Abstract
Background:
Previous research has established an association between pandemic fears and the development of obsessive-compulsive symptoms mainly in the general population.
Aim:
To explore whether COVID-19 pandemic fears are associated with obsessive-compulsive symptoms and vice versa in adolescents with preexisting mental and behavioural disorders.
Methods:
A questionnaire-based cross-sectional study among adolescents with pre-existing mental disorders. The extent of worrying related to the COVID-19 pandemic was measured using the COVID-19 inventory whereas obsessive-compulsive symptoms were assessed using the obsessive-compulsive inventory-revised (OCI-R). Pearson correlation coefficient (r) was used to explore the relationship between COVID-19 pandemic fears and the development of obsessive-compulsive symptoms.
Results:
A total of 57 patients out of 63 participants (90.4%) had a COVID-19 inventory score of 12 or higher suggesting that a vast majority of young people with mental disorders had significant pandemic-related worries. Out of these 57 patients, over half (31) had an OCI-R modified score of 17 or higher indicating significant obsessive-compulsive symptoms. A positive correlation was found between the means of the two scores. This relationship was statistically significant – {r = 0.405, Sig. (two-tailed) = 0.001}.
Conclusion:
Adolescents with mental disorders can exhibit significant pandemic fears and this is likely to be associated with obsessive-compulsive symptoms.
Keywords: COVID-19, pandemic fears, adolescents, mental disorder, obsessive-compulsive symptoms
Introduction
The highly contagious, novel Coronavirus (SARS-CoV-2) disease, officially designated as COVID-19 by the World Health Organization (WHO), was first identified in Wuhan, China in December 2019. It caused outbreaks of acute infectious pneumonia in China initially before spreading at an extraordinarily fast pace to different parts of the world, reaching the level of a global pandemic by March 2020. In order to prevent or slow down the transmission of COVID-19, various public health measures have been implemented including frequent handwashing, use of face masks, social distancing, isolation and quarantining of infected individuals and tracking and testing of potential contacts (Adhikari et al., 2020).
The widespread outbreak of COVID-19 has been associated with psychological burden and manifestations of mental illness, due to various factors related to the pandemic, such as the worry of being infected, the unpredictability of future events, misinformation to the public through inconsistent news reports and restrictions on travel (Bao et al., 2020). All these factors have contributed to the development of pandemic-specific fears of varied severity among individuals. Fear is considered a normal adaptive response to threat-related stimuli which involves either coping with the threat or avoiding it. However, a persistent and/or disproportionate level of fear may be harmful and has the potential to contribute to development of various mental disorders (Garcia, 2017; Shin & Liberzon, 2010).
Pandemic fears can increase levels of anxiety and stress in the healthy population and worsen symptoms among individuals with pre-existing mental disorders (Shigemura et al., 2020). It was demonstrated during the Severe Acute Respiratory Syndrome (SARS) pandemic, which had primary outbreaks in Hong Kong and Toronto, that there was high anxiety regarding the risk of illness in the general population in Hong Kong (Mak et al., 2009) and among attendees at a conference in Toronto (Stinson et al., 2004). Another study has previously concluded that widely publicised pandemics are associated with an increased level of anxiety and potential worsening of psychiatric vulnerabilities (Lancee et al., 2008).
Obsessive-Compulsive Disorder (OCD) is particularly relevant to Pandemic-related worrying and is most significant in this context (Banerjee, 2020). OCD is characterized by the presence of obsessions and/or compulsions. Obsessions are recurrent and persistent thoughts, urges or images that are experienced as intrusive and unwanted, whereas Compulsions are repetitive behaviours or mental acts that an individual feel driven to perform in response to an obsession or according to rules that must be applied rigidly (American Psychiatric Association, 2013). Fears of contamination and washing compulsions are among the four major symptom dimensions of OCD (Bloch et al., 2008). In previous outbreaks such as SARS and H1N1 influenza, obsessive-compulsive beliefs and symptoms were exacerbated and predicted fears related to the infection (Brand et al., 2013; Mak et al., 2009). This association can be explained by the striking similarity between fears of contamination and compulsive handwashing found in OCD, as one of its major symptom dimensions, and fears related to Pandemics in which the risk of acquiring infection can be reduced specifically by performing similar repetitive and ritualistic safety behaviours. The stress on the importance of adhering to strict hygiene measures (regular handwashing, social distancing, etc.) can, therefore, trigger significant distress among individuals with OCD.
The prevalence of Obsessive-compulsive disorder among children and adolescents is in the range of 1% to 3%, reaching up to 4% in some populations (Flament et al., 1988; Fontenelle et al., 2006; Krebs and Heyman., 2015; Valleni-Basile et al., 1994), a rate similar to that observed in adults. Its lifetime prevalence ranges between 2% and 3% by late adolescence (Zohar, 1999). Research suggests that almost half of all diagnosed individuals have their onset in childhood and adolescence (Janowitz et al., 2009; Pauls et al., 1995).
It is therefore of utmost importance to acknowledge the extent of the impact of a pandemic on the lives of adolescents in general and their mental health in particular. Closure of schools or limited access to typical classroom learning, cessation or reduction in interaction with friends and cancelation of outdoor activities have all had a significant impact on the lives of children and young people. These among other factors have put children and adolescents in circumstances where distress and mental health problems could rise (Fegert et al., 2020).
