Abstract
Background
Clinical effectiveness of video consultations in the mental health services is comparable with in-person consultations. Acceptance has typically been rated in surveys that do not give a deeper understanding behind the phenomenon. The aim of this synthesis is to explore mental health patients’ perceptions of factors that influence their acceptance of video consultations viewed from the perspective of the patient.
Methods
A literature search in scientific databases was conducted. Peer-reviewed reports of qualitative research exploring patients’ experiences with video consultations from the patients’ perspectives were included. Then a meta-summary and a taxonomic analysis were conducted.
Results
A total of 11 reports met the inclusion criteria. Through the analysis, a model was generated with five factors that precede each other and interact with each other. Patients thought video consultations were acceptable when (1) they experienced barriers and inconvenience to accessing the location of services, (2) they had already established a trustful relationship with their therapist, (3) technical interferences were minor and problems were resolved quickly, (4) patients expected a less personal meeting, and (5) the degree of the patients’ issues were less complex.
Discussion
This model is intended to help clinicians identify circumstances where offering video consultations make best sense to patients and help sustain meaningful use prospectively. When patients encounter barriers to in-person services, clinicians should consider offering video consultations when the technology is adequately integrated in practice, and it is perceived not to intervene with treatment or the therapeutic process.
Keywords: Video consultation, mental health patient, telepsychiatry, synthesis of qualitative research
Introduction
Consultations via videoconference can increase access to health care services by overcoming barriers such as social distancing needs currently caused by the COVID-19 pandemic, long distance to services, transportation costs, long waiting times, and more.1–5 In the mental health services, many consultations are based on conversations with patients and appear, therefore, to be easily transferable to videoconferencing consultations. Treatment via videoconference might further alleviate mental health patients’ concerns of stigmatization for treatment-seeking since it is possible to get treatment without leaving home.6,7
Several studies have shown that the clinical effect of using videoconferencing in the delivery of psychotherapy for multiple disorders is equally effective as in-person, and high levels of satisfaction and acceptance have been displayed.8–14 Psychiatric assessments via videoconferencing have also been found to be equivalent to in-person assessments.4,9,15 Practitioners have been concerned about establishing rapport with patients in psychotherapy over videoconferencing;9,16–18 however, the therapeutic alliance has repeatedly been rated high by therapists and patients.8,12,13,19
During the COVID-19 pandemic, many practitioners have been compelled to convert in-person sessions to virtual ones. It has been suggested to continue these new services post COVID-19 to increase access to mental health services and to prepare health care systems for future similar unforeseen disruptive events. 20 As health care services return to having the possibility of same room encounters, it is important to explore how to blend in-person sessions with videoconferencing sessions. Studies have already found that patients find videoconferencing sessions acceptable,1,5 but these studies are often limited to survey questions about easier access and usability of the technologies involved in regard to particular settings. To inform clinical decision-making, it is relevant to understand what factors influence patients’ acceptability of these services in general. In that regard, qualitative research has the advantage of being open to explore anticipated as well as unanticipated issues and get a deeper understanding of the phenomenon. Extending upon previous reviews, which have considered clinical effectiveness, therapeutic alliance, satisfaction, and survey measured acceptance, we sought to explore patients’ perceptions of factors influencing their acceptability of video consultations viewed from the perspectives of the patients. To focus the investigation further, only individual psychotherapy or psychiatric assessments were included.
Methods
Search methods
A systematic search was conducted in the following databases: Academic Search Premiere, CINAHL, Embase, PsycINFO, PubMed, Scopus, Sociological Abstracts, and Web of Science. The search was divided into two focus areas: words related to the videoconferencing modality and words related to the treatment of mental health patients. The search additionally included keywords specific to each database. The full search matrix is presented in Table 1. Words categorized under the same focus area were combined with “OR,” and then the two focus areas were searched with “AND.” The search was restricted to words that could be found in abstracts. Words with different endings were searched with truncations, and words that belong together were searched with quotation marks.
Table 1.
