Highlights
-
•
The relationship between obesity and exposure to food advertising meets all criteria commonly used to demonstrate the presence of a causal relationship in epidemiology.
-
•
Younger children (≤8 years of age) are more susceptible to the impacts of food marketing, in terms of quantity and quality of calories consumed, than older children and adults, although emerging evidence suggests that adolescents (10–19 years) may be most susceptible to the impacts of online advertisements.
-
•
Children from socio-economically disadvantaged and ethnic minority backgrounds are disproportionately exposed to unhealthy food advertisements.
-
•
Statutory regulation is a potentially cost-effective policy option, in terms of healthcare savings outweighing the costs of implementing the policy. However, advertising restrictions must be accompanied by community-based interventions that address other causes of poor diet and sedentary behaviour; this is because online and TV advertisements represent one small dimension in the wider obesogenic environment.
-
•
Voluntary bans are ineffective. Exposure to unhealthy food advertising is similar before and after the introduction of voluntary food advertisements.
Keywords: Unhealthy eating, Obesity, TV and online food advertisements, Advertisement restrictions
Abstract
The World Health Organisation has urged all governments to address rising rates of obesity by implementing population-based interventions, such as restrictions on the marketing to children of unhealthy food and beverage items. However, the relationship between unhealthy food advertisements and childhood obesity is disputed by industry-sponsored reports, which recommend promoting physical activity and weight loss campaigns rather than policies to limit exposure to advertisements. We aimed to elucidate this debate by providing a narrative review of the evidence on the relationship between unhealthy TV and online food advertisements, short-term food consumption and childhood obesity. We also examined the impact of unhealthy food advertisements on vulnerable groups and identified which policy interventions are supported by current evidence.
We conducted a rapid overview of reviews published since 2006. From a synthesis of 18 reviews meeting the inclusion criteria, we conclude that exposure to unhealthy TV and online food advertising is a contributing factor to childhood obesity. Evidence of a relationship between exposure to unhealthy food advertisements and childhood obesity was evident at all stages of the causal pathway, including a clear dose-response relationship. The evidence base was particularly strong for children aged 3–12 years of age and for children from socio-economically disadvantaged and minority ethnic backgrounds.
The introduction of statutory regulation is a potentially cost-effective policy option, in terms of healthcare savings outweighing the costs of implementing the policy, although voluntary codes were shown to be ineffective, with exposure to unhealthy food advertisements similar in countries before and after their introduction. Food advertising, however, is just one factor in the wider obesogenic environment and further advertising restrictions must be implemented alongside population-based interventions that aim to address systemic causes of poor diet.
1. Introduction
Globally, obesity in childhood and adolescence has reached epidemic proportions (Bhadoria et al., 2015, Global Burden of Disease Study, 2015). Between 1980 and 2013; the prevalence of excess weight and obesity in high-income countries increased from 16.9% to 23.8% for boys (≥18 years) and from 16.2% to 22.6% for girls (Ng et al., 2014). Over the same period; prevalence in low- and middle-income countries increased from 8.1% to 12.9% for boys and from 8.4% to 13.4% for girls. Excess weight in childhood and adolescence is associated with the development of morbidities traditionally observed during adulthood, including type 2 diabetes, hypertension and fatty liver disease (Kumar and Kelly, 2017, Daniels, 2009). Children who are obese are also at increased risk of developing cardiovascular disease; cancer, osteoarthritis, chronic kidney disease and psychological disorders in later life (Wormser et al., 2011, Renehan et al., 2008, MacMahon et al., 2009).
The World Health Organisation has urged all governments to address rising rates of obesity by implementing a variety of population-based interventions (World Health Organisation, 2014); including restrictions on the marketing to children of food and beverages high in fat, sugar and salt (HFSS) (World Health Organisation, 2012). In 2007; the UK became the first country to introduce a total ban on HFSS food advertisements around children’s television (TV) programmes (Boyland and Harris, 2017, House of Commons, 2020). By 2019; a further 15 countries had introduced similar statutory regulation (Taillie et al., 2019). However; a 2019 policy evaluation found small or no policy-related reductions in HFSS food advertisements following the introduction of marketing restrictions: and any potential reduction in TV marketing exposure to have been offset by increased HFSS food marketing via other platforms (Taillie et al., 2019). In particular; online advertising has become ever more prevalent, with marketers directly targeting children via websites, advergames and other digital platforms (Culp et al., 2010). While online advertisements are often regulated by national agencies (e.g.; Advertising Standards Authority in the UK), there is difficulty in determining whether they are indeed advertisements, as they are often presented as entertainment platforms.
In 2020, the UK government introduced a national obesity strategy with the aim of addressing the causes of weight gain in both children and adults (Department of Health and Social Care, 2020). One of the main initiatives; and a primary focus, of this strategy is to further restrict the online and TV (screen) advertising of unhealthy food and beverage items directed at children and adolescents (Department of Health and Social Care, 2020). While it may seem logical that exposure to unhealthy food advertisements results in increased consumption of HFSS food and beverage items; therefore contributing towards weight gain and obesity, this relationship is disputed by industry experts and industry-sponsored reports, which instead argue ‘there is no scientific consensus that food advertising causes obesity’ (Interactive Advertising Bureau UK, 2020, Advertising Association, 2014). In this paper; we aim to elucidate this debate by providing a narrative review of the evidence about screen advertising of HFSS products. While previous reviews have examined the impact of HFSS food advertisements on specific outcomes (e.g., short-term dietary intake, see (Folkvord and van ‘t Riet, 2018, Russell et al., 2019, Sadeghirad et al., 2016, Boyland et al., 2016), this is the first review to consider all stages in the causal pathway, from the prevalence of TV and online HFSS food advertisements to short-term food consumption and obesity, while also considering the impact of HFSS food advertisements on vulnerable groups and examining key policy implications. This is also the first overview of existing systematic reviews to be undertaken (i.e., an umbrella review). The defining feature of umbrella reviews, which are particularly important for providing healthcare professionals and policy makers with a clear understanding of complex topics, is that they only consider for inclusion the highest level of academic evidence, namely other systematic reviews and meta-analyses (Aromataris et al., 2015).
One difficulty in regulating food advertisements, often exploited by media companies, is the absence of a universal definition for HFSS foods (Jenkin et al., 2009). However, one widely accepted convention for categorising food types is the Nutrient Profile model developed by the UK’s Food Standards Agency in 2004/05 (Jenkin et al., 2009, Food Standards Agency, 2011). This model applies a scoring system which balances the contribution made by beneficial nutrients, that are particularly important in children’s diets, with components in the food that children should eat less of. However, studies included within this review applied a range of definitions for HFSS and ‘unhealthy’ foods, which means studies conducted in different locations may not be directly comparable (i.e., an external validity bias).
In this review, we examine current levels of exposure to HFSS food advertisements and the impact of statutory legislation on children’s (up to 18 years old) exposure to such advertisements. We then explore the relationship between exposure to HFSS food advertisements and both short-term and long-term health and behavioural outcomes, including calorie intake and childhood obesity. Finally, we explore which groups are most exposed to HFSS food advertisements and identify how the available evidence supports different policy options.