The main aim of this study was to explore whether adolescents with pre-existing mental disorders exhibited high levels of pandemic fears and if so whether individuals with heightened pandemic fears also reported symptoms of obsessive-compulsive disorder and vice versa. The investigators were also interested to know whether certain variables (gender, diagnosis and type of intervention) were more likely to be associated with significant pandemic fears and obsessive-compulsive symptoms.
Methods
Design and participants
To our knowledge, no previous study has aimed to explore the extent of pandemic fears and its association with obsessive-compulsive symptoms among young people with established mental or behavioural disorders. Therefore, this study was designed as an exploratory study (cross sectional, web-based survey) and thus looking at the study design and exploratory objectives we didn’t set and formulate any prior statistical hypothesis and hence we didn’t perform any formal sample size calculation into this study.
The study was conducted in the Community Child and Adolescent mental health service (CAMHS) at Hamad Medical Corporation in the state of Qatar. It is the only community-based service in the country providing support to children and young people below 18 years of age with mental and behavioural disorders of moderate to severe intensity. The service receives approximately 1,000 referrals annually which, upon acceptance, are allocated to a clinician of the multidisciplinary team (psychiatry, psychology, occupational therapy, speech and language therapy, dietetics, social services) depending on the needs of the individual and family for further management.
All 147 young people aged 14 to 18 years, that is, 14 or older but not yet reached their 18th birthday, who were seen in the medical psychiatric outpatient clinics at least on one occasion between July 1, 2019 and December 31, 2019, were enroled in the study. Twenty-five individuals refused to participate in the study. The remaining 122 were assessed for eligibility. Young People (a) with an intellectual disability of severity greater than mild, (b) with an acute clinical presentation of a severe mental disorder affecting their cognitive ability to the extent that they could not participate in the study and (c) who were not fluent in both English and Arabic were excluded from the study. Fifty-nine individuals had to be excluded after applying the exclusion criteria reducing the final sample size to 63.
Ethical considerations and data collection
The study was reviewed and approved by the Medical Research Center (MRC-05-037) and the Institutional Review Board (IRB) at Hamad Medical Corporation, Qatar. The required data was collected by a specialist Child and Adolescent mental health nurse. Phone calls were made to all individuals and their Parents included in the sample to invite them to the study. All information relevant to the study including its purpose, impact on clinical care and confidentiality safeguards was provided using an invitation form with a standard script developed specifically for the study, in both English and Arabic languages.
Consent of the participating individuals and their Parents’ was obtained verbally over the phone and recorded on the respective invitation forms. The link for the online questionnaires was sent to participants upon their acceptance to participate in the study. Responses were submitted online. All participating individuals and their Parents further reconfirmed their willingness to participate in the study by selecting ‘Yes’ to the first two questions related to the consent of the participant and the Parent on the online questionnaire before proceeding further.
Measures
The following measures were used in this study:
COVID-19 inventory
Adapted from the swine flu inventory (Wheaton et al., 2012) which is a pool of 10 items collaboratively developed by a group of clinicians and researchers with experience in evaluating and treating individuals with anxiety disorders and somatisation. The Swine Flu Inventory is an 11-item, self-report, inventory examining attitudes and behaviours associated with fears of Swine Flu and measures taken to prevent getting Swine Flu. It has been used previously in research studies and has demonstrated acceptable reliability (Wheaton et al., 2012).
The only modification made to the Swine Flu inventory for this study was the removal of one item about worrying related to the disease becoming a pandemic. This study was conducted when COVID-19 had already been declared a pandemic. The remaining nine items on the Swine Flu inventory were retained in their original form except that the term ‘swine flu’ was replaced with ‘COVID-19’. As in the Swine Flu inventory, items were designed to assess participants’ concerns about the spread of COVID-19, perceived likelihood of contracting the infection, perceived severity of infection, avoidance of certain places and people, use of safety behaviours and degree of exposure to information about the Coronavirus (SARS-CoV-2) virus. Respondents rated their responses to nine items on a five-point scale ranging from zero (very little) to four (very much). The scores on this form could range from 0 (minimum) to 36 (maximum).
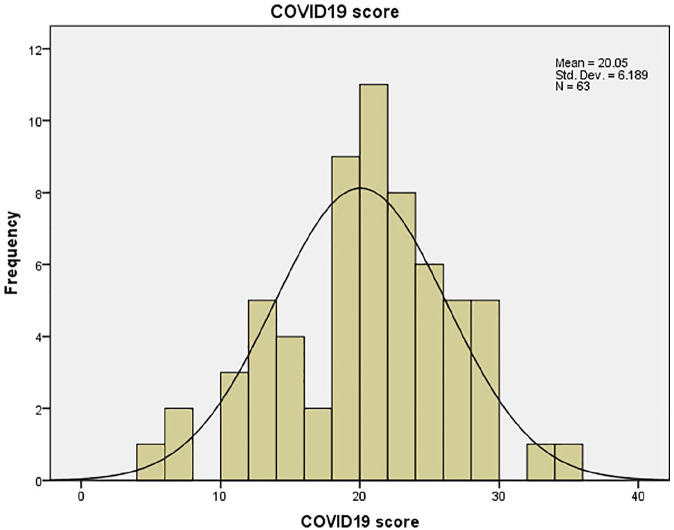
A cut-off score of 12 was considered clinically significant for pandemic fear. This was an arbitrary cut-off score chosen in view of clinical significance and used mainly to descriptively summarise COVID-19 score distributions as shown in the histogram (Figure 3). There were no statistical associations/comparisons made between the cut-off score and other variables.
