Abstract
Background
The COVID-19 pandemic and the subsequent lockdown have a strong impact on health and health behaviours, such as alcohol consumption. Although there is some evidence of an overall decline in alcohol consumption during the lockdown, studies also show an increase in risky drinking patterns, e.g. solitary drinking, and differences between subgroups of individuals, e.g. depending on their living arrangement. Yet most studies rely on cross-sectional designs with retrospective questions, and small samples.
Methods
A longitudinal study was conducted using 13 waves of the COVID-Questionnaire within the Lifelines cohort from the northern Netherlands (n = 63,194). The outcome was alcohol consumption (glasses per week) between April 2020 and July 2021. Linear fixed-effects models were fitted to analyse trends in alcohol consumption, and these were compared with pre-COVID drinking levels. Moreover, the role of living arrangement and feelings of social isolation as potential moderators was tested.
Results
Alcohol consumption during the pandemic was lower than in previous years, and the seasonal pattern differed from the pre-COVID one, with levels being lower when lockdown measures were stricter. Moreover, the seasonal pattern differed by living arrangement: those living alone saw a relative increase in drinking throughout tight lockdown periods, whereas those living with children showed the strongest increase during the summer. Social isolation showed a weaker moderation effect.
Conclusions
Overall alcohol levels were down in the pandemic, and in particular during strict lockdowns. Those living on their own and those who felt more isolated reacted more strongly to the lockdown, the longer it lasted.
Keywords: Covid-19, Alcohol consumption, Isolation, Living arrangement, Lockdown
1. Introduction
The COVID-19 pandemic, as well as the regulations to control the spread of the virus, represent a “natural experiment”, as they abruptly affected a vast majority of the population world-wide (Bierman et al., 2021), who was suddenly exposed to unprecedented restrictions (i.e. lockdown) and fear of viral infection. Although its consequences in terms of impact on health (behaviours) are still to be fully grasped, there is some evidence that almost two years of lockdown -defined as all preventive measures implemented to control the spread of the virus- had undesirable effects on individuals, such as increased feelings of loneliness, stress and mental health issues (Chandola et al., 2020, Czeisler et al., 2021, Grace, 2021). Moreover, there is evidence showing changes in health behaviours, such as alcohol consumption (Knell et al., 2020, Roberts et al., 2021).
Alcohol consumption, particularly in high doses, has large public health consequences, as it is associated with chronic medical conditions, such as cardiovascular diseases (Mackenbach et al., 2015), cancer, and mental disorders (Rehm et al., 2010). Alcohol consumption is responsible for 6% of all deaths worldwide, and for more than 25% of deaths among young men aged 15–29 years in the E.U (Collins, 2016). Moreover, it has been rated as one of the four most harmful drugs on a population level (Nutt et al., 2010, Van Amsterdam et al., 2010), as it is also associated with undesirable social outcomes, such as higher rates of violent behaviour and traffic accidents (Rehm et al., 2010, de Goeij et al., 2015).
Several studies have analysed changes in alcohol consumption during the first few months of the pandemic, showing mixed results: while some show an overall decrease in alcohol levels compared with the pre-COVID period (Panagiotidis et al., 2020, Sallie et al., 2020, Wardell et al., 2020, Valente et al., 2021, Wang et al., 2021) -in some cases relying on objective measurements, such as wastewater analyses (Bade et al., 2021)-, others show an increase (Grigoletto et al., 2020, Rogers et al., 2020, Roberts et al., 2021). These contrasting results may be due to different pathways leading to alcohol consumption. On the one hand, alcohol consumption has been shown to be associated with positive affect and social gatherings (Cooper et al., 2016). From this perspective, a decrease in alcohol consumption could be explained by lower alcohol availability due to the closure of bars and restaurants (Roberts et al., 2021), as well as restrictions on social gatherings that kept “social drinking” -and, therefore, peer pressure to drink as well- at minimum levels. In turn, a possible increase could be viewed as alcohol acting as a coping mechanism (Rehm et al., 2020, Rogers et al., 2020) for increased feelings of loneliness and psychological distress.
Moreover, studies that looked beyond the amount of alcohol consumed during the COVID-19 pandemic found an increase in specific drinking patterns, such as higher drinking frequency (Wardell et al., 2020, White et al., 2020, Niedzwiedz et al., 2021, Thompson et al., 2021), binge drinking (Grigoletto et al., 2020, Niedzwiedz et al., 2021) and solitary drinking (Panagiotidis et al., 2020, Ramalho, 2020, Wardell et al., 2020). The latter has been shown to lead to the development of alcohol-related problems, such as alcohol abuse and dependence (Skrzynski and Creswell, 2020), especially when drinking is used as a coping mechanism against stress (Dawson et al., 2005, Corbin et al., 2013), anxiety (Rehm et al., 2010), or loneliness (Corbin et al., 2020, Niedzwiedz et al., 2021, Oksanen et al., 2021).
However, there are important gaps in the literature that need to be addressed. First, the vast majority of studies use cross-sectional data and rely on retrospective questions (Panagiotidis et al., 2020, Vanderbruggen et al., 2020, Wardell et al., 2020), and therefore do not capture changes over time. This is particularly relevant because time-related issues, such as the duration or the strictness of the lockdown, as well as the period of the year, may play a role in shaping drinking patterns (Prati and Mancini, 2021).
Second, most studies do not examine heterogeneity in the impact of the lockdown on drinking patterns. Yet, there may be differences between groups of individuals. For instance, the living arrangements in which individuals faced the lockdown -i.e. whether they lived alone or a shared a household with partner and/or family- may be relevant (Corbin et al., 2020, Skrzynski and Creswell, 2020). Accordingly, studies analysing the impact of the lockdown on mental health have shown that the effect was stronger for individuals who lived alone (Ahrens et al., 2021), whereas others have shown that those with children in the household during the lockdown suffered higher stress levels, which may have exposed them to increased alcohol consumption (Villanueva-Blasco et al., 2021).
Moreover, the subjective element of whether individuals feel lonely or isolated may be a key element in explaining differences in the response to the lockdown (Chandola et al., 2020, Ramalho, 2020, Wardell et al., 2020). Although some cross-sectional studies have pointed in that direction (Gritsenko et al., 2020, Newby et al., 2020, Sallie et al., 2020, Yazdi et al., 2020), to the best of our knowledge no longitudinal study so far has provided evidence on how living arrangements and feelings of social isolation have affected alcohol consumption during the lockdown.
This study relies on a large sample and a longitudinal design and aims at testing: (1) whether the lockdown had an effect on alcohol consumption levels; (2) whether this effect was different for those who lived alone compared with those who lived with others, and (3) whether this effect differed between individuals who felt isolated and those who did not.
