Abstract
Background
The coronavirus disease 2019 (COVID-19) outbreak had rapidly become a global health threat, and its impact on the mental health was transmitted among different populations, especially from parents to children. The study aimed to investigate Chinese parents’ influence on their children, in terms of mental health and lifestyles (screen time and physical exercise), during the COVID-19.
Methods
Self-reported online questionnaires of depression, anxiety, COVID-19 related worries, physical exercise, and screen time were completed by 3471 Chinese children and one of their parents (1514 fathers and 1957 mothers), during the COVID-19 epidemic in February 2020. Path analysis was used to examine the extent of transmission of psychological distress and whether lifestyles tied to transmission.
Results
During the quarantine, Chinese parents’ depression and anxiety both positively predicted their children's depression and anxiety; parents’ COVID-19 related worries, physical exercise and screen time separately had positive effects on children's COVID-19 related worries, physical exercise and screen time; parents’ depression and anxiety were positively influenced by their COVID-19 related worries, self-quarantine and quarantine of family members, relatives or friends; children's depression and anxiety positively predicted their non-suicidal self-injury and suicide ideation. Bootstrap analyses showed that parents’ COVID-19 related worries and lifestyles increased children's depression and anxiety via children's COVID-19 related worries and lifestyles, as well as parents’ depression and anxiety.
Conclusions
When families face to public events, parents’ psychological distress and lifestyles are related to children's psychological stress and lifestyles. Interventions of parents’ psychological distress and lifestyles would improve family resilience.
Keyword: COVID-19, parents, children, depression, anxiety, screen time, physical exercise
1. Introduction
As the largest outbreak of atypical pneumonia since the 2003 severe acute respiratory syndrome (SARS) outbreak, the coronavirus disease 2019 (COVID-19) outbreak had rapidly become a global health threat (Wang, Horby, Hayden, & Gao, 2020). Since the outbreak, the Chinese government has established an effective system for monitoring and responding to infectious diseases and implemented unprecedented strict quarantine measures, with schools and non-essential businesses at all levels closed indefinitely, in order to reduce further spread of the virus in China and other regions. Since January 31th, 2020, the date for the resumption of work and school has been repeatedly postponed. People had to stay at home in quarantine and there were significant changes in their daily life. However, it was suggested that the psychological impact of quarantine was extensive, substantial and long-term, and several negative psychological effects associated with quarantine had been proved, including depression, anxiety, post-traumatic stress, confusion, and anger (Brooks et al., 2020).
Due to the COVID-19 outbreak, parents had to cope with plenty of stressful factors, including financial losses, the need for basic supplies and reductions in social support outside the family, especially the fear of infection in themselves, families, friends and neighbors. A study on parents’ internalizing symptoms suggested that the fear of infection negatively affected psychological well-being of healthy adults (Crescentini et al., 2020). Moreover, many previous studies showed that the COVID-19 had a negative impact on parents’ mental health. A national survey in the US reported that 26.9% of parents faced with worsening of mental health during the outbreak (Patrick et al., 2020). Another study from the Netherlands found that parents who experienced higher stress levels showed stronger increases in negative feelings, including depression, anxiety, hostility, and sensitivity to interpersonal relationships, during COVID-19 lockdown (Achterberg, Dobbelaar, Boer, & Crone, 2021). However, there is a lack of research on major mental health problems, such as anxiety and depression, among Chinese parents during COVID-19. Besides, whether the quarantine state and worries about being infection have a direct impact on the mental health of Chinese parents during COVID-19 is worth studying.
With schools closed during the outbreak, children were asked to stay home and required to report their daily health status. Stressful factors such as frustration and boredom, fear of infection, lack of face-to-face contact with classmates and teachers, family financial losses and lack of personal space at home could have a more problematic and lasting impact on children (Wang, Zhang, Zhao, Zhang, & Jiang, 2020). It was demonstrated that the COVID-19 pandemic could lead to an increase in mental health problems among children (Golberstein, Wen, & Miller, 2020). In a sample of 8079 Chinese middle and high school students, the prevalence of depression symptoms, anxiety symptoms, and mixed symptoms of depression and anxiety was 43.7%, 37.4%, and 31.3%, respectively, during the COVID-19 outbreak (Zhou et al., 2020). Besides, children's ability to process information and regulate emotions was limited, and they could have serious self-injurious behavior and suicidal ideation due to depression and anxiety. There were suggestions that suicide rates would rise during the COVID-19 pandemic (Gunnell et al., 2020). Therefore, it is vital important to focus on the mental health of Chinese children during the COVID-19 and to study whether their depression and anxiety can lead to self-injury or suicidal ideation.
During the COVID-19 outbreak, parents and children stayed at home together almost every day and faced the myriad stresses of the epidemic. Therefore, parents’ perceptions of the epidemic and their psychological changes could have a direct influence on children through daily communication and behavior. Results from a study of Italian parents and their children showed that quarantine measures during the outbreak and changes in daily routine had a negative impact on parents’ psychological dimensions, thus exposing their children's mental health to a significant risk (Cusinato et al., 2020). As we already knew, both parents and children showed higher levels of depression and anxiety during the epidemic (Achterberg et al., 2021; Courtney, Watson, Battaglia, Mulsant, & Szatmari, 2020; Yue, Zang, Le, & An, 2020; Zhou et al., 2020). Similarly, parents’ depression and anxiety during the COVID-19 could have an effect on their children's depression and anxiety. A study conducted in Turkey proved that parents’ anxiety had a significant positive correlation with children's anxiety and predicted children's anxiety (Akgul & Ergin, 2021). However, the valuable topic of whether depression and anxiety in Chinese children are influenced by their parents’ depression and anxiety during the COVID-19 outbreak has not been studied.
In addition to mental health, the lifestyles of parents and children changed dramatically during the COVID-19 outbreak. At home, physical activities for both parents and children might be reduced due to space constraints. Besides, children were more dependent on social media and the Internet, and their screen time increased. Studies at home and abroad had confirmed that during the COVID-19 pandemic children's screen time increased and physical activity reduced (Francisco et al., 2020; Lau & Lee, 2020), which might negatively impact children's physical and mental health (Xiang, Zhang, & Kuwahara, 2020). Furthermore, with the interruption of daily schedules and activities, parents might rely on electronic devices to occupy children's time, and children's screen time could be greatly affected by their parents. A study among parents and their children in Guangdong, China found that the screen time of children was positively correlated with their parents’ screen time, types and habits (Hu, Johnson, & Wu, 2018). More studies that focus on the effect of parents’ physical exercise on children's physical exercise and the effect of parents’ screen time on children's screen time during the COVID-19 outbreak are needed.
