Abstract
Context
Prevalence of overweight and obesity has been rising in the past 3 decades among Mexican children and adolescents.
Objective
To systematically review experimental studies evaluating interventions to treat obesity in Mexican children and adolescents (≤18 years old).
Data Sources
For this study, 13 databases and 1 search engine were searched.
Data Analysis
A total of 29 studies met the inclusion criteria. Overall, 2302 participants (age range, 8–16 years) from 11 states in Mexico were included. Most of the studies (n = 17 of 29) were provided in a clinical setting. A random-effect meta-analysis of 4 randomized controlled trials was conducted and a significant effect was found on body mass index reduction that favored the intervention group (−1.52; 95%CI, −2.15 to −0.89) for short-term (≤6 mo) interventions.
Conclusions
A multicomponent, multidisciplinary, and individualized intervention that includes dietary modifications, physical activity practice, behavioral strategies, and active parental involvement might help treat childhood obesity in Mexico. However, long-term results need to be produced to identify effectiveness pointers that might help establish an integrated, long-lasting care model to treat obesity.
Keywords: adolescents, children, intervention, Mexico, obesity, overweight
INTRODUCTION
Mexico is an upper-middle-income Latin American country, and it has been experiencing the double burden of malnutrition in recent decades.1 Specifically, childhood overweight and obesity rates have been increasing in the population younger than 19 years. According to the latest results from the National Health and Nutrition Survey 2018, it is estimated that in Mexico, 8.2% of infants (0–4 years old), 35.6% of children (5–11 years old), and almost 40% of the adolescents (12–19 years old) present overweight or obesity.2 These increasing levels position Mexico among the countries with higher levels of overweight worldwide.3 According to the Organization for Economic Cooperation and Development ’s estimations, such rates will continue to increase if no effective strategies are implemented.4 Currently, no national intervention or guideline exists targeting obesity treatment among children and adolescents.
Excess body fat in children and adolescents can lead to a variety of clinical conditions and psychosocial disorders. Children with obesity might have significant reductions in quality of life and a greater risk of early discrimination, low self-esteem, and depression. Children and adolescents with overweight and obesity are likely to maintain their weight status into adulthood and are at higher risk of development of chronic diseases, contributing to increased morbidity or premature death.5
Lifestyle interventions can lead to improvements in weight and cardiometabolic outcomes in children or adolescents.6 However, effectiveness can be smaller compared with pharmacologic or surgical interventions.7 Still, most of the evidence shows short-term effects, with limited evidence about long-term efficacy. In addition, the safety of such pediatric obesity treatments remains unclear.7
Because of the severity of the consequences childhood obesity has on the child's health and well-being, it is essential to identify interventions that can treat obesity in the short and long term.8 The “Childhood and Adolescent Obesity in Mexico: Evidence, Challenges, and Opportunities” (COMO) Project aims to synthesize and use data to comprehend the extent, nature, effects, and costs of childhood or adolescent obesity in Mexico.9 This article is part of the COMO project. In this study, we aimed to systematically review experimental studies assessing lifestyle, environmental, behavioral, pharmacologic, or surgical interventions to treat obesity in Mexican children and adolescents (<18 years old).
METHODS
This systematic review has been registered with the International Prospective Register of Systematic Reviews (PROSPERO registration no. CRD42019154132).10 Also, it has been reported according to Preferred Reporting Items for Systematic Reviews and Meta‐analyses (PRISMA) guidelines.11 The systematic review strategy was based on the Population, Intervention, Comparator, Outcomes, Study (PICOS) design framework (Table 1). For more details on the methods we used, see Appendix 1.
Table 1.
PICOS framework
| Population | Children and adolescents from zero to 18 years old (mean age at the start of the study or evaluation) from any ethnicity or sex living in Mexico, with overweight or obesity, were included. |
|---|---|
| Interventions | Studies testing obesity treatment through lifestyle, environmental, behavioral, pharmacologic, or surgical interventions, delivered in any setting, were considered. |
| Comparator | Studies with or without a control group were considered. |
| Outcomes | Weight-related outcomes (eg, body mass index,, body mass index z-score) |
| Study design | Experimental studies |
Electronic searches
Terms such as “overweight,” “obesity,” “child,” “adolescent,” “intervention,” “program,” “Mexico” in the search strategy. The databases searched included Medline, Embase, the Cochrane Library, Global Health Library, LILACS, CINAHL, CAB abstracts, ERIC, PsycINFO, ScienceDirect, Scopus, AGRICOLA, and SciELO Citation Index. Also, relevant material was searched in the search engine Google Scholar. When possible, searches were also conducted in Spanish to capture relevant references. No inclusion study design restrictions were applied. Full reports and conference abstracts were included if these met the inclusion criteria. Reference lists of included studies also were scrutinized for additional publications. Searches were performed in January 2020 and updated in January 2021.
Selection criteria
Reports from 1995 onward in English, Spanish, or Portuguese were considered in this review. Following the PICOS framework (Table 1), the inclusion criteria were as described in the following paragraphs.
Population
Children and adolescents from zero to 18 years old (mean age at the start of the study or evaluation) from any ethnicity or sex living in Mexico were considered in this review. Studies including children and adolescents with overweight or obesity (defined as body mass index [BMI] above a healthy weight range; BMI z‐score > 1; clinical diagnosis; or study population reported as having overweight or obesity) were included. Mexican children living in a different country were excluded from this review to conceptualize the obesity problem within the country sociodemographic characteristics and avoid confounding information inherent to migration phenomena. Studies in which children were analyzed under severe conditions (eg, HIV, cancer, fibrosis, Down syndrome), premature babies, and pregnant adolescents were excluded.
Studies
Studies in which obesity treatment was tested through lifestyle, environmental, behavioral, pharmacologic, or surgical interventions were considered. Studies delivered in any setting (eg, home, school, clinic, community) or digital domains (eg, mobile-phone-network interventions) were considered.
Comparator
Studies with or without a control group were considered.
Outcomes
Effectiveness measurements included anthropometric changes (eg, weight, BMI, BMI z-score). Because of the type of interventions considered in this review, any lifestyle changes (eg, dietary, physical activity, behavioral outcomes) were also recorded.
Study design
Experimental studies were considered in this review.
Data extraction
Titles and abstract screening and full-text review was performed by 2 reviewers (L.L.-C., M.G.-B.) and 100% checked by a third reviewer (M.A.-M.). Two reviewers (M.A.-M. and L.L.-C.) extracted data independently from included papers. In case of any disagreement, a third author was contacted (Y.Y.G.-G.). A data extraction form was created based on the Effective Public Health Practice Project Quality Assessment Tool12 and the Template for Intervention Description and Replication.13 Data on the main components of the studies were extracted and categorized according to the components included: nutritional (eg, diet prescriptions, nutritional advice); physical activity (PA; eg, PA practices, PA advice); behavioral or psychological (eg, psychological, family, or behavioral therapy); environmental (ie, changes in children's settings to promote a weight change); pharmacologic (eg, sibutramine); or bariatric surgery. Any theory or framework used in the design or delivery of the intervention was recorded.
