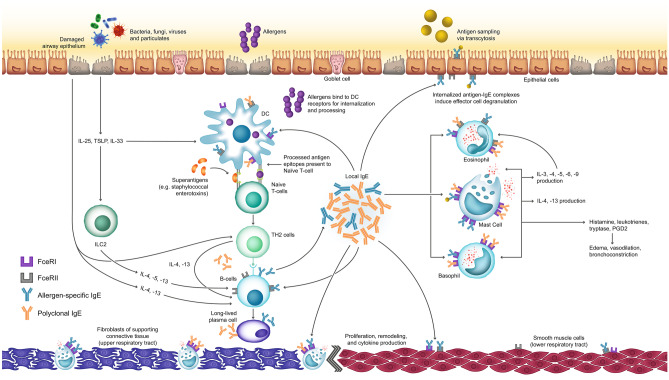
Fig. 1.
Mechanism of IgE-mediated upper and lower airway disease. In response to allergen exposure, dendritic cells present allergen-specific antigens to naïve T cells, which are activated and differentiate into Th2 cells. These Th2 cells produce key cytokines (IL-4, IL-13), prompting B cells to produce allergen-specific IgE. Alternatively, exposure to external stimuli such as bacteria, fungi, viruses, and particulates promotes epithelial release of IL-25, TSLP, and IL-33. These factors stimulate ILC2 cells to produce IL-5, IL-13, and to a lesser extent, IL-4, which in turn promote B cell production of IgE. Finally, superantigens, including Staphylococcal enterotoxins, can directly cross-link antigen-presenting cells with naïve T cells, bypassing the antigen presentation step, yielding polyclonal IgE. Once produced, local IgE acts on the FcεRI receptors of tissue-resident mast cells and basophils, prompting the release of histamine, leukotrienes, tryptase, and prostaglandin, which manifest as edema, vasodilation, and bronchoconstriction as part of the early response. IgE also binds to FcεRII receptors on B cells for enhanced antigen presentation. Later release of key cytokines recruits proinflammatory cells, including eosinophils and basophils, to the site of inflammation, and additionally promotes the overexpression of mucus-producing goblet cells and contributes to airway hyperresponsiveness. Crosstalk within the inflammatory pathway promotes a self-propagating cycle of chronic inflammation. The lower left side of the figure depicts the fibroblasts and mast cells within the supporting connective tissue of the nasal cavity, while the lower right side depicts the smooth muscle cell layer surrounding the lower respiratory airway. DC, dendritic cell; FcεRI, high-affinity immunoglobulin E receptor; FcεRII, low-affinity immunoglobulin E receptor; IgE, immunoglobulin E; IL, interleukin; ILC, innate lymphoid cell; PGD2, prostaglandin D2; Th2, T helper 2; TSLP, thymic stromal lymphopoietin