2. Methods
The Lifelines COVID-19 Questionnaire was launched within the Lifelines Cohort Study, a large prospective population-based prospective cohort study and biobank in the three northern provinces of the Netherlands, examining in a three-generation design the biomedical, socio-demographic, behavioural, physical and psychological factors contributing to the health and disease of 167,729 individuals living in the north of the Netherlands (Hoveling et al., 2021) -composition and characteristics of the sample have been discussed elsewhere (Klijs et al., 2015, Scholtens et al., 2015).
In order to assess the effects of the pandemic, the attitudes towards the COVID-19 regulations, and the (health) behaviours of the population of study, the Lifelines COVID-19 cohort was developed (n = 76,795) (Mc Intyre et al., 2021). Participants were asked to fill out detailed web-based questionnaires about their physical and mental health, living situation, and health behaviours between late March 2020 and July 2021 -first, on a biweekly basis, after June 2020 on a monthly basis-, with a total of 24 waves. For the purpose of our study, 13 waves of COVID-19 questionnaire panel data were used (those with questions on alcohol consumption), covering the period between April 2020 and July 2021. Our final sample consists of 451,128 observations nested in 63,194 individuals (61.2% female; mean age 57.2 years). Moreover, data of the same participants from three previous waves of the Lifelines cohort study that included information on alcohol consumption -waves 1, 4 and 5- were used for comparative purposes.
2.1. Measurements
Outcome. Alcohol consumption: Alcohol consumption was assessed from wave 5 (April 2020) until wave 24 (July 2021), with 13 measurements in total. Questions referred to the amount of alcohol consumed: “How many glasses of alcohol did you drink in the past 7 days?” (“in the past 14 days” from wave 7 onwards). In the Netherlands, a standard glass is defined as containing roughly 10 g of alcohol (Gezondheidsraad, Health Council of the Netherlands, 2015). In order to harmonize the data, the average weekly alcohol consumption score (in glasses per week) was calculated (the same variable was created for previous waves of the Lifelines cohort). The scores range from 0 to 70 (all values higher than 70 were recoded to 70).
Independent variable. COVID lockdown: a variable “Days since first lockdown (15th of March, 2020)” was created and converted into a categorical variable with categories coinciding with every month of the observation period (category 1 =April 2020; category 24 = July 2021). Due to the timing of Lifelines assessments, some months had very few observations (e.g. August 2020), or no observations at all (e.g. February 2021). These categories were merged with the previous month (e.g. “July/August 2020″) or dropped (February 2021).
Time-varying covariates. Living arrangements were captured by a dichotomous variable: “lives alone” / “lives in a shared household”, based on the question “do you have one or more housemates?”. Additionally, sensitivity analyses distinguishing between “adult(s) with children (<18) living at home”, and “adults without children living at home” were carried out.
Feelings of social isolation were measured by the following question: “How socially isolated have you felt in the last 14 days?”, with responses ranging from 1 (“not isolated”) to 10 (“extremely isolated”). For the descriptive analyses, a dichotomous version of this variable was created, assessing “low isolation” (scores 1–6) and “high isolation” (≥7). This question was not asked in wave 11 -mid-end of July-, which created a large number of missing values. These were imputed by taking the last observation available (n = 33,867) from wave 10 -early to mid-July. Alternatively, they were also imputed by means of multiple imputation (MICE). Yet, as results were practically identical, the models presented rely on the first method.
Employment status was a categorical variable, comparing “employed” -including full- and part-time as well as freelancers- (reference category), “retired”, “unemployed”, “disabled”, and “others” -which included students, homemakers, those on maternity leave, etc.–.
Time-constant confounders. Although they drop out of the fixed-effects models, we use the following additional variables to describe the sample: Gender (male/female); Age at baseline, categorized in age groups (<40, 41–50, 51–60, 61–70 and >70); and Socioeconomic status (SES), assessed through educational level: a variable, based on the Dutch educational system, was created with three categories: “low” (up to general secondary education), “middle” (secondary vocational education, or higher general and pre-university education), and “high” (higher professional education or university education).
2.2. Statistical analyses
Our analytical strategy was based on the following steps: first, linear regression models (OLS) accounting for fixed-effects (FE) were fitted, with weekly alcohol consumption as the outcome variable and the lockdown period as a main independent variable. Additionally, employment status was accounted for as a potential time-varying confounder (whereas time-constant confounders dropped out of the models). FE models focus on the changes within individuals throughout the observation period, net of time-constant unobserved confounding. Thus, they allow us to infer the impact of the lockdown on alcohol consumption. Based on this FE model, predicted margins estimated alcohol consumption levels at every time point. Sensitivity analyses with FE Poisson models were carried out, due to the large number of zero values of the outcome. As shown in the appendix -see table A2 and figure A2 -, the patterns are practically identical, although the coefficients differ because Poisson models are expressed different units, which makes them harder to interpret. In contrast, an advantage of OLS models is that they allow to interpret the coefficients in the same units of the outcome. For this reason, we decided to stick to OLS models.
Second, alcohol consumption during the lockdown was compared with alcohol consumption in previous years among the same population. For that purpose, data from the Lifelines Cohort (observations collected from 2007 until 2018) were used. Alcohol consumption during this period was estimated by means of cross-sectional pooled OLS models, in which alcohol consumption was regressed on the variable “month of the observation”, using the same categories as the independent variable “lockdown period”, for comparative purposes. Additionally, “year of observation” was accounted for in the models. Posterior margins predicted the estimated average alcohol consumption for each month, thus making results comparable with the ones from the COVID cohort.
Third, back to the COVID cohort, a potential role of living arrangement as moderator was tested by adding interactions between living arrangement and each time point of the lockdown period to the main-effects FE model. Additionally, the moderating role of subjective feelings of isolation was tested by adding an interaction between social isolation and the lockdown period. Again, based on this model, the predicted alcohol consumption at each time point for these subgroups of individuals was estimated. All analyses were carried out with Stata 13.
3. Results
The descriptive analyses of the main variables of interest by alcohol consumption at baseline are shown in Table 1. Women report much lower alcohol consumption than men (3.14 versus 5.68 glasses/week on average, respectively). Alcohol consumption is higher among older age groups (with the exception of those over 70), and individuals under 40 report the lowest consumption. The lower educated report the lowest drinking levels, whereas the higher educated report the highest (3.88 and 4.55 glasses/week respectively). As for employment status, the retired report the highest drinking (4.34), followed by the employed (4.26) and the unemployed and the disabled (3.67 and 3.05 respectively). Finally, those living alone, as well as those reporting higher levels of social isolation report lower alcohol consumption (3.77 and 4.06 respectively, compared to 4.18 and 4.14 among their counterparts).
Table 1.