2. Methods
We conducted a rapid overview of reviews published in the medical literature on the links between food advertising and obesity in children and adolescents up to 18 years old. When compared with full reviews, rapid reviews incur no discernible impacts on derived conclusions (Watt et al., 2008, Haby et al., 2016). We searched MEDLINE in November 2020 to identify relevant literature. Reviews were supplemented with original research articles if sufficient evidence was not identified. The review covered English-language studies published from 2006 to 2020. We included any reviews that contained an advertisement element (intervention/exposure) of food and drink and captured obesity related outcomes (short term food intake, weight gain and BMI). Studies were abstracted using a pre-defined framework to extract key data, such as design of included studies, sample size, analysis, population, intervention/exposure and outcomes. This review identified 18 reviews (systematic, narrative and scoping), incorporating results of some 400 peer-reviewed studies involving more than 9000 individuals.
The study was based on publicly available anonymised datasets and was thus exempt from ethical compliance (we have our exemption on file from University of Warwick’s institutional review board).
3. Results
3.1. Children’s exposure to HFSS food advertisements
The screen advertising of HFSS food products is extensive around the world and disproportionately directed at children rather than adults (Smith et al., 2019). A 2019 study; collating TV advertising data from 22 countries (including Australia, Canada, Chile, Costa Rica, Guatemala, Malta, Mexico, New Zealand, and Slovenia), found children aged up to 18 years were exposed to between 1.7 (Malta) to 13.4 (Canada) HFFS advertisements per hour during peak viewing times, with a global average of 3.1 HFFS food advertisements per hour (Kelly et al., 2019). The most frequently advertised food and beverage items globally were carbonated soft drinks; flavoured waters, chocolate and confectionary. Overall, HFSS food items are promoted four times more than healthier food items, with the majority of HFSS food advertisements derived from a small number of transnational companies.
Children aged 5 – 15 years in the UK spend an average of 1 h 52 min in front of a TV set (Ofcom, 2018), compared to around 3.8 h per day in the USA (Walsh et al., 2020) and 3 h per day in Canada (Statistics Canada, 2019). The UK’s regulatory authority for broadcasting, Ofcom, suggests that children aged 4 – 15 years were exposed to 34% fewer HFSS food advertisements following the introduction of statutory legislation in 2007 (Ofcom, 2010). However, this reduction has been contested by academic studies which indicate any impact has either been minimal or not occurred at all (Boyland et al., 2008, Adams et al., 2012, Adams et al., 2012, Boyland and Halford, 2013, Pournaghi Azar et al., 2018), partly as a result of two-thirds of children watching TV during what is considered ‘adult-air time’ and therefore not covered by the current advertising ban (Foundation, 2016). For example, a 2017 study examining advertisements broadcast on the UK’s leading commercial channel between 06:00 and 22:00 found food adverts to account for 16.7% of all advertisements (n = 1532) with the majority (61%; n = 934) classified as potentially harmful to children’s (oral) health due to their high sugar or acid content (Al-Mazyad et al., 2017). A similar trend was observed globally, with a study using data captured between 2008 and 2017 identifying no difference in the frequency of HFSS food advertisements targeting children in countries with statutory legislation (e.g., Australia, Mexico, South Africa, Thailand) when compared to countries with no restrictions (e.g., Argentina, Chile and China) or self-enforced regulations (e.g., Canada, Spain and New Zealand) at the time of data captured (Kelly et al., 2019).
In addition to TV advertising, children are increasingly exposed to new forms of online marketing. One example is the ‘advergame’, an interactive online game that contains embedded media content with the purpose of promoting specific brands or products (Culp et al., 2010). A 2018 meta-analysis of 15 global studies; focusing on children aged 5 – 17 years, found 97% of all food and beverage advergames to contain at least one food cue that is considered a brand identifier, such as placing a branded food item (e.g., cereal, soft drink or snack food) in the mouth of a popular children’s character (Folkvord and van ‘t Riet, 2018). The primary focus of most advergames is the promotion of HFSS food (Sonntag et al., 2015). As advergames do not typically include age restrictions; it is likely that children are accessing advergames that are not age appropriate. Parents and children are often unaware that advergames have a marketing element and instead mistake these advertising vehicles for generic online games (Folkvord and van ‘t Riet, 2018). Difficulties in determining whether advergames are paid for advertisements; rather than generic online games; prevents advertising standards authorities from effectively monitoring their content. The highly targeted nature of online advertisements also makes it difficult to quantify exact levels of exposure, although it is known that children aged 5 – 15 years in the UK spend an average of 2 h 11 min per day online (Ofcom, 2018).
3.2. Relationship between HFSS food advertisements and food consumption
Five systematic reviews, focusing on children and adolescents up to 19 years, in the last 15 years have examined the relationship between exposure to HFSS food advertisements and short-term food consumption in children, all of which found a significant increase in HFSS food consumption following exposure to screen advertisements (Folkvord and van ‘t Riet, 2018, Russell et al., 2019, Sadeghirad et al., 2016, Boyland et al., 2016, Qutteina et al., 2019). The most recent of these systematic reviews, published in 2019, collated evidence from 39 published studies and found that children aged 2 – 18 years exposed to 4.4 min of TV food advertisements increased their short-term food consumption by 60.0 kcal compared to children exposed to non-food advertisements (Russell et al., 2019). The effect of advergames was found to be similar, with the same systematic review finding that playing an advergame containing a food cue for five minutes increased children’s short-term food consumption by 53.4 kcal when compared to advergames without food cues (Russell et al., 2019). The study authors noted that real-world exposure to food advertisements is likely to be in excess of the levels included in these studies (Russell et al., 2019). A second systematic review, also published in 2019, found both unhealthy food consumption and brand recognition to increase among both pre-adolescents (8–11 year olds) and adolescents (12–19 year olds) in response to media food marketing (Qutteina et al., 2019). Earlier systematic reviews found a similar increase in short-term food consumption following exposure to HFSS food advertisements (Folkvord and van ‘t Riet, 2018, Boyland et al., 2016), including a 2016 meta-analysis of 17 randomised control trials, focusing on children aged 2–18 years, which found a 30 kcal increase in dietary intake following five minutes exposure to unhealthy food and beverage marketing (Sadeghirad et al., 2016). Food advertisements seem to have a more powerful influence on children’s preference for less healthy food options, for example, if the same character is used to promote fruit or vegetables it does not have the same effect on increased consumption of the promoted food (Kraak and Story, 2015).
