Abstract
Objective:
To compare the short-term treatment effects of face mask therapy with miniplates (FM-MP) and face mask therapy with rapid maxillary expansion appliance (FM-RME) in growing Class III malocclusion patients with maxillary hypoplasia.
Materials and Methods:
Twenty patients were allocated into two groups according to the anchorage device: FM-MP group (n = 10; mean age = 11.2 ± 1.2 years; miniplates in the zygomatic buttress area) and FM-RME group (n = 10; mean age = 10.7 ± 1.3 years; bonded or banded RME). The face mask was applied for 12 to 14 hours/day in both groups with a force of 400 g/side directed 30° downward and forward from the occlusal plane. Lateral cephalograms were taken before (T1) and after FM-MP or FM-RME therapy (T2). Skeletodental and soft-tissue variables were measured. Paired and independent t-tests were performed for statistical analysis.
Results:
Both groups exhibited significant forward movement of point A and posterior repositioning and opening rotation of the mandible from T2 to T1. The FM-MP group showed significant protraction of orbitale (ΔSNO), and the FM-RME group showed a decrease in overbite and an increase in Björk sum. Comparing the amount of changes between the two groups, the FM-MP group displayed greater forward movement of the maxilla than the FM-RME group (ΔSNA, ΔA to N perp, all P < .05). However, the FM-RME group exhibited a greater opening rotation of the mandible (ΔSNB, Björk sum, all P < .01; ΔPog to N-perp, P < .05) and labioversion of the maxillary incisors (ΔU1-FH, P < .05).
Conclusion:
FM-MP therapy induces a greater advancement of the maxilla, less posterior repositioning and opening rotation of the mandible, and less proclination of the maxillary incisors than FM-RME therapy.
Keywords: Face mask, Miniplates, RME, Class III malocclusion
INTRODUCTION
Face mask therapy has been applied to treat growing Class III patients with mild to moderate maxillary hypoplasia.1,2 Several tooth-borne anchorage devices, such as a labiolingual arches, Quad-helix appliances, or rapid maxillary expansion appliances (RMEs), are used for face mask therapy.2–4 Numerous studies have shown that use of a face mask in conjunction with tooth-borne anchorage devices results in a combination of the following skeletal and dental changes: forward movement of the maxilla, opening rotation of the mandible, closing rotation of the palatal plane, labioversion of the maxillary incisors, extrusion of the maxillary molars, and lingual tipping of the mandibular incisors.3,4
Because the skeletal effect decreases and the dental effect increases with age,5–7 skeletal anchorages, such as intentionally ankylosed deciduous canines, osseointegrated onplants and implants, and orthodontic miniscrews, have been introduced to maximize the skeletal effects in face mask therapy.8–13 The surgical miniplate can be used as a reliable anchorage tool for applying orthopedic forces to the maxillofacial skeletal complex; thus, face mask therapy combined with miniplate anchorage has recently been studied.14–18 However, a few studies have compared the effects of face mask therapy with miniplates (FM-MP) to face mask therapy with RME (FM-RME).18 Therefore, the purpose of this study was to compare the short-term treatment effects of FM-MP and FM-RME in growing Class III malocclusion patients with mild to moderate maxillary hypoplasia. The null hypothesis was that there was no significant difference in the skeletodental and soft-tissue variables between the two treatment modalities.
MATERIALS AND METHODS
In this retrospective study, the samples consisted of 20 growing Class III malocclusion patients with maxillary hypoplasia who had similar skeletal and dental patterns. The patients were selected based on the following inclusion criteria: (1) skeletal and dental Class III malocclusion with maxillary hypoplasia in the mixed or early permanent dentition (SNA<80°; ANB<−1°; A to N perp <0 mm); (2) anterior crossbite and positive overbite; (3) no cleft and other craniofacial syndromes; and (4) no significant skeletal asymmetry (less than 2 mm chin-point deviation).
The patients were allocated into two groups according to the anchorage device: FM-MP group (n = 10; five girls and five boys; mean age = 11.2 ± 1.2 years; miniplates in the zygomatic buttress area of the maxilla) and FM-RME group (n = 10; six girls and four boys; mean age = 10.7 ± 1.3 years; eight bonded-type RME and two banded-type RME). Both groups were treated until an overjet greater than 2 to 3 mm and a Class II canine and molar relationship were achieved.