Main variables of interest by alcohol consumption at baseline (n = 45,384).
| N (%) | Glasses/week (mean) | |
|---|---|---|
| Gender | ||
| Male | 17,658 (38.91%) | 5.68 |
| Female | 27,726 (61.09%) | 3.14 |
| Age group | ||
| < 40 | 5037 (11.10%) | 3.69 |
| 41–50 | 7873 (17.35%) | 3.85 |
| 51–60 | 16,149 (35.58%) | 4.11 |
| 61–70 | 10,292 (22.68%) | 4.64 |
| > 70 | 6033 (13.29%) | 4.02 |
| Educational Attainment | ||
| Low | 12,077 (27.24%) | 3.88 |
| Middle | 16,881 (38.08%) | 3.94 |
| High | 15,376 (34.68%) | 4.55 |
| Employment Status | ||
| Employed | 27,057 (59.63%) | 4.26 |
| Retired | 12,038 (26.53%) | 4.34 |
| Unemployed | 1440 (3.17%) | 3.67 |
| Disabled | 1098 (2.42%) | 3.05 |
| Other | 3743 (8.25%) | 2.99 |
| Living arrangement | ||
| Living with others | 39,100 (86.17%) | 4.18 |
| Living alone | 6274 (13.83%) | 3.77 |
| Social Isolation | ||
| Low isolation (score <7) | 35,967 (81.59%) | 4.14 |
| High isolation (score ≥7) | 8114 (18.41%) | 4.06 |
3.1. Alcohol consumption during the lockdown
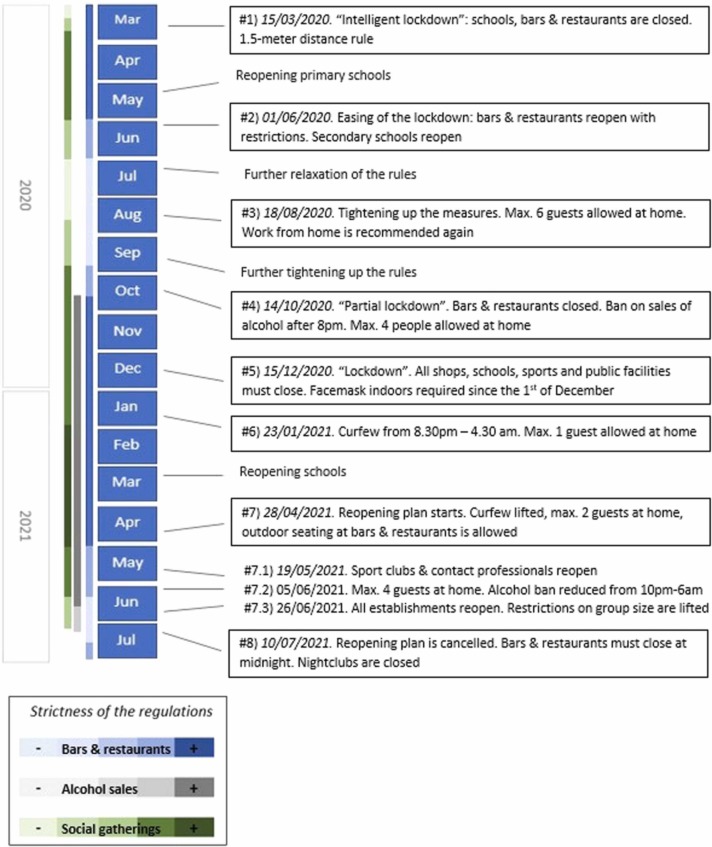
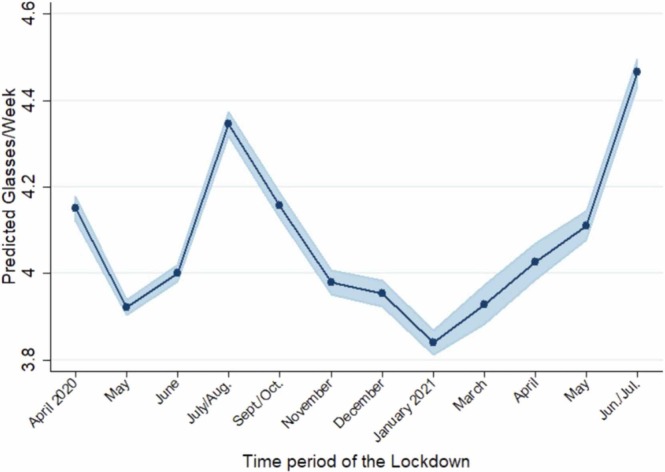
An overview of the most relevant preventive measures implemented in the Netherlands during the observation period is shown in Fig. 1 (for a more exhaustive timeline see Table A1 in the appendix). The main effects of the lockdown period on alcohol consumption are shown in Table 2 (Model 0). Based on this model, predicted drinking levels during the whole lockdown period were estimated, as shown in Fig. 2.
Fig. 1.
Timeline of COVID-19 preventive measures implemented in the Netherlands (March 2020 – July 2021).1
Table 2.
Effects of the lockdown period on alcohol consumption. Main effects (Model 0) and interaction terms (Models 1 & 2). OLS fixed-effects modelsa.
| Model 0 (n = 451,064) |
Model 1 (n = 451,052) |
Model 2 (n = 450,029) |
||||
|---|---|---|---|---|---|---|
| β | CI 95% | β | CI 95% | β | CI 95% | |
| Living arrangement (shared household) | ||||||
| Lives alone | -0.03 | (−0.13 to 0.06) | -0.04 | (−0.13 to 0.06) | ||
| Lockdown Period (April 2020) | ||||||
| May | -0.23 * * | (−0.26 to −0.19) | -0.23 * * | (−0.27 to −0.19) | -0.24 * * | (−0.32 to −0.17) |
| June | -0.15 * * | (−0.18 to −0.11) | -0.15 * * | (−0.19 to −0.12) | -0.08 * | (−0.16 to −0.01) |
| July/August | 0.20 * * | (0.16–0.24) | 0.21 * * | (0.17–0.26) | 0.29 * * | (0.21–0.37) |
| September/October | 0.01 | (−0.03 to 0.05) | -0.01 | (−0.06 to 0.03) | 0.04 | (−0.05 to 0.12) |
| November | -0.17 * * | (−0.21 to −0.13) | -0.18 * * | (−0.23 to −0.14) | -0.09 * | (−0.18 to −0.01) |
| December | -0.20 * * | (−0.24 to −0.15) | -0.21 * * | (−0.26 to −0.17) | -0.17 * * | (−0.26 to −0.08) |
| January 2021 | -0.31 * * | (−0.35 to −0.27) | -0.35 * * | (−0.40 to −0.31) | -0.30 * * | (−0.39 to −0.21) |
| March | -0.22 * * | (−0.27 to −0.17) | -0.26 * * | (−0.32 to −0.20) | -0.20 * * | (−0.32 to −0.09) |
| April | -0.12 * * | (−0.17 to −0.07) | -0.16 * * | (−0.22 to −0.10) | -0.15 * * | (−0.26 to −0.04) |
| May | -0.04 | (−0.08 to 0.00) | -0.07 * * | (−0.12 to 0.02) | 0.01 | (−0.07 to 0.10) |
| June/July | 0.31 * * | (0.27–0.36) | 0.32 * * | (0.28–0.37) | 0.48 * * | (0.39–0.56) |
| Lockdown ## Living arrangement | ||||||
| May##Alone | 0.02 | (−0.08 to 0.12) | 0.02 | (−0.08 to 0.12) | ||
| June##Alone | 0.05 | (−0.05 to 0.15) | 0.06 | (−0.04 to 0.16) | ||
| July/August##Alone | -0.06 | (−0.18 to 0.04) | -0.05 | (−0.17 to 0.06) | ||
| September/October##Alone | 0.13 * | (0.01–0.24) | 0.13 * | (0.01–0.25) | ||
| November##Alone | 0.10 | (−0.01 to 0.22) | 0.10 | (−0.01 to 0.23) | ||
| December##Alone | 0.14 * | (0.02–0.26) | 0.14 * | (0.02–0.27) | ||
| January 2021##Alone | 0.34 * * | (0.22–0.46) | 0.34 * * | (0.22–0.46) | ||
| March##Alone | 0.27 * * | (0.11–0.42) | 0.27 * * | (0.12–0.42) | ||
| April##Alone | 0.25 * * | (0.10–0.40) | 0.25 * * | (0.10–0.40) | ||
| May##Alone | 0.22 * * | (0.10–0.35) | 0.23 * * | (0.11–0.36) | ||
| June/July##Alone | -0.04 | (−0.16 to 0.08) | -0.02 | (−0.14 to 0.10) | ||
| Social Isolation | 0.004 | (−0.01 to 0.02) | ||||
| Lockdown ## Isolation | ||||||
| May##Isolation | 0.00 | (−0.01 to 0.02) | ||||
| June##Isolation | -0.02 * * | (−0.04 to −0.01) | ||||
| July/August##Isolation | -0.02 * | (−0.04 to 0.00) | ||||
| September/October##Isolation | -0.01 | (−0.03 to 0.01) | ||||
| November##Isolation | -0.03 * | (−0.05 to −0.01) | ||||
| December##Isolation | -0.01 | (−0.03 to 0.01) | ||||