For all we know, there is a lack of research examining parents’ influence on their children during the COVID-19 epidemic, especially in terms of mental health and lifestyles. The COVID-19 first broke out across China at extremely rapid rates, and China is the fastest country in the world to implement strict quarantine measures and establish an effective epidemic surveillance and prevention system. Therefore, it is meaningful and valuable to study the changes and connections between Chinese parents and their children in mental health and lifestyles during the quarantine. The present study aimed to investigate Chinese parents’ influence on their children, in terms of depression, anxiety, the COVID-19 related worries, physical exercise and screen time, during the COVID-19 outbreak. Besides, parents’ self-quarantine, quarantine of family members, relatives or friends, children's non-suicidal self-injury, children's suicidal ideation and other variables were also taken into account, exploring their effects on the mental health of parents and children.
2. Method
2.1. Sample
Sample data for this study were collected in Nanchang City, Jiangxi Province, during the COVID-19 epidemic in February 2020. Adjacent to Hubei Province, Jiangxi Province has a medium economic level in China, and Nanchang is about 260 km southeast of Wuhan. The participants were 3471 Grade 4 and above students from 4 schools in Lidu Town and Wengang Town and one of their parents. The four schools had a total of 7145 students in Grade 4 and above, and 4708 students participated in this survey. After matching with the parents’ data, 3471 pairs of data were used. In the children aged from 9 to 19 years (14.1±2.56), 51.6% were boys and 48.4% were girls. In the parents aged from 27 to 69 years (39.97±5.41), 43.6% were fathers and 56.4% were mothers. There were 44.3% urban residents and 55.7% rural residents. As for the education level of parents, 77.1% were primary or junior high school and only 22.9% were high school or above. Other demographics were shown in Table 1 .
Table 1.
Demographics and COVID-19 related worries.
| Parents | Children | |||
|---|---|---|---|---|
| Variables | n | % | n | % |
| Gender | ||||
| Male | 1514 | 43.6 | 1791 | 51.6 |
| Female | 1957 | 56.4 | 1680 | 48.4 |
| Location | ||||
| Rural | 1932 | 55.7 | 1932 | 55.7 |
| Urban | 1539 | 44.3 | 1539 | 44.3 |
| Education | ||||
| Primary or junior high school | 2673 | 77.1 | | |
| High school or above | 796 | 22.9 | | |
| Self-quarantine | ||||
| Yes | 333 | 9.6 | | |
| No | 3138 | 90.4 | | |
| Quarantine of relatives and friends | ||||
| Yes | 236 | 6.8 | | |
| No | 3235 | 93.2 | | |
| Worrying about yourself being infected with COVID-19 | ||||
| Not worry | 904 | 26.0 | 1299 | 37.4 |
| Worry | 1812 | 52.2 | 1639 | 47.2 |
| Very worry | 755 | 21.8 | 533 | 15.4 |
| Worrying about family members being infected with COVID-19 | ||||
| Not worry | 640 | 18.4 | 1007 | 29.0 |
| Worry | 1819 | 52.4 | 1759 | 50.7 |
| Very worry | 1012 | 29.2 | 705 | 20.3 |
| Worrying about neighborsbeing infected with COVID-19 | ||||
| Not worry | 644 | 18.6 | 1167 | 33.6 |
| Worry | 1871 | 53.9 | 1722 | 49.6 |
| Very worry | 956 | 27.5 | 582 | 16.8 |
| Mean | SD | Mean | SD | |
| Age, years | 39.97 | 5.41 | 14.1 | 2.56 |
2.2. Procedure
All children and parents finished a self-reported structured questionnaire online at certain times. Students from Lidu Town filled in questionnaires from February 18 to 28, 2020 and their parents filled in questionnaires from February 13 to 19, 2020. Students from Wengang Town completed questionnaires from February 18 to 28, 2020 and their parents completed questionnaires from February 4 to 10, 2020. At that time, the COVID-19 epidemic was serious in Jiangxi Province. On January 24, 2020, Jiangxi province launched a first-level public health response, ordering entertainment venues to close and implement closed management. The resumption of work and the opening of primary and secondary schools were postponed until at least February 29 and May 11, respectively. On February 4, 2020, the Health Commission of Jiangxi Province reported 548 confirmed cases in the province.
The electronic link of the questionnaire was sent in the wechat group by teachers, and the questionnaires were distributed through the Wenjuanxing platform (https://www.wjx.cn/). Electronic informed consent was provided and all parents and children were required to sign electronically. Children filled out questionnaires under parental supervision, and the questionnaire can only be submitted after it is completely filled out. The results of the first filling were selected, and the questionnaires whose filling time exceeds ±4 standard deviations were screened out. Furthermore, at the end of the questionnaire, access to online counseling was provided. The study was approved by the Ethics Committee of School of Psychology, Jiangxi Normal University (Nanchang, China), and Jinxian County Education and Sports Bureau provided permissions and support.
2.3. Measures
2.3.1. Sociodemographic variables
Sociedemographic information included parents’ gender, age, location, education and children's gender, age.
2.3.2. Depression symptoms
The Patient Health Questionnaire-9 (PHQ-9) was used to measure depression symptoms in the past two weeks (Kroenke, Spitzer, & Williams, 2001), which has good reliability and validity in the general Chinese population (Wang et al., 2014). The PHQ-9 contains 9 items and each item has four choices: 0 = not at all; 1 = several days; 2 = more than half the days; 3 = nearly every day. The total score can range from 0 to 27, with higher scores indicating more severe depression symptoms. A total score of 5 is suggested to screen clinical depression symptoms. The Cronbach's α in parent and children were 0.856 and 0.900 respectively.