3.3. Relationship between HFSS food advertisements and obesity
Whether the acute increase in food consumption, in response to food advertising, is associated with long-term health outcomes such as obesity is not clear from the literature, due to a lack of longer-term longitudinal evidence. However, a 2016 systematic review found that the relationship between obesity and exposure to food advertising meets all criteria used to determine the presence of a causal relationships in epidemiology (Norman et al., 2016). This research was undertaken using the ‘Bradford Hill Criteria’. The Bradford Hill Criteria, a recognised public health framework, consists of nine conditions (strength of evidence; consistency of findings; specificity; temporality; biological gradient; plausibility; coherence; experimental evidence; and analogy) which are often used in epidemiological studies to provide evidence of a relationship between a presumed cause and an observed outcome (Bradford, 1965). Previous studies have applied the Bradford Hill Criteria to identify relationships between alcohol consumption and cardiovascular disease, pesticide use and decline of pollinator species and exposure to ultraviolet radiation and development of skin cancer (Ronksley et al., 2011, Cresswell et al., 2012, Grant, 2009).
A relationship between exposure to unhealthy food advertisements and childhood obesity was evident for each condition associated with the Bradford Hill Criteria, including presence of a clear dose-response relationship; consistency of evidence; presence of a temporal relationship and existence of a plausible biological mechanism. The review cited numerous cross-sectional studies demonstrating a dose-response relationship, including an Australian study, focusing on children aged 10–16 years, showing that every hour of commercial TV viewing per week was associated with a 0.067 unit increase in unhealthy diet scores based on data collected using a population health survey (Kelly et al., 2016a). The evidence base was particularly strong for children aged 3–12 years, with exposure to marketing across all media platforms consistently demonstrating significant, adverse effects on food preferences and food consumption (Norman et al., 2016).
The exact mechanism underpinning the relationship between exposure to HFSS food advertisements and obesity is still to be identified, however, it is hypothesised that exposure to screen advertisements initiate a lack of impulsive inhibition in children, making them less able to control eating impulses and more susceptible to unhealthy food stimuli such as those found in HFSS advertisements. Indeed, research by Norman et al (Norman et al., 2019), examining eating behaviour (snacking and lunch) in children (7–12 years) following exposure to food and non-food screen advertisements determined that this imbalance, if sustained over time, could drive a positive energy gap capable of underpinning excess weight gain in children. This energy gap has been shown to be most pronounced in children that are overweight and obese.
3.4. Impact on vulnerable groups
There is strong and consistent evidence, from a 2020 systematic review collating evidence from 25 studies, that children up to the age of 18 from socio-economically disadvantaged and ethnic minority backgrounds, who may face greater health-risks from obesity (Marmot et al., 2020), are disproportionately exposed to all forms of advertising promoting HFSS foods (Backholer et al., 2020). In relation to TV advertising, all included studies found a significant negative relationship between household income and exposure to HFSS food advertisements. In total, 19 out of the 25 studies included in this review revealed higher exposure to unhealthy food advertisements among ethnic minority and economically disadvantaged children across numerous countries, including the USA, New Zealand and the UK. This included two studies from the USA which found a greater proportion of unhealthy food advertisements on television networks targeting Black and Spanish-speaking children compared with the sample mean and English-speaking channels (Kunkel et al., 2013, Bell et al., 2009), as well as one study from the UK which found that exposure to food advertising was 2.1 times greater among the least, compared with the most, affluent areas (Adams et al., 2012, Adams et al., 2012). This is partly due to the fact that children from the most deprived regions and ethnic minority groups spend more time than their higher-income peers watching TV and playing online games (Ofcom, 2018).
Younger children (≤8 years of age) are also more susceptible to the impacts of food marketing, in terms of quantity and quality of calories consumed, than older children and adults because they are unable to understand its selling or persuasive intent (Sadeghirad et al., 2016, Boyland et al., 2016). In fact, a systematic review examining food promotions in Australia found that 75%-100% of 6-year-olds fail to comprehend the basic purpose of food advertisements (Carter, 2006). Children who are overweight or obese are also more vulnerable to the influence of marketing. Following exposure to HFSS food advertisements, children who are overweight or obese consume an average of 45.6 kcal more than children of healthy weight (Russell et al., 2019). A further subgroup analysis found the difference between children with healthy weight and children with overweight/obesity to be statistically significant.
3.5. Effectiveness of policy implications
A total of four systematic reviews were identified examining the effectiveness of policy interventions that aim to reduce exposure to HFSS advertisements (Gortmaker et al., 2015, Lobstein et al., 2020, Chambers et al., 2015, Galbraith-Emami and Lobstein, 2013). Despite these studies being heterogenous in study design, further statutory regulation was determined to be a potentially cost-effective policy option, in terms of healthcare savings outweighing the costs of implementing the policy (Carter et al., 2009, Gortmaker et al., 2015). Identified studies included a 2015 systematic review and microsimulation model (to calculate the costs and effectiveness of interventions through their impact on BMI changes), which identified three out of seven interventions (a sugar-sweetened beverage excise tax; eliminating the tax subsidy for advertising unhealthy food to children; and setting nutrition standards for food and beverages sold in schools outside of school meals) to save more in health care costs than they cost to implement. Each of the three interventions were projected to prevent 129,000–576,000 cases of childhood obesity in the USA in 2025 (Gortmaker et al., 2015). A narrative review of 30 studies, examining the cost-effectiveness of different policy options to reduce HFSS food consumption in children, found restrictions of online and TV advertisements to be the single most cost-effective option available to policy makes when compared to interventions such as nutritional labelling or introducing a processed food tax (Lobstein et al., 2020). The same review highlighted that these health care savings are likely to be underestimated, as not all health benefits have been included in studies to date.
A 2015 systematic review of 47 publications identified voluntary codes to be insufficient in reducing the advertising of HFSS food, however, statutory regulation could reduce the volume of children's exposure to advertising for HFSS foods (Chambers et al., 2015). Finally; a 2013 systematic review of 21 publications found exposure to HFSS food advertising to be similar in countries before and after the introduction of voluntary food advertisement restrictions (Galbraith-Emami and Lobstein, 2013); while industry-sponsored reports typically overestimate the effect of voluntary bans (Galbraith-Emami and Lobstein, 2013). The introduction of further statutory regulations is widely supported by both the general public and health care professionals (Lobstein et al., 2020).
