Abstract
Objectives
Following the emergence of the Delta variant of SARS-CoV-2 in Singapore, our hospital experienced a Delta-linked ward cluster. In this study, we review the enhanced strategies in preventing nosocomial transmission of COVID-19 following widespread community transmission of the Delta variant.
Methods
We conducted a cohort study on exposures to unexpected COVID-19 cases for which contact tracing was initiated from June 2021 to October 2021. Strategies evaluated included upgraded personal protective equipment (PPE) and rostered routine testing (RRT) for staff and patients, surveillance of staff with acute respiratory illness (ARI), and expanded quarantining and testing for contacts of identified cases.
Results
From 193 unexpected COVID-19 exposures, 2,573 staff, 542 patients, and 128 visitor contacts were traced. Four staff contacts subsequently had SARS-CoV-2 infection. Two were likely from exposure in community settings, whereas 2 had exposure to the same COVID-19 positive staff in the hospital, forming the only hospital cluster. One inpatient had a nosocomial infection, possibly from visitors. The SARS-CoV-2 detection rate among staff was 0.3% (of 11,200 staff) from biweekly RRT and 2.5% (of 3,675 staff) from ARI surveillance.
Conclusion
Enhanced hospital measures, including upgraded PPE and RRT for staff and patients, staff sickness surveillance, and more rigorous management of contacts of COVID-19 cases, were likely to have reduced nosocomial transmission amid the Delta variant.
Keywords: COVID-19, Delta, personal protective equipment, staff surveillance, rostered routine testing
Introduction
From September 2020 to mid-April 2021, fewer than 5 COVID-19 community cases were reported in Singapore daily. However, in April 2021, the Delta (B.1.617.2) variant of SARS-CoV-2 emerged, with a shorter incubation period and higher transmissibility compared with the ancestral strain (Zhang et al., 2021). This variant was responsible for causing a hospital cluster in end-April 2021 and quickly became the predominant circulating strain in Singapore, fueling the resurgence of COVID-19 cases despite >80% vaccination rate in the Singaporean adult population (Lim et al., 2022, Ministry of Health S 2021a, 2021b).
Until then, hospital measures against COVID-19, including appropriate personal protective equipment (PPE) for staff, staff temperature and sickness monitoring, and contact tracing and surveillance of individuals with potential COVID-19 exposure have been effective in preventing nosocomial transmission of COVID-19 (Chow et al., 2020a; Htun et al., 2020). However, the emergence of the Delta-linked ward cluster signaled a need to strengthen our hospital's defenses in managing COVID-19 (Teo, 2021). Thus, we implemented PPE upgrade and rostered routine testing (RRT) for staff and inpatients, aggressive quarantine practices and testing measures for exposed contacts, and ward environmental enhancements. We describe and review the effectiveness of these strategies in preventing the nosocomial transmission of COVID-19 amid widespread community transmission.
Material and methods
Design, Setting, and Participants
Tan Tock Seng Hospital (TTSH) is a 1,600-bed multidisciplinary acute care hospital with close to 13,000 staff. It supports the co-located 330-bed National Centre for Infectious Diseases (NCID), which is the designated center for outbreaks of Emerging Infectious Diseases (EIDs) in Singapore. Since January 2020, the campus has managed more than 14,000 patients with COVID-19.
We conducted a cohort study of unexpected exposures to COVID-19 cases for which contact tracing was initiated from June 6, 2021, to October 9, 2021, covering 18 epidemiological weeks, post-closure of the Delta-linked cluster in TTSH.
Upgraded PPE for staff, patients, and visitors
From May 2, 2021, the recommended minimum PPE for all staff during patient interactions in non-COVID-19 wards was upgraded from surgical mask to N95 mask and eye protection, and this was extended to staff in clinics from July 23, 2021 (Table 1 ). Staff managing suspected/confirmed COVID-19 cases, working in high-risk areas such as the emergency department, or performing aerosol-generating procedures had to don a full set of PPE (N95 mask or equivalent, gown, gloves, and eye protection) as per existing recommendations.
Table 1.