In the FM-MP group, two titanium miniplates (curvilinear type miniplate, LeForte system, Jeil Medical, Seoul, Korea) were used as a skeletal anchorage for extraoral elastics. The FM-MP protocol was performed as reported previously.15,17 After an approximately 2 cm horizontal vestibular incision was made just below the zygomatic buttress area under local anesthesia, the zygomatic buttress was exposed with a subperiosteal flap. Curvilinear surgical miniplates were bent according to the anatomic shape of the zygomatic buttress. After the miniplates were placed into the zygomatic buttress areas, three self-tapping type screws (diameter of 2 mm and length of 6 mm; Jeil Medical Co, Seoul, Korea) per side were used to fix the miniplates (Figure 1A). The distal end of the miniplate was exposed through the attached gingiva between the maxillary deciduous canine and deciduous first molar or between the maxillary permanent canine and first premolar to control the vector of elastic traction. Four to eight weeks after miniplate placement,15,17 mobility was assessed and the distal end hole of the miniplate was cut to create a hook for elastics (Figure 1B). An orthopedic force of at least 400 g/side directed 30° downward and forward from the occlusal plane, was applied for 12 to 14 hours per day.
Figure 1.
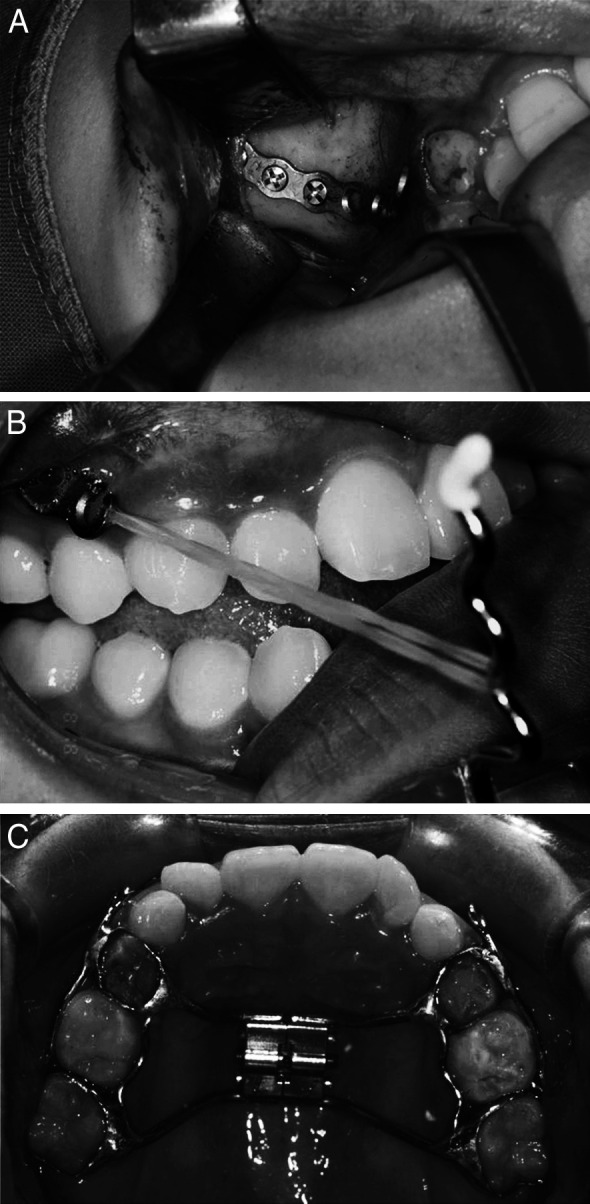
(A) After the miniplates were placed into the zygomatic buttress areas, three self-tapping type screws per side were used to fix the miniplates. (B) The distal end of the miniplate was exposed through the attached gingiva between the maxillary deciduous canine and deciduous first molar or between the maxillary permanent canine and first premolar to control the vector of elastic traction. Four to eight weeks after miniplate placement, their mobility was assessed and the distal end hole of the miniplate was cut to make a hook for elastics. (C) A conventional banded or bonded RME appliance was used as a tooth-borne anchorage for extraoral elastics.