4. Discussion
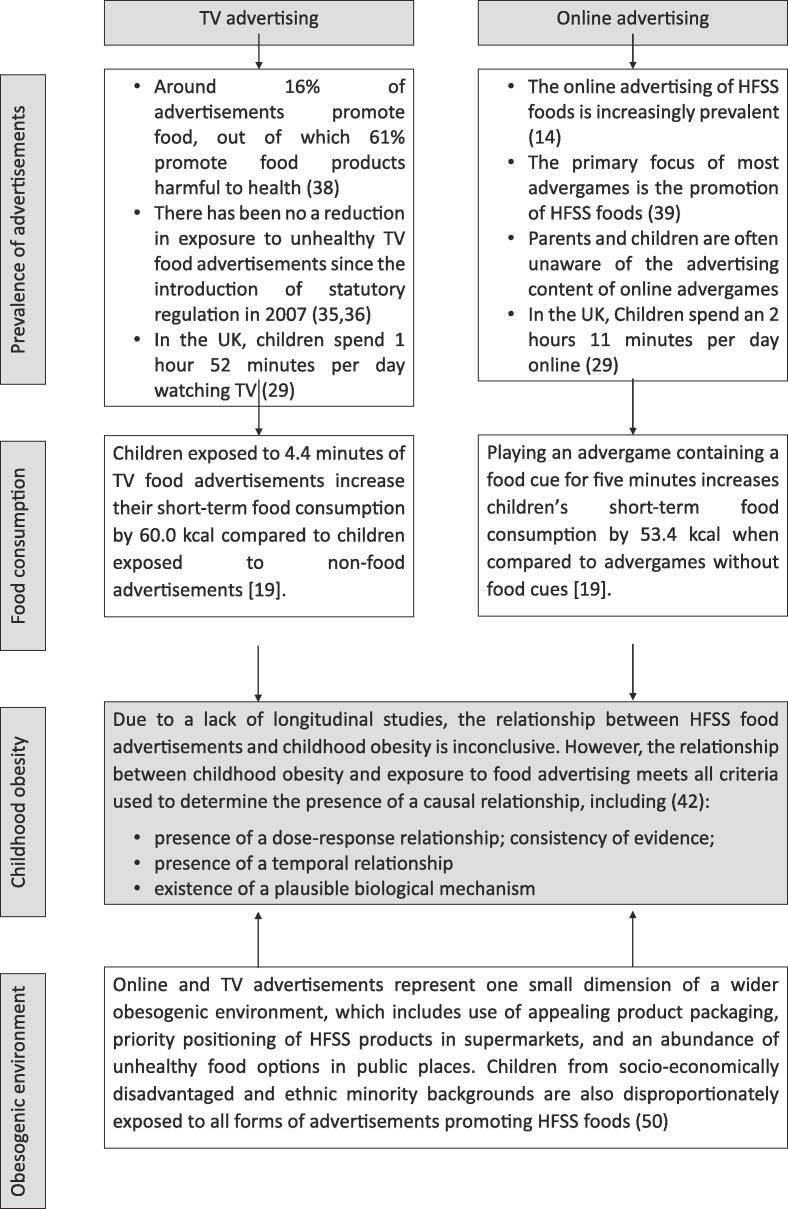
The primary aim of this review was to examine the relationship between exposure to unhealthy TV and online food advertisements, short-term food consumption and obesity in children and adolescents (up to the age of 18 years). This review also examined the impact of HFSS food advertisements on vulnerable groups and identified key policy implications. From this synthesis, we conclude that exposure to online and TV HFSS food advertisements is associated with increased short-term food consumption and is a contributing factor to childhood obesity (Fig. 1). The evidence base is particularly strong for children aged 3–12 years of age and for children from socio-economically disadvantaged and minority ethnic backgrounds. However, online and TV advertisements represent just one small dimension in the wider obesogenic environment and the food industry targets children in multiple ways, including the use of appealing product packaging, priority positioning of HFSS products in supermarkets, and an abundance of unhealthy food options in public places (Elliott and Truman, 2020, Paes et al., 2015;.).
Fig. 1.
The relationship between exposure to TV and online unhealthy food advertising and childhood obesity.
The relationship between exposure to HFSS food advertisements and childhood obesity was evident at all stages of the causal pathway (Fig. 1), with food advertisements dominated by HFSS foods and a clear association between exposure to unhealthy food advertisements and increased food consumption and calorie intake. The subsequent relationship between HFSS food advertisements and childhood obesity meets all criteria conventionally used to determine the presence of a causal relationship, while children from socio-economically disadvantaged and ethnic minority groups are disproportionately exposed to all forms of screen advertising. While most studies to date have focused on the impact of exposure to advertisements in children, emerging evidence suggests that adolescents (10–19-year-olds) may actually be more susceptible to the impacts of online advertisements than younger children (Harris et al., 2020).
Despite the consistent evidence (Folkvord and van ‘t Riet, 2018, Russell et al., 2019, Boyland et al., 2016, Qutteina et al., 2019, Galbraith-Emami and Lobstein, 2013) that exposure to HFSS food advertisements promotes short-term consumption of energy dense, nutrient poor foods, in contrast to academic publications, industry sponsored reports consistently reject the existence of a relationship between exposure to HFSS advertisements and childhood obesity (Interactive Advertising Bureau, 2020, Advertising Association, 2014) and instead recommend interventions that promote physical activity and weight loss (Elliott and Truman, 2020). This is likely due to the lack of studies linking the immediate behaviour change with longer term health outcomes, however in our synthesis we elucidate strong evidence supporting a likely causal relationship, ultimately driving health outcomes. While the mechanisms by which food advertising affects eating behaviour are beyond the scope of this review, it appears that exposure to unhealthy food advertising reinforces social norms related to unhealthy eating and more strongly shapes desire and preference for unhealthy foods. Food advertisements activate a region of children’s brains called the ventromedial prefrontal cortices, which play a role in decision-making, reward valuation and self‐control (Bruce et al., 2016). This activation results in more rapid food decisions, a tendency to favour taste over nutrition and reduced impulse inhibition. If sustained over a prolonged period, as occurs in real-world settings, this response has the potential to drive a positive energy gap, resulting in increased weight gain and obesity (Norman et al., 2019, Paes et al., 2015). Indeed, the obesogenic environment framework, as proposed by Swinburn et al. (2004), outlines how unhealthy dietary patterns are continually promoted both within an individual’s micro- (e.g., schools, supermarkets and homes) and macro-environment (e.g., through failure of government policy and healthcare systems). Previous systematic reviews have also found mechanisms that are used by the advertising industry to promote HFSS foods to be ubiquitous across different environments (television, internet, within supermarkets) and countries, including use of attractive packaging, brand mascots, toys and development of emotional appeal to establish lasting relationships and brand loyalty (Paes et al., 2015). However, it must be noted that most studies to date have focused on responses to food advertising in high-income countries and no systematic reviews have yet been published that focus exclusively on impacts of food advertising in low- or middle-income countries, although emerging evidence does suggest that children in these countries may be more vulnerable to impacts of screen marketing given the relative novelty and recent expansion of screen advertising in these countries (Kelly et al., 2016b).
While the focus of this review is the relationship between HFSS food advertisements and childhood obesity, we recognise that there are many genetic and non-genetic determinants of obesity. However, it is well recognised that the primary cause of obesity is calorie intake exceeding calorie expenditure (Kumar and Kelly, 2017, Harris et al., 2020). A 2019 systematic review of 33 childhood obesity prevention programmes found that interventions were only effective in reducing prevalence of overweight/obesity in children if they considered both the food environment and levels of physical activity (Bramante et al., 2019). Further regulation of HFSS food advertisements is therefore unlikely to reduce rates of childhood obesity unless implemented alongside population-based interventions that address systemic causes of poor diet; sedentary behaviour and socio-economic drivers of food insecurity (Biddle et al., 2017, Hemmingsson, 2018, Pachucki, 2015, Weihrauch-Blüher et al., 2018). Additionally; screen advertisements represent just one small dimension in the wider obesogenic environment.