Risk-based enhanced personal protective equipment matrix for staff, patients, and visitors
| Category | Hand hygiene | N95 mask or equivalent | Surgical mask | Eye protection (e.g. face shield/goggles) | Gown/ Apron | Gloves |
|---|---|---|---|---|---|---|
| STAFF | ||||||
| (1) Isolation rooms | ||||||
| All staff, including housekeeping staff | ✓ | ✓ | ✓ | ✓ | ✓ | |
| (2) Inpatients/ Ambulatory/ Radiology and Procedural areas | ||||||
| Medical/ Nursing, allied health professionals*, housekeeping staff | ✓ | ✓ | ✓ | |||
| (3) Specialist outpatient clinics | ||||||
| Medical/ Nursing staff, allied health professionals* | ✓ | ✓ | ✓ | |||
| Patient service associates | ✓ | ✓ | ✓ | |||
| Staff transporting specimens to laboratory | ✓ | ✓ | ||||
| Housekeeping staff (when cleaning toilets) | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Staff at forward triage areas (e.g., hospital entrances, gantries) | ✓ | ✓ | ✓ | |||
| (4) Emergency department | ||||||
| Security officers at ED entrances | ✓ | ✓ | ✓ | |||
| Security officers at ED non-fever/fever zone | ✓ | ✓ | ✓ | ✓ | ✓ | |
| All other staff working at any area of ED | ✓ | ✓ | ✓ | ✓ | ✓ | |
| (5) Ancillary staff | ||||||
| Ambulance driver | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Staff performing ambulance decontamination | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Waste disposal | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Spill management | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Mortuary staff† | ✓ | |||||
| (6) Non-patient-fronting staff | ✓ | |||||
| PATIENTS (inpatients or outpatients) | ✓ | |||||
| VISITORS (inpatients or outpatients) | ✓ |
Allied health professionals include pharmacists, occupational therapists, physiotherapists, phlebotomists, radiographers, and respiratory therapists.
No autopsy or embalmment done.
Abbreviations: ED = emergency department.
Inpatients were advised to don surgical masks where tolerated, particularly when leaving their rooms/beds and during transfers for procedures outside the ward. In line with the national mask-wearing policy, patients visiting outpatient clinics and visitors to the hospital were also required to wear masks.
Management of unexpected exposures
Unexpected exposure was defined as exposure to an individual with polymerase chain reaction (PCR)–confirmed COVID-19 within the hospital premises when the individual was not identified at the outset and managed according to the suspected COVID-19 protocol. Upon the detection of an unexpected COVID-19 case, contact tracing would immediately commence. The following 2 types of contacts during the index case's infectious period were traced: (i) close contact: an individual within 2 meters of the COVID-19 case for a cumulative duration of ≥15 minutes and (ii) transient contact: a potentially exposed person (e.g. in the ward at the same time but did not fulfill the close contact criteria). Each contact was followed up for 14 days (the maximum incubation period of SARS-CoV-2) from the last exposure.
Staff close contacts who had unprotected exposure (minimally not donning a surgical mask) were furloughed and quarantined at home for 14 days following the last date of exposure to the case, whereas those with protected exposure (minimally donning a surgical mask, or N95 or equivalent, but not the full set of PPE) underwent various combinations of hospital measures, including SARS-CoV-2 PCR testing regimes, and temperature and acute respiratory illness (ARI) symptom surveillance by the Ministry of Health (MOH) or their respective Heads of Departments. Staff contacts who were in a full set of PPE did not require follow-up. Inpatient close contacts were isolated in negative pressure single rooms for 14 days and underwent SARS-CoV-2 PCR testing. The MOH followed up with public health actions for outpatient or visitor close contacts.
Areas and surfaces contacted by the unexpected COVID-19 case were thoroughly cleaned. For exposures in the general ward, the ward would be locked down to restrict patient movements (admission/transfer/discharge), and visitors would be disallowed, with exceptions for critically ill patients. In addition, staff based in the affected wards would also be screened for SARS-CoV-2 by way of a PCR test at the point of notification of exposure event. The lockdown would then be lifted when SARS-CoV-2 was not detected in all screening swabs.
Enhanced staff ARI surveillance
Ongoing hospital-wide enhanced staff sickness surveillance was established in addition to routine staff sickness absenteeism surveillance to identify sick staff early and prevent nosocomial COVID-19 transmission owing to infected staff. Sick staff and their SARS-CoV-2 PCR results were monitored daily (Htun et al., 2020).
