previous studies of adolescents and adults with BPD, the young people in the current study had a high burden of mental state and personality psychopathology, 54 –56 high rates of lifetime self-harm, and a mean age of 13.2 years for the onset of self-harming behavior. 25,55 –58 Moreover, BPD severity, depressive symptomatology, and emotion regulation difficulties were all more severe in the current sample than among comparable samples of adolescents or adults (18- to 65-year-olds) with BPD. 37,38,59 –64 Notably, one-third of the sample met criteria for ASPD, reflecting broad inclusion criteria and few barriers to referral and a deliberate but uncommon decision not to exclude those with ASPD features from treatment services.
Nearly one-third of the current sample had posttraumatic stress disorder, which is around double the 9.9% to 16.9% reported in other adolescent samples 65,66 and more consistent with the 23.5% to 29% reported in young adults 22,23,67 and the 33% to 79% reported in adult samples. 68 This might reflect the older mean age of the sample and consequent greater chance of being exposed to trauma. This is consistent with the observation that traumatic experiences in people with BPD are not limited to childhood. 69
Consistent with the literature, the current sample evidenced severe functional impairment. 23,56,70 –74 For example, only 65.5% had passed an age-appropriate year level at school and 40% were NEET. In line with studies of adults with BPD, 75 –78 participants reported severely impaired quality of life, which was substantially worse than among their Australian peers (of any age) and also Australians with current mental state disorders and medical conditions, including cancer and cardiovascular disease. 79,80
With regard to the second aim of the study, adolescents (15 to 17 years, n = 64) and young adults (18 to 25 years, n = 75) in the current study showed substantial similarities among 20 key aspects of their presentation (e.g., quality of life, social functioning, mental state, and PD diagnoses). In concert with the data substantiating the developmental coherence of this age group, the findings of this study support the demographic, psychopathological, and functional consistency of BPD among adolescents and young adults. Notwithstanding this, there were some notable differences evident in the household makeup, treatment history, presence of ASPD (despite allowing for the diagnosis in the younger group), emotion dysregulation, substance use, self-harm, and educational/occupational engagement and achievement. This suggests that a “one size fits all” approach to early intervention is likely to be inadequate.
It is possible that observed differences in emotion dysregulation reflect greater divergence from normative development of regulation skills with increasing age. 81 –83 Greater emotion dysregulation might reflect the decreasing utility of individual’s adaptive strategies as they age 84 or greater societal tolerance of higher levels of emotion dysregulation among adolescents than among young adults. Persistence of this dysregulation into young adulthood might be increasingly recognized as pathological but might also lead to increasing substance use and/or use of prescribed psychotropic medication, again bringing this group to clinical attention.
Differences in substance use were evident, particularly in terms of polysubstance use, amphetamine, and alcohol use, with the young adults engaging in substance use at higher rates and severity. This finding is consistent with the peak age for the onset of substance use disorders being 18 to 20 years. 85 The finding might reflect the increasing accessibility and affordability of alcohol, with the purchase of alcohol being prohibited in Australia for those under 18 years of age.
The 2 age groups did not differ with regard to the severity of suicidal ideation and number of suicide attempts. However, a significantly greater proportion of the adolescent group reported engaging in NSSI and reported a greater number of NSSI acts. These findings are consistent with the natural course of self-harm, which peaks during the teenage years, then declines in late adolescence and early adulthood. 83,86,87
A higher proportion of young adults had not completed the expected level of secondary school education for their age and a higher proportion were NEET. This finding is likely to reflect, in part, that a young person cannot leave schooling until they are 17 years old and that they must attend a school campus until they finish Year 10. Overall, the findings are consistent with the literature demonstrating that mental health problems are associated with school dropout. 88 Failure to achieve normative educational milestones is likely to lead to cascading difficulties with pursuing further study and/or securing employment.
