Many researchers have investigated the effect of the COVID-19 pandemic on mental health problems. Depression, anxiety, alcohol and substance misuse, and violence increase as a result of fear of infection and death, loss of loved ones, social distancing, income insecurities, and drastic changes in daily routines.1 However, important epidemiological questions have yet to be assessed, such as whether the prevalence of mental health problems increased in the general population and subpopulations worldwide during the COVID-19 pandemic. If so, how are mental health problems associated with characteristics of the pandemic and the extent and intensity of measures to contain the pandemic (such as lockdown and movement restriction)?
The answers to these questions cannot be provided by a single study because the exposures of interest (ie, local characteristics of the pandemic and stringency of containment measures) would apply to all participants. Longitudinal studies can play a part in examining the associations of interest but they are limited in population representation. A meta-ecological study is needed to explore the effect of geographically and temporally different pandemic characteristics on populations' mental health. Despite their potential shortcomings due to confounding and aggregation bias, meta-ecological study designs have successfully answered similar global questions, such as the role of air pollution on morbidity.2
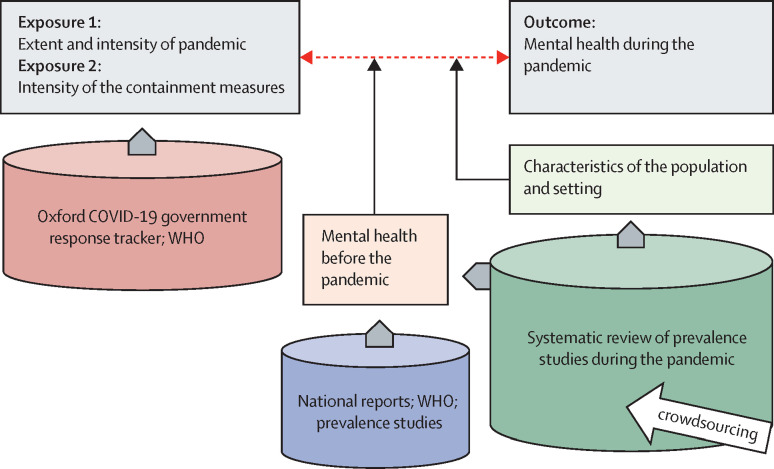
In a meta-ecological study, a systematic review of prevalence before and during the pandemic in various locations with different responses to the pandemic should shed light on changes in mental health problems (figure ). Since February, 2020, many COVID-19 studies have been published, and creative approaches, such as crowdsourcing, are needed to undertake parts of the systematic review.3 Lay volunteers can be trained to screen and evaluate identified studies in a rapid, yet reproducible way. Then, publicly available information can be used to quantify the intensity of the pandemic and the stringency of containment measures locally and associate them with the changes in prevalence of mental health problems. As the COVID-19 pandemic is likely to continue, the whole process needs to be repeated as a living systematic review.4 In our Mental Health in COVID-19 meta-epidemiological study, 75 trained crowd volunteers with experience in systematic reviews have screened more than 25 000 references. Such a study presents many challenges. Confounding and moderating factors need to be explored via meta-regression techniques. Studies are expected to be heterogeneous in the way they measure symptoms and diagnoses, and potentially large uncertainty in model input should be accounted for.
Figure.
A meta-ecological study to assess the effect of the COVID-19 pandemic on mental health
Schematic presentation of a meta-ecological study to associate time and location specific COVID-19 pandemic characteristics and stringency of containment policies with changes in population mental health while adjusting for population and setting characteristics. Cylinders represent data sources that will inform exposures and outcomes.
Because the study uses published and regularly updated information, it does not require expensive or time-consuming data collection. The crowdsourcing approach will speed up the process and could be the way forward to do large-scale research in times of social isolation. Investment in methods for harnessing information in a reliable and rapid way will enable decision makers worldwide to integrate a mental health science perspective into their response to the pandemic.
For the Mental Health in COVID-19 meta-epidemiological study see https://mhcovid.ispm.unibe.ch
Acknowledgments
AC reports grants and personal fees from the Italian Network for Paediatric Trials and Angelini Pharma; and personal fees from the Cariplo Foundation, outside the submitted work. AC is also supported by the National Institute for Health Research (NIHR) Oxford Cognitive Health Clinical Research Facility, by an NIHR Research Professorship (grant RP-2017-08-ST2-006), by the NIHR Oxford and Thames Valley Applied Research Collaboration, and by the NIHR Oxford Health Biomedical Research Centre (grant BRC-1215-20005). SL reports personal fees from LB Pharma, Otsuka, Lundbeck, Boehringer Ingelheim, LTS Lohmann Therapy Systems, Janssen Pharmaceuticals, Johnson & Johnson, Teva, MSD, Sandoz, Sanofi, Angelini Pharma, Recordati, and Gedeon Richter, outside the submitted work. TAF reports grants and personal fees from Mitsubishi-Tanabe and Shionogi; and personal fees from MSD, outside the submitted work. All other authors declare no competing interests. Our work is funded by the National Research Programme 78 COVID-19 scheme of the Swiss National Science Foundation (grant number 198418). The views expressed are those of the authors and not necessarily those of the UK National Health Service, the NIHR, or the UK Department of Health.
References
- 1.Centers for Disease Control and Prevention COVID-19: coping with stress. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html
- 2.Künzli N, Kaiser R, Medina S, et al. Public-health impact of outdoor and traffic-related air pollution: a European assessment. Lancet. 2000;356:795–801. doi: 10.1016/S0140-6736(00)02653-2. [DOI] [PubMed] [Google Scholar]
- 3.Vaish R, Gaikwad SNS, Kovacs G, et al. Crowd research: open and scalable university laboratories. Proceedings of the 30th Annual ACM Symposium on User Interface Software and Technology; Québec City, QC, Canada: Oct 25–27, 2017 (pp 829–43).
- 4.Elliott JH, Turner T, Clavisi O, et al. Living systematic reviews: an emerging opportunity to narrow the evidence-practice gap. PLoS Med. 2014;11 doi: 10.1371/journal.pmed.1001603. [DOI] [PMC free article] [PubMed] [Google Scholar]