Risk of bias
Following the Cochrane Handbook's recommendation for Systematic Reviews of Interventions for health promotion interventions,14 the Effective Public Health Practice Project Quality Assessment Tool12 tool was used. Evidence was rated as strong, moderate, or weak on the basis of their selection bias; study design; confounders; blinding; data collection methods; withdrawals and drop-outs; intervention integrity; and analysis. Also, funding sources and reported conflicts of interests were extracted and considered in this review. For more details, see Appendix 1.
Data synthesis and analysis
A narrative synthesis was conducted across all the included studies. From those randomized controlled trials (RCTs) in which the mean difference and its standard deviation of BMI were reported or could be calculated, a meta-analysis was conducted. Whenever provided, intention-to-treat data were used. WebplotDigitizer software was used to extract data when data were provided in graphs. The formulas from the Cochrane Guidelines were used to estimate the effect size.15,16 Lifestyle interventions in obesity are quite heterogeneous; hence, we chose a random effect model for this analysis.17,18 Because of the small sample sizes, the Hedges estimator19 was used to fit the random-effect model. The analysis was done using R statistical software, using the library “metafor”.
RESULTS
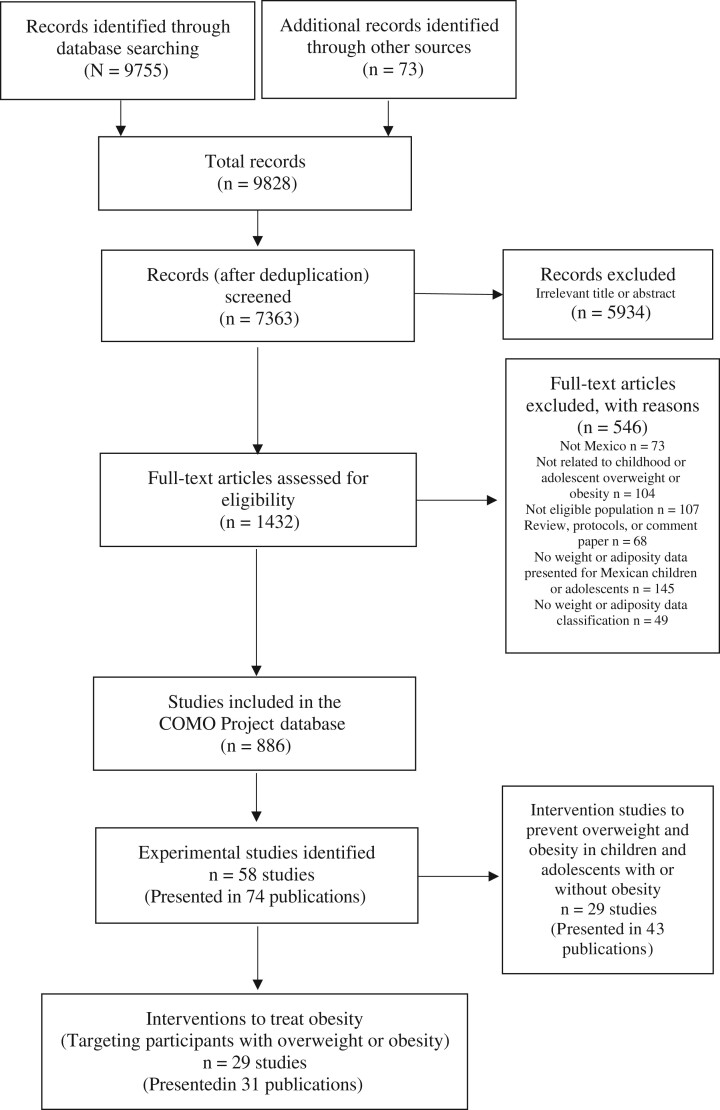
Through the searches, 7363 references were identified, from which 1432 were retrieved for full-text review. Overall, 886 references were identified by reporting obesity-related data in Mexican children and are included in the COMO database. From these, 29 studies (presented in 31 publications)20–50 met the inclusion criteria (Figure 1). Most of the publications were full-text papers, except for 3 abstracts,24,32,45 1 doctoral thesis,46 and 1 letter to the editor.50 Ten studies were RCTs,20,21,25,26,34,40–43,48 3 were controlled clinical trials,27,29,35 3 were cohort analytic studies with >1 group (2 or 3 groups, before and after),32,39,46 and 13 were cohort analytic studies with a single group (before and after).22–24,28,33,36–38,44,45,47,49,50
Figure 1.
PRISMA flowchart. COMO, Childhood and Adolescent Obesity in Mexico: Evidence, Challenges, and Opportunities.
Overall, the 29 identified studies included 2302 participants (age range, 8–16 years) recruited from 11 states of 32 states in Mexico (Figure 2). Most of the studies were conducted in a clinical setting (n = 17); some (n = 7) in a school setting. One included both settings (ie, school and clinic).40 In 1 study, participants were recruited in a school, but activities were delivered outside school hours.41 Two studies were conducted in summer camps39,46; the setting was unclear in 1 of the studies24 (Table 2).20–50
Figure 2.
Map of the Mexican 11 states from which evidence was reported.
Table 2.
