FIG 1.
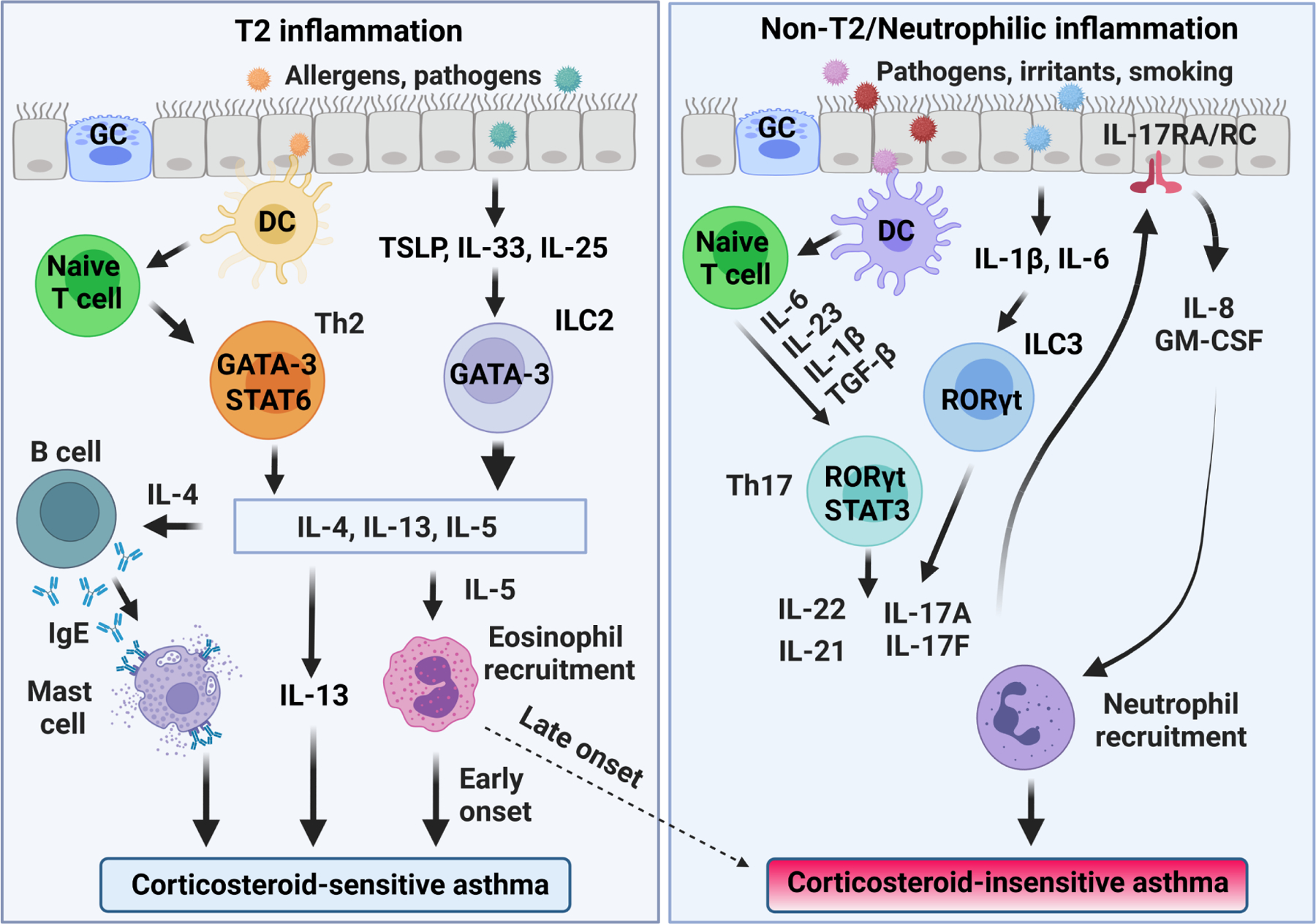
T2 and non-T2 inflammation in corticosteroid-sensitive and -insensitive asthma. Airway epithelia stimuli result in the production of alarmins, thymic stromal lymphopoietin (TSLP), IL-33, and IL-25 that stimulate differentiation of innate lymphoid type 2 cells (ILC2). Dendritic cells (DC) induce the differentiation of Th2 cells. ILC2 and Th2 cells produce the T2 cytokines IL-4, IL-5, and IL-13 via GATA binding protein 3 (GATA3), contributing to the development of corticosteroid-sensitive asthma. Late-onset eosinophilic asthmatics can have persistent airway eosinophilia despite corticosteroid therapy (dashed line). Corticosteroid-insensitive asthma results from exposure to pathogens, irritants, and smoking triggering release of TGF-β, IL-6, IL-1β, and IL-23 that stimulate differentiation of Th17 cells via transcription factors RORγt and STAT3. Th17 cells produce cytokines IL-17A, IL-17F, IL-21, and IL-22 that stimulate the production of neutrophilic chemokines (e.g., IL-8 and GM-CSF). Innate lymphoid type 3 cells (ILC3) also produce IL-17 and play roles in obesity-associated, corticosteroid-insensitive asthma. GC, goblet cells; GM-CSF, granulocyte-macrophage colony-stimulating factor. Created with BioRender.com.