Figure 3.
COVID-19 inventory scores.
Obsessive-compulsive inventory-revised (OCI-R)
The OCI-R (Foa et al., 2002) is an 18-item, self-report inventory developed from the earlier 42-item Obsessive-Compulsive Inventory (Foa et al., 1998). Each item describes a symptom commonly associated with obsessive-compulsive disorder. The measure utilises a five-point scale, with participants rating from zero to four the degree to which each item has caused distress in the last month. Higher scores indicate greater levels of distress due to symptoms. The total score, ranging from 0 to 72, is then divided into subscales to reflect the severity of symptoms in the following six dimensions of OCD: washing, checking, ordering, obsessing, hoarding and neutralizing. The OCI-R demonstrates good internal consistency and test-retest reliability, along with strong convergent validity (Abramowitz & Deacon, 2006).
Both the above instruments were forward-translated into Arabic and further back-translated into English by experienced Psychiatrists in the local Child and Adolescent mental health services with excellent proficiency in both English and Arabic languages. It was ensured that the original and the translated versions achieved conceptual, cultural and linguistic equivalence. The translated questionnaires were piloted on the first five respondents. Their understanding of each item on the questionnaire and its response was explored to ensure the translated items retained the same meaning as the original items.
Statistical analysis
Descriptive statistics were used to summarise and determine the sample characteristics and distribution of participants’ data. The normally distributed data and results were reported with mean and standard deviation (SD); the remaining results reported with median and inter-quartile range (IQR). Statistical graphs such as histogram and scatter diagram were constructed to depict the data distribution for quantitative variables and assess linear relationship between COVID-19 and OCI-modified scores. Categorical data were summarised using frequencies and proportions.
Mean scores measured for both inventories COVID-19 and OCI-modified scores between the two independent groups (gender: male and female) and across various diagnosis and intervention groups were compared using unpaired t-test and one-way analysis of variance (ANOVA) or non-parametric Kruskal–Wallis test where appropriate. Pearson correlation coefficient was used to examine and assess correlation between COVID-19 inventory scores and OCI-modified scores. All p values presented were two-tailed, and p values <.05 were considered as statistically significant. All Statistical analyses were done using statistical packages SPSS version 27 (SPSS Inc., Chicago, IL).
Results
Demographic and descriptive characteristics
All 63 participants (35 males and 28 females) completed both the questionnaires. Details related to the two independent variables, diagnosis and intervention, are provided in Table 1:
Table 1.
Diagnosis and intervention.
| Frequency | Percentage | |
|---|---|---|
| Diagnosis | ||
| OCD | 8 | 12.7 |
| Neurodevelopmental, disruptive, impulse control and conduct disorders | 27 | 42.9 |
| Mood and anxiety disorders | 23 | 36.5 |
| Others | 5 | 7.9 |
| Total | 63 | 100.0 |
| Intervention | ||
| Medication alone | 18 | 28.6 |
| Psychotherapy alone | 11 | 17.5 |
| Both | 30 | 47.6 |
| None | 4 | 6.3 |
| Total | 63 | 100.0 |
COVID-19 inventory and OCI-R scores
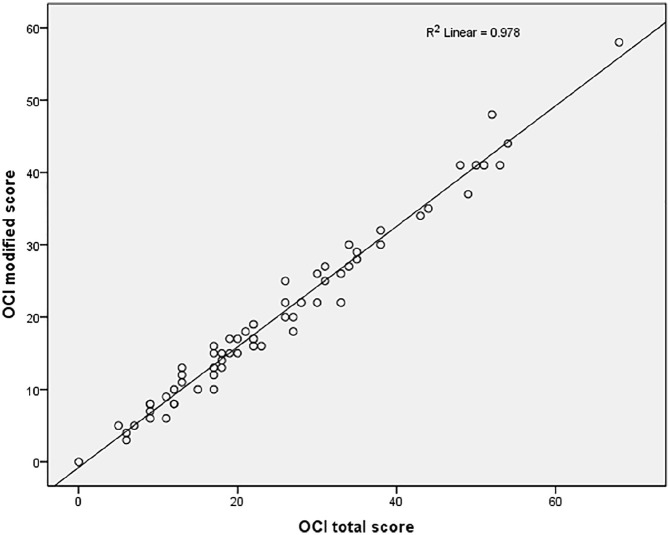
Table 2 presents the scores of all 63 participants on both the questionnaires (COVID-19 and OCI-R). We had to make an adjustment to the OCI-R scoring by ignoring the scores of its three items (5, 11 and17) as behaviours described by these items were related to preventive measures mandatory for reducing the spread of infection and were therefore considered normal in the COVID-19 pandemic. This adjusted score, termed as ‘OCI-R modified score’ and included in the last column in Table 2, therefore, did not include the scores for the three mentioned items. The validity of OCI-R modified version was found to be optimal, having significant correlation (Figure 1) with the original OCI-R version (r = 0.989 and R2 linear = 0.978). Whilst, we retained the scores of OCI-R, we relied mainly on the OCI-R modified scores to establish the presence of obsessive-compulsive symptoms.