General characteristics of included studies
| Reference; study design | Setting characteristics: location, setting, year intervention was implemented | Participants’ characteristics: total initial sample, female sex (%), mean (SD) age | Main intervention | Main characteristics of intervention: duration, follow-up period, intensity and frequency | Nutritional component | PA component | Psychological or behavioral component | Pharmacologic or surgery component | Other relevant component |
|---|---|---|---|---|---|---|---|---|---|
|
|
|
The CENLO (not an abbreviation) health program considered 3 simultaneously: nutritional orientation, PA practice, and phototherapy (ie, light therapy or heliotherapy post-PA) |
|
✓ | ✓ | NR | NR | Phototherapy was implemented in 1 of the interventions groups. |
|
|
|
Behavioral modification intervention based on a program, culturally appropriate topics focused mainly on the health belief model and a simple food guide |
|
✓ | ✓ | ✓ | NR | Parents received 6 education sessions and were encouraged to lose weight if they were overweight. |
|
|
|
Dietetic and lifestyle intervention, including individualized diets and PA, advice Information was given to parents about healthy food and eating. |
|
✓ | ✓ | NR | NR | Parents were involved in the intervention. |
|
|
|
|
|
✓ | NR | NR | NR | Parents were involved in the intervention. |
|
|
|
Lifestyle intervention based on the Spanish program “Kids in Motion,” which aims to produce changes in the child and their family, lifestyle, eating habits, and emotional factors contributing to weight gain |
|
✓ | ✓ | ✓ | NR | NR |
|
|
|
Pharmacologic intervention (ie, sibutramine) plus lifestyle changes intervention Participants received individually tailored diet and exercise advice. |
|
✓ | ✓ | NR | ✓ | NR |
|
|
|
Patients received a lifestyle intervention program and were randomly assigned to receive either metformin (1 g/d) and conjugated linoleic acid (3 g/d) or a placebo (1 g/d). Lifestyle intervention included a structured PA session, followed by a psychoeducational group session and educational material about healthy lifestyles. |
|
✓ | ✓ | ✓ | ✓ | Parents were involved in the intervention. |
|
|
|
Lifestyle intervention focused on eating habits modification through individualized diets. |
|
✓ | NR | NR | NR | The intervention included personalized diet for the parents and children. |
|
|
|
PA practice intervention based on the CATCH model (US program), including moderate to vigorous exercise |
|
NR | ✓ | NR | NR | Pedagogical elements of teaching support for the teacher to instruct PA with moderate to vigorous intensity for ≥50% of class time. |
|
|
|
Lifestyle intervention included dietary advice, PA practices, behavioral counselling, and active involvement of the family. |
|
✓ | ✓ | ✓ | NR | Family (parents and siblings) was involved in the intervention. |
|
|
|
Surgery intervention. Two different bariatric surgeries: in 1 cohort, the gastric sleeve was performed, and in the other, gastric bypass. |
|
NR | NR | NR | ✓ | NR |
|
|
|
Lifestyle intervention included the “PREVENIMSS program” (lifestyle change comprehensive program used in the public health system), nutritional support, and PA performance. |
|
✓ | ✓ | NR | NR | NR |
|
|
245 52.6% 13.6 (1.8) y |
Supplementation intervention. Participants were randomly assigned to receive 800 mg EPA + 400 mg DHA or a placebo. |
|
✓ | NR | NR | NR | NR |
|
2018 |
|
Mindfulness intervention with guided sessions, with interactive activities to teach standard mindfulness skills. A short homework exercise was assigned to help children apply mindfulness skills to daily life. |
|
? | NR | ✓ | NR | Sessions were delivered for parents in parallel with the sessions provided to the children. |
|
|
|
Educational intervention that included children’s’ mothers. It used a participatory technique following a diabetes mellitus educational program. Also, outdoor PA for mothers and children |
|
✓ | ✓ | NR | NR | Parents were involved in the intervention. |
|
|
|
“Light mind and weight” was a lifestyle intervention for children and parents. Participants were taught how to put together their menus with no restrictions. They were thought to achieve the right nutritional balance. PA practice sessions were delivered. Cognitive behavioral therapy was conducted in group sessions for children's parents. |
|
✓ | ✓ | ✓ | NR | Parents were involved in the intervention. |
|
|
|
Educational intervention including both children and parents in small groups (5 children with their parents or guardians) provided material about the importance of adequate nutrition. |
|
✓ | ✓ | NR | NR | Parents were involved in the intervention. |
|
|
|
Lifestyle intervention delivered at a 5-day summer camp. Activities included group sessions where participants were encouraged to express their feelings about eating behavior and express their thoughts and emotions. |
|
? | ? | ? | NR | In group 2, parents were involved in the intervention. |
|
|
|
Cognitive behavioral therapy plus indications for a low-calorie diet and PA practice |
|
✓ | ✓ | ✓ | NR | Parents were invited to participate in the exercise group sessions. |
|
|
|
PA practice group sessions intervention |
5 mo NR 40 sessions (50 min each × 2 times a week) Delivered by: NR |
NR | ✓ | NR | NR | NR |
|
|
|
Intervention looking at the increase in ready-to-eat cereal (from Kellogg’s) intake |
|
✓ | NR | NR | NR | Mothers were involved in the intervention. |
|
|
|
Supplementation intervention. Participants were randomly assigned to (1) 2 gummies 60 mg of DHA and EPA; (2) 3 gummies (90 mg DHA and EPA); (3) 10 g of salmon (211 mg DHA); or (4) 15 g of salmon (316 mg DHA) |
|
× | NR | NR | NR | Supplements of DHA |
|
|
|
Educational intervention targeting adolescents and mothers to modify the level of PA and the consumption of foods rich in fat. PA practice sessions were delivered for both mothers and adolescents. |
|
✓ | ✓ | NR | NR | Mothers were involved in the intervention. |
|
|
|
Individualized lifestyle intervention |
|
? | ? | NR | NR | NR |
|
|
|
Multidisciplinary intervention for weight loss treatment, which consisted of a weeklong summer camp and a monthly follow-up for6 mo (no additional information provided) |
|
? | ? | NR | NR | NR |
|
|
|
All patients and their families received personalized nutritional advice once a month. |
|
✓ | ✓ | NR | NR | Family (parents and siblings) was involved in the intervention. |
|
|
|
Nutritional intervention comparing Mediterranean-style vs a standard diet style. |
|
✓ | ✓ | NR | NR | Family (parents and siblings) was involved in the intervention. |
|
|
|
Pharmacologic intervention (ie, sibutramine 10 mg/d) with behavioral modification intervention, and PA and dietetic advice. |
|
✓ | ✓ | ✓ | ✓ | NR |
|
|
|
PA practice and a diet modification intervention |
|
✓ | ✓ | NR | NR | NR |
Abbreviations: DHQ, docosahexaenoic acid; EPA, eicosapentaenoic acid; NR, not reported; PA, physical activity; SES, socioeconomic status; CATCH, Coordinated Approach to Child Health, PREVENIMSS program, Spanish abbreviation for "Prevention program from the Mexican Institute of Social Security"; ✓, component included; ?, unclear if the component was included; ×, component not included.
Unclear from the publications if the population data of Elizondo-Montemayor et al22 and Elizondo-Montemayor et al23 overlapped. For this reason, these publications are presented separately.
Overall, 20 of the 29 studies included a nutritional component, 19 included a PA component, 8 included a psychological or behavioral component, and 3 studies included pharmacologic treatment. The effects of 2 different bariatric surgeries among participants were reported in 1 study32; however, this was 1 of the included abstracts, and it was poorly reported. None of the included studies reported an environmental change to aid the weight-loss process. In 16 studies, parents or siblings were included. The duration of the 29 studies ranged from 1 week to 12 months. There was no long-term (>12 mo) study identified in this review. An approximate number of sessions was calculated from reported information in the publications, and this number varied from 4 to 106 sessions. See Table 2 or Table S1 in Appendix 2 in the Supporting Information online.
Significant reductions in anthropometric outcomes were reported in 10 of the 29 studies,21–23,25,33,36,38,47–49 9 reported no significant changes,20,26,27,34,35,40,41,43,44 and the effect of the intervention was unclear in 5 studies.24,32,37,39,45 In 2 studies,28,50 significant changes were reported in some, but not all, of the anthropometric outcomes considered (eg, changes in skin folds, but not in BMI). Two studies29,46 reported effectiveness only in those participants who finished the intervention. For more details on the outcomes see Table S2 in Appendix 2 in the Supporting Information online.