2.3.3. Anxiety symptoms
The generalized anxiety disorder - 7 (GAD-7) was used to assess anxiety symptoms over the last two weeks (Spitzer, Kroenke, Williams, & Lowe, 2006), which was applicable in the Chinese population (Tong, An, McGonigal, Park, & Zhou, 2016). The GAD-7 contains 7 items and each item has four choices: 0 = not at all; 1 = several days; 2 = more than half the days; 3 = nearly every day. The total score can range from 0 to 21, with higher scores indicating more severe anxiety symptoms. A total score of 5 is suggested to screen anxiety symptoms. The Cronbach's α in parent and children were 0.896 and 0.915 respectively.
2.3.4. COVID-19 related worries
Participants’ COVID-19 related worries were measured by three items: “Are you worried about yourself being infected with COVID-19?”, “Are you worried about your family members being infected with COVID-19?” and “Are you worried about residents of your community or village being infected with COVID-19?”. Each item was rated on a three-point scale: 1 = not worry; 2 =worry; 3 = very worry. The total scores were calculated by adding up the three items. The Cronbach's α in parent and children were 0.839 and 0.863 respectively.
2.3.5. Screen time
Screen time was measured by asking participants to report how much time they spent on TV, computer use and cell phone/tablet use in the past half month. Each question has 4 choices: <1 h per day, 1–2 h per day, 3–5 h per day and ≥ 6 h per day, which are assigned values from 1 to 4. The total screen time was calculated by adding the three screen types.
2.3.6. Physical exercise
Physical exercise was measured by one item: “In the past half month, how many days per week did you spend on doing physical exercise?” There are 5 choices: null,<1 day per week,1–2 days per week, 3–4 days per week and 5–7 days per week, which are assigned values from 1 to 5.
2.3.7. Self-quarantine
Parents were required to report their current identity category to find out if they were currently in quarantine. They had five choices: 1 = confirmed, 2 = suspected, 3 = isolated in hospital, 4 = home isolation, 5 = normal people. The first four options were combined as “self-quarantine” and were assigned a value of 1. The last option was identified as “not self-quarantine” and was assigned a value of 0.
2.3.8. Quarantine of family members, relatives or friends
Parents were required to report whether their family members, relatives, or friends were under quarantine. There were three items: “Are your family members (living together) being infected with COVID-19?”, “Are your relatives (not living together) being infected with COVID-19?” and “Are your friends being infected with COVID-19?” Each item had five choices: 1 = confirmed; 2 = suspected; 3 = home isolation; 4 = normal people; 5 = unknown. The first three options were combined as “quarantine” and the last two options were combined as “no”. If there was an item with a value of 1, the sum was 1, and parents were considered to have family members, relatives or friends in quarantine.
2.3.9. Non-suicidal self-injury and suicidal ideation
Children's non-suicidal self-injury was assessed by one item: “In the past two weeks, have you intentionally hurt yourself, but not with the intention of killing yourself?” Children's suicidal ideation was assessed by one item: “In the past two weeks, have you had suicidal thoughts?” Each item has six choices: no, 1, 2, 3, 4, and 5 or more. The two variables were recorded into no (0) and ≥ 1 times (1).
2.4. Statistical analysis
First, demographic characteristics, COVID-19 related worries, frequency of physical activities, frequency of screen time and other study variables in this sample were calculated by descriptive statistical analysis. Second, the correlation relationship among study variables was provided by calculating Pearson correlation coefficient and Spearman's rank correlation coefficient. Additionally, a path analysis model was built to further examine correlations found and possible mediating effect among study variables. The bootstrap analysis was used to calculate indirect effect. Goodness of model fit was verified according to the literature guidance (Hu & Bentler, 1999): Comparative Fit Index (CFI) > 0.90; Tucker-Lewis Index (TLI) > 0.90; Root Mean Square Error of Approximation (RMSEA)< 0.08. Statistical analyses were conducted by using SPSS 23.0 and Mplus 7.0.
3. Results
Demographic characteristics and COVID-19 related worries of this sample were shown in Table 1. Of the 3471 parents, 9.6% were in self-quarantine, and 6.8% reported their family members, relatives or friends were in quarantine. The proportion of parents who were very worried about self, family members and neighbors being infected with COVID-19 was 21.8%, 29.2% and 27.5%, respectively. Less than parents, the children very worrying about self, family members and neighbors being infected with COVID-19 respectively accounted for 15.4%, 20.3% and 16.8%. In addition, the prevalence of depression and anxiety among parents was 13.7% and 12.8%, respectively, and in children, the proportion was 12.2% and 8.0%. Of the 3471 children, 2.0% had non-suicidal self-injurious behaviors and 3.3% had suicidal ideation during the past two weeks.
Table 2 displayed frequencies of physical activities and screen time among parents and children. As we can see, the proportion of parents and children spending 1–2 days per week on physical exercise was the highest, with 27.7% and 29.7%, respectively. Screen time for parents and children had a similar frequency distribution: 40.7% of parents and 44.3% of children watched TV for 1–2 h per day; 74.4% of parents and 65.7% of children spent less than 1 h per day on the computer; the percentage of using cell phone/tablet for 1–2 h per day among parents and children was 31.7% and 33.9%, respectively, and parents and children using 3–4 h per day on cell phone/tablet accounted for 33.3% and 31.5%.
Table 2.
Frequencies of physical activities and screen time.
| Parents | Children | |||
|---|---|---|---|---|
| Variables | n | % | n | % |
| Physical exercise | ||||
| Null | 717 | 20.7 | 410 | 11.8 |
| <1 day per week | 690 | 19.9 | 655 | 18.9 |
| 1–2 days per week | 961 | 27.7 | 1031 | 29.7 |
| 3–4 days per week | 652 | 18.8 | 787 | 22.7 |
| 5–7 days per week | 451 | 13.0 | 588 | 16.9 |
| Watching TV | ||||
| <1 hour per day | 923 | 26.6 | 1027 | 29.6 |
| 1–2 hours per day | 1412 | 40.7 | 1536 | 44.3 |
| 3–4 hours per day | 816 | 23.5 | 713 | 20.5 |
| ≥6 hours per day | 320 | 9.2 | 195 | 5.6 |
| Using computers | ||||
| <1 hour per day | 2581 | 74.4 | 2279 | 65.7 |
| 1–2 hours per day | 563 | 16.2 | 757 | 21.8 |
| 3–4 hours per day | 223 | 6.4 | 323 | 9.3 |
| ≥6 hours per day | 104 | 3.0 | 112 | 3.2 |
| Using cell phone/tablet | ||||
| <1 hour per day | 556 | 16.0 | 768 | 22.1 |
| 1–2 hours per day | 1101 | 31.7 | 1175 | 33.9 |
| 3–4 hours per day | 1156 | 33.3 | 1092 | 31.5 |
| ≥6 hours per day | 658 | 19.0 | 436 | 12.6 |
Means, SD, and correlations of studied variables were reported in Table 3 . When the correlation coefficient is greater than or equal to 0.03, the correlation is significant. As shown, parents’ depression and anxiety were both significantly associated with their children's depression and anxiety. The correlation relationships between parents and children on COVID-19 related worries, physical exercise and screen time were all significant. Furthermore, parents’ depression was significantly related to their anxiety, as the same finding among children. It was demonstrated that children with depression or anxiety were more likely to have non-suicidal self-injurious behaviors and suicidal ideation. Children's non-suicidal self-injury was significantly correlated to their suicidal ideation.