| January 2021##Isolation | -0.01 | (−0.03 to 0.01) | ||||
| March##Isolation | -0.01 | (−0.04 to 0.10) | ||||
| April##Isolation | 0.00 | (−0.03 to 0.02) | ||||
| May##Isolation | -0.03 * | (−0.05 to −0.01) | ||||
| June/July##Isolation | -0.06 * * | (−0.09 to −0.04) | ||||
* p-value < 0.05; ** p-value < 0.01.
All models account for employment status. Model 0 accounts for “lockdown period”; Model 1 adds the interaction between “lockdown period” and “living arrangement”; Model 2 adds the interaction between “lockdown period” and “feelings of isolation”.
Fig. 2.
Alcohol consumption during the COVID lockdown (April 2020 – July 2021). Predictive margins based on fixed-effects linear regression models.
Alcohol consumption levels tend to decrease during the first months of the so-called “intelligent lockdown”, when bars and restaurants were closed and social interactions reduced to a minimum. At the beginning of June, there is an inflection point and a second phase starts, in which alcohol consumption shows a steep increase, with a peak around July-August, which could be attributed to the summer holidays season. However, it is also remarkable that, on June the 1st, most lockdown measures were relaxed and bars and restaurants were allowed to open again, as shown in Fig. 1 (#2).
By the end of August, a third phase starts with alcohol consumption steadily decreasing again. At that time, the Dutch government announced a renewed tightening of the measures due to the increasing number of infections (#3 in Fig. 1). By mid-October, a ban on alcohol sales between 8 pm and 7 am was enacted (#4), as alcohol consumption was considered to be hindering the compliance with social distancing rules. Results show that alcohol consumption decreased throughout the autumn, reaching its lowest levels after the Christmas season. In January 2021 the lockdown measures were tightened again and a curfew was imposed (#6), due to the rising concern about the spread of new virus variants.
Finally, a fourth phase starts during Spring 2021, with an increase in alcohol consumption before the strict lockdown measures were relaxed by the end of April. Alcohol consumption steadily increases during early summer, when restrictions are lifted and vaccination starts to be massive, until the end of the observation period (end of July 2021). Although a new set of measures were implemented by mid-July (#8), its effects are unlikely to be captured by our data, since the observation period ended shortly after.
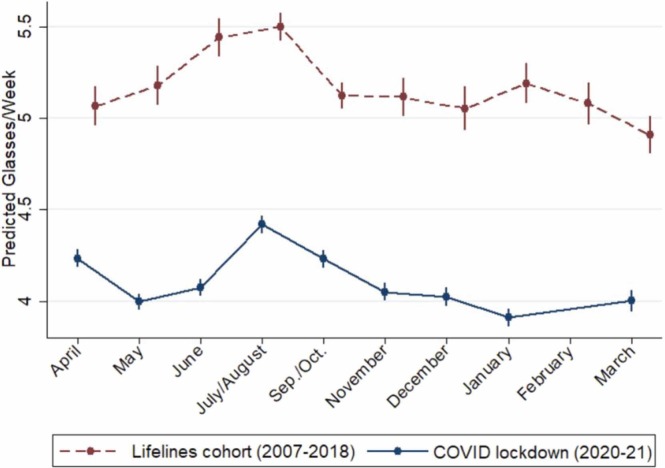
3.2. Alcohol seasonality
In order to disentangle potential effects of the lockdown from the typical seasonal pattern in alcohol consumption, results have been compared with previous waves of Lifelines data. It is worthwhile to mention that alcohol consumption in the Netherlands is pretty average in European terms -e.g. the rate of binge drinking is the same as the European average (Eurostat, 2019), which is slightly lower than in the US (NIAAA, 2019), and there are no significant differences in terms of seasonality either.
Thus, Fig. 3 compares alcohol consumption during the first year of the lockdown (blue line) with a cross-sectional analysis of pooled observations of waves 1, 4 and 5 of the Lifelines cohort study among the same individuals (red line) in the decade before the pandemic.
Fig. 3.
Seasonality in alcohol consumption. Comparison between the lockdown period (blue line) and previous observations from the Lifelines cohort (2007–2018) (dashed red line).
First, results clearly show that average alcohol consumption was lower during the lockdown period than in previous years (2007 – 2018). Second, although the seasonal pattern is roughly similar, there are some differences: while in previous years alcohol consumption steadily increased during spring and peaked in mid-summer, drinking levels decreased during spring 2020, which made the summer peak somewhat abrupter. After the summer period, the decline in alcohol consumption was steeper and steadier during the lockdown period. Last but not least, results from previous years show a small peak around Christmas -although rather small compared with the usual “January effect” reported in the literature (Lemmens and Knibbe, 1993; Uitenbroek, 1996; Carpenter, 2003)-, whereas in January 2021 not only no peak is observed but the lowest drinking levels of the whole observation period were reported.