We assessed the changes in temporal trends of ARI incidence among staff using joinpoint regression, with an epidemiological week as the independent variable. This regression uses data to fit the simplest joinpoint model and tests the statistical significance of joinpoints using the Monte Carlo permutation while setting the level of significance at 0.05 and a maximum number of joinpoints at 2 (Kim et al., 2000). Weekly percent change (WPC) was estimated for each segment along with a 95% confidence interval (CI) using the Joinpoint Regression Program version 4.9.0.0.
Staff and patient rostered routine testing
Singapore implemented RRT for all staff working in acute care hospitals on May 5, 2021. At TTSH and NCID, weekly or fortnightly RRT cycles were administered by way of SARS-CoV-2 PCR test for unvaccinated and fully vaccinated staff, respectively.
SARS-CoV-2 PCR tests were performed for all inpatients on admission on day 4, day 7, and subsequently, weekly. Inpatients also needed to undergo a PCR test 48 hours before planned discharges to home or step-down healthcare facilities.
Individuals were considered fully vaccinated 2 weeks after receiving the second dose of either the Pfizer-BioNTech (BNT162b2), Moderna (mRNA-1273), or Sinovac-CoronaVac COVID-19 Vaccine series.
Other safe management measures
Staff were advised to order only takeout meals and to eat alone at their work desks or assigned staff pantries within their work zones. Vaccinated staff were further allowed to use designated staff eating areas within the hospital food and beverage outlets but were to eat alone with no interactions across tables. Other workplace measures included split-teams, teleconsultations, and work-from-home arrangements where practicable.
Visitor restriction
Visiting guidelines changed several times throughout the study period. The maximum number of visitors per patient per day and at the bedside at any one time, as well as maximum visiting duration, was limited to varying degrees, with exceptions granted on a case-by-case basis (Chan, 2021). From August 19, 2021, all visitors to hospital wards also needed to show a valid negative Antigen Rapid Test (ART) or PCR result within 24 hours, with fully vaccinated visitors exempted only until September 23, 2021 (Ministry of Health, 2021c, Tham, 2021).
Enhancements to the hospital environment
Other safe management measures such as safe distancing in clinic waiting areas and enhanced cleaning of common facilities, high-touch surfaces, and equipment were implemented. Several environmental enhancements, including installation of high-speed extraction fans to improve air circulation in general wards and placement of portable high-efficiency particulate absorbing (HEPA) filters in patients’ rooms and clinics, were carried out.
Results
Staff RRT
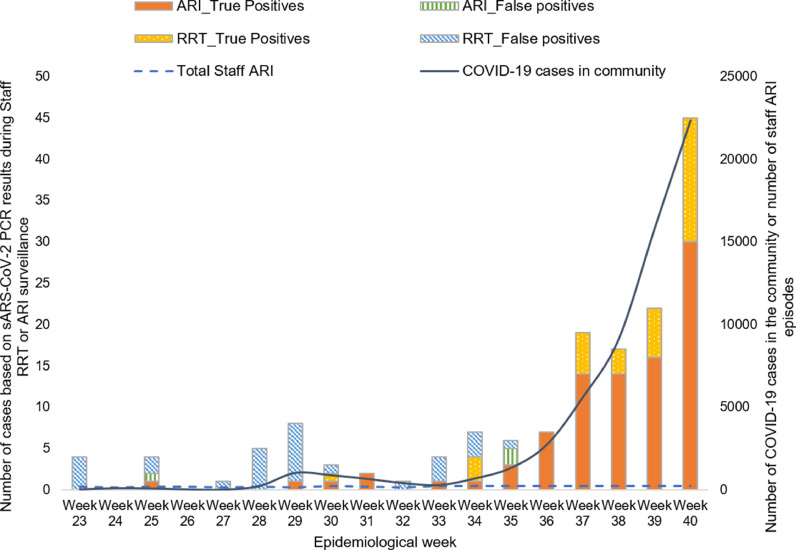
From June 6, 2021, to October 9, 2021 (Epidemiological Weeks 23-40, 2021), an average of 11,200 staff underwent biweekly SARS-CoV-2 PCR RRT, and 61 (0.5%) had detected/equivocal results. Among them, 40 (66%) and 21 (34%) were ‘detected’ and ‘equivocal’ (i.e. borderline positive with cycle threshold >37-45), respectively (Fig. 1 ). Among the 40 staff with detected SARS-CoV-2 results, 7 (17.5%) had 2 subsequent swabs taken 24 hours apart yielding negative results by the hospital's laboratory and the national reference laboratory and were classified as ‘false positives’ (Table 2 ). Of the remaining 33 (82.5%) staff that were true positives, 22 remained asymptomatic throughout the illness, whereas 11 subsequently developed ARI symptoms. All 21 staff with equivocal SARS-CoV-2 results remained asymptomatic, and 2 subsequent swabs taken 24 hours apart yielded negative results and were categorized as false positives. Thus, 33 staff had true positives PCR arising from RRT provided a SARS-CoV-2 detection rate of 0.3% (Table 2).
