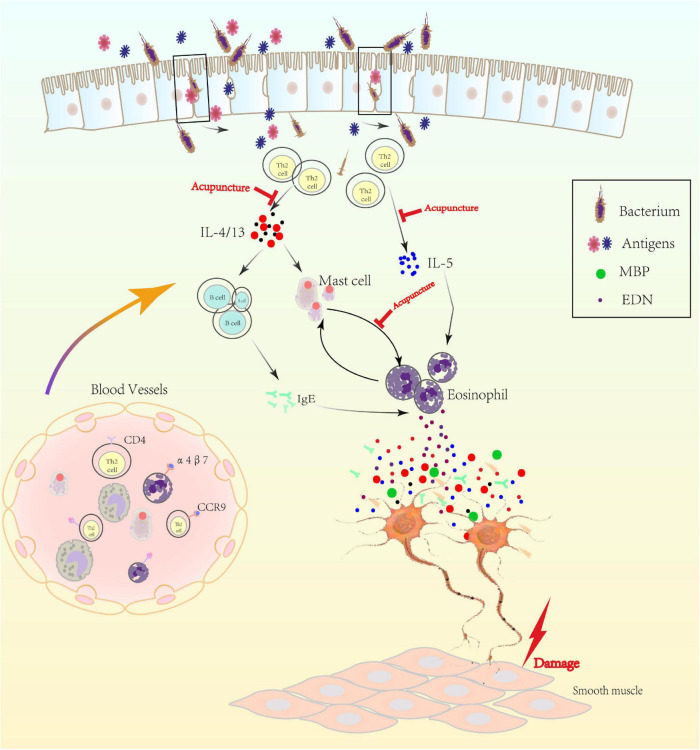
FIGURE 2.
The mechanism of low-grade inflammation in gastroduodenal tissue. Th2 cell was activated in the duodenum, possibly by bacterium or antigens, which crossed the epithelium after impairing of mucosal integrity. Activated eosinophil acted as antigen-presenting cell to Th2-lymphocytes with Ig class switching of B cells to proallergic IgE-antibodies via IL-4 or IL-13. Besides, Th2 cell was the key driver of mast cell and eosinophil via IL-4/13 or IL-5, separately. Activated eosinophil released major basic protein (MBP), eosinophil derived neurotoxin (EDN) and others, which regulated the plasticity of peripheral nerve and then caused visceral hypersensitivity. Gut-homing T cells and other immune cells (expressing α4β7 and CCR9) may also increase in number and produce excess inflammatory cytokines that could increase vascular permeability and alter smooth muscle contraction and then delay gastric empty.