While the World Health Organization has called for governments to restrict food and beverage marketing to children, the evidence we have reviewed suggests that even statutory legislation has little impact in reducing exposure to HFSS advertisements, with children exposed to a similar volume of HFSS advertisements in countries with no restrictions, self-regulation and statutory legislation (Kelly et al., 2019). In addition; the purpose of legislation to date has been to reduce children’s exposure to HFSS advertisements; this is despite the increasing difficulty in defining ‘children’s’ content in the online world of 24-hour streaming services and advergames. It is clear that any attempt to address underlying causes of childhood obesity must apply a whole food systems approach which considers how all dimensions of the food system, from food production to purchasing and marketing, interact and determine dietary behaviour, while also addressing the social and economic drivers of poor diet, such as food availability and affordability. In 2021, the UK’s Institute for Public Policy Research outlined six immediate actions that local and national policy makers can take to ensure everyone, irrespective of socio-economic status, can access healthy and affordable food (Coleman et al., 2021). These six recommendations were: (1) enshrining the right to healthy food in law; (2) the development of regional food councils; (3) establishment of nationally agreed targets to increase uptake of sustainably and ethically produced meat and plant-based options; (4) improved quality of food in public institutions, such as schools; (5) ensuring all members of society have the financial means to access healthy food and (6) introduction of codes of compliance for fair supply chain practice across agri-food sectors. It is only through this whole food systems lens, alongside legislation that limits exposure to HFSS advertisements, that governments, policy makers and health professionals will address the drivers of poor diet, weight gain and obesity.
During this review, we noted a lack of evidence on the relationship between HFSS food advertisements and obesity in adulthood. This is an important area of future research, as current empirical evidence does not exist to support the introduction of advertising restrictions after 21:00 (i.e., during adult viewing time). Systematic reviews to date have also applied a heterogenous definition of children’s TV hours, which can include any TV before 21:00, only TV programmes containing children’s content or any programme during certain hours (e.g., 08:00–11:00 on weekend mornings), limiting our ability to estimate current levels of exposure to HFSS food advertisements. Similarly, ‘children’ is not always clearly defined and is often used to include both younger children and adolescents. The inclusion criteria utilised in this study included any study focusing on children up to the age of 18 years old. The majority of studies to date have focused on TV rather than online advertisements, although the association with short-term food consumption and childhood obesity is similar for both online and TV advertisements. Exposure to online and TV advertising is also associated with other unhealthy behaviours, such as increased sedentary behaviour (Biddle et al., 2017), suggesting it may be a combination of interacting factors that drive childhood obesity. There is also considerable variation in the definition of ‘unhealthy’/HFSS foods between studies, introducing limitations when comparing findings between different countries. It may be helpful for studies to apply a single recognised convention in defining HFSS foods, such as the Nutrient Profile model (Jenkin et al., 2009, Food Standards Agency, 2011). In addition, there is limited information on gender differences following exposure to HFSS food advertisements and limited information on whether increased calorie intake associated with exposure to HFSS food advertisements is clinically significant. Finally, as this review focused exclusively on publications available via MEDLINE there will have been publications, particularly from the social sciences, available on search engines such as PsycInfo and Communication & Mass Media Complete not included in this review. However, it has previously been shown that rapid reviews incur no discernible impacts on derived conclusions when compared with full reviews (Watt et al., 2008, Haby et al., 2016).
5. Conclusion and policy implications
On the basis of the literature reviewed in this paper, we argue there is sufficient evidence for governments to implement restrictions that would further limit children’s exposure to both TV and on-line advertising of HFSS food. In the UK, current regulations restrict the advertising of HFSS food immediately before, during, or after children’s television programmes (Burki, 2018). However, this represents just 27% of children’s TV viewing time, with children instead watching a majority of programmes that are classified as ‘family entertainment’ between 18:00–21:00, when restrictions are not in place (Cancer Research UK, 2018). Cancer Research UK have proposed introducing a total ban on HFSS food advertisements before 21:00 (Cancer Research UK, 2018). The evidence we reviewed justifies this proposal. The introduction of further statutory regulation in the UK is widely supported by both the general public and health care professionals (Lobstein et al., 2020).
The online advertising of HFSS food in the UK is regulated by the UK’s Advertising Standards Authority, however enforcement is often impeded by the difficulty in determining whether online content is identifiable as an advertisement (Advertising Standards Authority, 2016). This is despite evidence, presented in this review, of a clear association between online HFSS food advertisements and increased food consumption (Russell et al., 2019). Consequently, a total ban on HFSS food advertisements before 21:00 should also be applied to online streaming services, as well as a total ban placed on online advergames which have been developed for the primary purpose of promoting HFSS foods. Even small effects on dietary behaviour from increased regulation of HFSS marketing at an individual level can have huge impacts across the whole population, as outlined by Rose’s prevention paradox (Geoffrey, 1981). However, this must be implemented alongside other population-based interventions that apply a whole food systems approach to addressing the systemic causes of poor diet and socio-economic drivers of food insecurity and obesity.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
All authors are members of The Warwick Obesity Network, an interdisciplinary team of academics and clinicians at the University of Warwick working on obesity interventions.
Disclosure of Funding and Conflicts of Interest
The activities of the network are supported by a Warwick ESRC IAA Internal Network Grant (reference ES/T502054/1). Oyinlola Oyebode is affiliated to the National Institute for Health Research (NIHR) Applied Research Collaboration (ARC) West Midlands. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Funding
This work was funded by a Warwick ESRC IAA Internal Network Grant (reference ES/T502054/1).
References
- Bhadoria A., Sahoo K., Sahoo B., Choudhury A., Sufi N., Kumar R. Childhood obesity: Causes and consequences. Journal of Family Medicine and Primary Care. Medknow. 2015;4:187. doi: 10.4103/2249-4863.154628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global Burden of Disease Study. Global Burden of Disease Study 2015: Obesity and Overweight Prevalence 1980-2015. Available from: http://ghdx.healthdata.org/record/ihme-data/gbd-2015-obesity-and-overweight-prevalence-1980-2015.