Figure 1.
Table 2.
Categories of staff screened for and detected with SARS-CoV-2 infection from rostered routine testing (RRT) and staff acute respiratory illness (ARI) surveillance, June 6, 2021 – October 9, 2021
| SARS-CoV-2 test result |
||||||
|---|---|---|---|---|---|---|
| Screening category | Staff screened | True positive SARS-CoV-2 DetectionRate, % | ||||
| Detected, No. | Equivocal and subsequent samples detected, No. | False positive*, No. | Not Detected, No. | |||
| Staff RRT | 11200 | 33 | 0 | 28 | 11142 | 0.3% |
| Staff ARI | 3675 | 90 | 1 | 3 | 3574 | 2.5% |
First swab result Detected/Equivocal but Not Detected on 2 subsequent samples sent 24 hours apart.
Abbreviations: ARI = acute respiratory illness; RRT = rostered routine testing
Staff ARI surveillance
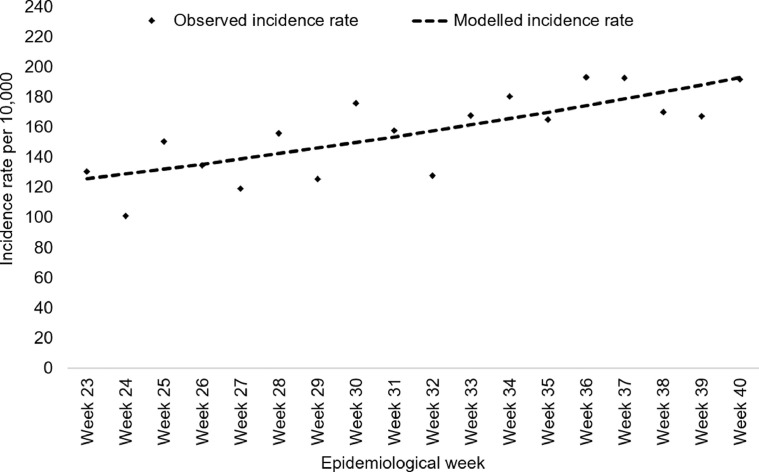
For the same period, 3,675 staff with ARI were identified. A joinpoint regression analysis showed a significant rising trend in the incidence rate of staff ARI (WPC 2.6%, 95% CI 1.4-3.7, P <0.001) (Fig. 2 ).
Figure 2.
A total of 94 (2.6%) staff had detected/equivocal SARS-CoV-2 test results, of which 92 (98%) were detected and 2 (2%) were equivocal. Of the 92 staff with a detected result, 2 had 2 subsequent swabs taken 24 hours apart that yielded negative results and were classified as false positives. Of the 2 staff with an equivocal result, 1 subsequently had a detected result and was confirmed with COVID-19. The remaining staff had 2 subsequent swabs taken 24 hours apart that yielded negative results and was classified as a false positive. Altogether, 91 staff had true positive results from staff ARI surveillance, giving a true positive SARS-CoV-2 detection rate of 2.5% (Table 2).
Unexpected exposures to COVID-19 staff and patients
There were 193 unexpected exposures to COVID-19 staff (n=135), patients (n=43) and visitors (n=15) (Table 3 ). Incidents occurred in the ward (n=83), clinic (n=51), and other parts of the hospital (n=58).
Table 3.