Table 3.
Means, SD, and correlations of studied variables.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 Sex (parents) | 1.00 | |||||||||||||||||
| 2 Education (parents) | -0.09 | 1.00 | ||||||||||||||||
| 3 Self-quarantine (parents) | 0.00 | -0.03 | 1.00 | |||||||||||||||
| 4 Quarantine of relatives and friends (parents) | -0.05 | 0.01 | 0.18 | 1.00 | ||||||||||||||
| 5 COVID-19 related worries (parents) | -0.04 | 0.02 | 0.07 | 0.09 | 1.00 | |||||||||||||
| 6 Physical exercise (parents) | 0.03 | 0.05 | 0.01 | -0.01 | -0.03 | 1.00 | ||||||||||||
| 7 Screen time (parents) | -0.03 | 0.07 | 0.00 | -0.01 | 0.03 | 0.04 | 1.00 | |||||||||||
| 8 Depression (parents) | -0.01 | -0.00 | 0.08 | 0.12 | 0.12 | -0.05 | 0.13 | 1.00 | ||||||||||
| 9 Anxiety (parents) | 0.04 | -0.01 | 0.09 | 0.10 | 0.19 | -0.03 | 0.09 | 0.68 | 1.00 | |||||||||
| 10 Sex (children) | 0.05 | -0.04 | -0.02 | -0.00 | 0.01 | -0.02 | -0.02 | 0.01 | -0.00 | 1.00 | ||||||||
| 11 Age (children) | -0.10 | -0.03 | 0.04 | 0.08 | -0.02 | 0.08 | -0.04 | 0.05 | 0.01 | 0.01 | 1.00 | |||||||
| 12 COVID-19 related worries (children) | -0.00 | -0.03 | 0.04 | 0.05 | 0.46 | -0.06 | 0.01 | 0.06 | 0.13 | 0.03 | -0.10 | 1.00 | ||||||
| 13 Physical exercise (children) | 0.02 | 0.09 | 0.00 | -0.02 | -0.01 | 0.36 | 0.04 | -0.06 | -0.03 | -0.06 | 0.04 | -0.02 | 1.00 | |||||
| 14 Screen time (children) | -0.01 | 0.02 | 0.04 | 0.02 | 0.00 | 0.04 | 0.29 | 0.08 | 0.06 | -0.05 | 0.09 | 0.00 | 0.06 | 1.00 | ||||
| 15 Depression (children) | -0.00 | -0.01 | 0.08 | 0.11 | 0.05 | -0.00 | 0.04 | 0.29 | 0.27 | 0.02 | 0.25 | 0.09 | -0.02 | 0.14 | 1.00 | |||
| 16 Anxiety (children) | 0.01 | -0.02 | 0.07 | 0.08 | 0.07 | -0.04 | 0.02 | 0.28 | 0.32 | 0.02 | 0.15 | 0.14 | -0.03 | 0.10 | 0.77 | 1.00 | ||
| 17 Non-suicidal self-injury (children) | 0.01 | -0.04 | 0.04 | 0.07 | 0.04 | -0.00 | -0.01 | 0.07 | 0.07 | 0.01 | 0.03 | 0.07 | -0.03 | 0.06 | 0.28 | 0.28 | 1.00 | |
| 18 Suicidal ideation (children) | 0.01 | -0.01 | 0.06 | 0.08 | 0.03 | -0.01 | 0.00 | 0.06 | 0.05 | 0.04 | 0.05 | 0.04 | -0.04 | 0.07 | 0.34 | 0.31 | 0.57 | 1.00 |
| Mean | 0.56 | 0.23 | 0.10 | 0.07 | 6.15 | 0.32 | 6.09 | 1.82 | 1.54 | 0.48 | 14.10 | 5.52 | 0.40 | 5.87 | 1.44 | 0.89 | 0.02 | 0.03 |
| SD | 0.50 | 0.42 | 0.30 | 0.25 | 1.78 | 0.47 | 1.82 | 2.95 | 2.69 | 0.50 | 2.56 | 1.84 | 0.49 | 1.75 | 2.87 | 2.19 | 0.14 | 0.18 |
Note: Absolute value of correlation coefficient ≥ 0.03, p<0.05.
Sex (parents): 0 = male 1 = female; sex (children): 0 = male 1 = female.
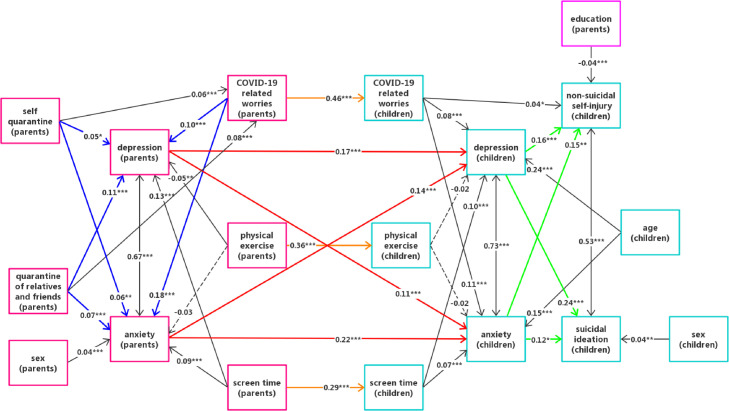
Fig. 1 showed the best fitting model that produced the following fitting indices: χ2 = 273.035, df = 87, RMSEA = 0.025, CFI = 0.981, TLI = 0. 973. In this figure, the significant main paths were represented by colorful solid lines. As shown, parents’ depression and anxiety both positively predicted their children's depression and anxiety levels. Parents’ COVID-19 related worries, physical exercise and screen time separately had positive effects on children's COVID-19 related worries, physical exercise and screen time. In addition, parents’ depression and anxiety were positively influenced by their COVID-19 related worries, self-quarantine and quarantine of family members, relatives or friends. Children's depression and anxiety positively predicted their non-suicidal self-injury and suicide ideation. Other significant relationships were shown in this figure.