In sum, results suggest that the lockdown had an effect in decreasing alcohol consumption. Moreover, it also modified alcohol seasonality, with decreased drinking levels during the initial “intelligent lockdown” and during the even more stringent lockdown in the winter of 2021, including the Christmas period.
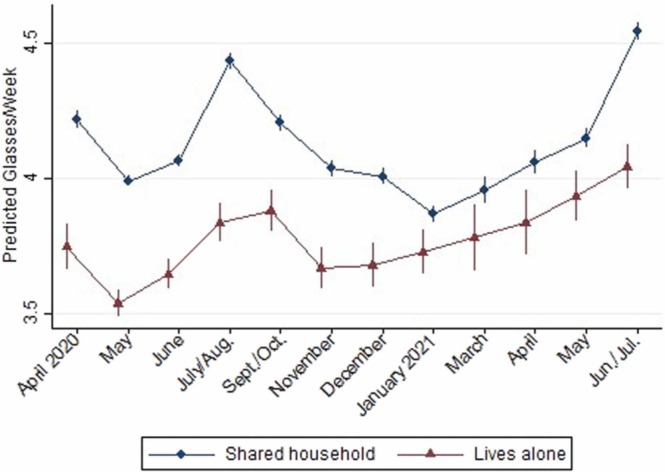
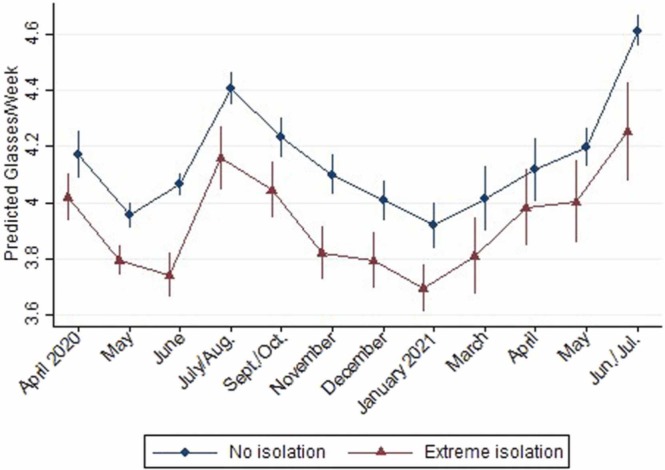
3.3. The moderating role of living arrangements and feelings of isolation
Our next aim was to test whether the effect of the pandemic on alcohol consumption differed by living arrangements and/or feelings of social isolation. For that purpose, interaction terms between these variables and time were added to the main effects model in a stepwise fashion.
First, as shown in Fig. 4, individuals who lived alone reported lower drinking levels throughout the whole observation period. Second, interaction coefficients are significant, as shown in Model 1 (Table 2)-, suggesting that the patterns differ between groups: the gap between those living alone and those with partner or family became smaller in relative terms during autumn and particularly winter, as those living alone showed a steady increase in alcohol consumption between November 2020 and May 2021 -i.e. during the strictest lockdown period when bars were closed and bans on alcohol sales were imposed-, whereas those living with others show a clear decrease until February 2021, and only increase afterwards.
Fig. 4.
Alcohol consumption during the lockdown, by living arrangement. Predictive margins based on fixed-effect models including the interaction term.
Furthermore, those living in a shared household report a higher increase in their consumption during the summer periods. Sensitivity analyses with a distinction among the latter between those who lived with other adults only and those who lived with children were performed. As shown in Figure A1 in the Appendix, the subgroup with children reports higher seasonal fluctuation, with very low consumption during autumn and winter but a steep increase in summer. That suggests that those living with others -and particularly those who lived with children- participated more in summer celebrations than those who lived alone.
Next, we tested the potential moderating role of social isolation by adding the interaction between “feelings of social isolation” and time to the model (Model 2 in Table 2). As the significant interaction coefficients show, differences between groups were smaller than by living arrangements, and mainly significant during the summer periods. As shown in Fig. 5, individuals who felt extremely socially isolated -i.e. isolation score ≥ 7- reported a lower increase in their alcohol consumption during both summer periods than those with no feelings of social isolation -score= 1-, whereas in the winter period they show similar trends.
Fig. 5.
Alcohol consumption during the lockdown by feelings of social isolation. Predictive margins based on fixed-effect models including the interaction term.
Moreover, the interaction coefficients for living arrangement and time remained intact after adding the interaction with social isolation, showing that their moderation effects follow independent patterns. Taken together, results show that the living arrangement, in which individuals lived during the lockdown, played a somewhat bigger role overall, particularly in the autumn - winter period. In turn, social isolation played a somewhat bigger role in summer, probably because the ones who felt most isolated did not participate so much in the summer celebrations, suggesting that fluctuations in alcohol consumption during the summer months seem more related with social drinking than with alcohol being a “coping mechanism”.
Last but not least, results suggest that the patterns differ more by living arrangement during the second year of the lockdown: the fluctuation in alcohol consumption is very similar until November 2020 (although drinking levels differ). Yet, from November onwards those living alone show a slow but steady increase in the pattern, whereas those living with partner/family have a much greater variation in the slope. Consistently, as shown in Table 1, the interaction term for those who lived alone in May 2020 was β = 0.02 (CI95% −0.08 to 0.12), whereas in the same month in 2021 it was β = 0.22 (CI95% 0.10–0.35).
4. Discussion
Our study, relying on a robust longitudinal design and a large sample, showed that overall alcohol consumption levels were far lower during the pandemic than in the years before. However, alcohol levels were not constant throughout the whole observation period but varied during the pandemic, in ways that partially differed from ‘normal’ seasonal patterns. Moreover, patterns differed by living arrangement and subjective feelings of social isolation, suggesting that different subgroups reacted to the pandemic and its related lockdown measures in different ways.
First, results show that alcohol consumption levels during the lockdown were lower than in previous years, which is probably due to the restrictions in social gatherings, and the closure of bars and restaurants, in line with what previous studies reported (Panagiotidis et al., 2020, Bade et al., 2021).
Second, the seasonal pattern of alcohol consumption during the pandemic differs from the one in previous years among the same population. Thus, our results show lower drinking levels during the strictest lockdown periods, compared to the equivalent periods before the pandemic. To the best of our knowledge, no other study has compared the seasonality of alcohol consumption during the pandemic with the periods prior to it. Moreover, our results contrast with one consistent finding in the literature, namely: the overall increase in alcohol consumption levels around the Christmas season. While this has been widely reported in different contexts (Lemmens and Knibbe, 1993, Uitenbroek, 1996) -sometimes called the “January effect” (Carpenter, 2003)-, our study shows that drinking levels during Christmas 2020 were at its lowest point, probably due to the strong restrictions in family gatherings that led many individuals to cancel or postpone their celebrations.