Search matrix.
| No. | Heading or subject term or keyword | Free text in abstract and title |
|---|---|---|
| Focus 1 | ||
| 1 | Teleconsultation (Embase) (Scopus) | |
| 2 | Teleconferencing (ASP) (CINAHL) (PsycINFO) Teleconference (Embase) |
Teleconf* |
| 3 | Telemedicine (ASP) (CINAHL) (Embase) (PsycINFO) (PubMed) | Telemedicine |
| 4 | Telemental | |
| 5 | Telepsychiatry (ASP) (CINAHL) (embase) (PsycINFO) | Telepsych* |
| 6 | Telepsychology (ASP) | |
| 7 | Teletherapy (Embase) | Teletherapy |
| 8 | Videoconferencing (ASP) (CINAHL) (Embase) (PsycINFO) (PubMed) | Videoconf* OR “video conf*” |
| 9 | “Video counseling” OR “video counselling” “Video counsel*” |
|
| 10 | Webcams (ASP) | “Web camera” OR webcam* |
| Focus 2 | ||
| 1 | Behavior therapy (ASP) (CINAHL) (Embase) (PsycINFO) (PubMed) Cognitive behavior therapy (PsycInfo) Cognitive behavioral therapy (PubMed) |
“Behavior therapy” OR “behaviour therapy” “Behavi* therapy” |
| 2 | Cognitive therapy (ASP) (CINAHL) (Embase) (PsycINFO) (Scopus) | “Cognitive therapy” |
| 3 | Psychoanalysis (ASP) (CINAHL) (Embase) (PsycINFO) (PubMed) (Scopus) (Soc Ab) | Psychoanaly* |
| 4 | Psychoeducation (ASP) (CINAHL) (Embase) (PsycINFO) | Psychoeducation |
| 5 | Psychotherapy (ASP) (CINAHL) (PsycINFO) (PubMed) (Scopus) (Soc Ab) | Psychotherap* |
| 6 | Counseling psychologists (ASP) Counseling psychology (ASP) (PsycINFO) |
“Counseling psycholog*” OR “counselling psycholog*” “Counsel* psycholog*” |
| 7 | Mental health counseling (ASP) Mental health counselors (ASP) |
”Mental health counseling” OR “mental health counselling” “Mental health counsel*” |
| 8 | Mental health consultation (ASP) | “Mental health consultation” |
| 9 | Psychological consultation (ASP) | “Psychological consultation” |
| 10 | Psychiatric consultation (ASP) Psychiatric day treatment (ASP) Psychiatric treatment (ASP) (Embase) Mental illness treatment (ASP) Mental health care (Embase) Psychiatric home care (CINAHL) |
Psychiatric |
| 11 | Psychiatry (ASP) (CINAHL) (Embase) (PsycINFO) (PubMed) (Soc Ab) Community psychiatry (PsycINFO) (PubMed) Social psychiatry (Embase) (PsycINFO) Mental Health Services (Soc Ab) |
Psychiatry |
Restrictions for all searches were that the articles had to be peer-reviewed and original research (not discussions, reviews, and letters); in one of the following languages: English, German, or Scandinavian; and published between 1 January 2000 and 1 November 2021. Literature from before this date can be found in Miller's review 21 about the doctor-patient communication in telemedicine.
Inclusion and exclusion criteria
Reports of studies where mental health patients had been using video consultations for individual psychotherapy with a therapist or for psychiatric assessments by a psychiatrist were included. In the remaining, video consultations refer to both psychotherapy and psychiatric assessment via videoconference. Interventions were not limited in scope, e.g. length of treatment, combinations of videoconferencing and in-person sessions, and psychotherapy type, but participants had to have tried at least one video consultation and be an adult outpatient (aged ≥18).
To get a more detailed description of the perspectives of video consultations, only qualitative research was included. Qualitative research was defined by Sandelowski and Barroso's typology of qualitative findings 22 where thematic surveys, thematic/conceptual descriptions, and interpretive explanations were included, and topical surveys and reports without an explicit analysis of the data were excluded.
Selection of studies
The first two authors conducted the search. After duplicates were excluded, these authors went through the titles and abstracts and independently assessed the eligibility of the studies. In this initial screening, all articles that included psychotherapy or psychiatric assessment using videoconferencing with adults went on to full-text screening. Eligibility was assessed in the full texts by two authors. Any disagreements were resolved by discussion.
Critical appraisal of the included reports
Two authors critically appraised the included reports based on the Critical Appraisal Skills Programme's qualitative checklist, 23 with any disagreements resolved by discussion. Articles were categorized as having high, medium, or low quality. Only the high-quality reports were included in the main analysis to avoid drawing unreliable conclusions. Low- and medium-quality reports were included after the main analysis was conducted to support or dispute the already existing themes. The appraisal refers to the qualitative parts of the studies. In Table 2, quality ratings are presented.
Table 2.