In the FM-RME group, a conventional banded or bonded RME was used for tooth-borne anchorage for extraoral elastics (Figure 1C). A banded or bonded RME with two hooks for elastics was placed on the maxillary deciduous first molar and permanent first molar or the maxillary permanent first premolar and first molar. The RME was activated twice a day until the desired transverse maxillary width was achieved. Immediately after expansion, an orthopedic force of at least 400 g/side (5/16 in, 32 oz, energy pak elastics, RMO, Denver, Colo), directed 30° downward and forward from the occlusal plane, was applied for 12 to 14 hours per day.
Lateral cephalograms with centric occlusion, a reposed lip, and natural head position were taken before (T1) and after FM-MP or FM-RME therapy (T2) (Figure 2). The mean treatment durations were 1.0 ± 0.1 years in the FM-MP group and 1.1 ± 0.1 years in the FM-RME group. The cephalometric variables are listed in Table 1. Cephalometric tracing and measurements were performed by one investigator using a digitizer (Intuos2 graphic tablet, Wacom Technology Co, Vancouver, Canada) and V-Ceph software (CyberMed, Seoul, Korea) at units of 0.05° and 0.05 mm, respectively. Five randomly selected sets of cephalograms were retraced and redigitized after 2 weeks to determine the level of error in the initial measurements. There was no significant difference between the measurements (Dahlberg's formula, error of the linear measurement <0.94 mm; error of the angular measurement <1.05°); thus, the initial set of measurements was used for this study. Paired and independent t-tests were performed for statistical analysis.
Figure 2.
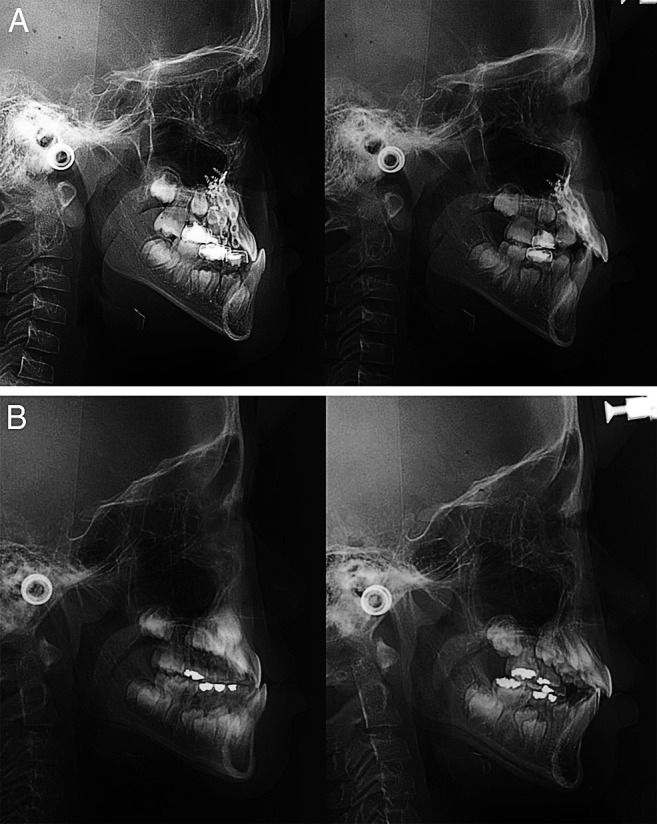
(A) Pretreatment (left) and posttreatment (right) cephalograms in one patient from the FM-MP group. (B) Pretreatment (left) and posttreatment (right) cephalograms in one patient from the FM-RME group.
