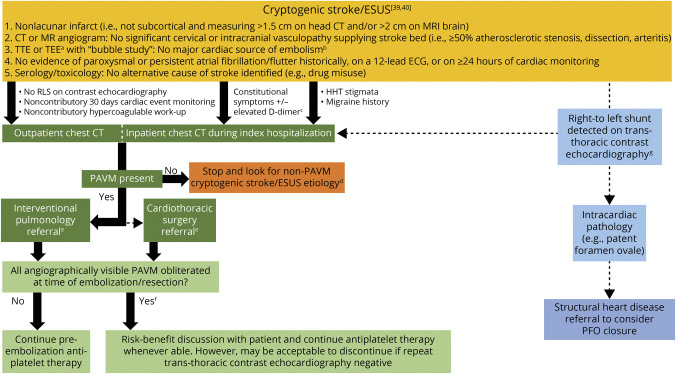
Figure 4. Diagnostic and Management Algorithm for Embolic Stroke Related to Pulmonary Arteriovenous Malformations.
Proposed diagnostic algorithm incorporating thoracic CT scans in the workup of embolic stroke of undetermined source (ESUS).39 aTransesophageal echocardiography (TEE) is considered when the transthoracic echocardiography (TTE) is technically limited or patient age is ≤60 years and there is high suspicion for atrial cardiopathy or aortic pathology.40 bPermanent or paroxysmal atrial fibrillation, sustained atrial flutter, intracardiac thrombus, prosthetic cardiac valve, atrial myxoma or other cardiac tumors, mitral valvulopathy, recent (<4 weeks) myocardial infarction, left ventricular ejection fraction less than 30%, or infective/other endocarditis.39 cCT chest may be performed as a part of a screening CT chest/abdomen/pelvis on a case-by-case basis, which may help identify a potentially occult solid organ malignancy.40 dPAVMs do not grow by any measurable extent in adult life (exceptions may include postpregnancy),5 and thus there is little value is repeating PAVM screening, even if the patient presents with subsequent ischemic stroke. eIf the risk-benefit analysis after considering surgical risk stratification, baseline functional status, concomitant vascular risk factor profile, and age (>60 years with a life expectancy <5 years considered a relative contraindication) is favorable, then endovascular embolization is performed. Rarely is surgical resection indicated when PAVMs are too diffuse to realistically achieve endovascular cure. fThe majority of treated patients will have residual right-to-left shunt (RLS), as demonstrated in Figure 1B. gLeft heart contrast opacification from an intrapulmonary RLS occurs within seconds, is not affected by cardiac cycles or respirations, and becomes certain if the bubble density is greater within left-heart than right (requires >30 seconds of recording).37 HHT = hereditary hemorrhagic telangiectasia; PFO = patent foramen ovale.