Autonomic sympathetic activation plays a key role in the pathophysiology of systemic hypertension and left ventricular hypertrophy. 1 , 2 As shown in the Symplicity HTN‐1 and HTN‐2 trials, percutaneous renal denervation (PRD) has proven to be an effective and safe method to treat patients with medically resistant hypertension and is considered to influence central sympathetic tone. 3 , 4 In patients after renal denervation, microneurography showed a gradual reduction in muscle sympathetic nerve activity in accordance with a modulation of central sympathetic tone. 2 The effect on cardiac autonomic tone is not known. Heart rate variability (HRV) is a marker of cardiac autonomic activity. 5 The present study assessed for the first time the effect of sympathetic renal denervation on heart rate dynamics in patients.
This prospective single‐center study was approved by the local ethics committee. All patients provided written informed consent. For inclusion, patients had to be older than 18 years with a systolic office blood pressure (BP) ≥150 mm Hg despite intake of ≥3 antihypertensive drugs, including one diuretic. Exclusion criteria were secondary causes of hypertension, reduced renal function (glomerular filtration rate <45 mL/min/1.73 m2), atrial fibrillation, pacemaker rhythm, and pregnancy. Patients with significant renal artery stenosis, abnormalities of renal artery anatomy, or a history of prior renal artery intervention were excluded from the study. Eligible patients had to document home BPs 3 times daily. Medication was maintained in all patients throughout follow‐up and changes were made only when symptomatic low BP occurred. In 14 patients, Holter electrocardiographic recordings were analyzed for time and frequency domain HRV parameters before and 3 months after percutaneous renal sympathetic denervation. Twenty‐four–hour electrocardiographic (ECG) recordings were performed using 3‐channel Holter recorders (LifeCard CF, Spacelabs; Delmar Reynolds, Hertford, UK) at a sampling rate of 1024 Hz. Office BP measurements were performed 1 month and 3 months after renal denervation.
One month and 3 months after renal denervation, office BPs were reduced by 16/4±6/5 mm Hg and 23/9±8/6 mm Hg (baseline of 170/94±18/14 mm Hg, P<.05). Three months after renal denervation, patients showed significantly higher values for mean RR interval (924±8.5 ms vs 957±8.9 ms; P<.01, mean±standard error of the mean), lower values for low‐frequency (LF) spectral component (398±30.1 ms2 vs 324±16.5 ms2; P<.05), LF normalized units (64±1.2 vs 60±1.1; P<.05), and lower values for LF/high‐frequency (HF) ratio (3.0±0.2 ms vs 2.6±0.1 ms; P<.05) as compared with baseline.
The Figure illustrates HRV spectral analyses from 24‐hour Holter‐ECG registrations in a patient undergoing PRD. Sympathetic cardiac autonomic tone dominates before renal denervation (top). After PRD, the LF spectral component was decreased and the HF spectral component was increased (bottom).
Figure FIGURE.
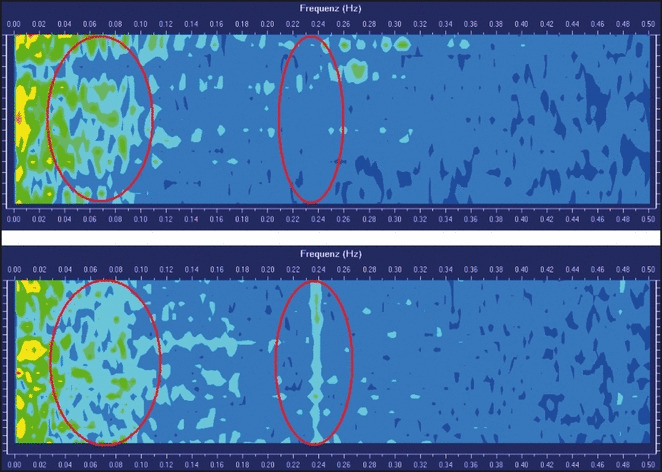
Heart rate variability spectral analyses from a 24‐h Holter‐electrocardiographic registration before (top) and 3 months after percutaneous renal denervation (bottom) in the same patient. Decrease of low‐frequency spectral component and increase of high‐frequency spectral component occurred after percutaneous renal denervation, reflecting decreased sympathetic cardiac tone.
PRD decreased office BP in medically resistant hypertension. Significant differences in cardiac autonomic tone were found before and after treatment. Heart rate dynamics were significantly improved in patients treated by catheter‐based renal denervation after 3 months.
Conclusions
Decreased cardiac sympathetic tone after renal denervation implies a beneficial effect on cardiac physiology in hypertensive patients, such as prevention of hypertrophy, and might diminish their cardiovascular risk. The evidence of attenuated cardiac sympathetic tone justifies future studies to quantify the protective effect of renal denervation on the heart.
References
- 1. Mahfoud F, Himmel F, Ukena C, et al. Treatment strategies for resistant arterial hypertension. Dtsch Arztebl Int. 2011;108:725–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Schlaich MP, Sobotka PA, Krum H, et al. Renal sympathetic‐nerve ablation for uncontrolled hypertension. N Engl J Med. 2009;361:932–934. [DOI] [PubMed] [Google Scholar]
- 3. Krum H, Schlaich M, Whitbourn R, et al. Catheter‐based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof‐of‐principle cohort study. Lancet. 2009;373:1275–1281. [DOI] [PubMed] [Google Scholar]
- 4. Symplicity HTN‐2 Investigators . Renal sympathetic denervation in patients with treatment‐resistant hypertension (The Symplicity HTN‐2 Trial): a randomised controlled trial. Lancet. 2010;376:1903–1909. [DOI] [PubMed] [Google Scholar]
- 5. Chakko S, Mulingtapang RF, Huikuri HV, et al. Alterations in heart rate variability and its circadian rhythm in hypertensive patients with left ventricular hypertrophy free of coronary artery disease. Am Heart J. 1993;126:1364–1372. [DOI] [PubMed] [Google Scholar]