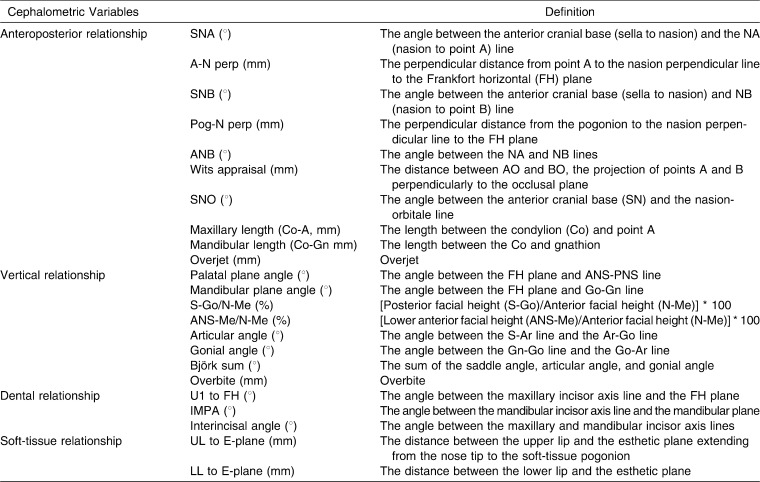
Table 1.
Definition of the Cephalometric Variables
RESULTS
Comparison of the Age and Treatment Duration According to Stage Between Two Groups
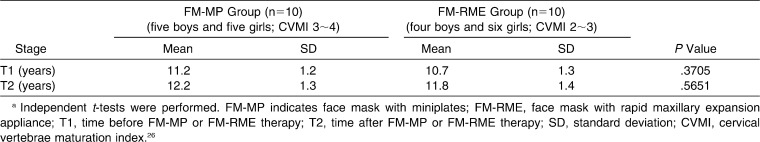
As shown in Table 2, there was no significant difference in age at each stage between the two groups, indicating that the samples were matched in terms of age. The mean durations of orthopedic treatment with the FM-MP and FM-RME therapies were 1.0 and 1.1 years, respectively.
Table 2.
Comparison of Age at the T1 and T2 Stages Between the FM-MP and FM-RME Groupsa
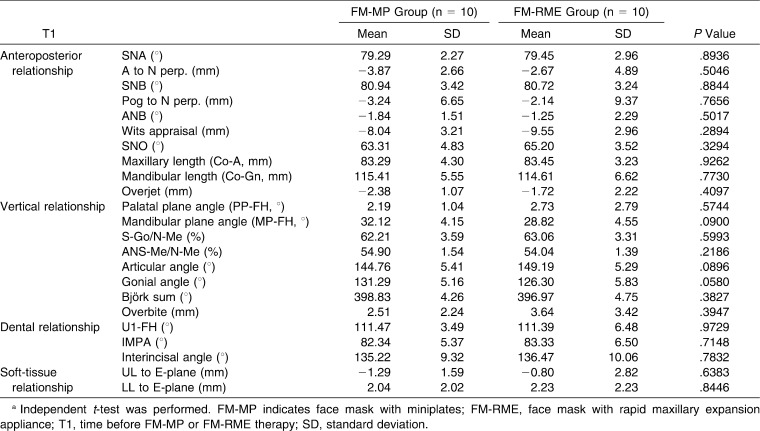
Comparison of the Cephalometric Variables Before Treatment Between Two Groups
As shown in Table 3, there was no significant difference in the cephalometric variables at the T1 stage between the two groups. These findings suggest that the samples had similar skeletodental and soft-tissue patterns at the T1 stage.
Table 3.
