Figure 1.
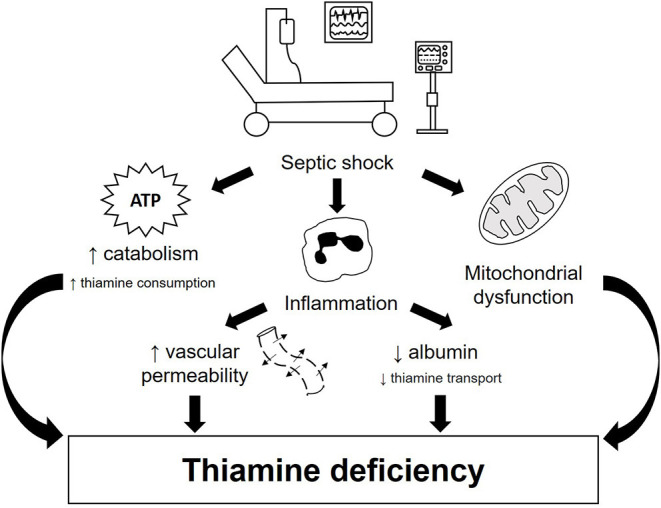
Pathophysiology of thiamine deficiency in septic shock patients. Thiamine deficiency in septic shock occurs both due to increased need and impaired transport. This condition can be triggered by three main mechanisms: hypercatabolism, exacerbated pro-inflammatory response and mitochondrial dysfunction. During septic shock, there is an increase in the metabolic demand for energy, resulting in increased glycogenolysis, inhibition of glycogenesis and increased production of glucose via gluconeogenesis, considerably increasing the need for thiamine for glucose metabolism. Inflammation, on the other hand, promotes increased vascular permeability and reduced albumin production, impairing thiamine transport. In addition, tissue hypoxia present in septic shock is one of the main triggers of mitochondrial dysfunction, which contributes to an imbalance in glucose homeostasis, including lower availability of ATP and increased serum lactate concentration. All these mechanisms together contribute to the development and/or worsening of thiamine deficiency in patients with septic shock.