Of the 29 included studies, 10 were RCTs; however, only 4 were included in the meta-analysis.20,21,40,48 One was excluded because it comprised a pharmacologic therapy (ie, sibutramine, banned since 2010 in Mexico).25 Three provided nutritional supplementation (with some generic dietary advice, but not a lifestyle intervention).26,34,43 One did not provide sufficient information to calculate the effect size.41 The study of Rosado et al42 was excluded from the meta-analysis because in that study, the aim was to increase ready-to-eat cereals as a strategy to reduce excess body weight, and no individualized nutritional advice was provided to participants.
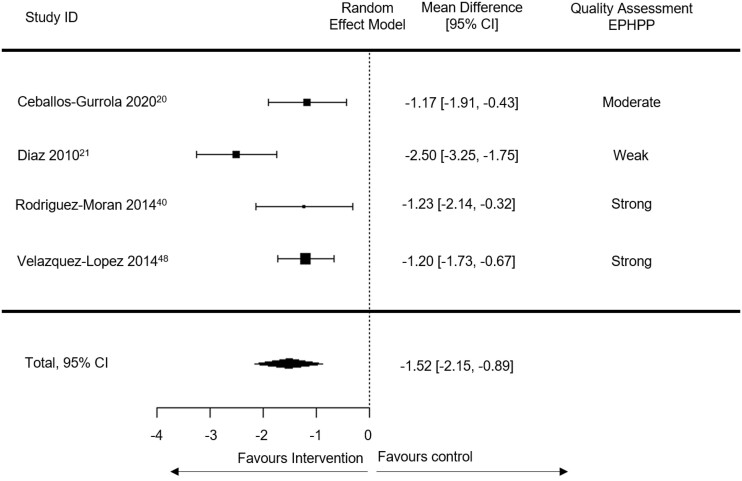
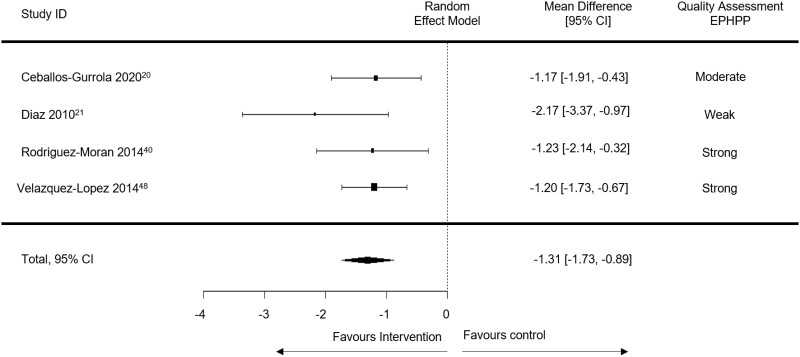
The population included in the 4 RCTs included in the meta-analysis was 237 participants (age range, 11–13 years old). The duration of these 4 RCTs varied from 3 months to 12 months. The intensity and frequency of sessions also varied, from 5 to 100 sessions. In the Díaz et al21 study, children with obesity participated in the intervention frequently during the first 12 weeks, and then the intensity decreased to monthly visits. The Díaz et al21 study was the only 1 presenting 6 and 12 months of data. Because the remaining studies included in the meta-analysis lasted 3.5 or 4 months, 2 analyses were done: 1 including data from Díaz et al 21 recorded at 6 months (Figure 3)20,21,40,48 and another with data at 12 months (Figure 4).20,21,40,48 Overall, there was a significant effect (−1.52; 95%CI, −2.15 to −0.89; I2 = 66%) (Figure 3) on BMI in the short term (≤6 mo) favoring the intervention groups. The effect was diminished but remained significant when including the 12 months of data from Díaz et al21 (−1.31; 95%CI, −1.73 to −0.89; I2 = 50%) (Figure 4).
Figure 3.
Meta-analysis with 6 months’ data (I2 = 66%). Weight of each study: Ceballos-Gurrola et al,20 12.7%; Diáz et al,21 27.5%; Rodríguez-Morán et al,40 26.9%; Velázquez-López et al,48 32.8%. Total number of participants in the intervention groups: 116; total number of participants in the control groups: 121. EPHPP, Effective Public Health Practice Project CI, Confidence Interval.
Figure 4.
Meta-analysis with 12 months’ data (I2 = 50%). Weight of each study: Ceballos-Gurrola et al,20 19.2%; Diáz et al,21 21.6%; Rodríguez-Morán et al,40 35.6%; Velázquez-López et al,48 23.5%. Total number of participants in the intervention groups: 116; total number of participants in the control groups: 121. EPHPP, Effective Public Health Practice Project, CI, Confidence Interval.
Overall, 6 of the 29 studies were considered of strong quality,25,29,34,40,42,47 5 of moderate quality,20,35,36,38,44 and the rest (n = 18) were considered of low quality. In 11 studies,20,21,25,26,34,40–43,48 participants were randomly assigned into different study groups; in 7 of these, the randomization methods were reported, and in 6,21,25,34,40,42,47 blinding of participants and personnel was reported. In most of the included studies (n = 20),20–23,25–29,33–36,38,40–42,47,48,50 individuals were somewhat likely to represent the target population. In 12 of the 29 studies, some relevant confounders were identified and controlled for.21,25,26,29,34,35,40,42,44,46,49 In most of the included studies, the data collection tools were valid and reliable. Data collection for anthropometric measurements did not raise any quality uncertainties, because all the studies collected data according to international protocols. However, lifestyle outcome measurements were very heterogeneous across studies, and the validity of tools was not reported in most cases. Withdrawals and drop-outs reported in 17 of the studies. When analyzing data, intention-to-treat analysis was used in only 3 studies.21,25,49 (Table 3).20–50
Table 3.