Numbers of staff, patient, and visitor contacts traced from exposures to unexpected staff, patient, and visitor COVID-19 cases in the hospital from June 6, 2021, to October 9, 2021, as well as details of positive SARS-COV-2 PCR test results from surveillance swabs of these contacts
| Unexpected COVID-19 cases | Staff contacts and PPE used during exposure to unexpected COVID-19 case | Close* patient contacts | Close* visitor contacts | |||
|---|---|---|---|---|---|---|
| N95 (close) | N95 (transient) | Surgical mask (close) | Unprotected exposure (close) | |||
| Staff cases (n=135) | 376 | 1459 | 170 | 160 | 355 | 28 |
| Patient cases (n=43) | 198 | 188 | 2 | 0 | 171 | 100 |
| Visitor cases (n=15) | 13 | 7 | 0 | 0 | 16 | 0 |
| Total no. of contacts | 587 | 1654 | 172 | 160 | 542 | 128 |
| Positive SARS-CoV-2 results from swabs of contacts | 4 staff contacts with detected SARS-CoV-2 PCR result1 unprotected, close*1 unprotected, transient†1 N95 mask, transient†1 surgical mask, transient† | 0 | 0 | |||
Close contacts: Contacts who are exposed <2 minutes and ≥ 15 minutes to a positive COVID-19 case (during unexpected exposures to SARS-CoV-2 cases whereby there was an exposure to a COVID-19 staff, patient, or visitor within the hospital premises) and not in a full set of PPE (N95 mask or equivalent, gown/apron, gloves, eye protection).
Transient contacts: those who had potential exposure to a COVID-19 case (e.g. were in the ward at the same time as the case), but did not fulfill the criteria for close contact.
Abbreviations: PCR = polymerase chain reaction; PPE = personal protective equipment.
As a result of these exposures, 2,573 staff contacts were traced (919 close and 1,654 transient). Among the close staff contacts, 160 had unprotected exposure to the index case, all of whom were immediately furloughed, with most receiving 14-day Quarantine Orders (QOs) from MOH; 172 close staff contacts who wore surgical masks during exposure to the case were furloughed and/or underwent SARS-CoV-2 testing; the remaining 2,241 staff contacts (587 close and 1,654 transient) who wore N95 masks and eye protection underwent various combinations of hospital measures, including enhanced surveillance swab regimes and surveillance of temperature and/or ARI symptoms. A QO is a legal order under the Infectious Diseases Act (IDA) requiring an individual who is suspected to be a carrier of an infectious disease or a contact of a confirmed case to be quarantined at a designated place. Orders end 14 days following the last exposure date to the case.
Likewise, 542 patients and 122 visitors who were close contacts were also traced. Among them, 198 patients and 38 visitors received QOs. Actions for the remaining patient and visitor contacts contacted directly by MOH's public health officers could not be ascertained in our study.
Among 2,573 staff contacts of COVID-19 cases, only 4 staff (Staff B, D, E, F) subsequently had detected SARS-CoV-2 results. Staff B had worked on the same shift in the same ward as the index staff (Staff A) but did not have close contact with that staff. Staff B (Staff A's transient contact) had undergone surveillance swabs on days 1, 4, 7, and 14 after exposure, of which the day-14 swab was detected and remained asymptomatic throughout the illness. Of interest, the other 3 staff contacts confirmed with COVID-19 (Staff D, E, and F) were epidemiologically linked to another index staff (Staff C). Staff D was a housemate of Staff C although they worked in different areas in the hospital, suggesting that transmission likely occurred outside of the hospital. Staff D had developed ARI symptoms the day after the RRT surveillance swab. The remaining 2 staff contacts (Staff E and F) worked in the same non-clinical area as Staff C. Both had transient unprotected contact with Staff C in the pantry. This departmental cluster was the only hospital cluster identified during the study period.
Of the 14 unexpected inpatient COVID-19 cases, only 1 case (Patient A) was infected in the hospital. Patient A's RRT swab was detected 44 days into the hospitalization, which surpassed the SARS-CoV-2 incubation period of 14 days. However, the source of infection was unknown, as SARS-CoV-2 was not detected in the swabs of staff (all who donned N95 masks and goggles) and close patient contacts. Nonetheless, during hospitalization, Patient A had 5 visitors, who could not be ruled out as potential sources of infection.