- Ng M., Fleming T., Robinson M., Thomson B., Graetz N., Margono C., Mullany E.C., Biryukov S., Abbafati C., Abera S.F., Abraham J.P., Abu-Rmeileh N.M.E., Achoki T., AlBuhairan F.S., Alemu Z.A., Alfonso R., Ali M.K., Ali R., Guzman N.A., Ammar W., Anwari P., Banerjee A., Barquera S., Basu S., Bennett D.A., Bhutta Z., Blore J., Cabral N., Nonato I.C., Chang J.-C., Chowdhury R., Courville K.J., Criqui M.H., Cundiff D.K., Dabhadkar K.C., Dandona L., Davis A., Dayama A., Dharmaratne S.D., Ding E.L., Durrani A.M., Esteghamati A., Farzadfar F., Fay D.F.J., Feigin V.L., Flaxman A., Forouzanfar M.H., Goto A., Green M.A., Gupta R., Hafezi-Nejad N., Hankey G.J., Harewood H.C., Havmoeller R., Hay S., Hernandez L., Husseini A., Idrisov B.T., Ikeda N., Islami F., Jahangir E., Jassal S.K., Jee S.H., Jeffreys M., Jonas J.B., Kabagambe E.K., Khalifa S.E.A.H., Kengne A.P., Khader Y.S., Khang Y.-H., Kim D., Kimokoti R.W., Kinge J.M., Kokubo Y., Kosen S., Kwan G., Lai T., Leinsalu M., Li Y., Liang X., Liu S., Logroscino G., Lotufo P.A., Lu Y., Ma J., Mainoo N.K., Mensah G.A., Merriman T.R., Mokdad A.H., Moschandreas J., Naghavi M., Naheed A., Nand D., Narayan K.M.V., Nelson E.L., Neuhouser M.L., Nisar M.I., Ohkubo T., Oti S.O., Pedroza A., Prabhakaran D., Roy N., Sampson U., Seo H., Sepanlou S.G., Shibuya K., Shiri R., Shiue I., Singh G.M., Singh J.A., Skirbekk V., Stapelberg N.J.C., Sturua L., Sykes B.L., Tobias M., Tran B.X., Trasande L., Toyoshima H., van de Vijver S., Vasankari T.J., Veerman J.L., Velasquez-Melendez G., Vlassov V.V., Vollset S.E., Vos T., Wang C., Wang XiaoRong, Weiderpass E., Werdecker A., Wright J.L., Yang Y.C., Yatsuya H., Yoon J., Yoon S.-J., Zhao Y., Zhou M., Zhu S., Lopez A.D., Murray C.J.L., Gakidou E. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar S., Kelly A.S. Review of Childhood Obesity: From Epidemiology, Etiology, and Comorbidities to Clinical Assessment and Treatment. Mayo Clin. Proc. Elsevier Ltd. 2017;92(2):251–265. doi: 10.1016/j.mayocp.2016.09.017. [DOI] [PubMed] [Google Scholar]
- Daniels S.R. Complications of obesity in children and adolescents. Int J Obes. 2009;33(S1):S60–S65. doi: 10.1038/ijo.2009.20. [DOI] [PubMed] [Google Scholar]
- Wormser D., Kaptoge S., Di Angelantonio E., Wood A.M., Pennells L., Thompson A., et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: Collaborative analysis of 58 prospective studies. Lancet. 2011;377:1085–1095. doi: 10.1016/S0140-6736(11)60105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renehan A.G., Tyson M., Egger M., Heller R.F., Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371(9612):569–578. doi: 10.1016/S0140-6736(08)60269-X. [DOI] [PubMed] [Google Scholar]
- MacMahon S., Baigent C., Duffy S., Rodgers A., Tominaga S., Chambless L., et al. Body-mass index and cause-specific mortality in 900 000 adults: Collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organisation. Obesity and inequities Guidance for addressing inequities in overweight and obesity. 2014. Available from: http://www.euro.who.int/pubrequest.
- World Health Organisation. A framework for implementing the set of recommendations on the marketing of foods and non-alcoholic beverages to children. 2012. Available from: http://www.who.int/about/licensing/.
- Boyland E.J., Harris J.L. Regulation of food marketing to children: are statutory or industry self-governed systems effective? Public Health Nutr. 2017;20(5):761–764. doi: 10.1017/S1368980017000465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House of Commons. Briefing paper: Advertising to children. 2020. Available from: https://researchbriefings.files.parliament.uk/documents/CBP-8198/CBP-8198.pdf.
- Taillie LS, Busey E, Stoltze FM, Dillman Carpentier FR. Governmental policies to reduce unhealthy food marketing to children. Nutr Rev.2019;77:787–816. [DOI] [PMC free article] [PubMed]
- Culp J., Bell R.A., Cassady D. Characteristics of Food Industry Web Sites and “Advergames” Targeting Children. J Nutr Educ Behav. 2010;42(3):197–201. doi: 10.1016/j.jneb.2009.07.008. [DOI] [PubMed] [Google Scholar]
- Department of Health and Social Care. Tackling obesity: government strategy. 2020. Available from: https://www.gov.uk/government/publications/tackling-obesity-government-strategy.
- Interactive Advertising Bureau UK. Q&A: What does an online HFSS ad ban mean? 2020. Available from: https://www.iabuk.com/news-article/qa-what-does-online-hfss-ad-ban-mean#:∼:text=Last updated%2C November 2020.&text=What has the Government said,by the end of 2022.
- Advertising Association. Understading Food Advertising. 2014. Available from: www.adassac.org.uk.
- Folkvord F., van ‘t Riet J. The persuasive effect of advergames promoting unhealthy foods among children: A meta-analysis. Appetite. 2018;129:245–251. doi: 10.1016/j.appet.2018.07.020. [DOI] [PubMed] [Google Scholar]
- Russell S.J., Croker H., Viner R.M. The effect of screen advertising on children’s dietary intake: A systematic review and meta-analysis. Obes Rev. 2019;20(4):554–568. doi: 10.1111/obr.12812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadeghirad B., Duhaney T., Motaghipisheh S., Campbell N.R.C., Johnston B.C. Influence of unhealthy food and beverage marketing on children’s dietary intake and preference: a systematic review and meta-analysis of randomized trials. Obes Rev. 2016;17(10):945–959. doi: 10.1111/obr.12445. [DOI] [PubMed] [Google Scholar]
- Boyland E.J., Nolan S., Kelly B., Tudur-Smith C., Jones A., Halford J.C., Robinson E. Advertising as a cue to consume: a systematic review and meta-analysis of the effects of acute exposure to unhealthy food and nonalcoholic beverage advertising on intake in children and adults 1,2. Am J Clin Nutr. 2016;103(2):519–533. doi: 10.3945/ajcn.115.120022. [DOI] [PubMed] [Google Scholar]
- Aromataris E., Fernandez R., Godfrey C., Holly C., Khalil H., Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. International journal of evidence-based healthcare. Int J Evid Based Healthc. 2015;13:132–140. doi: 10.1097/XEB.0000000000000055. [DOI] [PubMed] [Google Scholar]
- Jenkin G., Wilson N., Hermanson N. Identifying ‘unhealthy’ food advertising on television: a case study applying the UK Nutrient Profile model. Public Health Nutrition. 2009;12(5):614–623. doi: 10.1017/S1368980008003029. [DOI] [PubMed] [Google Scholar]
- Food Standards Agency. The nutrient profiling model. 2011. Available from: https://www.gov.uk/government/publications/the-nutrient-profiling-model.