Fig. 1.
path analysis.
Bootstrap analysis results of indirect effects were revealed in appendix. Parents’ screen time, COVID-19 related worries, self-quarantine, quarantine of family members, relatives or friends all had significant indirect effects on their children's depression and anxiety. Furthermore, the indirect effects of parents’ depression and anxiety on children's non-suicidal self-injury and suicide ideation were also significant.
4. Discussion
This study was the first to investigate Chinese parents’ influence on their children, in terms of mental health and lifestyles, during the COVID-19 epidemic. Parents and children used the same questionnaire and separately reported their symptoms, reducing report bias. The influence of Chinese parents on their children during the COVID-19 was clearly demonstrated for the first time: parents’ depression and anxiety both positively predicted their children's depression and anxiety; parents’ COVID-19 related worries, physical exercise and screen time separately positively predicted their children's COVID-19 related worries, physical exercise and screen time. In addition, our findings confirmed the indirect effects of parents’ COVID-19 related worries and lifestyles on children's depression and anxiety for the first time.
The proportion of parents who were worried and very worried about self, family members and neighbors being infected with COVID-19 was higher than that of their children, which suggested that parents had higher levels of COVID-19 related worries. The reason for this phenomenon might be that parents got more information from the outside world than their children, took on the family's financial pressure and the responsibility of raising children, and thus felt more psychological pressure. Compared to worrying or very worrying about themselves, more parents and children worried or very worried about family members and neighbors being infected with COVID-19, which was consistent with the fact that Chinese people were more considerate of others. Moreover, in this study, during the outbreak, the prevalence of depression and anxiety during past two weeks among children was 12.2% and 8.0%, respectively. An online survey conducted after lockdown in Chinese children and adolescents (Liu et al., 2021) showed that 12.33% and 6.26% of participants reported depression and anxiety, separately, which was similar to our results. Higher than children, the prevalence of depression and anxiety among parents during the epidemic was 13.7% and 12.8%, respectively, conforming to higher levels of COVID-19 related worries in parents.
This study proved that Chinese parents’ depression and anxiety were directly and positively influenced by epidemic-related variables, including their COVID-19 related worries, self-quarantine and quarantine of family members, relatives or friends, consistent with several studies during epidemics (Crescentini et al., 2020; Mazza et al., 2020). It was demonstrated that during the COVID-19 outbreak, Chinese children's depression and anxiety positively predicted their non-suicidal self-injury and suicide ideation, which was confirmed by many previous studies (Balazs et al., 2013; Claes, Luyckx, & Bijttebier, 2014; Hill, Castellanos, & Pettit, 2011). Furthermore, the transition of psychological distress and lifestyles from Chinese parents to children during COVID-19 would be elaborated in the following.
This study was the first to show clear evidence that during the COVID-19 outbreak, Chinese parents’ depression and anxiety both positively predicted their children's depression and anxiety. Parents’ depression and anxiety were associated with increased risk for depression and anxiety in offspring, which was confirmed by a large number of previous studies (Aktar, Nikolic, & Bogels, 2017; Biederman et al., 2001; Chang & Fu, 2020; Eley et al., 2015; Leis & Mendelson, 2010; Liu, Li, Zheng, & Wang, 2021). Although there was consistent evidence that anxiety and depression had shared genetic liability (Kendler, Gardner, & Lichtenstein, 2008), it was proved that intergenerational transmission of depression and anxiety was partly due to environmental mechanisms (Eley et al., 2015; Lewis, Rice, Harold, Collishaw, & Thapar, 2011), such as negative rearing environment and negative parenting behavior (Goodman, 2020; Hammen, Shih, & Brennan, 2004), imitating parents’ behavior (Eley et al., 2015), presenting non-verbal signals and communicating threatening information (Aktar et al., 2017), transmitting cognitive styles (Liu et al., 2021) and so on. To make matters worse, the ongoing crisis and long-term quarantine made depressed and anxious parents have higher levels of psychological stress, resulting in long-term problematic parenting behaviors (Prime, Wade, & Browne, 2020), which might lead to an escalation of negative relationships between parents and children and exacerbate negative impacts on children's mental health.
It was confirmed that during the COVID-19 epidemic, Chinese parents’ COVID-19 related worries, physical exercise and screen time separately positively predicted their children's COVID-19 related worries, physical exercise and screen time. Parents’ fears and worries about infection might be transmitted to their children mainly through daily conversation and emotional expressions. Lots of previous studies proved that parents’ physical activities positively associated with children's physical activities (Hinkley, Crawford, Salmon, Okely, & Hesketh, 2008), and parents’ screen time also positively associated with children's screen time (Cillero & Jago, 2010; Duch, Fisher, Ensari, & Harrington, 2013; Hu et al., 2018). These could be attributed to parents’ role modeling and encouragement (Dwyer, Higgs, Hardy, & Baur, 2008; Garriguet, Colley, & Bushnik, 2017). In addition, a review found that increasing parents’ self-efficacy and improving parenting styles might be effective ways to reduce children's screen time (Xu, Wen, & Rissel, 2015). If parents spend plenty of time on electronic entertainment instead of working or taking care of their children, during the COVID-19, this could mean they have a lower self-efficacy and a negative parenting style, leading to an increase in their children's screen time.