Discussion
Our findings provide confidence that the enhanced hospital measures implemented after the ward cluster were likely to have reduced nosocomial transmission risks despite widespread community transmission of the highly transmissible Delta variant. Among 2,531 staff contacts who had unexpected exposures to a COVID-19 case across the 193 incidents, only 4 were subsequently confirmed with COVID-19. For Staff B, a few factors suggest that acquisition from the index case was unlikely, such as, (i) transient and protected exposure to the index case (Staff A) and (ii) positive result only on day 14 post-exposure, whereas the mean incubation period of the Delta variant is reported to be under 4 days (Li et al., 2021). For our only hospital cluster, transmission was likely to have occurred in the pantry when the 2 staff contacts had unprotected exposures to the index staff in the pantry when the index staff was infectious. Within the hospital, the risk of spread in non-clinical areas (such as in office and rest areas) where staff may mingle (particularly, when masks are taken off during meals or drinks) are higher than in clinical areas, thus safe workplace measures play a crucial role (Wee et al., 2020). Staff are at a high risk of acquiring COVID-19 and Emerging Infectious Diseases (EIDs) during patient care, and countries have reported outbreaks occurring in healthcare settings (Abbas et al., 2021; Nguyen et al., 2020; Suwantarat and Apisarnthanarak, 2015). As staff also interface with the community, they may initiate or amplify outbreaks in hospital settings; thus, the protection of staff is a key priority (Asad et al., 2020). Contrasting our hospital cluster with other COVID-19 nosocomial outbreaks in Israel (Shitrit et al., 2021) and Canada (Susky et al., 2021) where surgical masks and American Society for Testing and Materials (ASTM) level 3 masks were used respectively, our enhanced measures, including upgraded PPE, surveillance, prompt detection and isolation of cases have been successful in reducing nosocomial transmission among staff.
During the study period, only 1 definitive nosocomial infection occurred among inpatients (Patient A), although investigations failed to identify the source of infection. Visitors may have played a role in the acquisition, as fully vaccinated visitors had been allowed in without requiring previous SARS-CoV-2 testing during the patient's probable incubation period. The case is consistent with other reported cryptogenic asymptomatic nosocomial transmissions of COVID-19 (Abbas et al., 2021). Active patient case-finding by way of patient RRT as well as testing visitors for SARS-CoV-2 may be advantageous as we transit toward living with COVID-19 and relaxing visitation policies.
Our study demonstrated that there was increased but still limited effectiveness of biweekly PCR staff RRT in detecting asymptomatic infection amid widespread community transmission of the Delta SARS-CoV-2 strain. Among the 11,200 staff who underwent RRT, 33 had a true detected result. Among the 33 true positives, 22 remained asymptomatic throughout the illness. The other 11 developed symptoms following the RRT swab and would have been identified by ARI surveillance regardless. Thus, RRT discovered 22 additional asymptomatic true positive cases. Unlike our previously published letter before the emergence of the Delta variant, RRT allowed for earlier detection and isolation of asymptomatic staff in our study (Chow et al., 2021). Nevertheless, the SARS-CoV-2 detection rate of staff RRT (0.2%) was considerably lower than that of active surveillance of staff with ARI symptoms (2.5%), and the numerous false positives resulted in unnecessary staff anxiety and furloughs. Routine asymptomatic surveillance has not been recommended as a primary infection prevention strategy to decrease COVID-19 transmission in healthcare facilities, and there is a possibility that the existing staff protection and surveillance measures may have played a role in the low detection rate of staff RRT in our study (Shenoy and Weber, 2021). The benefits of RRT for staff remain questionable and further studies are required (Tan et al., 2021).
As community transmission in Singapore surged, the number of COVID-19 cases detected among staff increased (Fig. 1). Staff should remain vigilant outside of the hospital in observing public health measures such as mask-wearing and physical distancing, especially during heightened community transmission of COVID-19. We also observed that ARI incidence among staff increased as community transmission of COVID-19 increased. Previous studies suggested that public health measures implemented to control COVID-19 could also have an inadvertent effect on the transmission of Streptococcus pneumoniae and Influenza (Chow et al., 2020b, Lim et al., 2020). By abiding by public health measures, staff may also protect themselves against ARI owing to other respiratory pathogens.
Although our measures were effective, they come at a cost. Significant resources were dedicated to supporting COVID-19 operations with numerous staff furloughed owing to contact tracing efforts. Quarantine and changes in working conditions to accommodate COVID-19 measures may affect the psychological well-being of staff (Digby et al., 2020; Fawaz and Samaha, 2020). Isolation of inpatient contacts has been associated with adverse effects on patient care, and cancellation or avoidance of elective appointments could also hinder timely access to healthcare (Abad et al., 2010; Kuhlen et al., 2020; Nair et al., 2020; Purssell et al., 2020). With a highly vaccinated population (>80%) and an even more highly vaccinated staff population (>90%), a balance needs to be struck between channeling healthcare resources toward managing COVID-19 and other competing priorities.