Quality assessment of included interventionsa
| Reference | Selection bias | Study design | Confounders | Blinding | Data collection methods | Withdrawals and drop-outs | Overall rating | Funding | COI |
|---|---|---|---|---|---|---|---|---|---|
| Ceballos-Gurrola 202020 | Moderate | Strong | Weak | Moderate | Strong | Moderate | Moderate | NR | NR |
| Diáz 201021 | Weak | Strong | Strong | Strong | Strong | Weak | Weak | Funded by an international agency | Nothing to declare |
| Elizondo-Montemayor 201322 | Moderate | Moderate | Weak | Moderate | Strong | Weak | Weak | No funding received | Nothing to declare |
| Elizondo-Montemayor 201423 | Weak | Moderate | Weak | Moderate | Strong | Strong | Weak | Funded by a private university | Nothing to declare |
| Escalante-Izeta 2013 (abstract)24 | Weak | Moderate | Weak | Moderate | Weak | Weak | Weak | NR | NR |
| García-Morales 200625 | Moderate | Strong | Strong | Strong | Strong | Moderate | Strong | Abbott Laboratories | NR |
| Garibay-Nieto 201726 | Weak | Strong | Strong | Moderate | Strong | Weak | Weak | Science Mexican Council | NR |
| González-Heredia 201427 | Moderate | Strong | Weak | Moderate | Strong | Weak | Weak | NR | Nothing to declare |
| Hall-López 201728 | Moderate | Moderate | Weak | Moderate | Strong | Weak | Weak | Funded by a public university | Nothing to declare |
| Huang 201029–31 | Moderate | Strong | Strong | Moderate | Strong | Strong | Strong | Funded by a public pediatric hospital | Nothing to declare |
| Jimenez 2017 (abstract)32 | Weak | Moderate | Weak | Moderate | Weak | Weak | Weak | NR | NR |
| Laguna-Alcaraz 201733 | Moderate | Moderate | Weak | Moderate | Strong | Weak | Weak | No funding received | Nothing to declare |
| López-Alarcon 201934 | Strong | Strong | Strong | Strong | Strong | Strong | Strong | Funded by public health institute and National Council of Education and Science Mexican Council | Nothing to declare |
| López-Alarcon 202035 | Moderate | Strong | Strong | Weak | Strong | Strong | Moderate | Funded by public health institute | Nothing to declare |
| Luna-Ruiz 200736 | Moderate | Moderate | Weak | Moderate | Strong | Strong | Moderate | NR | NR |
| Martin-Mosqueda 201237 | Weak | Moderate | Weak | Moderate | Strong | Weak | Weak | NR | NR |
| Moran 201738 | Moderate | Moderate | Weak | Moderate | Strong | Strong | Moderate | NR | NR |
| Pompa-Guajardo 201839 | Weak | Moderate | Weak | Moderate | Strong | Moderate | Weak | NR | NR |
| Rodríguez-Morán 201440 | Moderate | Strong | Strong | Moderate | Strong | Moderate | Strong | Partially funded by public health institute | Nothing to declare |
| Romero-Pérez 202041 | Moderate | Strong | Weak | Moderate | Strong | Weak | Weak | No funding received | Nothing to declare |
| Rosado 200842 | Strong | Strong | Strong | Moderate | Strong | Moderate | Strong | Funded by industry (Kellogg’s) | Nothing to declare |
| Rosas-Nexticapa 201743 | Weak | Strong | Weak | Moderate | Strong | Weak | Weak | Funded by the National Council of Education and Science Mexican Council | NR |
| Sáenz-Soto 200444 | Weak | Moderate | Strong | Moderate | Strong | Moderate | Moderate | NR | NR |
| Santiago-Lagunes 2018 (Abstract)45 | Weak | Moderate | Weak | Moderate | Strong | Weak | Weak | NR | NR |
| de Sanchez 200446 | Weak | Moderate | Weak | Moderate | Strong | Strong | Weak | NR | NR |
| Velázquez-López 200947 | Moderate | Moderate | Weak | Moderate | Strong | Weak | Weak | Unclear if funded by public health institute | Nothing to declare |
| Velázquez-López 201448 | Moderate | Strong | Strong | Strong | Strong | Strong | Strong | Funded by public health institute | Nothing to declare |
| Violante-Ortíz 200549 | Weak | Moderate | Strong | Moderate | Strong | Weak | Weak | NR | NR |
| Virgen-Ortíz 2007 (letter to the editor)50 | Weak | Moderate | Weak | Moderate | Strong | Weak | Weak | NR | NR |
Abbreviations: COI, conflict of interest; NR, not reported.
Quality assessed using the Effective Public Health Practice Project Quality Assessment Tool12 for quantitative studies.
Thirteen of the 29 studies did not report any funding source, and 3 reported not receiving funding for the intervention.22,33,41 For 1 study, authors reported receiving funding from the food industry,42 and in another, authors reported receiving funding from a pharmaceutical company.25 National funding was reported in 2 studies,26,43 and for 1 study, authors reported receiving support from international organizations.21 Six of the 29 studies reported28,29,34,35,40,48 receiving funding from public institutions (eg, public hospitals, public universities), and 123 reported receiving funding from private institutions (eg, private universities, insurance companies). The authors’ conflicts of interest were not reported in 17 studies. In those studies that reported it, no conflict of interest was declared.
DISCUSSION
In this systematic review and meta-analysis of evidence from studies of obesity in Mexican children and adolescents, we found a significant short-term (≤12 mo) effectiveness on BMI reduction. However, these results need to be cautiously interpreted in the light of the analysis’ limitations. Only 4 RCTs,20,21,40,48 with an overall sample of 237 participants (age range, 11–13 years old), were suitable to be included in a meta-analysis, and only 2 of these were of strong quality. Moreover, these 4 RCTs were delivered in different settings. Also, from the 29 studies included in this review, evidence regarding weight-related outcomes improvement was heterogeneous and inconclusive. Most of the evidence was of low quality, which increased the risk of bias. Across all the studies, several interventions with different durations and intensities were found. Still, no long-term interventions (≥12 mo) were identified in this systematic review.
Overall, the purposes of the interventions in the 29 studies identified mainly were to reduce energy intake, increase energy expenditure, and decrease sedentary behavior. Some interventions (n = 8) also included a psychological or behavioral component, and 3 included pharmacologic treatment. One abstract reported the comparison of 2 types of bariatric surgery among adolescents. There is still no gold standard childhood obesity treatment. However, some effectiveness has been shown in multicomponent interventions.51
In 12 studies, parents were included in the activities, and in 3, siblings were included as well. The involvement of parents has been described as a critical factor for the effectiveness of childhood obesity treatments.52 Family-based obesity therapy provides interventions for both children and their parents, but children benefit more compared with their parents.53
We found that most interventions to treat obesity in Mexican children and adolescents were delivered in a clinical setting (n = 17 of 29). Also, from the included studies, no environmental changes were identified. Childhood obesity treatment ideally should be provided within an integrated care system, including primary care practice, a tertiary care center, and support at home, school, and in community settings.51 The conception of a support network for young people while attempting to lose weight and maintain a healthy weight needs to target different settings and include several stakeholders. Likewise, environmental changes need to be made to facilitate behavioral change.54
It is noteworthy that Mexico has led the implementation of different nationwide strategies to tackle obesity among the general population. For instance, Mexico recently introduced a 1 peso/L excise tax on sugar-sweetened beverages.55,56 More recently, a front-of-pack labelling system has been implemented.57 Still, effective and targeted strategies are needed urgently to tackle this problem among children and adolescents. Some institutional documents about generic obesity prevention and diagnostic procedures can be found.58–60 However, such documents are not targeted to populations <18 years old, do not contemplate a comprehensive treatment of obesity, and are mainly limited to primary health care.