Our findings showed that screen time was a positive predictor of depression and anxiety for both Chinese parents and their children, during the COVID-19 epidemic. A study among Chinese children and adolescents also demonstrated that prolonged screen time might negatively influence children's mental health during the COVID-19 pandemic (Xiang et al., 2020). This result might be due to too much media exposure. Studies proved that during the outbreak, people relied more on the media for up-to-date information, and excessive media use, especially exposure to disaster news, could lead to depression and anxiety (Garfin, Silver, & Holman, 2020; Zhao & Zhou, 2020). Furthermore, this study confirmed that during the COVID-19, Chinese parents’ screen time had significant indirect effects on their children's depression and anxiety via parents’ depression, anxiety, and children's screen time, which further suggested that parents had to consciously limit their screen time and maintain a healthy lifestyle, for the sake of their children's mental health.
4.1. Implications
Our findings identified complex dynamic transitions of psychological distress and lifestyles exist in family when face to public events and we determined several risk factors affecting the mental health of parents and their children. The results suggest that parents should first ensure their own positive attitude in dealing with the epidemic, take care of their children's mental health and pay attention to their influence on their children, avoiding harm and adverse consequences as much as possible. These results also can be used to guide psychological interventions and to develop targeted preventive measures to improve the mental health of parents and children during epidemics. Furthermore, interventions of parents’ psychological stress and lifestyles would improve family resilience, which could help family better cope with large public events and emergencies.
4.2. Limitation
There are several limitations that should be noticed. First, cross-sectional data were used in this study, so causal inferences could not be made. Second, only one parent completed the survey, the potential differences on the effects of mothers’ or fathers’ psychological distress and lifestyles on their children could not be explored in the same family system. Third, PHQ-9 has not been used in children aged 9, and some variables such as physical exercise were study-developed. Therefore, the validity of these variables are unclear. Fourth, this study was conducted in February 2020, during the COVID-19 outbreak; the long-term impact of the epidemic is unknown. Furthermore, common environmental factors for children and parents (e.g. COVID-19 related stressors) were not assessed. In the final, the participants were mainly ordinary people in rural areas, and there was a lack of urban population data and data on confirmed patients or medical personnel. Future longitudinal studies should focus on parents’ influence on their children, in terms of various mental health problems and lifestyles, after long-term quarantine.
Funding
The present study was funded by National Natural Science Foundation of China (grant numbers: 31,700,987). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author statement contributors
FLG designed the study. NLZ and JQZ collected the data. YQZ, FLG, and NLZ performed data analysis. YQZ and FLG drafted the manuscript. DJX and MFL commented the manuscript. All authors provided critical revision of the manuscript.
Role of the funding source
The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Declaration of Competing Interest
No.
Acknowledgments
The present study was funded by National Natural Science Foundation of China (grant numbers: 31700987).
Appendix
Bootstrap analysis of indirect effects
| Bootstrapping(95%CI) | |||
|---|---|---|---|
| Effect | Lower 2.5% | Upper 2.5% | |
| Total indirect effects from PST to DEP | 0.064 | 0.046 | 0.081 |
| DEP-PDEP-PST | 0.021 | 0.012 | 0.032 |
| DEP-PANX-PST | 0.012 | 0.006 | 0.020 |
| DEP-ST-PST | 0.030 | 0.017 | 0.043 |
| Total indirect effects from PCOVSUB to DEP | 0.079 | 0.061 | 0.099 |
| DEP-PDEP-PCOVSUB | 0.017 | 0.009 | 0.027 |
| DEP-PANX-PCOVSUB | 0.024 | 0.013 | 0.036 |
| DEP-COVSUB-PCOVSUB | 0.038 | 0.023 | 0.053 |
| Total indirect effects from SELF to DEP | 0.021 | 0.009 | 0.036 |
| DEP-PDEP-SELF | 0.008 | 0.002 | 0.018 |
| DEP-PANX-SELF | 0.008 | 0.003 | 0.016 |
| DEP-PDEP-PCOVSUB-SELF | 0.001 | 0.000 | 0.002 |
| DEP-PANX-PCOVSUB-SELF | 0.001 | 0.001 | 0.003 |
| DEP-COVSUB-PCOVSUB-SELF | 0.002 | 0.001 | 0.004 |
| Total indirect effects from OTHER to DEP | 0.034 | 0.022 | 0.048 |
| DEP-PDEP-OTHER | 0.018 | 0.009 | 0.028 |
| DEP-PANX-OTHER | 0.010 | 0.004 | 0.018 |
| DEP-PDEP-PCOVSUB-OTHER | 0.001 | 0.001 | 0.002 |
| DEP-PANX-PCOVSUB-OTHER | 0.002 | 0.001 | 0.003 |
| DEP-COVSUB-PCOVSUB-OTHER | 0.003 | 0.001 | 0.005 |
| Total indirect effects from PST to ANX | 0.052 | 0.035 | 0.069 |
| ANX-PDEP-PST | 0.014 | 0.006 | 0.023 |
| ANX-PANX-PST | 0.019 | 0.010 | 0.030 |
| ANX-ST-PST | 0.019 | 0.008 | 0.031 |
| Total indirect effects from PCOVSUB to ANX | 0.101 | 0.082 | 0.120 |
| ANX-PDEP-PCOVSUB | 0.012 | 0.004 | 0.020 |
| ANX-PANX-PCOVSUB | 0.038 | 0.025 | 0.053 |
| ANX-COVSUB-PCOVSUB | 0.052 | 0.038 | 0.065 |
| Total indirect effects from SELF to ANX | 0.025 | 0.012 | 0.040 |
| ANX-PDEP-SELF | 0.006 | 0.001 | 0.013 |
| ANX-PANX-SELF | 0.013 | 0.004 | 0.024 |
| ANX-PDEP-PCOVSUB-SELF | 0.001 | 0.000 | 0.001 |
| ANX-PANX-PCOVSUB-SELF | 0.002 | 0.001 | 0.004 |
| ANX-COVSUB-PCOVSUB-SELF | 0.003 | 0.001 | 0.005 |
| Total indirect effects from OTHER to ANX | 0.036 | 0.022 | 0.051 |
| ANX-PDEP-OTHER | 0.012 | 0.004 | 0.021 |
| ANX-PANX-OTHER | 0.016 | 0.007 | 0.028 |
| ANX-PDEP-PCOVSUB-OTHER | 0.001 | 0.000 | 0.002 |
| ANX-PANX-PCOVSUB-OTHER | 0.003 | 0.002 | 0.005 |
| ANX-COVSUB-PCOVSUB-OTHER | 0.004 | 0.002 | 0.006 |
| Total indirect effects from PDEP to INJURY | 0.044 | 0.023 | 0.066 |
| INJURY-DEP-PDEP | 0.027 | 0.010 | 0.048 |
| INJURY-ANX-PDEP | 0.017 | 0.003 | 0.035 |
| Total indirect effects from PANX to INJURY | 0.055 | 0.033 | 0.079 |
| INJURY-DEP-PANX | 0.022 | 0.008 | 0.040 |
| INJURY-ANX-PANX | 0.033 | 0.009 | 0.058 |
| Total indirect effects from PDEP to SUICIDE | 0.054 | 0.030 | 0.081 |
| SUICIDE-DEP-PDEP | 0.041 | 0.021 | 0.065 |
| SUICIDE-ANX-PDEP | 0.014 | 0.002 | 0.030 |
| Total indirect effects from PANX to SUICIDE | 0.060 | 0.037 | 0.084 |
| SUICIDE-DEP-PANX | 0.033 | 0.017 | 0.053 |
| SUICIDE-ANX-PANX | 0.026 | 0.005 | 0.049 |
DEP-Depression (children) PDEP-Depression (parents)
ANX-Anxiety (children) PANX-Anxiety (parents)
ST-Screen time (children) PST-Screen time (parents)