Quality assessment of the included reports guided by the CASP qualitative checklist.
| Checklist itema | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Quality rating | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Report | ||||||||||||
| 1 | Ashwick et al. 2019 | Y | Y | Y | Y | Y | - | Y | Y | Y | H | High |
| 2 | Christensen et al. 2020 | Y | Y | Y | Y | Y | - | Y | Y | Y | H | High |
| 3 | Frank et al. 2017 | Y | Y | Y | Y | Y | - | ? | Y | Y | H | High |
| 4 | Frayn et al. 2021 | Y | Y | ? | Y | ? | - | Y | Y | Y | H | High |
| 5 | Hensel et al. 2020 | Y | Y | Y | Y | Y | - | Y | Y | Y | H | High |
| 6 | Leukhardt et al. 2021 | Y | Y | Y | Y | Y | Y | Y | Y | Y | H | High |
| 7 | May et al. 2000 | Y | Y | Y | Y | Y | - | - | Y | Y | H | High |
| 8 | Simpson et al. 2015 | Y | Y | Y | Y | Y | - | Y | Y | Y | H | High |
| 9 | Tarp and Nielsen, 2017 | Y | Y | Y | Y | Y | - | Y | Y | Y | H | High |
| 10 | Trondsen et al. 2018 | Y | Y | Y | Y | Y | - | Y | Y | Y | H | High |
| 11 | Ye et al. 2012 | Y | Y | Y | Y | ? | - | Y | - | - | L | Low |
Note: aCASP criteria for qualitative reports: 1. Was there a clear statement of the aims of the research? 2. Is a qualitative methodology appropriate? 3. Was the research design appropriate to address the aims of the research? 4. Was the recruitment strategy appropriate to the aims of the research? 5. Was the data collected in a way that addressed the research issue? 6. Has the relationship between researcher and participants been adequately considered? 7. Have ethical issues been taken into consideration? 8. Was the data analysis sufficiently rigorous? 9. Is there a clear statement of findings? (Yes: Y, No: -, Unclear: ?) 10. How valuable is the research? (H: Highly, L: Little). The assessment is only based on the qualitative part of a report.
Data analysis
All text labeled as “results” or “findings” was extracted as data for the analysis. In studies with both quantitative and qualitative findings, only the qualitative findings were extracted. Following Sandelowski and Barrosós meta-summary method for synthesizing qualitative research, 24 findings were extracted and separated into meaning units while editing the text to make it accessible to any reader. The meaning units were grouped into descriptive categories and then assembled into themes. Synthesis of the findings was then guided by Sandelowski and Barrosós description of taxonomic analysis 24 where the purpose is to identify underlying conceptual relations signified in the findings.
The first author conducted all the steps of the analysis, and the third and fourth authors functioned as auditors at each step.
Results
Included articles
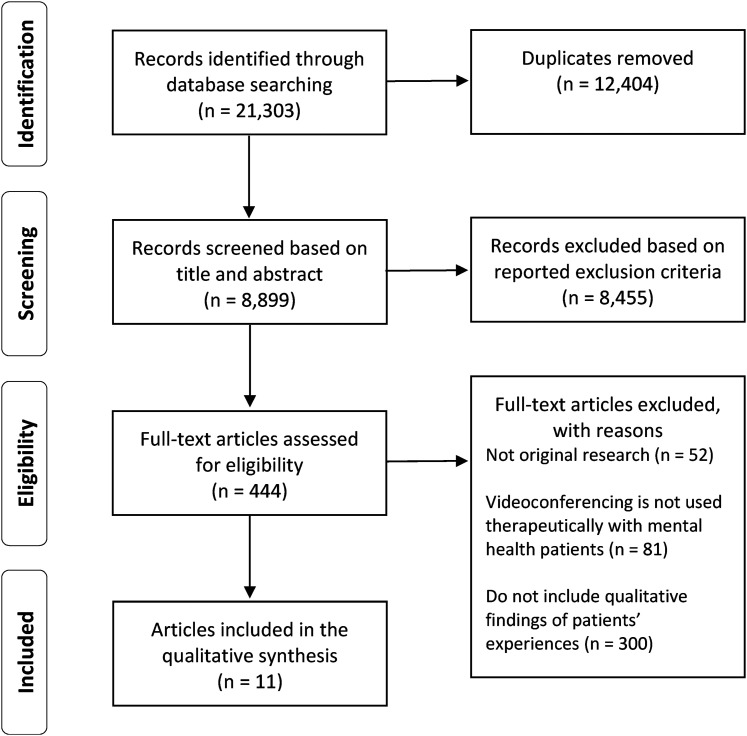
The initial search identified 8899 articles when duplicates were removed. After screening title and abstract, 444 articles remained which were reviewed for eligibility. Of these, most did not report qualitative findings of patients’ experiences. Finally, 11 articles met the inclusion criteria (Figure 1).
Figure 1.
Selection flow chart.