Table 2.
COVID-19 inventory, OCI-R and OCI-R modified scores.
| COVID-19 score | OCI-R score | OCI modified score | |
|---|---|---|---|
| N | |||
| Valid | 63 | 63 | 63 |
| Missing | 0 | 0 | 0 |
| Mean | 20.05 | 24.97 | 20.03 |
| Median | 21.00 | 22.00 | 17.00 |
| Std. deviation | 6.189 | 14.716 | 12.399 |
| Range | 30 | 68 | 58 |
| Minimum | 5 | 0 | 0 |
| Maximum | 35 | 68 | 58 |
Figure 1.
Correlation between OCI-R and OCI-R-modified scores.
Correlation between COVID-19 inventory and OCI-R modified scores
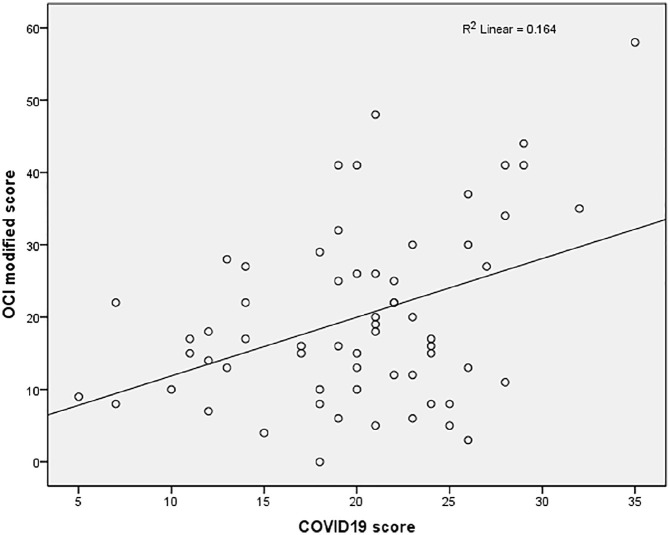
A positive correlation was found between the means of the two scores. This relationship was statistically significant – {r = 0.405, Sig. (two-tailed) = 0.001} (Figure 2). The clinical significance of this correlation can be interpreted as moderate (Table 3).
Figure 2.
Correlation between COVID-19 inventory and OCI-R-modified scores.
Table 3.
Correlation between COVID-19 inventory and OCI-R-modified scores.
| Age | COVID-19 score | OCI total score | OCI modified score | |
|---|---|---|---|---|
| Age | ||||
| Pearson correlation | 1 | 0.036 | −0.056 | −0.018 |
| Sig. (two-tailed) | 0.778 | 0.660 | 0.890 | |
| N | 63 | 63 | 63 | 63 |
| COVID19 score | ||||
| Pearson correlation | 0.036 | 1 | 0.386** | 0.405** |
| Sig. (two-tailed) | 0.778 | 0.002 | 0.001 | |
| N | 63 | 63 | 63 | 63 |
| OCI total score | ||||
| Pearson correlation | −0.056 | 0.386** | 1 | 0.989** |
| Sig. (two-tailed) | 0.660 | 0.002 | 0.000 | |
| N | 63 | 63 | 63 | 63 |
| OCI modified score | ||||
| Pearson correlation | −0.018 | 0.405** | 0.989** | 1 |
| Sig. (two-tailed) | 0.890 | 0.001 | 0.000 | |
| N | 63 | 63 | 63 | 63 |
Correlation is significant at the 0.01 level (2-tailed).
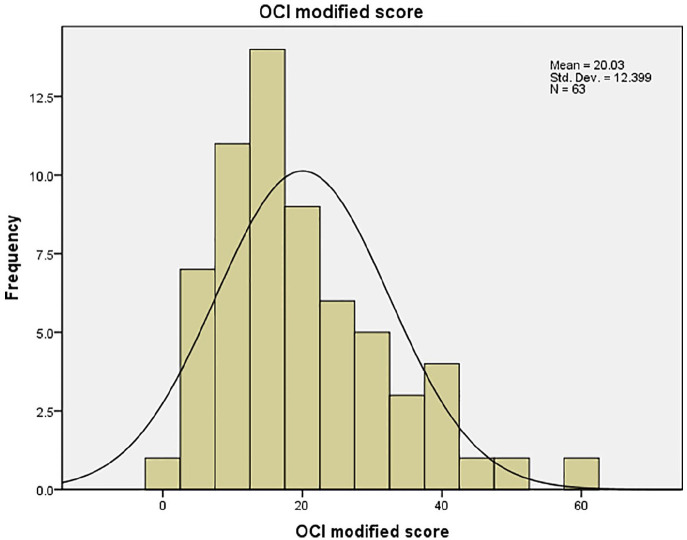
A total of 57 patients (90.4%) had a COVID-19 inventory score of 12 or higher suggesting that a vast majority of young people with mental disorders had significant pandemic-related worries (Figure 3). Out of these 57 patients, over half (31) had an OCI-R modified score of 17 or higher indicating that pandemic-related worrying may predict obsessive-compulsive symptoms to a certain extent (Figure 4). However, when the data of the COVID-19 scores of these 57 patients was broken down into mild (12–19), moderate (20–27) and severe (28–36) categories, it was noted that 45% in the mild category, 53.3% in the moderate category whereas 85.7% in the severe category on the COVID-19 inventory had significant obsessive-compulsive symptoms. This finding suggests that the likelihood of experiencing obsessive-compulsive symptoms becomes greater with increase in the severity of pandemic fears.