COVSUB-COVID-19 related worries (children)
PCOVSUB-COVID-19 related worries (parents)
SELF-Self-quarantine (parents)
OTHER-Quarantine of relatives and friends (parents)
INJURY-Non-suicidal self-injury (children)
SUICIDE-Suicidal ideation (children)
Reference
- Achterberg M., Dobbelaar S., Boer O.D., Crone E.A. Perceived stress as mediator for longitudinal effects of the COVID-19 lockdown on wellbeing of parents and children. Sci. Rep. 2021;11(1):2971. doi: 10.1038/s41598-021-81720-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akgul G., Ergin D.A. Adolescents’ and parents’ anxiety during COVID-19–Is there a role of cyberchondriasis and emotion regulation through the internet? Curr. Psychol. 2021;40:4750–4759. doi: 10.1007/s12144-020-01229-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aktar E., Nikolic M., Bogels S.M. Environmental transmission of generalized anxiety disorder from parents to children–Worries, experiential avoidance, and intolerance of uncertainty. Dialogues Clin. Neurosci. 2017;19(2):137–146. doi: 10.31887/DCNS.2017.19.2/eaktar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balazs J., Miklosi M., Kereszteny A., Hoven C.W., Carli V., Wasserman C., …, Wasserman D. Adolescent subthreshold-depression and anxiety–Psychopathology, functional impairment and increased suicide risk. J. Child Psychol. Psychiatry. 2013;54(6):670–677. doi: 10.1111/jcpp.12016. [DOI] [PubMed] [Google Scholar]
- Biederman J., Faraone S.V., Hirshfeld-Becker D.R., Friedman D., Robin J.A., Rosenbaum J.F. Patterns of psychopathology and dysfunction in high-risk children of parents with panic disorder and major depression. Am. J. Psychiatry. 2001;158(1):49–57. doi: 10.1176/appi.ajp.158.1.49. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it–Rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang L.Y., Fu M.C. Disentangling the effects of intergenerational transmission of depression from adolescence to adulthood–The protective role of self-esteem. Eur. Child Adolesc. Psychiatry. 2020;29(5):679–689. doi: 10.1007/s00787-019-01390-w. [DOI] [PubMed] [Google Scholar]
- Cillero I.H., Jago R. Systematic review of correlates of screen-viewing among young children. Prev. Med. 2010;51(1):3–10. doi: 10.1016/j.ypmed.2010.04.012. [DOI] [PubMed] [Google Scholar]
- Claes L., Luyckx K., Bijttebier P. Non-suicidal self-injury in adolescents–Prevalence and associations with identity formation above and beyond depression. Personal. Individ. Differ. 2014;61-62:101–104. doi: 10.1016/j.paid.2013.12.019. [DOI] [Google Scholar]
- Courtney D., Watson P., Battaglia M., Mulsant B.H., Szatmari P. COVID-19 impacts on child and youth anxiety and depression–Challenges and opportunities. Can. J. Psychiatry. 2020;65(10):688–691. doi: 10.1177/0706743720935646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crescentini C., Feruglio S., Matiz A., Paschetto A., Vidal E., Cogo P., Fabbro F. Stuck outside and inside–An exploratory study on the effects of the COVID-19 outbreak on italian parents and children's internalizing symptoms. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.586074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cusinato M., Iannattone S., Spoto A., Poli M., Moretti C., Gatta M., Miscioscia M. Stress, resilience, and well-being in italian children and their parents during the COVID-19 pandemic. Int. J. Environ. Res. Public Health. 2020;17(22):8297. doi: 10.3390/ijerph17228297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duch H., Fisher E.M., Ensari I., Harrington A. Screen time use in children under 3 years old–A systematic review of correlates. Int. J. Behav. Nutr. Phys. Act. 2013;10:102. doi: 10.1186/1479-5868-10-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwyer G.M., Higgs J., Hardy L.L., Baur L.A. What do parents and preschool staff tells us about young children’s physical activity–A qualitative study. Int. J. Behav. Nutr. Phys. Act. 2008;5:66. doi: 10.1186/1479-5868-5-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eley T.C., McAdams T.A., Rijsdijk F.V., Lichtenstein P., Narusyte J., Reiss D., Neiderhiser J.M. The intergenerational transmission of anxiety–A children-of-twins study. Am. J. Psychiatry. 2015;172(7):630–637. doi: 10.1176/appi.ajp.2015.14070818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francisco R., Pedro M., Delvecchio E., Espada J.P., Morales A., Mazzeschi C., Orgiles M. Psychological symptoms and behavioral changes in children and adolescents during the early phase of COVID-19 quarantine in three European countries. Front. Psychiatry. 2020;11:570164. doi: 10.3389/fpsyt.2020.570164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfin D.R., Silver R.C., Holman E.A. The novel coronavirus (COVID-2019) outbreak–Amplification of public health consequences by media exposure. Health Psychol. 2020;39(5):355–357. doi: 10.1037/hea0000875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garriguet D., Colley R., Bushnik T. Parent-Child association in physical activity and sedentary behaviour. Health Rep. 2017;28(6):3–11. [PubMed] [Google Scholar]
- Golberstein E., Wen H.F., Miller B.F. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatrics. 2020;174(9):819–820. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- Goodman S.H. Intergenerational transmission of depression. Annu. Rev. Clin. Psychol. 2020;16:213–238. doi: 10.1146/annurev-clinpsy-071519-113915. 2020. [DOI] [PubMed] [Google Scholar]
- Gunnell D., Appleby L., Arensman E., Hawton K., John A., Kapur N., …, Co C.-S.P.R. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7(6):468–471. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C., Shih J.H., Brennan P.A. Intergenerational transmission of depression–Test of an interpersonal stress model in a community sample. J. Consult. Clin. Psychol. 2004;72(3):511–522. doi: 10.1037/0022-006x.72.3.511. [DOI] [PubMed] [Google Scholar]
- Hill R.M., Castellanos D., Pettit J.W. Suicide-related behaviors and anxiety in children and adolescents–A review. Clin. Psychol. Rev. 2011;31(7):1133–1144. doi: 10.1016/j.cpr.2011.07.008. [DOI] [PubMed] [Google Scholar]
- Hinkley T., Crawford D., Salmon J., Okely A.D., Hesketh K. Preschool children and physical activity–A review of correlates. Am. J. Prev. Med. 2008;34(5):435–441. doi: 10.1016/j.amepre.2008.02.001. [DOI] [PubMed] [Google Scholar]
- Hu B.Y., Johnson G.K., Wu H.P. Screen time relationship of Chinese parents and their children. Child. Youth Serv. Rev. 2018;94:659–669. doi: 10.1016/j.childyouth.2018.09.008. [DOI] [Google Scholar]
- Hu, L. t., & Bentler, P.M. 1999. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Modeling 6(1), 1–55. doi:10.1080/10705519909540118.
