Figure 1.
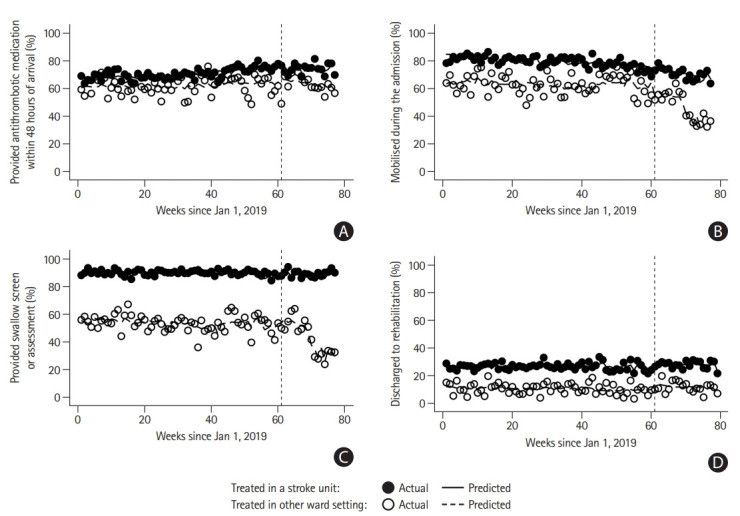
Proportion of patients (A) provided antithrombotic medication within 48 hours of arrival (excluding patients with intracerebral hemorrhage), (B) mobilized during the admission, (C) provided swallow screen or assessment, and (D) discharged to rehabilitation. The vertical line (week 61) indicates the week of the interruption used in this study (1/3/2020, the first coronavirus disease 2019 [COVID-19] related death in Australia). Significant difference in weekly trend between groups prior to interruption (β and 95% confidence intervals [CIs] presented): provided antithrombotic medication within 48 hours of arrival 0.09 (95% CI, 0.04 to 0.14); mobilized during the admission –0.15 (95% CI, –0.23 to –0.07). Significant difference during week of interruption between groups (week 61): provided antithrombotic medication within 48 hours of arrival –5.35 (95% CI, –9.08 to –1.61); provided swallow screen or assessment –5.81 (95% CI, –8.62 to –2.99); discharged to rehabilitation –2.2 (95% CI, –3.72 to –0.68). Significant difference in weekly trend between groups in post-interruption period: provided swallow screen or assessment 0.86 (95% CI, 0.48 to 1.24); discharged to rehabilitation 0.6 (95% CI, 0.37 to 0.83). β in a period signifies the difference in the average weekly percentage change over several weeks (trend) between groups. β during the week of the interruption signifies the difference in a percentage change during that week between groups. Positive values indicate a greater relative percentage increase in the provision of evidence-based care in stroke units compared with other ward settings. Negative values indicate a greater relative percentage decrease in the provision of evidence-based care in stroke units compared with other ward settings. Other point estimates relevant to the figure are provided in the Supplementary Table 1.