Our study had several limitations. During the study period, the infection control and safety management measures, as well as guidelines for the management of contacts, were ever-evolving, thus recommendations for a specific regime could not be made. Furthermore, as there was only 1 staff cluster observed, we were unable to compare the efficacy of certain measures, such as the adequacy of surgical versus N95 masks in protecting against COVID-19 acquisition in the hospital. In addition, our healthcare system had sufficient manpower and financial and infrastructural resources to perform extensive surveillance, testing, and quarantining of staff, although the same practices may not be feasible for resource-limited settings or if the hospital was overwhelmed with the management of COVID-19 cases.
In the era of the highly transmissible Delta variant, hospitals need to strengthen their defenses against COVID-19. Enhanced measures, including upgraded PPE for staff and patients, RRT for staff and patients, surveillance of staff with ARI, and aggressive testing and quarantining measures for contacts with potential COVID-19 exposure, may have reduced nosocomial transmission of COVID-19 despite widespread community transmission of the Delta variant.
Acknowledgments
Potential conflicts of interest
The authors report no conflicts of interest.
Financial support
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethics approval
The study was approved with a waiver of informed consent by the Domain Specific Review Board of National Healthcare Group, Singapore (DSRB - 2021/00891).
References
- Abad C, Fearday A, Safdar N. Adverse effects of isolation in hospitalised patients: a systematic review. Journal of Hospital Infection. 2010;76(2):97–102. doi: 10.1016/j.jhin.2010.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abbas M, Robalo Nunes T, Martischang R, Zingg W, Iten A, Pittet D, et al. Nosocomial transmission and outbreaks of coronavirus disease 2019: the need to protect both patients and healthcare workers. Antimicrobial Resistance & Infection Control. 2021;10(1):7. doi: 10.1186/s13756-020-00875-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asad H, Johnston C, Blyth I, Holborow A, Bone A, Porter L, et al. Health Care Workers and Patients as Trojan Horses: a COVID19 ward outbreak. Infection Prevention in Practice. 2020;2(3) doi: 10.1016/j.infpip.2020.100073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan E. Hospitals can allow some visitors to stay beyond 20 minutes if they take a COVID-19 test: MOH. Channel News Asia 2021.
- Chow A, Guo H, Kyaw WM, Li AL, Lim RHF, Ang B. Rostered routine testing for severe acute respiratory coronavirus virus 2 (SARS-CoV-2) infection among healthcare personnel—Is there a role in a tertiary-care hospital with enhanced infection prevention and control measures and robust sickness-surveillance systems? Infection Control & Hospital Epidemiology. 2021:1–2. doi: 10.1017/ice.2021.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow A, Htun HL, Kyaw WM, Ang H, Tan G, Tan HN, et al. Atypical COVID-19: Preventing transmission from unexpected cases. Infect Control Hosp Epidemiol. 2020:1–3. doi: 10.1017/ice.2020.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow A, Hein AA, Kyaw WM. Unintended Consequence: Influenza plunges with public health response to COVID-19 in Singapore. The Journal of infection. 2020;81(2):e68–ee9. doi: 10.1016/j.jinf.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Digby R, Winton-Brown T, Finlayson F, Dobson H, Bucknall T. Hospital staff well-being during the first wave of COVID-19: Staff perspectives. International Journal of Mental Health Nursing. 2020;30 doi: 10.1111/inm.12804. [DOI] [PubMed] [Google Scholar]
- Fawaz M, Samaha A. The psychosocial effects of being quarantined following exposure to COVID-19: A qualitative study of Lebanese health care workers. International Journal of Social Psychiatry. 2020;66(6):560–565. doi: 10.1177/0020764020932202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Htun HL, Lim DW, Kyaw WM, Loh WJ, Lee LT, Ang B, et al. Responding to the COVID-19 Outbreak in Singapore: Staff Protection and Staff Temperature and Sickness Surveillance Systems. Clin Infect Dis. 2020;71(8):1947–1952. doi: 10.1093/cid/ciaa468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Kuhlen R, Schmithausen D, Winklmair C, Schick J, Scriba P. The Effects of the COVID-19 Pandemic and Lockdown on Routine Hospital Care for Other Illnesses. Dtsch Arztebl Int. 2020;117(27-28):488–489. doi: 10.3238/arztebl.2020.0488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li B, Deng A, Li K, Hu Y, Li Z, Xiong Q, et al. Viral infection and transmission in a large well-traced outbreak caused by the Delta SARS-CoV-2 variant. medRxiv. 2021 doi: 10.1038/s41467-022-28089-y. 2021.07.07.21260122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim RH, Chow A, Ho HJ. Decline in pneumococcal disease incidence in the time of COVID-19 in Singapore. J Infect. 2020;81(6):e19–e21. doi: 10.1016/j.jinf.2020.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim W-Y, Tan GSE, Htun HL, Phua HP, Kyaw WM, Guo H, et al. The first nosocomial cluster of COVID-19 due to the Delta variant in a major acute-care hospital in Singapore – investigations and outbreak response. Journal of Hospital Infection. [DOI] [PMC free article] [PubMed]
- Ministry of Health S. APPROACH TO TRANSIT TO THE ENDEMIC STAGE. 2021a.