Figure 4.
OCI-R-modified scores.
We also looked at the possibility of an inverse relationship, that is, whether significant obsessive-compulsive symptoms could predict increased pandemic-related worrying. We found that 33/63 (52.3%) participants met or exceeded the OCI-R-modified cut-off score of 17. A striking finding was that 93.9% of these patients with significant obsessive-compulsive symptoms also achieved a score of 12 or higher on the COVID-19 inventory consolidating the hypothesis that obsessive-compulsive beliefs and symptoms predict a higher level of pandemic-related worrying.
Furthermore, a total of eight patients among the 63 who participated in the study had a prior diagnosis of Obsessive-compulsive disorder out of who seven patients (87.5%) rated themselves above the OCI-R-modified cut off score. Interestingly, all but one patient out of the eight with established obsessive-compulsive disorder also rated themselves as 12 or higher on the COVID-19 inventory, further consolidating the probable association between Obsessive-compulsive symptoms and pandemic fears.
Relationship between Diagnosis and COVID-19/OCI-R modified scores
We found small, statistically insignificant differences in the mean COVID-19 and OCI-R-modified scores of the different diagnostic groups (Table 4).
Table 4.
Relationship between diagnosis, intervention, gender and COVID-19 inventory/OCI-R modified mean scores.
| COVID-19 inventory mean scores with SD | OCI-R modified mean scores with SD | |
|---|---|---|
| Diagnosis | ||
| OCD | 16.5 (±6.118) | 20.75 (±7.106) |
| Neurodevelopmental, disruptive, impulse control and conduct disorders | 20.78 (±6.254) | 18.30 (±13.632) |
| Mood and anxiety disorders | 20.65 (±5.982) | 21.83 (±12.967) |
| Others | 19.00 (±4.743) | 20.00 (±11.045) |
| Sig. | 0.345 | 0.800 |
| Intervention | ||
| Medication alone | 20.94 (±5.916) | 23.00 (±14.653) |
| Psychotherapy alone | 18.82 (±6.705) | 18.27 (±11.976) |
| Both | 20.03 (±6.305) | 18.17 (±11.308) |
| None | 19.50 (±6.952) | 25.50 (±10.376) |
| Sig. | 0.846 | 0.447 |
| Gender | ||
| Male (N = 35) | 19.60 (±6.436) | 19.97 (±13.407) |
| Female (N = 28) | 20.61 (±5.934) | 20.11 (±11.256) |
| Sig. | 0.894 | 0.735 |
We were interested to know whether mental and behavioural disorders other than obsessive-compulsive disorder may also have a role in predicting pandemic fears. We found that the mean COVID-19 inventory score of patients from each diagnostic group (OCD, Neurodevelopmental disorders, Mood and anxiety disorders and others) exceeded the cut-off score, with the mean score of the OCD group being the lowest. Similarly, the mean OCI-R-modified scores from all groups exceeded the cut-off score with the ‘Mood and anxiety disorders’ group returning a higher mean score even than the OCD group. We can therefore argue that patients with mental and behavioural disorders other than OCD may also report significant obsessive-compulsive symptoms during a pandemic and can exhibit levels of pandemic-related worrying that are even higher than patients with obsessive-compulsive disorder.
Relationship between Intervention and COVID-19/OCI-R modified scores
Although we found small, statistically insignificant differences in the mean COVID-19 and OCI-R-modified scores for different clinical intervention groups (Table 4), these means scores were above the cut-off for patients across the different intervention groups and even where there was no formal intervention of any type made. No one type of treatment was found to be significantly superior than the other in reducing pandemic-related worrying or obsessive-compulsive beliefs and symptoms.
It was interesting to note though that patients on combined treatment, that is, medication (irrespective of the type) and psychological intervention returned the lowest mean OCI-R modified score, however, this finding was not seen in the mean COVID-19 scores where psychological treatment alone fared the best among different types of interventions by returning the lowest mean score.
Gender differences
There were no significant differences found between males and females in the mean scores on both the inventories (Table 4).
Discussion
The COVID-19 pandemic has demonstrated its negative impact on mental health of various population groups, including the youth (World Health Organization, 2020). Worries related to health are quite common in the general population and are believed to lie on a spectrum (Salkovskis & Warwick, 2001), however, such worrying is considered pathological if it lies more on the top end of this spectrum. There is evidence that health-related worrying and associated behaviour are common in adolescents with one study reporting rates as high as 15.7% among a sample of participants aged 14 to 19 years (Sirri et al., 2015). Health-related worrying has the tendency to impact the functioning of children and adolescents significantly and has been found to be associated with mental disorders (Rask et al., 2016). Furthermore, the management of children and young people is associated with significant healthcare costs (Rimvall et al., 2021).
It is therefore particularly crucial to identify young people with established mental health conditions who may have significantly high levels of pandemic fears and health worries with a view to providing them an enhanced level of care and support. Our study mainly explored the possibility of a relationship between COVID-19-related fears and the emergence or maintenance of OCD symptoms among adolescents with a range of pre-existing mental health diagnoses including obsessive-compulsive disorder.
