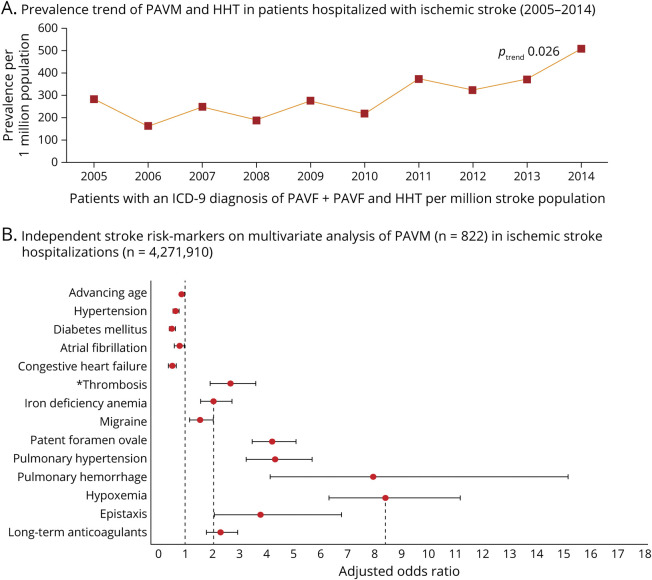
Figure 2. Prevalence and Risk Markers of Pulmonary Arteriovenous Malformation in Patients Hospitalized With Ischemic Stroke.
(A) 2021 nationwide analysis of pulmonary arteriovenous malformations (PAVMs) across a non-selected US population of 4,271,910 patients hospitalized with acute ischemic stroke (2005–2014), observing a significant increase in the prevalence of PAVMs in a combined cohort of patients with and without a concomitant ICD-9-CM diagnosis of hereditary hemorrhagic telangiectasia (HHT).19 (B) Clinical variables found to be independently associated with ischemic stroke on multivariable logistic regression analysis included hypoxemia as the strongest independent stroke risk marker (odds ratio [OR] 8.4, 95% confidence interval [CI] 6.3–11.2); iron deficiency anemia (OR 2.03, 95% CI 1.5–2.7) and epistaxis (OR 3.7, 95% CI 2.0–6.7), a common cause of iron deficiency anemia in patients with HHT, were the major modifiable risk markers. *Patients with PAVMs were 2.3-fold more likely to be on long-term anticoagulation even after adjusting for age, atrial fibrillation, primary hypercoagulable states, venous thrombosis, and pulmonary embolism.