- Watt A, Cameron A, Sturm L, Lathlean T, Babidge W, Blamey S, et al. Rapid versus full systematic reviews: Validity in clinical practice?. ANZ J.2008; 1037–40. [DOI] [PubMed]
- Haby M.M., Chapman E., Clark R., Barreto J., Reveiz L., Lavis J.N. What are the best methodologies for rapid reviews of the research evidence for evidence-informed decision making in health policy and practice: A rapid review. Heal Res Policy Syst. 2016;14(1) doi: 10.1186/s12961-016-0155-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith R., Kelly B., Yeatman H., Boyland E. Food Marketing Influences Children’s Attitudes, Preferences and Consumption: A Systematic Critical Review. Nutrients. 2019;11(4):875. doi: 10.3390/nu11040875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly B., Vandevijvere S., Ng SeeHoe, Adams J., Allemandi L., Bahena‐Espina L., Barquera S., Boyland E., Calleja P., Carmona‐Garcés I.C., Castronuovo L., Cauchi D., Correa T., Corvalán C., Cosenza‐Quintana E.L., Fernández‐Escobar C., González‐Zapata L.I., Halford J., Jaichuen N., Jensen M.L., Karupaiah T., Kaur A., Kroker‐Lobos M.F., Mchiza Z., Miklavec K., Parker W.-a., Potvin Kent M., Pravst I., Ramírez‐Zea M., Reiff S., Reyes M., Royo‐Bordonada M.Á., Rueangsom P., Scarborough P., Tiscornia M.V., Tolentino‐Mayo L., Wate J., White M., Zamora‐Corrales I., Zeng L., Swinburn B. Global benchmarking of children’s exposure to television advertising of unhealthy foods and beverages across 22 countries. Obesity Reviews. 2019;20(S2):116–128. doi: 10.1111/obr.12840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ofcom. Children and parents: media use and attitudes report 2018. 2018. Available from: https://www.ofcom.org.uk/research-and-data/media-literacy-research/childrens/children-and-parents-media-use-and-attitudes-report-2018.
- Walsh JJ, Barnes JD, Tremblay MS, Chaput JP. Associations between duration and type of electronic screen use and cognition in US children. Computers in Human Behavior. Pergamon; 2020;108:106312.
- Statistics Canada. Physical activity and screen time among Canadian children and youth, 2016 and 2017. 2019. Available from: https://www150.statcan.gc.ca/n1/pub/82-625-x/2019001/article/00003-eng.htm.
- Ofcom. HFSS advertising restrictions Final Review Statement. 2010. Available from: https://www.ofcom.org.uk/research-and-data/tv-radio-and-on-demand/broadcast-advertising/hfss-final-review.
- Boyland EJ, Harrold JA, Kirkham TC, Halford JCG. The extent of food advertising to children on UK television in 2008. Int J Pediatr Obes. Int J Pediatr Obes. 2011;6:455–61. [DOI] [PubMed]
- Adams J., Tyrrell R., Adamson A.J., White M. Effect of Restrictions on Television Food Advertising to Children on Exposure to Advertisements for ‘Less Healthy’ Foods: Repeat Cross-Sectional Study. PLoS One. 2012;7 doi: 10.1371/journal.pone.0031578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyland E.J., Halford J.C.G. Television advertising and branding. Effects on eating behaviour and food preferences in children. Appetite. 2013:236–241. doi: 10.1016/j.appet.2012.01.032. [DOI] [PubMed] [Google Scholar]
- Pournaghi Azar F, Mamizadeh M, Nikniaz Z, Ghojazadeh M, Hajebrahimi S, salehnia F, et al. Content analysis of advertisements related to oral health in children: a systematic review and meta-analysis. Public Health. 2018;109–16. [DOI] [PubMed]
- British Heart Foundation. Millions of children exposed to junk food TV adverts. 2016. Available from: https://www.bhf.org.uk/what-we-do/news-from-the-bhf/news-archive/2016/january/millions-of-children-exposed-to-junk-food-adverts-during-family-tv-shows.
- Al-Mazyad M., Flannigan N., Burnside G., Higham S., Boyland E. Food advertisements on UK television popular with children: A content analysis in relation to dental health. Br Dent J. 2017;222:171–176. doi: 10.1038/sj.bdj.2017.120. [DOI] [PubMed] [Google Scholar]
- Sonntag D., Schneider S., Mdege N., Ali S., Schmidt B. Beyond Food Promotion: A Systematic Review on the Influence of the Food Industry on Obesity-Related Dietary Behaviour among Children. Nutrients. 2015;7:8565–8576. doi: 10.3390/nu7105414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qutteina Y., de Backer C., Smits T. Media food marketing and eating outcomes among pre-adolescents and adolescents: A systematic review and meta-analysis. Obesity Reviews. 2019;20:1708–1719. doi: 10.1111/obr.12929. [DOI] [PubMed] [Google Scholar]
- Kraak V.I., Story M. Influence of food companies’ brand mascots and entertainment companies’ cartoon media characters on children’s diet and health: a systematic review and research needs. Obes Rev. 2015;16:107–126. doi: 10.1111/obr.12237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman J., Kelly B., Boyland E. Evaluating the Evidence for a Causal Relationship. Curr. Nutr. Rep; The Impact of Marketing and Advertising on Food Behaviours: 2016. McMahon AT; pp. 139–149. [Google Scholar]
- Bradford Hill A. The Environment and Disease: Association or Causation? Proc R Soc Med. 1965;58:296. [PMC free article] [PubMed] [Google Scholar]
- Ronksley P.E., Brien S.E., Turner B.J., Mukamal K.J., Ghali W.A. Association of alcohol consumption with selected cardiovascular disease outcomes: A systematic review and meta-analysis. BMJ. 2011;342:479. doi: 10.1136/bmj.d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cresswell J.E., Desneux N., vanEngelsdorp D. Dietary traces of neonicotinoid pesticides as a cause of population declines in honey bees: an evaluation by Hill’s epidemiological criteria. Pest Manag Sci. 2012;68:819–827. doi: 10.1002/ps.3290. [DOI] [PubMed] [Google Scholar]
- Grant W.B. How strong is the evidence that solar ultraviolet B and vitamin D reduce the risk of cancer? An examination using Hill’s criteria for causality. Dermatoendocrinol. 2009;1:17–24. doi: 10.4161/derm.1.1.7388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly B., Freeman B., King L., Chapman K., Baur L.A., Gill T. Television advertising, not viewing, is associated with negative dietary patterns in children. Pediatr Obes. 2016;11:158–160. doi: 10.1111/ijpo.12057. [DOI] [PubMed] [Google Scholar]
- Norman J, Kelly B, Mcmahon A-T, Boyland E, Baur LA, Chapman K, et al. Sustained impact of energy-dense TV and online food advertising on children’s dietary intake: a within-subject, randomised, crossover, counter-balanced trial. Int J Behav Nutr Phys Act, 2019; s12966-018-0672-6. [DOI] [PMC free article] [PubMed]
- Marmot M., Allen J., Boyce T., Goldblatt P., Morrison J. Health Equity in England. The Marmot Review 10 Years On. 2020 doi: 10.1136/bmj.m693. https://www.health.org.uk/publications/reports/the-marmot-review-10-years-on Available from: [DOI] [PubMed] [Google Scholar]