From the 4 RCTs included in the meta-analysis, the studies of Rodríguez-Morán et al40 and Diáz et al21 showed the most beneficial effect across studies. However, the Rodríguez-Morán et al40 study was considered to have a strong quality, whereas the study of Diáz et al21 was considered to be of low quality. The intervention delivered by Rodríguez-Morán et al40 included an individualized low-calorie diet, individualized PA advice, group exercise sessions (including parents), and individualized cognitive behavioral therapy as adjuvant treatment. This intervention was delivered in a public clinic by a multidisciplinary team (including doctors, psychologists, nutritionists, and graduates in physical education and sport). Although it was a short-term intervention (4 mo), the frequency was greater than in other included studies. Participants received 20 nutrition sessions (1 h/wk), plus 80 after-school PA sessions, plus individualized cognitive behavioral therapy sessions (when necessary). This intervention's effect size was significant, favoring the intervention group, and might indicate the importance of an individualized, frequent, and multidisciplinary effort, considering close relatives for treating childhood obesity in a Mexican context. Nevertheless, better-quality research needs to be done in Mexico to determine the optimal length, intensity, and long-term effectiveness of obesity treatment interventions among children and adolescents.
A multicomponent and individualized study that comprises dietary modifications, PA practice, behavioral strategies, and active parental involvement has been suggested in other countries.6,7,51 Long-term results are needed to measure and identify effectiveness pointers, and might help create an integrated long-lasting health care model that aids in preventing and treating obesity. Such a health care model should make available the integration of follow-up visits to monitor and maintain behavioral change as needed, facilitating the provision of the required intensity and frequency of treatment sufficient to achieve meaningful outcomes.61,62
While conducting this systematic review, we found some challenges, including for instance, the poor description of methods across the included papers. The lack of high-quality RCTs also is noticeable. Ten of the 29 studies were RCTs, but only 4 could be included in a meta-analysis. The sample sizes of the included RCTs were relatively small. Few studies with small sizes could introduce into the model bias or variability because of sampling. Some other limitations of this systematic review include the heterogeneity of included studies in terms of intervention design, sample size and characteristics, intervention approach, primary measures used to assess intervention effects, length of follow-up, analytical approaches, and overall quality. Such variability made it challenging for cross-comparisons. Also, the retrieved evidence came from 11 of 32 states in Mexico, so the results might not reflect a nationwide picture.
This work's strengths include, to our knowledge, being the first systematic review conducted about intervention to treat obesity in Mexican children and adolescents. This is relevant considering that most of the published systematic reviews include only English publications, excluding valuable evidence from non–English-speaking low- or middle-income countries such as Mexico. The exhaustive search for evidence was done across 13 databases and 1 search engine, in 2 languages (whenever possible), which helped us capture relevant publications. The included studies’ particular characteristics were extracted, and the quality of evidence was appraised, which was considered in the synthesis.
No cost-effectiveness studies regarding Mexican interventions to prevent or tackle childhood obesity were identified in the COMO project. However, some economic models have suggested that the costs of childhood obesity in Mexico from 2006 to 2050 (considering only 2 comorbidities: diabetes and hypertension) will be much higher than the health care system can stand, jeopardizing the health and well-being of the population.63,64 Early intervention is essential, because less weight change is needed at younger ages to achieve a healthy weight than the amount of weight loss necessary at older ages.65 Moreover, it has been acknowledged that the ability to estimate a national impact systematically and cost-effectiveness of implementation of childhood obesity interventions enables comparison within and across sector-specific interventions to inform primary prevention investment.66
CONCLUSION
Efforts to identify vulnerable populations and implementation barriers among different populations are needed in Mexico. Long-term nationwide interventions and comprehensive recommendations that can guide health professionals and other stakeholders in the obesity treatment at individual and community levels are essential to change the upward trends in obesity prevalence. Such efforts need to be comprehensive, multidisciplinary, and target several risk factors in the long term. This review is part of a broader project aiming to synthesize and use data to comprehend the extent, nature, effects, and costs of childhood or adolescent obesity in Mexico (ie, the COMO Project).9 Because of the increasing levels of obesity in Mexico, every action measuring or attempting to tackle obesity in Mexico should be acknowledged. Any effort should be considered an experiment, where effects must be documented and evaluated to benefit every other initiative or strategy. Such efforts need to enhance their methodological quality, including different settings, stakeholders, and target different health risk behaviors. Interventions should be designed using a comprehensive approach within the national sociopolitical, cultural, and economic contexts.
Supporting Information
The following Supporting Information is available through the online version of this article at the publisher’s website.
Appendices 1 and 2 (which contain Table S1 and Table S2) are supplied as supporting information.
Supplementary Material
Acknowledgements
Author contributions. M.A.-M. and C.F.M.-G. conceptualized and lead the COMO Project. All the authors contributed significantly to the data collection, or data interpretation and analysis; participated in the writing and critical revision of the article; and read and approved the versions submitted to the journal.
Funding. No funding was received to do this work.
M.A.-M. is currently funded by the Scottish Government's Rural and Environment Science and Analytical Services Division.
Declaration of interest. Y.Y.G.-G. received funding from Bonafont to present findings at a congress in 2016 and funding from Abbott in 2020 to write 2 books’ chapters. The other authors have no conflict of interest to declare.
References
- 1. Aceves-Martins M, Llauradó E, Tarro L, et al. Obesity-promoting factors in Mexican children and adolescents: challenges and opportunities. Global Health Action. 2016;9:29625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Instituto Nacional de Salud Pública. Encuesta Nacional de Salud y Nutrición 2018. Presentación de resultados. 2018. Available at: https://ensanut.insp.mx/encuestas/ensanut2018/doctos/informes/ensanut_2018_presentacion_resultados.pdf. Accessed October 20, 2020.
- 3.World Obesity Federation. Global Obesity Observatory. 2019. Available at: https://www.worldobesitydata.org/map/overview-children. Accessed October 20, 2020
- 4.Organisation for Economic Co-operation and Development. Obesity update 2017. Available at: https://www.oecd.org/els/health-systems/Obesity-Update-2017.pdf. Accessed October 20, 2020.
- 5. Wang Y, Lim H.. The global childhood obesity epidemic and the association between socio-economic status and childhood obesity. Int Rev Psychiatry. 2012;24:176–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ho M, Garnett SP, Baur L, et al. Effectiveness of lifestyle interventions in child obesity: systematic review with meta-analysis. Pediatrics. 2012;1;130:e1647–e1671. [DOI] [PubMed] [Google Scholar]
- 7. McGovern L, Johnson JN, Paulo R, et al. Treatment of pediatric obesity: a systematic review and meta-analysis of randomised trials. J Clin Endocrinol Metabol. 2008;1;93:4600–4605. [DOI] [PubMed] [Google Scholar]
- 8. Axon E, Atkinson G, Richter B, et al. Drug interventions for the treatment of obesity in children and adolescents. Cochrane Database Syst Rev. 2016;11:CD012436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Aceves-Martins M. “COMO Project Perspectives.” 2021. Available at: https://www.comoprojectmx.com/perspectives. Accessed March 24, 2021.
- 10.National Institute for Health Research. International Prospective Register of Systematic Reviews (PROSPERO). Available at: https://www.crd.york.ac.uk/prospero. Accessed October 23, 2019.