Finally, these findings suggest different pathways to care for adolescents versus young adults with BPD. In line with normal development, membership of the adolescent group was predicted by living with parent(s), as well as NSSI behaviors. This suggests that there is likely to be a stronger “safety net” of family, friends, or school staff in which self-harm is more readily identified, leading to a referral for care. Consistent with this, a higher proportion of the adolescent group had a history of psychosocial treatment and they had attended more mental health-related sessions, compared with the young adults. In contrast, membership of the young adult group was predicted by not completing education milestones and NEET status, along with emotion dysregulation (with a very small OR). Moreover, young adults were more disconnected from family, work, and study and only 17% were living with a partner. Taken together, this suggests a potentially longer pathway to care for young adults. It might be that, among this group, antisocial behaviors and substance use are key factors propelling entry into care. Yet, clinical experience suggests that antisocial behavior and substance use are often cited as reasons for clinical services to exclude individuals with BPD from care. Therefore, young adults with first-presentation BPD might be at particularly high risk of falling through the cracks of the mental health system, despite their demonstrably complex presentation and high need for care. This finding also suggests that the criteria for entry into BPD care should give equal or greater weight to factors in addition to self-harm, such as functional impairment.
Strengths and Limitations
This is a large and well characterized sample of young outpatients with BPD, having undergone comprehensive, standardized, multi-method (and multi-informant, where indicated) assessments, conducted by well-trained psychology graduates, as demonstrated by the high inter-rater reliability. All participants were assessed at a similar stage of illness (i.e., early in the course of the disorder) and they had not previously received evidence-based treatment for BPD. Therefore, course of illness effects, such as iatrogenic harm, polypharmacy, and other treatment effects are likely to have been minimized. The study had a high consent rate (80%), “real-world” inclusion criteria, and minimal exclusion criteria that allowed inclusion of young people with ASPD and substance use, which are typically associated with BPD. This means that this sample is likely to be highly representative of young people presenting to frontline, community mental health services, in both age categories, thus increasing the external validity of the findings.
Identifying, recruiting, and retaining such an acutely unwell group of young people with BPD is challenging. Despite assertive outreach by the research assistants, 23 young people were unable to complete the assessment in a timely manner, and 9 individuals moved out of the catchment area within 4 weeks of consent, thus rendering them ineligible for the study. Previous evidence from our group indicates that follow-up contact difficulty is associated with a greater burden of psychopathology, suggesting that the findings presented here might be an underestimate of the severity of problems among this sample. 89 Also, as the sample in the current study is derived from a RCT, participants were not only consenting to a cross-sectional assessment but also to treatment and longitudinal follow-up. This might have introduced biases into the sample.
Clinical and Research Implications
This study demonstrates the demographic, psychopathological, and functional consistency of BPD between the ages of 15 to 25 years. It appears no longer valid to distinguish adolescents from young adults with BPD, especially at the point where they turn 18-years-old. Many health systems are still limited by age divisions that reflect anachronistic development models. The current findings suggest that the PD and youth mental health fields should be more closely aligned, in order to guide prevention and early intervention and to assist young people with BPD to better navigate their transition to adulthood.
Acknowledgments
The authors would like to thank the patients, families, and staff of the Helping Young People Early program at Orygen and headspace Sunshine.
Authors’ Note: The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This trial was funded by a National Health and Medical Research Council (NHMRC) project grant (GNT0628739). Sue Cotton was supported by a NHMRC Career Development Fellowship (APP1061998, 2014-2017) and is currently supported by a NHMRC Senior Research Fellowship (APP1136344, 2018-). Christopher Davey was supported by a NHMRC Career Development Fellowship (APP1061757, 2014-2017).