Comparison of Changes in the Cephalometric Variables Between Groups Before FM-MP or FM-RME Therapya
Comparison of Change in the Cephalometric Variables During FM-MP or FM-RME Therapy in Each Group
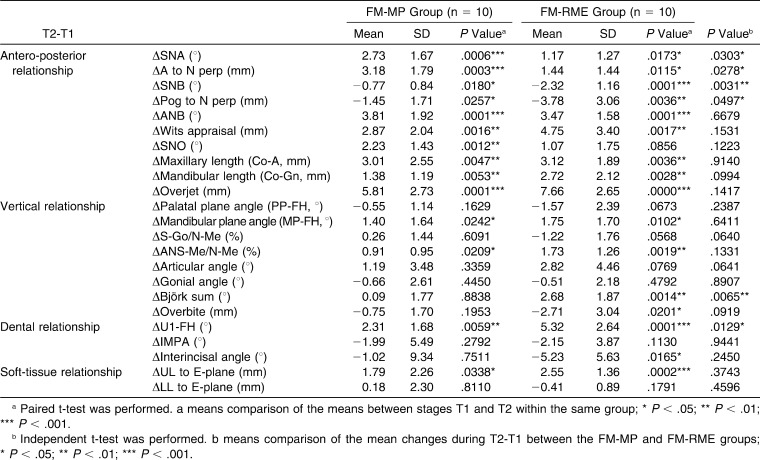
As shown in Table 4, in terms of the anteroposterior position of the maxilla, both the FM-MP and FM-RME groups showed forward movement of point A (ΔSNA, 2.7°, P < .001, and 1.2°, P < .05; ΔA to N-per, 3.2 mm, P < .001 and 1.4 mm, P < .05; ΔCo-A, 3.0 mm and 3.1 mm, all P < .01). In addition, the FM-MP group exhibited significant protraction of the orbitale (ΔSNO, 2.2°, P < .01).
Table 4.
Comparison of the Amount of Changes in the Cephalometric Variables During FM-MP or FM-RME Therapy in Each Group and Between Groups a
In terms of the anterior-posterior position of the mandible, both the FM-MP and FM-RME groups had posterior repositioning of the mandible (ΔSNB, −0.8°, P < .05, and −2.3°, P < .001; ΔPog to N-per, −1.5 mm, P < .05, and −3.8 mm, P < .01) and increases in ANB, Wits appraisal, and overjet (ΔANB, 3.8° and 3.5°; Δ overjet, 5.8 mm and 7.7 mm, all P < .001; ΔWits appraisal, 2.9 mm and 4.8 mm, all P < .01).
Regarding the changes in the vertical relationship, both the FM-MP and FM-RME groups showed opening rotation of the mandible (ΔMP-FH, 1.4° and 1.8°, all P < .05; ΔANS-Me/N-Me, 0.9%, P < .05, and 1.7%, P < .01). In addition, the FM-RME group exhibited a significant decrease in overbite (−2.7 mm, P < .05) and an increase in the Björk sum (2.7°, P < .01).
A comparison of the amounts of dental and soft-tissue change within each group revealed that both the FM-MP and FM-RME groups had an increase in labioversion of the maxillary incisors (ΔU1-FH, 2.3°, P < .01, and 5.3°, P < .001) and protrusion of the upper lip (ΔUL to E-plane, 1.8 mm, P < .05, and 2.6 mm, P < .001). In addition, the FM-RME group exhibited a significant decrease in the interincisal angle (Δinterincisal angle, −5.2°, P < .05).
Comparison of the Amount of Changes in the Cephalometric Variables Between Two Groups
As shown in Table 4, the FM-MP group demonstrated greater forward movement of the maxilla than the FM-RME group (ΔSNA, 2.7° vs 1.2°; ΔA to N perp, 3.2 mm vs 1.4 mm; all P < .05). These findings suggest that FM-MP therapy may induce more forward growth of the maxilla than the FM-RME therapy. However, the FM-RME group showed greater backward and downward rotation of the mandible than the FM-MP group (ΔSNB, −0.8° vs −2.3°; ΔBjörk sum, 0.1° vs 2.7°; all P < .01; ΔPog to N-per, −1.5 mm vs −3.8 mm, P < .05). These findings suggest that FM-RME therapy may induce more opening rotation of the mandible as well as an increase in the vertical dimension compared with FM-MP therapy. In addition, the FM-RME group had significant labioversion of the maxillary incisors compared with the FM-MP group (ΔU1-FH, 2.3° vs 5.3°; P < .05). This finding indicates that FM-RME therapy may induce a greater dental effect in the maxillary incisors compared with FM-MP therapy. There was no significant difference in the amount of change in the soft-tissue variables between the two groups.
DISCUSSION
Achieving skeletal movement without compensatory tooth movement is desirable in the orthopedic treatment of growing Class III patients with maxillary hypoplasia. The use of miniplates as a skeletal anchorage for maxillary protraction has recently been studied.14–21 The present study was performed to compare the short-term skeletodental effects of FM-MP and FM-RME in growing Class III malocclusion patients with mild to moderate maxillary hypoplasia.