- Kendler K.S., Gardner C.O., Lichtenstein P. A developmental twin study of symptoms of anxiety and depression–Evidence for genetic innovation and attenuation. Psychol. Med. 2008;38(11):1567–1575. doi: 10.1017/S003329170800384x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9–Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau E.Y.H., Lee K. Parents’ views on young children’s distance learning and screen time during COVID-19 class suspension in Hong Kong. Early Educ. Dev. 2020;32(6):863–880. doi: 10.1080/10409289.2020.1843925. [DOI] [Google Scholar]
- Leis J.A., Mendelson T. Intergenerational transmission of psychopathology minor versus major parental depression. J. Nerv. Ment. Dis. 2010;198(5):356–361. doi: 10.1097/NMD.0b013e3181da8514. [DOI] [PubMed] [Google Scholar]
- Lewis G., Rice F., Harold G.T., Collishaw S., Thapar A. Investigating environmental links between parent depression and child depressive/anxiety symptoms using an assisted conception design. J. Am. Acad. Child Adolesc. Psychiatry. 2011;50(5):451–459. doi: 10.1016/j.jaac.2011.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L., Li S., Zheng Y., Wang M.F. Intergenerational transmission of anxiety in Chinese migrant families–The mediating role of parents' perceptions of coparenting. J. Affect. Disord. 2021;280:287–294. doi: 10.1016/j.jad.2020.10.069. [DOI] [PubMed] [Google Scholar]
- Liu Y., Yue S., Hu X.R., Zhu J., Wu Z.F., Wang J.L., Wu Y.L. Associations between feelings/behaviors during COVID-19 pandemic lockdown and depression/anxiety after lockdown in a sample of Chinese children and adolescents. J. Affect. Disord. 2021;284:98–103. doi: 10.1016/j.jad.2021.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., Roma P. A nationwide survey of psychological distress among italian people during the COVID-19 pandemic–Immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health. 2020;17(9):3165. doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick S.W., Henkhaus L.E., Zickafoose J.S., Lovell K., Halvorson A., Loch S., …, Davis M.M. Well-being of Parents and Children During the COVID-19 Pandemic–A National Survey. Pediatrics. 2020;146(4):2020016824. doi: 10.1542/peds.2020-016824. [DOI] [PubMed] [Google Scholar]
- Prime H., Wade M., Browne D.T. Risk and resilience in family well-being during the COVID-19 pandemic. Am. Psychol. 2020;75(5):631–643. doi: 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Lowe B. A brief measure for assessing generalized anxiety disorder - The GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Tong X., An D.M., McGonigal A., Park S.P., Zhou D. Validation of the generalized anxiety disorder-7 (GAD-7) among Chinese people with epilepsy. Epilepsy Res. 2016;120:31–36. doi: 10.1016/j.eplepsyres.2015.11.019. [DOI] [PubMed] [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern (vol 395, pg 470, 2020) Lancet. 2020;395(10223) doi: 10.1016/S0140-6736(20)30250-6. 496-496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang G.H., Zhang Y.T., Zhao J., Zhang J., Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395(10228):945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W.Z., Bian Q., Zhao Y., Li X., Wang W.W., Du J., …, Zhao M. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatry. 2014;36(5):539–544. doi: 10.1016/j.genhosppsych.2014.05.021. [DOI] [PubMed] [Google Scholar]
- Xiang M., Zhang Z.R., Kuwahara K. Impact of COVID-19 pandemic on children and adolescents' lifestyle behavior larger than expected. Prog. Cardiovasc. Dis. 2020;63(4):531–532. doi: 10.1016/j.pcad.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu H.L., Wen L.M., Rissel C. Associations of parental influences with physical activity and screen time among young children–A systematic review. J. Obes. 2015;2015:546925. doi: 10.1155/2015/546925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yue J.M., Zang X.Y., Le Y.Y., An Y.Y. Anxiety, depression and PTSD among children and their parent during 2019 novel coronavirus disease (COVID-19) outbreak in China. Curr. Psychol. 2020:1–8. doi: 10.1007/s12144-020-01191-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao N., Zhou G.Y. Social media use and mental health during the COVID-19 pandemic–Moderator role of disaster stressor and mediator role of negative affect. Appl. Psychol. Health Well Being. 2020;12(4):1019–1038. doi: 10.1111/aphw.12226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou S.J., Zhang L.G., Wang L.L., Guo Z.C., Wang J.Q., Chen J.C., …, Chen J.X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry. 2020;29(6):749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]