- 11.Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Available at: http://prisma-statement.org/. Accessed October 15, 2020.
- 12.Effective Public Health Practice Project. Quality Assessment Tool for Quantitative Studies. 2010. Available at: https://merst.ca/ephpp/. Accessed October 15, 2020.
- 13.Equator Network. Template for intervention description and replication (TIDieR) checklist Available at: https://www.equator-network.org/reporting-guidelines/tidier/. Accessed October 15, 2020.
- 14. Armstrong R, Waters E, Doyle J.. Reviews in public health and health promotion. Chapter 21. In: Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. Updated. London, UK: The Cochrane Collaboration; 2011. Available at: www.cochrane-handbook.com. [Google Scholar]
- 15. Higgins JP, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons; 2019.
- 16. Higgins JP, Altman D.. Imputing standard deviations for changes from baseline. In: Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Book Series. Chichester, UK: Wiley; 2008. [Google Scholar]
- 17. Aceves-Martins M, Llauradó E, Tarro L, et al. Effectiveness of social marketing strategies to reduce youth obesity in European school-based interventions: a systematic review and meta-analysis. Nutr Rev. 2016; 1;74:337–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rajjo T, Mohammed K, Alsawas M, et al. Treatment of pediatric obesity: an umbrella systematic review. J Clin Endocrinol Metabol. 2017;102:763–775. [DOI] [PubMed] [Google Scholar]
- 19. Hedges LV, Olkin I.. Statistical Methods for Meta-Analysis. San Diego, CA; Academic Press; 1985. [Google Scholar]
- 20. Ceballos-Gurrola O, Acosta RL, Martínez MA, et al. Impacto de un programa de salud sobre perfil metabólico y autoconcepto en adolescentes con obesidad. Retos. 2020;38:452–458. [Google Scholar]
- 21. Díaz RG, Esparza-Romero J, Moya-Camarena SY, et al. Lifestyle intervention in primary care settings improves obesity parameters among Mexican youth. J Am Diet Assoc. 2010;110:285–290. [DOI] [PubMed] [Google Scholar]
- 22. Elizondo‐Montemayor L, Gutierrez NG, Moreno DM, et al. School‐based individualised lifestyle intervention decreases obesity and the metabolic syndrome in Mexican children. J Hum Nutr Diet. 2013;26:82–89. [DOI] [PubMed] [Google Scholar]
- 23. Elizondo-Montemayor L, Moreno-Sànchez D, Gutierrez NG, et al. Individualised tailor-made dietetic intervention program at schools enhances eating behaviors and dietary habits in obese Hispanic children of low socioeconomic status. ScientificWorldJournal 2014;2014:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Escalante-Izeta E, Vergara A, Parra A, et al. “Kids in motion” program for obese Mexican population: a case report: PO2304. Ann Nutr Metabol 2013;63:1368–1369. [Google Scholar]
- 25. García-Morales LM, Berber A, Macias-Lara CC, et al. Use of sibutramine in obese Mexican adolescents: a 6-month, randomized, double-blind, placebo-controlled, parallel-group trial. Clin Ther. 2006;28:770–782. [DOI] [PubMed] [Google Scholar]
- 26. Garibay-Nieto N, Queipo-García G, Alvarez F, et al. Effects of conjugated linoleic acid and metformin on insulin sensitivity in obese children: randomized clinical trial. J Clin Endocrinol Metab. 2017;102:132–140. [DOI] [PubMed] [Google Scholar]
- 27. González-Heredia R, Castañeda-Sánchez O, López-Morales CM, et al. Intervención familiar para el manejo de sobrepeso y obesidad en escolares. Rev Med Inst Mex Seguro Soc. 2014;52:S74–7. [PubMed] [Google Scholar]
- 28. Hall-López JA, Martínez PY, Bernal AZ, et al. Efecto de un programa de actividad física de moderada a vigorosa de diez meses sobre el Vo2máx y el porcentaje de grasa corporal en niños con sobrepeso y obesidad. MHSalud. 2017;14:6. [Google Scholar]
- 29. Huang F, Del‐Río‐Navarro BE, de Castro GT, et al. Weight loss induced by 6‐month lifestyle intervention improves early endothelial activation and fibrinolysis in obese adolescents. Child Care Health Dev. 2011;37:377–384. [DOI] [PubMed] [Google Scholar]
- 30. Huang F, Del-Río-Navarro B, Pérez-Ontivero J, et al. Effect of weight loss induced by 6-month lifestyle intervention on adipokines in obese adolescents: 27/2. Nutrition in the Prevention of Non-Communicable Diseases. Ann Nutr Metabol 2011;58:306–307. [Google Scholar]
- 31. Huang F, Del-Río-Navarro BE, Ontiveros JA, et al. Changes in ghrelin and asymmetrical dimethylarginine in obese Mexican adolescents after six-month lifestyle intervention. Endocrine. 2013;43:603–610. [DOI] [PubMed] [Google Scholar]
- 32. Jimenez JA, Castaneda JA.. Situation of bariatric surgery in Mexican teenagers by surgical group. Bariatric surgery in children, adolescents and young adults. Obes Surg. 2017;1:423–423. [Google Scholar]
- 33. Laguna-Alcaraz AD, Mejía-Rodríguez O, Rendón-Paredes AL, et al. Impact of a comprehensive intervention to families with teenage sons with overweight and obesity in a primary care: a case report. Diabetes Metab Syndr. 2017;11:S195–200. 10.1016/j.dsx.2016.12.031 [DOI] [PubMed] [Google Scholar]
- 34. López‐Alarcón M, Inda‐Icaza P, Márquez‐Maldonado MC, et al. A randomized control trial of the impact of LCPUFA‐ω3 supplementation on body weight and insulin resistance in pubertal children with obesity. Pediatr Obes. 2019;14:e12499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. López-Alarcón M, Zurita-Cruz JN, Torres-Rodríguez A, et al. Mindfulness affects stress, ghrelin, and BMI of obese children: a clinical trial. Endocr Connect. 2020;9:163–172. 10.1530/EC-19-0461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Luna-Ruiz MÁ, Rangel-Vázquez D, Guizar-Mendoza JM, et al. Modificación de factores de riesgo para desarrollar diabetes mellitus tipo 2 en escolares obesos. Rev Med Inst Mex Seguro Soc. 2007;45:53–62. [PubMed] [Google Scholar]
- 37. Martin-Mosqueda CA, García RR.. Resultados preliminares de un programa de tratamiento integral para la obesidad en niños Mexicanos. Rev Mex Invest Psicolog 2012;1:50–57. [Google Scholar]
- 38. Moran S, Mina A, Duque X, et al. Effect of a lifestyle intervention in children with obesity and nonalcoholic fatty liver disease. Top Clin Nutr. 2017;32:15–26. 10.1097/TIN.0000000000000094 [DOI] [Google Scholar]
- 39. Pompa-Guajardo EG, Castro L, Garza ML.. Intervención y seguimiento psicológico en un campamento de verano de niños con sobrepeso y obesidad en el norte de México. Interacción Perspect Rev Trabajo Soc. 2018;8:150–166. [Google Scholar]
- 40. Rodríguez-Morán M, Mendoza-Ávila E, Cumplido-Fuentes A, et al. Terapia cognitivo-conductual en el manejo integral de la obesidad en adolescentes. Rev Med Inst Mex Seguro Soc 2014;52:S68–73. [PubMed] [Google Scholar]
- 41. Romero-Pérez EM, González-Bernal JJ, Soto-Cámara R, et al. Influence of a physical exercise program in the anxiety and depression in children with obesity. IJERPH. 2020;17:4655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rosado JL, del R Arellano M, Montemayor K, et al. An increase of cereal intake as an approach to weight reduction in children is effective only when accompanied by nutrition education: a randomised controlled trial. Nutr J. 2008;7:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Rosas-Nexticapa M, Caballero-Rodríguez DA, Herrera-Meza S, et al. Supplementation effect of omega-3 fatty acids in overweight and obese Mexican schoolchildren. Interciencia. 2017;42:698–704. [Google Scholar]
- 44. Sáenz NE, Gallegos EC.. Efecto de intervención física sobre alimentación y actividad física en adolescentes Mexicanos con obesidad . Texto Contexto Enfermagem. 2004;13:17–25. [Google Scholar]
- 45. Santiago Lagunes LM, Perea Martínez A, López Navarrete GE, et al. Obesity in childhood and adolescence. Evaluation of a therapeutic model based on a frequent clinical intervention. 51st Annual Meeting of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition. Abstract A-968–0019. 01191.