ORCID iD: Andrew M. Chanen, MBBS (Hons), PhD, FRANZCP https://orcid.org/0000-0003-4468-622X
Jennifer K. Betts, DPsych(Clin) https://orcid.org/0000-0003-4146-2343
References
- 1. Chanen AM, McCutcheon L. Prevention and early intervention for borderline personality disorder: current status and recent evidence. Br J Psychiatry Suppl. 2013;54s:s24–29. [DOI] [PubMed] [Google Scholar]
- 2. Chanen AM, Thompson KN. The age of onset of personality disorders. In: de Girolamo G, McGorry PD, Sartorius N, editors. Age of onset of mental disorders: etiopathogenetic and treatment implications. Cham: Springer International Publishing; 2019:183–201. [Google Scholar]
- 3. Chanen A, Sharp C, Hoffman P, Prevention GA. Prevention and early intervention for borderline personality disorder: a novel public health priority. World Psychiatry. 2017;16(2):215–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chanen AM, Nicol K, Betts JK, Thompson KN. Diagnosis and treatment of borderline personality disorder. Curr Psychiatry Rep. 2020;22(5):25. [DOI] [PubMed] [Google Scholar]
- 5. Laurenssen EMP, Hutsebaut J, Feenstra DJ, Van Busschbach JJ, Luyten P. Diagnosis of personality disorders in adolescents: a study among psychologists. Child Adolesc Psychiatry Ment Health. 2013;7(1):1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dahl RE, Allen NB, Wilbrecht L, Suleiman AB. Importance of investing in adolescence from a developmental science perspective. Nature. 2018;554(7693):441–450. [DOI] [PubMed] [Google Scholar]
- 7. Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child Adolesc Health. 2018;2(3):223–228. [DOI] [PubMed] [Google Scholar]
- 8. Arnett JJ, Žukauskienė R, Sugimura K. The new life stage of emerging adulthood at ages 18–29 years: implications for mental health. Lancet Psychiatry. 2014;1(7):569–576. [DOI] [PubMed] [Google Scholar]
- 9. Newton-Howes G, Clark LA, Chanen A. Personality disorder across the life course. Lancet. 2015;385(9969):727–734. [DOI] [PubMed] [Google Scholar]
- 10. Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry 2005;62(6):593–602. [DOI] [PubMed] [Google Scholar]
- 11. Malla A, Iyer S, McGorry P, et al. From early intervention in psychosis to youth mental health reform: a review of the evolution and transformation of mental health services for young people. Soc Psychiatry Psychiatr Epidemiol. 2016;51(3):319–326. [DOI] [PubMed] [Google Scholar]
- 12. McGorry PD, Mei C. Early intervention in youth mental health: progress and future directions. Evid Based Ment Health. 2018;21(4):182–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chanen AM. Borderline personality disorder in young people: are we there yet? J Clin Psychol. 2015;71(8):778–s791. [DOI] [PubMed] [Google Scholar]
- 14. Wong J, Bahji A, Khalid-Khan S. Psychotherapies for adolescents with subclinical and borderline personality disorder: a systematic review and meta-analysis. Can J Psychiatry. 2020;65(1):5–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gleeson JFM, Chanen A, Cotton SM, Pearce T, Newman B, McCutcheon L. Treating co-occurring first-episode psychosis and borderline personality: a pilot randomized controlled trial. Early Interv Psychiatry. 2012;6(1):21–29. [DOI] [PubMed] [Google Scholar]
- 16. Wong J, Bahji A, Khalid-Khan S. Systematic review and meta-analyses of psychotherapies for adolescents with subclinical and borderline personality disorder: a reply to the commentary by Jørgensen, Storebø, and Simonsen. Can J Psychiatry. 2020;65(5):356–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Scalzo F, Hulbert CA, Betts JK, Cotton SM, Chanen AM. Substance use in youth with borderline personality disorder. J Pers Disord. 2018;32(5);603–618. [DOI] [PubMed] [Google Scholar]