Third, we observe that changes in drinking patterns are not homogeneous across the whole population but differ by living arrangement and, to a lesser degree, by feelings of social isolation. Although it could be argued that both variables are highly related, it is interesting that their role as moderators is independent from each other, and the relative importance of one or the other changes throughout the observation period. Thus, the long covid winter of 2021 made a different impact among those living alone, who increased their drinking earlier than those sharing a household, in line with studies reporting increased solitary drinking during the lockdown (Wardell et al., 2020). On the other hand, those living with partner and/or family, particularly those with children, reported higher alcohol consumption in summer, probably in the context of outdoor activities and social gatherings during the summer holidays season.
Consistently, the subjective assessment of feeling socially isolated was associated with lower alcohol consumption in both summer periods, when most restrictions were lifted. Furthermore, social isolation shows a negative association with alcohol use, with those who feel most socially isolated drinking the least. This finding, at odds with the predictions that isolation during the lockdown would lead individuals to increase their alcohol consumption (Ramalho, 2020), suggests that, in the context of our study, drinking is mainly recreational and related with social events rather than a coping mechanism against loneliness, as previous evidence suggested (Gritsenko et al., 2020, Wardell et al., 2020). These contrasting results may be due to different factors, ranging from study design -previous studies often rely on small sample sizes and cross-sectional designs- and different characteristics of the sample, e.g. in terms of age (Gritsenko et al., 2020, Wardell et al., 2020). It is noteworthy that our sample is mainly composed by older adults, and those who report higher alcohol consumption in our study are mostly medium-educated males in their late fifties.
The question is, then, why would those who spent the strictest periods of the lockdown on their own report different drinking patterns, if it is not due to feelings of social isolation? Results suggest that other mechanisms may operate, e.g. higher family support may buffer the negative effects of the lockdown that could otherwise lead to higher alcohol consumption (Wardell et al., 2020, Valente et al., 2021). Alternatively, other mediators may be at play, e.g. boredom, which has been shown to be one of the main stressors during the pandemic (Yan et al., 2021), as well as a risk factor for alcohol abuse (Kuerbis et al., 2018). The fact that parents with children at home reported the lowest alcohol consumption during the strictest periods of the lockdown seems to point in that direction, as they certainly did not have time to be bored.
Last but not least, the finding that differences between these subgroups became larger in the second year of the pandemic suggests that some of the lockdown-related stress may have accumulated over time. Moreover, the potential buffering effect of, e.g. family support, may become less effective over time. Further longitudinal research is needed in order to disentangle these potential mechanisms.
This study has several limitations. First, information on alcohol consumption did not contain specific information on drinking patterns such as solitary drinking and, for that reason, the study design was based on “proxy variables”, such as living arrangement or feelings of isolation that, in a context of restricted social interactions, allowed us to approach this issue. However, interpretation of the results must be done being aware of this limitation. Second, although for those sharing a household, we had information about the household members and their ages, no information about their relationship status was available. However, given the age of our sample, and the very low prevalence of students, we assumed that most of them would be living with partner and/or family.
5. Conclusions
This longitudinal study shows that the Covid pandemic and subsequent lockdown had an impact in reducing overall alcohol consumption levels in the northern provinces of the Netherlands. However, this effect was not homogeneous but differed by living arrangement and subjective feelings of social isolation: those living alone and/or feeling more socially isolated reacted more strongly to the lockdown. Moreover, the impact of the lockdown was not constant over time but it was stronger, the longer it lasted, suggesting an accumulative effect and a reduction of resilience of some groups of individuals to cope with it.
CRediT authorship contribution statement
Lluís Mangot-Sala: Data cleaning and harmonization, Statistical analyses, Drafting of the manuscript. Khoa A. Tran: Literature review, Drafting of the manuscript. Aart C. Liefbroer, Nynke Smidt: Obtained funding and study supervision. Lluís Mangot-Sala, Aart C. Liefbroer, Nynke Smidt: Study concept and design, Acquisition and interpretation of data, Critical revision of the analyses and the manuscript.
Funding
This work was supported by the Research Fund of the Royal Netherlands Academy of Arts and Sciences (KNAW-Institutes).
Author disclosure
Lluís Mangot-Sala was responsible for the data cleaning and harmonization, performed the statistical analyses and wrote the manuscript. Khoa A. Tran carried out the literature review and wrote a first draft of the introduction. Aart C. Liefbroer and Nynke Smidt obtained funding for the study, supervised it and reviewed the final versions of the manuscript. The study concept and design, acquisition and interpretation of data, and the critical revision of the analyses and the manuscript were carried out by Lluís Mangot-Sala, Aart C. Liefbroer and Nynke Smidt. All authors have read and approved the manuscript for submission. None of the original material contained in the manuscript has been submitted for consideration nor will any of it be published elsewhere.
Conflicts of interest
None.
Footnotes
For an up-to-date version of COVID-cases and preventive measures, see: https://coronadashboard.rijksoverheid.nl/landelijk/positief-geteste-mensen
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.drugalcdep.2022.109349.
Appendix A. Supplementary material
Supplementary material.
.
Data Availability Statement
The data underlying this article were provided by Lifelines under licence. Access to the data can be granted under licence by Lifelines and the authors will share their codes used to produce the results presented in this paper upon request.