- 46. De Sanchez ES. Relationship of leptin concentrations with insulin, glucose, lipoproteins, cholesterol, triglycerides, and body mass index in obese children in Monterrey, Mexico (doctoral dissertation). College of health Sciences, The Texas Womans’s University; 2004.
- 47. Velázquez López L, Rico Ramos JM, Torres Tamayo M, et al. Impacto de la educación nutricional sobre alteraciones metabólicas en niños y adolescentes con obesidad. Endocrinol Nutr. 2009;56:441–446. [DOI] [PubMed] [Google Scholar]
- 48. Velázquez-López L, Santiago-Díaz G, Nava-Hernández J, et al. Mediterranean-style diet reduces metabolic syndrome components in obese children and adolescents with obesity. BMC Pediatr. 2014;14:175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Violante-Ortíz R, Del-Rio-Navarro BE, Lara-Esqueda A, et al. Use of sibutramine in obese Hispanic adolescents. Adv Therapy. 2005;22:642–649. [DOI] [PubMed] [Google Scholar]
- 50. Virgen Ortiz A, Muñiz Murguía JD, La Mota AJ, et al. Efectos de programa de intervención en sobrepeso y obesidad de niños escolares en Colima, México. Salud Publica Mex. 2007;49:389–391. [DOI] [PubMed] [Google Scholar]
- 51. Wilfley DE, Staiano AE, Altman M, et al. ; Improving Access and Systems of Care for Evidence‐Based Childhood Obesity Treatment Conference Workgroup. Improving access and systems of care for evidence‐based childhood obesity treatment: conference key findings and next steps. Obesity. 2017;25:16–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Loveman E, Al ‐Khudairy L, Johnson RE, et al. Parent‐only interventions for childhood overweight or obesity in children aged 5 to 11 years. Cochrane Database Syst Rev. 2015;12:CD012008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Trier C, Dahl M, Stjernholm T, et al. Effects of a family-based childhood obesity treatment program on parental weight status. PLoS One. 2016;11:e0161921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Cauchi D, Glonti K, Petticrew M, et al. Environmental components of childhood obesity prevention interventions: an overview of systematic reviews. Obes Rev. 2016;17:1116–1130. [DOI] [PubMed] [Google Scholar]
- 55. Mostert CM. Sugar-sweetened beverage tax in Mexico. Health Aff (Millwood). 2017;36:1144. [DOI] [PubMed] [Google Scholar]
- 56. Colchero MA, Rivera-Dommarco J, Popkin BM, et al. In Mexico, evidence of sustained consumer response two years after implementing a sugar-sweetened beverage tax. Health Aff (Millwood). 2017;36:564–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Kaufer-Horwitz M, Tolentino-Mayo L, Jáuregui A, et al. A front-of-pack labelling system for food and beverages for Mexico: a strategy of healthy decision-making. Salud Publica Mex. 2018;60:479–486. [DOI] [PubMed] [Google Scholar]
- 58.Secretaría de Salud. CENETEC. Guía de Práctica Clínica. Prevención y diagnóstico de sobrepeso y obesidad en niños y adolescentes en el primer nivel de atención. Available at: www.cenetec.salud.gob.mx/interior/gpc.html. Accessed November 22, 2019.
- 59.Secretaría de Salud. CENETEC. Intervención dietética. Paciente con obesidad – Cenetec. Available at: http://www.cenetec-difusion.com/CMGPC/IMSS-684-13/ER.pdf. Accessed March 24, 2021.
- 60.Secretaría de Salud. CENETEC. Tratamiento del sobrepeso y la obesidad exógena. GPC. Guía de Práctica Clínica. Available at: http://www.cenetec.salud.gob.mx/descargas/gpc/CatalogoMaestro/046_GPC_ObesidadAdulto/IMSS_046_08_EyR.pdf. Accessed March 24, 2021.
- 61.US Preventive Services Task Force. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. Pediatrics. 2010;125:361–367. [DOI] [PubMed] [Google Scholar]
- 62. Whitlock EP, O'Connor EA, Williams SB, et al. Effectiveness of weight management interventions in children: a targeted systematic review for the USPSTF. Pediatrics. 2010;125:e396–418. [DOI] [PubMed] [Google Scholar]
- 63. Ortega-Cortés R. Costos económicos de la obesidad infantil y sus consecuencias. Rev Med Inst Mex Seguro Soc 2014;52:8–11. [PubMed] [Google Scholar]
- 64. Garduño-Espinosa J, Morales-Cisneros G, Martínez-Valverde S, et al. Una mirada desde los servicios de salud a la nutrición de la niñez Mexicana. III. Carga económica y en salud de la obesidad en niños Mexicanos. Proyecciones de Largo Plazo. Bol Med Hosp Infant Mex 2008;65:49–56. [Google Scholar]
- 65. Goldschmidt AB, Wilfley DE, Paluch RA, et al. Indicated prevention of adult obesity: how much weight change is necessary for normalisation of weight status in children? JAMA Pediatr 2013;167:21–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Cradock AL, Barrett JL, Kenney EL, et al. Using cost-effectiveness analysis to prioritise policy and programmatic approaches to physical activity promotion and obesity prevention in childhood. Prev Med. 2017;95:S17–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.