- 18. Scalzo F, Hulbert CA, Betts JK, Cotton SM, Chanen AM. Predictors of substance use in youth with borderline personality disorder. Personal Disord. 2018;9(4):390–396. [DOI] [PubMed] [Google Scholar]
- 19. Andrewes HE, Hulbert C, Cotton SM, Betts J, Chanen AM. Patterns of non-suicidal self-injury and their relationship with suicide attempts in youth with borderline personality disorder. Arch Suicide Res 2018;22(3):465–478. [DOI] [PubMed] [Google Scholar]
- 20. Andrewes HE, Hulbert C, Cotton SM, Betts J, Chanen AM. Relationships between the frequency and severity of non-suicidal self-injury and suicide attempts in youth with borderline personality disorder. Early Interv Psychiatry. 2019;13(2):194–201. [DOI] [PubMed] [Google Scholar]
- 21. Andrewes HE, Hulbert C, Cotton SM, Betts J, Chanen AM. Ecological momentary assessment of nonsuicidal self-injury in youth with borderline personality disorder. Personal Disord. 2017;8(4):357–365. [DOI] [PubMed] [Google Scholar]
- 22. Kaplan C, Tarlow N, Stewart JG, Aguirre B, Galen G, Auerbach RP. Borderline personality disorder in youth: the prospective impact of child abuse on non-suicidal self-injury and suicidality. Compr Psychiatry. 2016;71:86–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Frías Á, Palma C, Solves L, Martínez B, Salvador A. Differential symptomatology and functioning in borderline personality disorder across age groups. Psychiatry Res. 2017;258:44–50. [DOI] [PubMed] [Google Scholar]
- 24. Cavelti M, Thompson KN, Hulbert C, et al. Exploratory comparison of auditory verbal hallucinations and other psychotic symptoms among youth with borderline personality disorder or schizophrenia spectrum disorder. Early Interv Psychiatry. 2019;13(5):1252–1262. [DOI] [PubMed] [Google Scholar]
- 25. Goodman M, Tomas IA, Temes CM, Fitzmaurice GM, Aguirre BA, Zanarini MC. Suicide attempts and self-injurious behaviours in adolescent and adult patients with borderline personality disorder. Personal Ment Health. 2017;11(3):157–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chanen AM, Velakoulis D, Carison K, et al. Orbitofrontal, amygdala and hippocampal volumes in teenagers with first-presentation borderline personality disorder. Psychiatry Res. 2008;163(2):116–125. [DOI] [PubMed] [Google Scholar]
- 27. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Arlington (VA; ): American Psychiatric Association; 2013. [Google Scholar]
- 28. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Text Rev. Washington (DC): American Psychiatric Association; 2000. [Google Scholar]
- 29. Chanen A, Jackson H, Cotton SM, et al. Comparing three forms of early intervention for youth with borderline personality disorder (the MOBY study): study protocol for a randomised controlled trial. Trials. 2015;16(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. National Collaborating Centre for Mental Health. Borderline Personality Disorder: the NICE Guideline on Treatment and Management. Leicester & London: The British Psychological Society & The Royal College of Psychiatrists; 2009. [Google Scholar]
- 31. Australian Bureau of Statistics. 2006 census of population and housing Australia (Cat. No. 2068.0 - 2006 Census Tables). [accessed 2021 Feb 02]. https://www.abs.gov.au/websitedbs/censushome.nsf/home/historicaldata2006?opendocument=280 2006.
- 32. Pink B, Bascand G. ANZSCO-Australian and New Zealand standard classification of occupations-first edition, revision 1. Canberra (ACT): Australian Bureau of Statistics; 2009. [Google Scholar]
- 33. Australian Bureau of Statistics. Census of population and housing: socio-economic indexes for areas (SEIFA), Australia 2011. (Catalogue number 2033.0.55.001); 2013.