References
- Ahrens K.F., Neumann R.J., Kollmann B., Brokelmann J., von Werthern N.M., Malyshau A., Weichert D., Lutz B., Fiebach C.J., Wessa M., Kalisch R., Plichta M.M., Lieb K., Tuscher O., Reif A. Impact of COVID-19 lockdown on mental health in Germany: longitudinal observation of different mental health trajectories and protective factors. Transl. Psychiatry. 2021;11(1):392. doi: 10.1038/s41398-021-01508-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bade R., Simpson B.S., Ghetia M., Nguyen L., White J.M., Gerber C. Changes in alcohol consumption associated with social distancing and self-isolation policies triggered by COVID-19 in South Australia: a wastewater analysis study. Addiction. 2021;116(6):1600–1605. doi: 10.1111/add.15256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bierman A., Upenieks L., Glavin P., Schieman S. Accumulation of economic hardship and health during the COVID-19 pandemic: Social causation or selection? Soc. Sci. Med. 2021;275 doi: 10.1016/j.socscimed.2021.113774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter C. Seasonal variation in self-reports of recent alcohol consumption: racial and ethnic differences. J. Stud. Alcohol. 2003;64(3):415–418. doi: 10.15288/jsa.2003.64.415. [DOI] [PubMed] [Google Scholar]
- Chandola T., Kumari M., Booker C.L., Benzeval M. The mental health impact of COVID-19 and lockdown-related stressors among adults in the UK. Psychol. Med. 2020;7:1–10. doi: 10.1017/S0033291720005048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins S.E. Associations between socioeconomic factors and alcohol outcomes. Alcohol Res. 2016;38(1):83–94. [PMC free article] [PubMed] [Google Scholar]
- Cooper M.L., Kuntsche E., Levitt A., Barber L.L., Wolf S. In: The Oxford handbook of substance use and substance use disorders. Sher K.J., editor. Oxford University Press; 2016. Motivational models of substance use: A review of theory and research on motives for using alcohol, marijuana, and tobacco; pp. 375–421. [Google Scholar]
- Corbin W.R., Farmer N.M., Nolen-Hoekesma S. Relations among stress, coping strategies, coping motives, alcohol consumption and related problems: a mediated moderation model. Addict. Behav. 2013;38(4):1912–1919. doi: 10.1016/j.addbeh.2012.12.005. [DOI] [PubMed] [Google Scholar]
- Corbin W.R., Waddell J.T., Ladensack A., Scott C. I drink alone: mechanisms of risk for alcohol problems in solitary drinkers. Addict. Behav. 2020;102 doi: 10.1016/j.addbeh.2019.106147. [DOI] [PubMed] [Google Scholar]
- Czeisler M.E., Lane R.I., Wiley J.F., Czeisler C.A., Howard M.E., Rajaratnam S.M.W. Follow-up Survey of US Adult Reports of Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic, September 2020. JAMA Netw. Open. 2021;4(2) doi: 10.1001/jamanetworkopen.2020.37665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson D.A., Grant B.F., Ruan W.J. The association between stress and drinking: modifying effects of gender and vulnerability. Alcohol Alcohol. 2005;40(5):453–460. doi: 10.1093/alcalc/agh176. [DOI] [PubMed] [Google Scholar]
- de Goeij M.C., Suhrcke M., Toffolutti V., van de Mheen D., Schoenmakers T.M., Kunst A.E. How economic crises affect alcohol consumption and alcohol-related health problems: a realist systematic review. Soc. Sci. Med. 2015;131:131–146. doi: 10.1016/j.socscimed.2015.02.025. [DOI] [PubMed] [Google Scholar]
- Gezondheidsraad – Health Council of the Netherlands . The Hague: Health Council of The Netherlands. .,; 2015. Dutch dietary guidelines 2015 (Richtlijnen goede voeding 2015) Publication no. 2015/24E. ISBN: 978-94-6281-104-1. [PubMed] [Google Scholar]
- Grace M.K. COVID-19 bereavement, depressive symptoms, and binge drinking. SSM - Ment. Health. 2021;1 doi: 10.1016/j.ssmmh.2021.100041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grigoletto V., Cognigni M., Occhipinti A.A., Abbracciavento G., Carrozzi M., Barbi E., Cozzi G. Rebound of Severe Alcoholic Intoxications in Adolescents and Young Adults After COVID-19 Lockdown. J. Adolesc. Health. 2020;67(5):727–729. doi: 10.1016/j.jadohealth.2020.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gritsenko V., Skugarevsky O., Konstantinov V., Khamenka N., Marinova T., Reznik A., Isralowitz R. COVID 19 fear, stress, anxiety, and substance use among Russian and Belarusian university students. Int J. Ment. Health Addict. 2020:1–7. doi: 10.1007/s11469-020-00330-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoveling L.A., Liefbroer A.C., Bültmann U., Smidt N. Understanding socioeconomic differences in incident metabolic syndrome among adults; What is the mediating role of health behaviours? Prev. Med. 2021;148 doi: 10.1016/j.ypmed.2021.106537. [DOI] [PubMed] [Google Scholar]
- Klijs B., Scholtens S., Mandemakers J.J., Snieder H., Stolk R.P., Smidt N. Representativeness of the lifelines cohort study. PLoS ONE. 2015;10(9) doi: 10.1371/journal.pone.0137203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knell G., Robertson M.C., Dooley E.E., Burford K., Mendez K.S. Health Behavior Changes During COVID-19 Pandemic and Subsequent “Stay-at-Home” Orders. Int J. Environ. Res Public Health. 2020;17(17):6268. doi: 10.3390/ijerph17176268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuerbis A., Treloar Padovano H., Shao S., Houser J., Muench F.J., Morgenstern J. Comparing daily drivers of problem drinking among older and younger adults: An electronic daily diary study using smartphones. Drug Alcohol Depend. 2018;183:240–246. doi: 10.1016/j.drugalcdep.2017.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemmens P., Knibbe R. Seasonal variation in survey and sales estimates of alcohol consumption. J. Stud. Alcohol. 1993;54(2):157–163. doi: 10.15288/jsa.1993.54.157. [DOI] [PubMed] [Google Scholar]
- Mackenbach J.P., Kulhanova I., Bopp M., Borrell C., Deboosere P., Kovacs K., Looman C.W., Leinsalu M., Makela P., Martikainen P., Menvielle G., Rodriguez-Sanz M., Rychtarikova J., de Gelder R. Inequalities in Alcohol-Related Mortality in 17 European Countries: A Retrospective Analysis of Mortality Registers. PLoS Med. 2015;12(12) doi: 10.1371/journal.pmed.1001909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mc Intyre K., Lanting P., Deelen P., Wiersma H.H., Vonk J.M., Ori A.P.S., Jankipersadsing S.A., Warmerdam R., van Blokland I., Boulogne F., Dijkema M.X.L., Herkert J.C., Claringbould A., Bakker O., Lopera Maya E.A., Bultmann U., Zhernakova A., Reijneveld S.A., Zijlstra E., Swertz M.A., Brouwer S., van Ooijen R., Angelini V., Dekker L.H., Sijtsma A., Scherjon S.A., Wijmenga C., Dekens J.A.M., Mierau J., Boezen H.M., Franke L. Lifelines COVID-19 cohort: investigating COVID-19 infection and its health and societal impacts in a Dutch population-based cohort. BMJ Open. 2021;11(3) doi: 10.1136/bmjopen-2020-044474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newby J.M., O'Moore K., Tang S., Christensen H., Faasse K. Acute mental health responses during the COVID-19 pandemic in Australia. PLoS One. 2020;15(7) doi: 10.1371/journal.pone.0236562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niedzwiedz C.L., Green M.J., Benzeval M., Campbell D., Craig P., Demou E., Leyland A., Pearce A., Thomson R., Whitley E., Katikireddi S.V. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of the UK Household Longitudinal Study. J. Epidemiol. Community Health. 2021;75(3):224–231. doi: 10.1136/jech-2020-215060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutt D., King L., Phillips L. Drug harms in the UK: a multi-criteria decision analysis. Lancet. 2010;376(9752):1558–1565. doi: 10.1016/S0140-6736(10)61462-6. [DOI] [PubMed] [Google Scholar]