Because the results of orthopedic treatment can be affected by the patient's original skeletal and dental characteristics as well as the growth of the maxilla and mandible, it is important to compare patients matched based on age and skeletodental pattern. There were no significant differences in age at each stage between the two groups (11.2 years vs 10.7 years at the T1 stage; 12.2 years vs 11.8 years at the T2 stage; Table 2) or in the skeletodental patterns at the T1 stage between the two groups (Table 3). Therefore, both groups appeared to be appropriately matched based on age and cephalometric characteristics of Class III malocclusion before orthopedic treatment. In addition, the sex distribution in the FM-MP group was not significantly different from that in the FM-RME group (five girls and five boys vs six girls and four boys).
The FM-MP group presented with greater forward movement of the maxilla than the FM-RME group (Table 4), which indicates that applying orthopedic force to the maxilla through miniplates might be more effective in protracting the maxilla than applying the orthopedic force through RME.18,19 This finding suggests that FM-MP therapy can effectively induce maxillary advancement by transferring the force directly to the circum-maxillary sutures. Numerous previous studies have reported that RME can disarticulate the circum-maxillary suture system, initiate cellular response in the sutures, and indirectly facilitate the orthopedic effect of the face mask.1,2,22,23 On the other hand, in meta-analysis study, Kim et al.24 found that the results of protraction were similar with or without expansion. A prospective, randomized clinical trial25 showed that face mask therapy, with or without RME, produced equivalent changes in the dentofacial complex and insisted that RME might not be indispensable to maxillary protraction unless a transverse deficiency exists. In conjunction with maxillary protraction with miniplates, Cevidanes et al.19 reported that bone-anchored maxillary protraction without expansion produced significantly larger maxillary advancement than the FM-RME therapy, which was consistent with the results from this study.
Miniplates can be placed at several places. For example, Sar et al.18 used the miniplate anchorage system installed at the lateral wall of the pyriform aperture of the maxilla on both sides. In contrast, Cevidanes et al.19 and De Clerck et al.20,21 performed maxillary protraction using intraoral Class III elastics from upper miniplates that were installed at the infrazygomatic crest to lower miniplates installed in the mandibular symphysis area on both sides. Various orthopedic protraction methods with miniplates can produce different skeletodental effects on the craniofacial structures due to different force vectors.
The reason the FM-RME group exhibited a greater opening rotation of the mandible as well as a greater increase in the vertical dimension than the FM-MP group (Table 4) may be because the extrusion of the maxillary posterior teeth occurred by force application (expansion and protraction) via tooth-borne anchorage and eventual closing rotation of the maxilla in the FM-RME group. These findings suggest that FM-MP therapy can minimize the opening rotation of the mandible in cases of Class III malocclusion with maxillary hypoplasia and a vertically excess mandible; the pure advancement effects are accompanied by a lesser closing rotation of the maxilla. Consistent with this finding, Sar et al.18 reported that the posterior rotation of the mandible and increased facial height were more evident in the FM-RME group than the FM-MP group. In contrast, some investigators also reported the lack of opening rotation of the mandible in maxillary protraction therapy using intraoral Class III elastics between upper and lower miniplates without a face mask.19,21
Some studies reported that FM-MP therapy can be considered an effective alternative treatment modality for obtaining maximum skeletal effects with minimal dental side effects in patients with severe maxillary hypoplasia or lacking anchorage teeth for the face mask.14–18 In this study, FM-MP therapy induced less labioversion of the maxillary incisors compared with FM-RME therapy (U1-FH, 2.3° vs 5.3°; P < .05; Table 4), which was consistent with the results from Sar et al.18 However, Cevidanes et al.19 reported that there was no difference in the degree of labioversion of the maxillary incisors between the bone anchor miniplates group and the FM-RME group. This difference might be due to the dissimilarity of the samples or to the orthopedic protraction of the maxilla using intraoral Class III elastics between the upper and lower miniplates applied without a face mask.