- Ministry of Health S. MINISTERIAL STATEMENT BY MR ONG YE KUNG, MINISTER FOR HEALTH ON DEVELOPMENT OF THE COVID-19 PANDEMIC, 26 JULY 2021. 2021b.
- Ministry of Health S. TIGHTENED MEASURES TO REDUCE HOSPITAL COVID-19 TRANSMISSION AND PRESERVE HOSPITAL CAPACITY. 2021c.
- Nair AG, Gandhi RA, Natarajan S. Effect of COVID-19 related lockdown on ophthalmic practice and patient care in India: Results of a survey. Indian Journal of Ophthalmology. 2020;68(5) doi: 10.4103/ijo.IJO_797_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo C-G, Ma W, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. The Lancet Public Health. 2020;5(9):e475–ee83. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purssell E, Gould D, Chudleigh J. Impact of isolation on hospitalised patients who are infectious: systematic review with meta-analysis. BMJ Open. 2020;10(2) doi: 10.1136/bmjopen-2019-030371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shenoy ES, Weber DJ. Routine surveillance of asymptomatic healthcare personnel for severe acute respiratory coronavirus virus 2 (SARS-CoV-2): Not a prevention strategy. Infection control and hospital epidemiology. 2021;42(5):592–597. doi: 10.1017/ice.2020.1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shitrit P, Zuckerman NS, Mor O, Gottesman B-S, Chowers M. Nosocomial outbreak caused by the SARS-CoV-2 Delta variant in a highly vaccinated population, Israel, July 2021. Eurosurveillance. 2021;26(39) doi: 10.2807/1560-7917.ES.2021.26.39.2100822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Susky EK, Hota S, Armstrong IE, Mazzulli T, Kestenberg S, Casaubon LK, et al. Hospital outbreak of the severe acute respiratory coronavirus virus 2 (SARS-CoV-2) delta variant in partially and fully vaccinated patients and healthcare workers in Toronto. Canada. Infection Control & Hospital Epidemiology. 2021:1–4. doi: 10.1017/ice.2021.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suwantarat N, Apisarnthanarak A. Risks to healthcare workers with emerging diseases: lessons from MERS-CoV, Ebola, SARS, and avian flu. Curr Opin Infect Dis. 2015;28(4):349–361. doi: 10.1097/QCO.0000000000000183. [DOI] [PubMed] [Google Scholar]
- Tan SY, How CH, Poon BH, Tan TY, Siau C. Rostered Routine Testing – A Necessary Evil? Open Forum Infectious Diseases. 2021 doi: 10.1093/ofid/ofab549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teo J. TTSH Covid-19 cluster sparked by new variant that originated in India. The Straits Times. 2021 [Google Scholar]
- Tham D. Hospital visits to resume; visitors need to be fully vaccinated or show negative COVID-19 test result: MOH. Channel News Asia 2021.
- Wee LE, Sim XYJ, Conceicao EP, Aung MK, Goh JQ, Yeo DWT, et al. Containment of COVID-19 cases among healthcare workers: The role of surveillance, early detection, and outbreak management. Infection Control & Hospital Epidemiology. 2020;41(7):765–771. doi: 10.1017/ice.2020.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang M, Xiao J, Deng A, Zhang Y, Zhuang Y, Hu T, et al. Transmission Dynamics of an Outbreak of the COVID-19 Delta Variant B.1.617.2 - Guangdong Province, China, May-June 2021. China CDC Wkly. 2021;3(27):584–586. doi: 10.46234/ccdcw2021.148. [DOI] [PMC free article] [PubMed] [Google Scholar]