- 34. First MB, Gibbon M, Spitzer RL, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders - Patient Version (SCID-I/P). New York (NY): Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- 35. First MB, Gibbon M, Spitzer RL, Benjamin LS, Williams JB. User’s guide for the structured clinical interview for DSM-IV axis II personality disorders. Washington (DC): American Psychiatric Press; 1997. [Google Scholar]
- 36. Cohen P, Crawford TN, Johnson JG, Kasen S. The children in the community study of developmental course of personality disorder. J Pers Disord. 2005;19(5):466–486. [DOI] [PubMed] [Google Scholar]
- 37. Arntz A, van den Hoorn M, Cornelis J, Verheul R, van den Bosch WM, de Bie AJ. Reliability and validity of the borderline personality disorder severity index. J Pers Disord. 2003;17(1):45–59. [DOI] [PubMed] [Google Scholar]
- 38. Giesen-Bloo JH, Wachters LM, Schouten E, Arntz A. The borderline personality disorder severity index-IV: psychometric evaluation and dimensional structure. Pers Individ Dif. 2010;49(2):136–141. [Google Scholar]
- 39. Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. 2004;26(1):41–54. [Google Scholar]
- 40. Gratz KL, Roemer L. The relationship between emotion dysregulation and deliberate self-harm among female undergraduate students at an urban commuter university. Cogn Behav Ther 2008;37(1):14–25. [DOI] [PubMed] [Google Scholar]
- 41. Eaton WW, Smith C, Ybarra M, Muntaner C, Tien A. Center for epidemiologic studies depression scale: review and revision (CESD and CESD-R). In: Maruish M, editor. The use of psychological testing for treatment planning and outcome assessment. 3rd ed. New York (NY): Lawrence Erlbaum; 2004:363–377. [Google Scholar]
- 42. Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389. [DOI] [PubMed] [Google Scholar]
- 43. Williams JBW, Kobak KA. Development and reliability of a structured interview guide for the Montgomery--Asberg depression rating scale (SIGMA). Br J Psychiatry. 2008;192(1):52–58. [DOI] [PubMed] [Google Scholar]
- 44. Beck AT, Brown GK, Steer RA. Psychometric characteristics of the scale for suicide ideation with psychiatric outpatients. Behav Res Ther. 1997;35(11):1039–1046. [DOI] [PubMed] [Google Scholar]
- 45. Linehan MM, Comtois KA, Brown MZ, Heard HL, Wagner A. Suicide attempt self-injury interview (SASII): development, reliability, and validity of a scale to assess suicide attempts and intentional self-injury. Psychol Assess. 2006;18(3):303–312. [DOI] [PubMed] [Google Scholar]
- 46. Darke S, Ward J, Hall W, Heather N, Wodak A. The opiate treatment index (OTI) manual. Sydney (NSW): National Drug and Alcohol Research Centre; 1991. [Google Scholar]
- 47. Saunders JB, Aasland OG, Babor TF, De La Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88(6):791–804. [DOI] [PubMed] [Google Scholar]
- 48. Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. 2nd ed. Geneva: World Health Organisation Department of Mental Health and Substance Dependence; [accessed 2021 Feb 2]. https://apps.who.int/iris/handle/10665/67205 2001. [Google Scholar]
- 49. Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Arch Gen Psychiatry. 1976;33(9):1111–1115. [DOI] [PubMed] [Google Scholar]
- 50. Alden LE, Wiggins JS, Pincus AL. Construction of circumplex scales for the inventory of interpersonal problems. J Pers Assess. 1990;55(3-4):521–536. [DOI] [PubMed] [Google Scholar]
- 51. Horowitz LM, Alden LE, Wiggins JS, et al. Inventory of Interpersonal Problems Manual. Menlo Park, (CA): Mind Garden, Inc; 2003. [Google Scholar]
- 52. Goldman HH, Skodol AE, Lave TR. Revising axis V for DSM-IV: a review of measures of social functioning. Am J Psychiatry. 1992;149(9):1148–1156. [DOI] [PubMed] [Google Scholar]
- 53. Richardson J, Iezzi A, Khan MA, Maxwell A. Validity and reliability of the assessment of quality of life (AQoL)-8D multi-attribute utility instrument. Patient. 2014;7(1):85–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Kaess M, von Ceumern-Lindenstjerna I-A, Parzer P, et al. Axis I and II comorbidity and psychosocial functioning in female adolescents with borderline personality disorder. Psychopathology. 2013;46(1):55–62. [DOI] [PubMed] [Google Scholar]