We have been able to establish that the rates of significant pandemic-related worrying in young people with mental disorders are alarmingly high (90.4%) suggesting the need of enhanced care for this specific group of population. More importantly, the rates were high across the different diagnostic groups indicating that such fears can be heightened in not just young people with obsessive-compulsive disorder but those with other mental disorders too including mood, anxiety and neurodevelopmental disorders. Previous research has concluded that effective control of ruminations can potentially reduce the onset or maintenance of anxiety and depression (Cook & Watkins, 2016) and may also reduce the severity of psychotic and bipolar disorders (Vallarino et al., 2015).
Our study further consolidated the hypothesis established in previous studies that increased pandemic fears can predict obsessive-compulsive symptoms. We found that the proportion of patients with clinically significant obsessive-compulsive symptoms increased with an increase in the scores on the COVID-19 inventory. This highlights the importance of Child and Adolescent mental health services to screen patients for obsessive-compulsive symptoms during pandemics to ensure any emergence of such co-morbid symptoms is not missed and managed effectively to prevent exacerbation in the symptoms of the primary condition and/or development of a full blown co-morbid condition, for example, Illness anxiety disorder.
Although the role of pandemic fears in the development of obsessive-compulsive symptoms is well-established, its effect on young people with pre-existing OCD and already receiving treatment is unclear. We found that a vast majority of these patients continued to rate their obsessive-compulsive symptoms high despite receiving different kind of interventions from the treating Child and Adolescent mental health team. We also noted that all eight patients with OCD except one had significantly high scores on the COIVD-19 inventory too. One possible explanation for the maintenance of OCD symptoms in this group could be the excessive worrying related to the pandemic (health anxiety).
We can also conclude through the findings of our study that no particular intervention, whether pharmacological/psychological on their own or combined, was clearly superior as none of them could be significantly associated with either low scores on the COVID-19 inventory (pandemic fears) or on OCI-R-modified (obsessive-compulsive symptoms). Gender was also not found to be protective for pandemic worrying or obsessive-compulsive symptoms.
We have demonstrated through our study that young people with pre-existing mental health problems can be negatively affected by the COVID-19 pandemic and are predisposed to developing new symptoms and maintenance of existing illnesses despite receiving appropriate interventions. It is therefore pertinent that Child and Adolescent mental health services continue providing their patients the required care during times of social restrictions and partial or complete lockdowns. As patients may have difficulties in accessing health care services due to pandemic-related restrictions to reduce spread of COVID-19, it is crucial to consider alternative strategies such as access to a mental health crisis phone-line and use of telepsychiatry and online therapies (Abramowitz et al., 2018; Ćosić, et al., 2020).
The findings of this study can have crucial implications on formulating effective healthcare strategies and can be used in the generation of hypotheses for future research studies.
Limitations and future direction
Some limitations in our study should be acknowledged. The participants in our study were young people with pre-existing mental health challenges before the pandemic, therefore our results cannot be generalised to include healthy population. Moreover, it would have been helpful to consolidate the significance of the COVID-19 inventory cut-off score by using it in a comparable non-clinical sample. While we were able to show a relationship between COVID-19 pandemic fears and OCD symptoms, it is difficult to draw a conclusion about any causal relationship due to the cross-sectional design of our study. Moreover, the conclusion that no intervention was particularly superior could have been influenced by the cross-sectional design of the study, not providing the investigators enough time to track progress of patients over a period of time that is considered long enough for certain interventions to produce desired results. A longitudinal study may therefore be helpful to ascertain the comparison of different interventions.
A future study involving collection of data prior to the participants receiving interventions could also prove helpful. This would allow for a comparison being drawn between the severity of pandemic fears and obsessive-compulsive symptoms before and after the participants receiving necessary therapeutic interventions. A reduction in the reported severity of symptoms following interventions, a likely probability, can emphasize further the need of providing additional support to this vulnerable population (children and adolescents) during the pandemic. Similarly, future studies could compare the severity of obsessive-compulsive symptoms in patients with a previous diagnosis of OCD during the pandemic with its severity prior to the onset of the pandemic to establish if there is any deterioration in symptoms despite clinical interventions.
Research focusing on the efficacy of delivering online therapies to patients with OCD during the pandemic period and drawing a comparison with patients who do not receive such an intervention can prove to be very useful. It could determine the nature of support Child and Adolescent mental health services need to provide to meet the pandemic-specific needs of patients with mental disorders. Another interesting topic of future research could be conducting a longitudinal study to explore whether the psychological implications of a pandemic like COVID-19, particularly on young people with OCD, persist even after the pandemic is long over or subside soon after return to a pandemic-free life.
Acknowledgements
We would like to thank Mr. Prem Chandra, for his support with statistical analysis and compilation of results and the Medical Research Centre, Hamad Medical Corporation, for their input. The guidance received from our colleague, Dr. Saleem al Nuaimi (Consultant Child and Adolescent Psychiatrist and CAMHS Research Lead), proved very helpful. We are also grateful to all the young people and their Parents for their participation.
Author biographies
Yasser Saeed Khan is a consultant child and adolescent psychiatrist and the Medical Lead for the Child and Adolescent Mental Health Service, Hamad Medical Corporation, Doha, Qatar.