This study has some limitations, such as a small sample size, use of chronological age, the lack of homogeneity of RME type, and the lack of untreated Class III or Class I malocclusion as control groups. Further studies are needed to examine the long-term stability of changes related to the maxilla and the mandible after FM-MP therapy and to compare the skeletal and dental effects on the craniofacial structure between various orthopedic protraction methods with miniplates.
CONCLUSIONS
The null hypothesis was rejected.
FM-MP therapy induced a remarkable advancement of the maxilla, less posterior repositioning and opening rotation of the mandible, and less proclination of the maxillary incisors than FM-RME therapy.
REFERENCES
- 1.McNamara J. A., Jr An orthopedic approach to the treatment of Class III malocclusion in young patients. J Clin Orthod. 1987;21:598–608. [PubMed] [Google Scholar]
- 2.Baik H. S. Clinical results of the maxillary protraction in Korean children. Am J Orthod Dentofacial Orthop. 1995;108:583–592. doi: 10.1016/s0889-5406(95)70003-x. [DOI] [PubMed] [Google Scholar]
- 3.Ngan P. W, Hagg U, Yiu C, Wei S. H. Treatment response and long-term dentofacial adaptations to maxillary expansion and protraction. Semin Orthod. 1997;3:255–264. doi: 10.1016/s1073-8746(97)80058-8. [DOI] [PubMed] [Google Scholar]
- 4.Ngan P, Yiu C, Hu A, Hägg U, Wei S. H, Gunel E. Cephalometric and occlusal changes following maxillary expansion and protraction. Eur J Orthod. 1998;20:237–254. doi: 10.1093/ejo/20.3.237. [DOI] [PubMed] [Google Scholar]
- 5.Kapust A. J, Sinclair P. M, Turley P. K. Cephalometric effects of face mask/expansion therapy in Class III children: a comparison of three age groups. Am J Orthod Dentofacial Orthop. 1998;113:204–212. doi: 10.1016/s0889-5406(98)70141-6. [DOI] [PubMed] [Google Scholar]
- 6.Saadia M, Torres E. Sagittal changes after maxillary protraction with expansion in Class III patients in the primary, mixed, and late mixed dentitions: a longitudinal retrospective study. Am J Orthod Dentofacial Orthop. 2000;117:669–680. [PubMed] [Google Scholar]
- 7.Westwood P. V, McNamara J. A, Jr, Baccetti T, Franchi L, Sarver D. M. Long-term effects of Class III treatment with rapid maxillary expansion and facemask therapy followed by fixed appliances. Am J Orthod Dentofacial Orthop. 2003;123:306–320. doi: 10.1067/mod.2003.44. [DOI] [PubMed] [Google Scholar]
- 8.Kokich V. G, Shapiro P. A, Oswald R, Koskinen-Moffett L, Clarren S. K. Ankylosed teeth as abutments for maxillary protraction: a case report. Am J Orthod. 1985;88:303–307. doi: 10.1016/0002-9416(85)90129-0. [DOI] [PubMed] [Google Scholar]
- 9.Smalley W. M, Shapiro P. A, Hohl T. H, Kokich V. G, Brånemark P. I. Osseointegrated titanium implants for maxillofacial protraction in monkeys. Am J Orthod Dentofacial Orthop. 1988;94:285–295. doi: 10.1016/0889-5406(88)90053-4. [DOI] [PubMed] [Google Scholar]
- 10.Singer S. L, Henry P. J, Rosenberg I. Osseointegrated implants as an adjunct to facemask therapy: a case report. Angle Orthod. 2000;70:253–262. doi: 10.1043/0003-3219(2000)070<0253:OIAAAT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Enacar A, Giray B, Pehlivanoglu M, Iplikcioglu H. Facemask therapy with rigid anchorage in a patient with maxillary hypoplasia and severe oligodontia. Am J Orthod Dentofacial Orthop. 2003;123:571–577. doi: 10.1067/mod.2003.S0889540603000520. [DOI] [PubMed] [Google Scholar]