- 55. Kaess M, Fischer-Waldschmidt G, Resch F, Koenig J. Health related quality of life and psychopathological distress in risk taking and self-harming adolescents with full-syndrome, subthreshold and without borderline personality disorder: rethinking the clinical cut-off? Borderline Personal Disord Emot Dysregul. 2017;4(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Chanen AM, Jovev M, Jackson HJ. Adaptive functioning and psychiatric symptoms in adolescents with borderline personality disorder. J Clin Psychiatry. 2007;68(2):297–306. [DOI] [PubMed] [Google Scholar]
- 57. Zanarini MC, Frankenburg FR, Ridolfi ME, et al. Reported childhood onset of self-mutilation among borderline patients. J Pers Disord 2006;20(1):9–15. [DOI] [PubMed] [Google Scholar]
- 58. Turner BJ, Dixon-Gordon KL, Austin SB, Rodriguez MA, Rosenthal MZ, Chapman AL. Non-suicidal self-injury with and without borderline personality disorder: differences in self-injury and diagnostic comorbidity. Psychiatry Res. 2015;230(1):28–35. [DOI] [PubMed] [Google Scholar]
- 59. Zanarini MC, Schulz SC, Detke HC, et al. A dose comparison of olanzapine for the treatment of borderline personality disorder: a 12-week randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2011;72(10):1353–1362. [DOI] [PubMed] [Google Scholar]
- 60. Bøen E, Hummelen B, Elvsåshagen T, et al. Different impulsivity profiles in borderline personality disorder and bipolar II disorder. J Affect Disord. 2015;170(C):104–111. [DOI] [PubMed] [Google Scholar]
- 61. Fowler JC, Madan A, Allen JG, Oldham JM, Frueh BC. Differentiating bipolar disorder from borderline personality disorder: diagnostic accuracy of the difficulty in emotion regulation scale and personality inventory for DSM-5. J Affect Disord. 2019;245:856–860. [DOI] [PubMed] [Google Scholar]
- 62. Krause-Utz A, Erol E, Brousianou AV, et al. Self-reported impulsivity in women with borderline personality disorder: the role of childhood maltreatment severity and emotion regulation difficulties. Borderline Personal Disord Emot Dysregul. 2019;6(1):1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Kröger C, Vonau M, Kliem S, Roepke S, Kosfelder J, Arntz A. Psychometric properties of the German version of the borderline personality disorder severity index--version IV. Psychopathology. 2013;46(6):396–403. [DOI] [PubMed] [Google Scholar]
- 64. Schuppert HM, Timmerman ME, Bloo J, et al. Emotion regulation training for adolescents with borderline personality disorder traits: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2012;51(12):1314–1323. [DOI] [PubMed] [Google Scholar]
- 65. Beck E, Bo S, Jørgensen MS, et al. Mentalization-based treatment in groups for adolescents with borderline personality disorder: a randomized controlled trial. J Child Psychol Psychiatry, 2020;61(5):594–604. [DOI] [PubMed] [Google Scholar]
- 66. Mehlum L, Tørmoen AJ, Ramberg M, et al. Dialectical behavior therapy for adolescents with repeated suicidal and self-harming behavior: a randomized trial. J Am Acad Child Adolesc Psychiatry. 2014;53(10):1082–1091. [DOI] [PubMed] [Google Scholar]
- 67. Venta A, Kenkel-Mikelonis R, Sharp C. A preliminary study of the relation between trauma symptoms and emerging BPD in adolescent inpatients. Bull Menninger Clin. 2012;76(2):130–146. [DOI] [PubMed] [Google Scholar]
- 68. Frías A, Palma C. Comorbidity between post-traumatic stress disorder and borderline personality disorder: a review. Psychopathology. 2015;48(1):1–10. [DOI] [PubMed] [Google Scholar]
- 69. Zanarini MC, Frankenburg FR, Reich DB, Hennen J, Silk KR. Adult experiences of abuse reported by borderline patients and axis II comparison subjects over six years of prospective follow-up. J Nerv Ment Dis. 2005;193(6):412–416. [DOI] [PubMed] [Google Scholar]
- 70. Kramer U, Temes CM, Magni LR, et al. Psychosocial functioning in adolescents with and without borderline personality disorder. Personal Ment Health. 2017;11(3):164–170. [DOI] [PubMed] [Google Scholar]