Muayad Jouda is a clinical fellow in Child and Adolescent Psychiatry at the Child and Adolescent Mental Health Service, Hamad Medical Corporation, Doha, Qatar.
Yahia Albobali is a clinical fellow in Child and Adolescent Psychiatry at the Child and Adolescent Mental Health Service, Hamad Medical Corporation, Doha, Qatar.
Manal Osman Abouelseoud is an associate consultant psychiatrist at the Child and Adolescent Mental Health Service, Hamad Medical Corporation, Doha, Qatar.
Aouatef Souid is a staff nurse at the Child and Adolescent Mental Health Service, Hamad Medical Corporation, Doha, Qatar.
May Jasem AlMeraisi is a clinical psychologist and the Clinical Director for the Child and Adolescent Mental Health Service, Hamad Medical Corporation, Doha, Qatar.
Majid Alabdulla is a senior consultant psychiatrist and chairman of Department of Psychiatry and Mental Health Services, Hamad Medial Corporation, Doha, Qatar.
Footnotes
Author’s Note: Majid Alabdulla is also affiliated with College of Medicine, Qatar University.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical information: Ethical approval was granted by the Institutional Review Board (IRB) and Medical Research Centre (MRC), Hamad Medical Corporation with the approval number MRC-05-037.
ORCID iDs: Yasser Saeed Khan  https://orcid.org/0000-0001-6575-5648
https://orcid.org/0000-0001-6575-5648
Muayad Jouda  https://orcid.org/0000-0002-7308-7624
https://orcid.org/0000-0002-7308-7624
References
- Abramowitz J. S., Deacon B. J. (2006). Psychometric properties and construct validity of the obsessive–compulsive inventory—revised: Replication and extension with a clinical sample. Journal of Anxiety Disorders, 20(8), 1016–1035. 10.1016/j.janxdis.2006.03.001 [DOI] [PubMed] [Google Scholar]
- Abramowitz J. S., Blakey S. M., Reuman L., Buchholz J. L. (2018). New directions in the cognitive-behavioral treatment of OCD: Theory, research, and practice. Behavior Therapy, 49(3), 311–322. 10.1016/j.beth.2017.09.002 [DOI] [PubMed] [Google Scholar]
- Adhikari S. P., Meng S., Wu Y. J., Mao Y. P., Ye R. X., Wang Q. Z., Sun C., Sylvia S., Rozelle S., Raat H., Zhou H. (2020). Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of corona virus disease (COVID-19) during the early outbreak period: A scoping review. Infectious Diseases of Poverty, 9(1), 29. 10.1186/s40249-020-00646-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). [Google Scholar]
- Banerjee D. D. (2020). The other side of COVID-19: Impact on obsessive compulsive disorder (OCD) and hoarding. Psychiatry Research, 288, 112966. 10.1016/j.psychres.2020.112966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao Y., Sun Y., Meng S., Shi J., Lu L. (2020). 2019-nCoV epidemic: Address mental health care to empower society. The Lancet, 395(10224), e37–e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloch M. H., Landeros-Weisenberger A., Rosario M. C., Pittenger C., Leckman J. F. (2008). Meta-analysis of the symptom structure of obsessive-compulsive disorder. The American Journal of Psychiatry, 165(12), 1532–1542. 10.1176/appi.ajp.2008.08020320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand J., McKay D., Wheaton M. G., Abramowitz J. S. (2013). The relationship between obsessive compulsive beliefs and symptoms, anxiety and disgust sensitivity, and Swine Flu fears. Journal of Obsessive-Compulsive and Related Disorders, 2(2), 200–206. 10.1016/j.jocrd.2013.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook L., Watkins E. (2016). Guided, internet-based, rumination-focused cognitive behavioural therapy (i-RFCBT) versus a no-intervention control to prevent depression in high-ruminating young adults, along with an adjunct assessment of the feasibility of unguided i-RFCBT, in the reducing stress and preventing depression trial (RESPOND): Study protocol for a phase III randomized controlled trial. Trials, 17(1), 1–11. 10.1186/s13063-015-1128-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ćosić K., Popović S., Šarlija M., Kesedžić I. (2020). Impact of human disasters and COVID-19 pandemic on mental health: Potential of digital psychiatry. Psychiatria Danubina, 32(1), 25–31. 10.24869/psyd.2020.25 [DOI] [PubMed] [Google Scholar]
- Fegert J. M., Vitiello B., Plener P. L., Clemens V. (2020). Challenges and burden of the coronavirus 2019. (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and Adolescent Psychiatry and Mental Health, 14, 20. 10.1186/s13034-020-00329-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flament M. F., Whitaker A., Rapoport J. L., Davies M., Berg C. Z., Kalikow K., Sceery W., Shaffer D. (1988). Obsessive compulsive disorder in adolescence: An epidemiological study. Journal of the American Academy of Child andAdolescent Psychiatry, 27(6), 764–771. 10.1097/00004583-198811000-00018 [DOI] [PubMed] [Google Scholar]
- Foa E. B., Huppert J. D., Leiberg S., Langner R., Kichic R., Hajcak G., Salkovskis P. M. (2002). The obsessive-compulsive inventory: Development and validation of a short version. Psychological Assessment, 14(4), 485–496. [PubMed] [Google Scholar]