- Backholer K, Gupta A, Zorbas C, Bennett R, Huse O, Chung A, et al. Differential exposure to, and potential impact of, unhealthy advertising to children by socio-economic and ethnic groups: A systematic review of the evidence. Obes. Rev. 2020; doi.org/10.1111/obr.13144. [DOI] [PubMed]
- Kunkel D., Mastro D., Ortiz M., McKinley C. Food marketing to children on U.S. Spanish-language television. J Health Commun. 2013;18:1084–1096. doi: 10.1080/10810730.2013.768732. [DOI] [PubMed] [Google Scholar]
- Bell R.A., Cassady D., Culp J., Alcalay R. Frequency and Types of Foods Advertised on Saturday Morning and Weekday Afternoon English- and Spanish-Language American Television Programs. J Nutr Educ Behav. 2009;41:406–413. doi: 10.1016/j.jneb.2008.05.008. [DOI] [PubMed] [Google Scholar]
- Adams J., Tyrrell R., Adamson A.J., White M. Socio-economic differences in exposure to television food advertisements in the UK: A cross-sectional study of advertisements broadcast in one television region. Public Health Nutr. 2012;15:487–494. doi: 10.1017/S1368980011001686. [DOI] [PubMed] [Google Scholar]
- Carter O.B.J. The weighty issue of Australian television food advertising and childhood obesity. Health Promot J Austr. 2006;17:5–11. doi: 10.1071/he06005. [DOI] [PubMed] [Google Scholar]
- Carter R., Moodie M., Markwick A., Magnus A., Vos T., Swinburn B., et al. Assessing Cost-Effectiveness in Obesity (ACE-Obesity): An overview of the ACE approach, economic methods and cost results. BMC Public Health. 2009;9:1–11. doi: 10.1186/1471-2458-9-419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gortmaker S.L., Wang Y.C., Long M.W., Giles C.M., Ward Z.J., Barrett J.L., et al. Three interventions that reduce childhood obesity are projected to save more than they cost to implement. Health Aff. 2015;34:1932–1939. doi: 10.1377/hlthaff.2015.0631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobstein T., Neveux M., Landon J. Costs, equity and acceptability of three policies to prevent obesity: A narrative review to support policy development. Obes Sci Pract. 2020;6:562–583. doi: 10.1002/osp4.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers S.A., Freeman R., Anderson A.S., Macgillivray S. Reducing the volume, exposure and negative impacts of advertising for foods high in fat, sugar and salt to children: A systematic review of the evidence from statutory and self-regulatory actions and educational measures. Prev Med. 2015;75:32–43. doi: 10.1016/j.ypmed.2015.02.011. [DOI] [PubMed] [Google Scholar]
- Galbraith-Emami S., Lobstein T. The impact of initiatives to limit the advertising of food and beverage products to children: a systematic review. Obes Rev. 2013;14:960–974. doi: 10.1111/obr.12060. [DOI] [PubMed] [Google Scholar]
- Elliott C., Truman E. The Power of Packaging: A Scoping Review and Assessment of Child-Targeted Food Packaging. Nutrients. 2020;12:958. doi: 10.3390/nu12040958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paes VM, Ong KK, Lakshman R. Factors influencing obesogenic dietary intake in young children (0-6 years): systematic review of qualitative evidence. BMJ Open. 2015;e007396. [DOI] [PMC free article] [PubMed]
- Harris JL, Yokum S, Fleming-Milici F. Hooked on Junk: Emerging Evidence on How Food Marketing Affects Adolescents’ Diets and Long-Term Health. Food Addiction. 2020;s40429.
- Interactive Advertising Bureau. Ad industry unites with joint letter to PM on HFSS. 2020. Available from: https://www.iabuk.com/news-article/ad-industry-unites-joint-letter-pm-hfss.
- Bruce A.S., Pruitt S.W., Ha O.R., Cherry J.B.C., Smith T.R., Bruce J.M., et al. The Influence of Televised Food Commercials on Children’s Food Choices: Evidence from Ventromedial Prefrontal Cortex Activations. J Pediatr. 2016;177:27–32. doi: 10.1016/j.jpeds.2016.06.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly B., Hebden L., King L., Xiao Y., Yu Y., He G., et al. Children’s exposure to food advertising on free-to-air television: an Asia-Pacific perspective. Health Promotion International. 2016;31:144–152. doi: 10.1093/heapro/dau055. [DOI] [PubMed] [Google Scholar]
- Swinburn B.A., Caterson I., Seidell J.C., James W.P.T. Diet, nutrition and the prevention of excess weight gain and obesity. Public Health Nutrition. 2004;7:123–146. doi: 10.1079/phn2003585. [DOI] [PubMed] [Google Scholar]
- Bramante C.T., Thornton R.L.J., Bennett W.L., Zhang A., Wilson R.F., Bass E.B., et al. Systematic Review of Natural Experiments for Childhood Obesity Prevention and Control. Am. J Prev Med. 2019:147–158. doi: 10.1016/j.amepre.2018.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biddle S.J.H., Bengoechea García E., Pedisic Z., Bennie J., Vergeer I., Wiesner G. Screen Time, Other Sedentary Behaviours, and Obesity Risk in Adults. A Review of Reviews. Curr Obes Rep. 2017:134–147. doi: 10.1007/s13679-017-0256-9. [DOI] [PubMed] [Google Scholar]
- Hemmingsson E. Early Childhood Obesity Risk Factors: Socioeconomic Adversity, Family Dysfunction, Offspring Distress, and Junk Food Self-Medication. Curr Obes Rep. 2018::204–209. doi: 10.1007/s13679-018-0310-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachucki M.C. Benefits of Incorporating a Lifecourse Perspective. Curr. Obes; Social Relationships and Obesity: 2015. Goodman E; pp. 217–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weihrauch-Blüher S., Kromeyer-Hauschild K., Graf C., Widhalm K., Korsten-Reck U., Jödicke B., et al. Current Guidelines for Obesity Prevention in Childhood and Adolescence. Obes Facts. 2018;11:263–276. doi: 10.1159/000486512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman PC, Murphy L, Nyman M, Oyebode O. Operationalising the EAT– Lancet Commissions’ targets to achieve healthy and sustainable diets. The Lancet Planetary Health. 2021;S2542519621001443. [DOI] [PubMed]
- Burki T.K. TV advertising and childhood obesity in the UK. Lancet Diabetes Endocrinol. 2018;6:604. [Google Scholar]
- Cancer Research UK. 10 Years on: New evidence on TV marketing and food consumption amongst 11-19 year olds 10 years after broadcast regulations. 2018. Available from: https://www.basw.co.uk/resources/10-years-new-evidence-tv-marketing-and-junk-food-eating-amongst-11-19-year-olds-10-years.
- Advertising Standards Authority. Remit: Advergames. 2016. Available from: https://www.asa.org.uk/advice-online/remit-advergames.html.
- Geoffrey R. Strategy of prevention: Lessons from cardiovascular disease. Br Med J. 1981;282:1847–51. [DOI] [PMC free article] [PubMed]
Further reading
- Swinburn B., Egger G., Raza F. Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Preventive medicine. 1999;29:563–570. doi: 10.1006/pmed.1999.0585. [DOI] [PubMed] [Google Scholar]