- Oksanen A., Savolainen I., Savela N., Oksa R. Psychological Stressors Predicting Increased Drinking During the COVID-19 Crisis: A Longitudinal National Survey Study of Workers in Finland. Alcohol Alcohol. 2021;56(3):299–306. doi: 10.1093/alcalc/agaa124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panagiotidis P., Rantis K., Holeva V., Parlapani E., Diakogiannis I. Changes in alcohol use habits in the general population, during the COVID-19 lockdown in Greece. Alcohol Alcohol. 2020;55(6):702–704. doi: 10.1093/alcalc/agaa092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prati G., Mancini A.D. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 2021;51(2):201–211. doi: 10.1017/S0033291721000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramalho R. Alcohol consumption and alcohol-related problems during the COVID-19 pandemic: a narrative review. Austral Psychiatry. 2020;28(5):524–526. doi: 10.1177/1039856220943024. [DOI] [PubMed] [Google Scholar]
- Rehm J., Baliunas D., Borges G.L., Graham K., Irving H., Kehoe T., Parry C.D., Patra J., Popova S., Poznyak V., Roerecke M., Room R., Samokhvalov A.V., Taylor B. The relation between different dimensions of alcohol consumption and burden of disease: an overview. Addiction. 2010;105(5):817–843. doi: 10.1111/j.1360-0443.2010.02899.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J., Kilian C., Ferreira-Borges C., Jernigan D., Monteiro M., Parry C.D.H., Sanchez Z.M., Manthey J. Alcohol use in times of the COVID 19: Implications for monitoring and policy. Drug Alcohol Rev. 2020;39(4):301–304. doi: 10.1111/dar.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts A., Rogers J., Mason R., Siriwardena A.N., Hogue T., Whitley G.A., Law G.R. Alcohol and other substance use during the COVID-19 pandemic: A systematic review. Drug Alcohol Depend. 2021;229(Pt A) doi: 10.1016/j.drugalcdep.2021.109150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers A.H., Shepherd J.M., Garey L., Zvolensky M.J. Psychological factors associated with substance use initiation during the COVID-19 pandemic. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallie S.N., Ritou V., Bowden-Jones H., Voon V. Assessing international alcohol consumption patterns during isolation from the COVID-19 pandemic using an online survey: highlighting negative emotionality mechanisms. BMJ Open. 2020;10(11) doi: 10.1136/bmjopen-2020-044276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholtens S., Smidt N., Swertz M.A., Bakker S.J., Dotinga A., Vonk J.M., van Dijk F., van Zon S.K., Wijmenga C., Wolffenbuttel B.H., Stolk R.P. Cohort Profile: Lifelines, a Three-Generation Cohort Study and Biobank. Int J. Epidemiol. 2015;44(4):1172–1180. doi: 10.1093/ije/dyu229. [DOI] [PubMed] [Google Scholar]
- Skrzynski C.J., Creswell K.G. Associations between solitary drinking and increased alcohol consumption, alcohol problems, and drinking to cope motives in adolescents and young adults: a systematic review and meta-analysis. Addiction. 2020;115(11):1989–2007. doi: 10.1111/add.15055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson K., Dutton D.J., MacNabb K., Liu T., Blades S., Asbridge M. Changes in alcohol consumption during the COVID-19 pandemic: exploring gender differences and the role of emotional distress. Health Promot Chronic Dis. Prev. Can. 2021;41(9):254–263. doi: 10.24095/hpcdp.41.9.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uitenbroek D. Seasonal variation in Alcohol use. J. Stud. Alcohol. 1996;1:47–52. doi: 10.15288/jsa.1996.57.47. [DOI] [PubMed] [Google Scholar]
- Valente J.Y., Sohi I., Garcia-Cerde R., Monteiro M.G., Sanchez Z.M. What is associated with the increased frequency of heavy episodic drinking during the COVID-19 pandemic? Data from the PAHO regional web-based survey. Drug Alcohol Depend. 2021;221 doi: 10.1016/j.drugalcdep.2021.108621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Amsterdam J., Opperhuizen A., Koeter M., van den Brink W. Ranking the harm of alcohol, tobacco and illicit drugs for the individual and the population. Eur. Addict. Res. 2010;16(4):202–207. doi: 10.1159/000317249. [DOI] [PubMed] [Google Scholar]
- Vanderbruggen N., Matthys F., Van Laere S., Zeeuws D., Santermans L., Van den Ameele S., Crunelle C.L. Self-reported alcohol, tobacco, and cannabis use during COVID-19 lockdown measures: results from a web-based survey. Eur. Addict. Res. 2020;26(6):309–315. doi: 10.1159/000510822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villanueva-Blasco V.J., Villanueva Silvestre V., Vazquez-Martinez A., Rial Boubeta A., Isorna M. Age and living situation as key factors in understanding changes in alcohol use during COVID-19 confinement. Int J. Environ. Res Public Health. 2021;18(21):11471. doi: 10.3390/ijerph182111471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Shi L., Que J., Lu Q., Liu L., Lu Z., Xu Y., Liu J., Sun Y., Meng S., Yuan K., Ran M., Lu L., Bao Y., Shi J. The impact of quarantine on mental health status among general population in China during the COVID-19 pandemic. Mol. Psychiatry. 2021;26(9):4813–4822. doi: 10.1038/s41380-021-01019-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardell J.D., Kempe T., Rapinda K.K., Single A., Bilevicius E., Frohlich J.R., Hendershot C.S., Keough M.T. Drinking to Cope During COVID-19 Pandemic: The Role of External and Internal Factors in Coping Motive Pathways to Alcohol Use, Solitary Drinking, and Alcohol Problems. Alcohol Clin. Exp. Res. 2020;44(10):2073–2083. doi: 10.1111/acer.14425. [DOI] [PubMed] [Google Scholar]
- White H.R., Stevens A.K., Hayes K., Jackson K.M. Changes in Alcohol Consumption Among College Students Due to COVID-19: Effects of Campus Closure and Residential Change. J. Stud. Alcohol Drugs. 2020;81:725–730. doi: 10.15288/jsad.2020.81.725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan L., Gan Y., Ding X., Wu J., Duan H. The relationship between perceived stress and emotional distress during the COVID-19 outbreak: Effects of boredom proneness and coping style. J. Anxiety Disord. 2021;77 doi: 10.1016/j.janxdis.2020.102328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yazdi K., Fuchs-Leitner I., Rosenleitner J., Gerstgrasser N.W. Impact of the COVID-19 Pandemic on Patients With Alcohol Use Disorder and Associated Risk Factors for Relapse. Front Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.620612. [DOI] [PMC free article] [PubMed] [Google Scholar]
Web References
- Eurostat - European Statistics, 2019 (accessed on 24/01/2022): 〈https://ec.europa.eu/eurostat/web/products-eurostat-news/-/edn-20210806–1〉.
- NIAAA – National Institute on Alcohol Abuse and Alcoholism. 2019, National survey on Drug Use and Health (NSDUH) (accessed on 24/01/2022): 〈https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/alcohol-facts-and-statistics〉.
- Rijksoverheid – Dutch Government. Coronavirus Dashboard (accessed on 24/01/2022): 〈https://coronadashboard.rijksoverheid.nl/landelijk/positief-geteste-mensen〉.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material.
Data Availability Statement
The data underlying this article were provided by Lifelines under licence. Access to the data can be granted under licence by Lifelines and the authors will share their codes used to produce the results presented in this paper upon request.