- Foa E. B., Kozak M. J., Salkovskis P. M., Coles M. E., Amir N. (1998). The validation of a new obsessive-compulsive disorder scale: The obsessive-compulsive inventory. Psychological Assessment, 10(3), 206–214. 10.1037/1040-3590.10.3.206 [DOI] [Google Scholar]
- Fontenelle L. F., Mendlowicz M. V., Versiani M. (2006). The descriptive epidemiology of obsessive–compulsive disorder. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 30(3), 327–337. [DOI] [PubMed] [Google Scholar]
- Garcia R. (2017). Neurobiology of fear and specific phobias. Learning & Memory, 24(9), 462–471. 10.1037/1040-3590.14.4.485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janowitz D., Grabe H. J., Ruhrmann S., Ettelt S., Buhtz F., Hochrein A., Schulze-Rauschenbach S., Meyer K., Kraft S., Ferber C., Pukrop R., Freyberger H. J., Klosterkötter J., Falkai P., John U., Maier W., Wagner M. (2009). Early onset of obsessive-compulsive disorder and associated comorbidity. Depress Anxiety, 26, 1012–1017. 10.1002/da.20597 [DOI] [PubMed] [Google Scholar]
- Krebs G., Heyman I. (2015). Obsessive-compulsive disorder in children and adolescents. Archives of Disease in Childhood, 100(5), 495–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancee W. J., Maunder R. G., Goldbloom D. S. (2008). Coauthors for the impact of SARS study. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatric Services, 59(1), 91–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak I. W. C., Chu C. M., Pan P. C., Yiu M. G. C., Chan V. L. (2009). Long-term psychiatric morbidities among SARS survivors. General Hospital Psychiatry, 31(4), 318–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pauls D. L., Alsobrook J. P., Goodman W., Rasmussen S., Leckman J. F. (1995). A family study of obsessive-compulsive disorder. The American Journal of Psychiatry. [DOI] [PubMed] [Google Scholar]
- Rask C. U., Munkholm A., Clemmensen L., Rimvall M. K., Ørnbøl E., Jeppesen P., Skovgaard A. M. (2016). Health anxiety in preadolescence-Associated health problems, healthcare expenditure, and continuity in childhood. Journal of Abnormal Child Psychology, 44(4), 823–832. 10.1007/s10802-015-0071-2 [DOI] [PubMed] [Google Scholar]
- Rimvall M. K., Jeppesen P., Skovgaard A. M., Verhulst F., Olsen E. M., Rask C. U. (2021). Continuity of health anxiety from childhood to adolescence and associated healthcare costs: A prospective population-based cohort study. Journal of Child Psychology and Psychiatry, 62(4), 441–448. [DOI] [PubMed] [Google Scholar]
- Salkovskis P. M., Warwick H. M. (2001). Making sense of hypochondriasis: A cognitive theory of health anxiety. In Asmundson G. J., Taylor S., Cox B. J. (Eds.), Health anxiety: Clinical and research perspectives on hypochondriasis and related conditions (pp. 46–64). John Wiley & Sons. [Google Scholar]
- Shigemura J., Ursano R. J., Morganstein J. C., Kurosawa M., Benedek D. M. (2020). Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry and Clinical Neurosciences, 74(4), 281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin L. M., Liberzon I. (2010). The neurocircuitry of fear, stress, and anxiety disorders. Neuropsychopharmacology, 35(1), 169–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirri L., Garotti M. G. R., Grandi S., Tossani E. (2015). Adolescents’ hypochondriacal fears and beliefs: Relationship with demographic features, psychological distress, well-being and health-related behaviors. Journal of Psychosomatic Research, 79(4), 259–264. 10.1016/j.jpsychores.2015.07.002 [DOI] [PubMed] [Google Scholar]
- Stinson J., McCartney C. J., Leung A., Katz J. (2004). Impact of attending a healthcare conference in Toronto during the severe acute respiratory syndrome crisis: Survey of delegates. Pain Research and Management, 9(3), 137–143. [DOI] [PubMed] [Google Scholar]
- Vallarino M., Henry C., Etain B., Gehue L. J., Macneil C., Scott E. M., Barbato A., Conus P., Hlastala S. A., Fristad M., Miklowitz D., Scott J. (2015). An evidence map of psychosocial interventions for the earliest stages of bipolar disorder. The Lancet Psychiatry, 2(6), 548–563. 10.1016/S2215-0366(15)00156-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valleni-Basile L. A., Garrison C. Z., Jackson K. L., Waller J. L., McKeown R. E., Addy C. L., Cuffe S. P. (1994). Frequency of obsessive-compulsive disorder in a community sample of young adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 33(6), 782–791. 10.1097/00004583-199407000-00002 [DOI] [PubMed] [Google Scholar]
- Wheaton M. G., Abramowitz J. S., Berman N. C., Fabricant L. E., Olatunji B. O. (2012). Psychological predictors of anxiety in response to the H1N1 (swine flu) pandemic. Cognitive Therapy and Research, 36, 210–218. [Google Scholar]
- World Health Organization. (2020, March18). Mental health and psychosocial considerations during the COVID-19 outbreak. https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations
- Zohar A. H. (1999). The epidemiology of obsessive-compulsive disorder in children and adolescents. Child and Adolescent Psychiatric Clinics, 8(3), 445–460. [PubMed] [Google Scholar]