- 12.Hong H, Ngan P, Han G, Qi L. G, Stephen H. Y. Use of onplants as stable anchorage for facemask treatment. Angle Orthod. 2005;75:453–460. doi: 10.1043/0003-3219(2005)75[453:UOOASA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 13.Vachiramon A, Urata M, Kyung H. M, Yamashita D. D, Yen S. L. Clinical applications of orthodontic microimplant anchorage in craniofacial patients. Cleft Palate Craniofac J. 2009;46:136–146. doi: 10.1597/06-219.1. [DOI] [PubMed] [Google Scholar]
- 14.Kircelli B. H, Pektaş Z. O, Uçkan S. Orthopedic protraction with skeletal anchorage in a patient with maxillary hypoplasia and hypodontia. Angle Orthod. 2006;76:156–163. doi: 10.1043/0003-3219(2006)076[0156:OPWSAI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Cha B. K, Lee N. K, Choi D. S. Maxillary protraction treatment of skeletal Class III children using miniplate anchorage. Korean J Orthod. 2007;37:73–84. [Google Scholar]
- 16.Kircelli B. H, Pektas Z. O. Midfacial protraction with skeletally anchored face mask therapy: a novel approach and preliminary results. Am J Orthod Dentofacial Orthop. 2008;133:440–449. doi: 10.1016/j.ajodo.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 17.Baek S. H, Kim K. W, Choi J. Y. New treatment modality for maxillary hypoplasia in cleft patients. Protraction facemask with miniplate anchorage. Angle Orthod. 2010;80:595–603. doi: 10.2319/073009-435.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sar C, Arman-Özçırpıcı A, Uçkan S, Yazıcı A. C. Comparative evaluation of maxillary protraction with or without skeletal anchorage. Am J Orthod Dentofacial Orthop. 2011;139:636–649. doi: 10.1016/j.ajodo.2009.06.039. [DOI] [PubMed] [Google Scholar]
- 19.Cevidanes L, Baccetti T, Franchi L, McNamara J. A, Jr, De Clerck H. Comparison of two protocols for maxillary protraction: bone anchors versus facemask with rapid maxillary expansion. Angle Orthod. 2010;80:799–806. doi: 10.2319/111709-651.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.De Clerck H. J, Cornelis M. A, Cevidanes L. H, Heymann G. C, Tulloch C. J. Orthopedic traction of the maxilla with miniplates: a new perspective for treatment of midface deficiency. J Oral Maxillofac Surg. 2009;67:2123–2129. doi: 10.1016/j.joms.2009.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.De Clerck H, Cevidanes L, Baccetti T. Dentofacial effects of bone-anchored maxillary protraction: a controlled study of consecutively treated Class III patients. Am J Orthod Dentofacial Orthop. 2010;138:577–581. doi: 10.1016/j.ajodo.2009.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haas A. J. The treatment of maxillary deficiency by opening the midpalatal suture. Angle Orthod. 1965;65:200–217. doi: 10.1043/0003-3219(1965)035<0200:TTOMDB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 23.Baccetti T, McGill J. S, Franchi L, McNamara J. A, Jr, Tollaro I. Skeletal effects of early treatment of Class III malocclusion with maxillary expansion and face-mask therapy. Am J Orthod Dentofacial Orthop. 1998;113:333–343. doi: 10.1016/s0889-5406(98)70306-3. [DOI] [PubMed] [Google Scholar]
- 24.Kim J. H, Viana M. A, Graber T. M, Omerza F. F, BeGole E. A. The effectiveness of protraction face mask therapy: a meta-analysis. Am J Orthod Dentofacial Orthop. 1999;115:675–685. doi: 10.1016/s0889-5406(99)70294-5. [DOI] [PubMed] [Google Scholar]
- 25.Vaughn G. A, Mason B, Moon H. B, Turley P. K. The effects of maxillary protraction therapy with or without rapid palatal expansion: a prospective, randomized clinical trial. Am J Orthod Dentofacial Orthop. 2005;128:299–309. doi: 10.1016/j.ajodo.2005.04.030. [DOI] [PubMed] [Google Scholar]
- 26.Hassel B, Farman A. G. Skeletal maturation evaluation using cervical vertebrae. Am J Orthod Dentofacial Orthop. 1995;107:58–66. doi: 10.1016/s0889-5406(95)70157-5. [DOI] [PubMed] [Google Scholar]