- 71. Chen H, Cohen P, Johnson JG, Kasen S, Sneed JR, Crawford TN. Adolescent personality disorders and conflict with romantic partners during the transition to adulthood. J Pers Disord. 2004;18(6):507–525. [DOI] [PubMed] [Google Scholar]
- 72. Vaillancourt T, Brittain HL, McDougall P, et al. Predicting borderline personality disorder symptoms in adolescents from childhood physical and relational aggression, depression, and attention-deficit/hyperactivity disorder. Dev Psychopathol. 2014;26(3):817–830. [DOI] [PubMed] [Google Scholar]
- 73. Wolke D, Schreier A, Zanarini MC, Winsper C. Bullied by peers in childhood and borderline personality symptoms at 11 years of age: a prospective study. J Child Psychol Psychiatry. 2012;53(8):846–855. [DOI] [PubMed] [Google Scholar]
- 74. Wlodarczyk J, Lawn S. The developmental trajectory of borderline personality disorder and peer victimisation: Australian family carers’ perspectives. Emot Behav Difficulties. 2017;22(2):98–110. [Google Scholar]
- 75. Grambal A, Prasko J, Kamaradova D, et al. Quality of life in borderline patients comorbid with anxiety spectrum disorders - a cross-sectional study. Patient Prefer Adherence. 2016;10:1421–1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. IsHak WW, Elbau I, Ismail A, et al. Quality of life in borderline personality disorder. Harv Rev Psychiatry. 2013;21(3):138–150. [DOI] [PubMed] [Google Scholar]
- 77. Narud K, Mykletun A, Dahl AA. Quality of life in patients with personality disorders seen at an ordinary psychiatric outpatient clinic. BMC Psychiatry. 2005;5(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Soeteman DI, Verheul R, Busschbach JJV. The burden of disease in personality disorders: diagnosis-specific quality of life. J Pers Disord. 2008;22(3):259–268. [DOI] [PubMed] [Google Scholar]
- 79. Maxwell A, Özmen M, Iezzi A, Richardson J. Deriving population norms for the AQoL-6D and AQoL-8D multi-attribute utility instruments from web-based data. Qual Life Res. 2016;25(12):3209–3219. [DOI] [PubMed] [Google Scholar]
- 80. Hawthorne G, Korn S, Richardson J. Population norms for the AQoL derived from the 2007 Australian national survey of mental health and wellbeing. Aust NZJ Public Health. 2013;37(1):7–16. [DOI] [PubMed] [Google Scholar]
- 81. Cole PM, Martin SE, Dennis TA. Emotion regulation as a scientific construct: methodological challenges and directions for child development research. Child Dev. 2004;75(2):317–333. [DOI] [PubMed] [Google Scholar]
- 82. Thompson RA. Emotion regulation: a theme in search of definition. Monogr Soc Res Child Dev. 1994;59(2-3):25–52. [PubMed] [Google Scholar]
- 83. Videler AC, Hutsebaut J, Schulkens JEM, Sobczak S, Van Alphen SP. A life span perspective on borderline personality disorder. Curr Psychiatry Rep. 2019;21(7):51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Daros AR, Williams GE. A meta-analysis and systematic review of emotion-regulation strategies in borderline personality disorder. Harv Rev Psychiatry. 2019;27(4):217–232. [DOI] [PubMed] [Google Scholar]
- 85. Dennis M, Scott CK. Managing addiction as a chronic condition. Addict Sci Clin Pract. 2007;4(1):45–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice GM. Fluidity of the subsyndromal phenomenology of borderline personality disorder over 16 years of prospective follow-up. Am J Psychiatry. 2016;173(7):688–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Moran P, Coffey C, Romaniuk H, et al. The natural history of self-harm from adolescence to young adulthood: a population-based cohort study. Lancet. 2012;379(9812):236–243. [DOI] [PubMed] [Google Scholar]
- 88. Caruana E, Farhall J, Cotton SM, et al. Vocational engagement among young people entering mental health treatment compared with their general population peers. Early Interv Psychiatry. 2019;13(3):692–696. [DOI] [PubMed] [Google Scholar]
- 89. Allott K, Chanen A, Yuen HP. Attrition bias in longitudinal research involving adolescent psychiatric outpatients. J Nerv Ment Dis. 2006;194(12):958–961. [DOI] [PubMed] [Google Scholar]