Study descriptions
Of the 11 included articles, 10 were rated with high-quality and 1 with low. The high-quality articles used qualitative interviews and the other used a questionnaire survey with open questions. The analyses used were thematic analysis (n = 5), qualitative content analysis (n = 3), discourse analysis (n = 1), grounded theory-based analysis (n = 1), and a stepwise-deductive-inductive approach (n = 1).
Study samples were drawn mostly from rural populations within the UK (n = 2), Denmark (n = 2), Germany (n = 2), Norway (n = 1), USA (n = 2), Canada (n = 1), and Australia (n = 1), with sample sizes of 1–27 patients. In all, there are data from 138 patients.
Patients were diagnosed with anxiety disorders, affective disorders, eating disorders, personality disorders, and alcohol dependency. Different treatments were used, most commonly a type of cognitive behavioral therapy. In five studies, the patients met their therapist in person initially, in five they did not, and in one study, it was optional. In seven studies, the patients received video consultations from their home, and in four of the studies, the patients received it from a rural clinic. An overview of study characteristics can be found in Table 3.
Table 3.
Study characteristics.
| Authors, publication year, and country | Aim of study, study design, method, analysis, typology, 22 language, and author discipline | Population (n), gender, age, diagnosis, type of provider, and sampling plan | Treatment type, sessions, met provider in-person first, and videoconference program | Findings |
|---|---|---|---|---|
| Ashwick et al. 2019 UK, England 25 |
Aim of study: To explore the acceptability of teletherapy in a sample of UK veterans with PTSD Design: Intervention study Method: Qualitative interviews Analysis: Thematic analysis Typology: Thematic survey Language: English Author discipline: Psychology |
N: 16 Gender: 15 men and 1 woman Age: Mean 41 years (27–58 years) Diagnosis: Combat-related post-traumatic stress disorder Provider: Psychologist Sampling plan: Purposive |
Treatment type: Cognitive behavioral therapy Sessions: 12 sessions received from home Met provider first: yes Videoconference program: Skype for business |
|
| Christensen et al. 2020 Denmark 26 |
Aim of study: To investigate older patients’ and their providers’ experiences with video consultations Design: Qualitative study Method: Semi-structured interviews Analysis: Thematic analysis Typology: Interpretive explanation Language: English Author discipline: Nursing |
N: 13 Gender: 5 men and 8 women Age: Mean 76 years Diagnosis: Depression Provider: Mental health nurses, psychiatrists, and psychologists Sampling plan: Purposive |
Treatment type: Treatment as usual Sessions: Varied. Patients had on average six sessions they received from home Met provider first: yes Videoconference program: Cisco Jabber |
|
| Frank et al. 2017 Germany 27 |
Aim of study: To report the first experiences with therapy over videoconference from a case Design: Case report Method: A structured interview based on open questions Analysis: Qualitative content analysis Typology: Thematic survey Language: German Author discipline: Social work |
N: 1 Gender: Man Age: 67 years Diagnosis: Chronic depression Provider: not stated Sampling plan: Purposive |
Treatment type: Cognitive behavioral analysis system Sessions: After 11 weeks of hospitalization, the treatment was continued through six sessions of video consultations received from home with the same therapist Met provider first: yes Videoconference program: not stated |
|
| Frayn et al. 2021 USA 28 |
Aim of study: To qualitatively examine patient perceptions of teletherapy Design: Mid-program assessment of a randomized controlled study Method: Individual semi-structured interviews Analysis: Thematic analysis Typology: Thematic survey Language: English Author discipline: Psychology |
N: 11 Gender: 3 men and 7 women and 1 transgender man Age: Mean 42.8 years Diagnoses: Binge eating disorder, bulimia nervosa, or other specified feeding and eating disorder Provider: not stated Sampling plan: Purposive |
Treatment type: Cognitive behavioral therapy combined with various components of mindfulness and acceptance-based treatment Sessions: 16 sessions received from home Met provider first: no Videoconference program: not stated |
|
| Hensel et al. 2020 Canada 29 |
Aim of study: To explore the factors that influence engagement with videoconferencing for psychotherapy for postpartum depressive and anxiety symptoms Design: Intervention study Method: Semi-structured telephone interviews after a 3 months’ intervention period Analysis: Thematic analysis Typology: Thematic description Language: English Author discipline: Psychiatry |
N: 12 (of whom 2 did not use video) Gender: All women Age: Mean 34.5 years Diagnosis: Postpartum depression or anxiety Provider: Master's trained social workers Sampling plan: Purposive |
Treatment type: Psychotherapy based on cognitive behavioral and interpersonal therapy approaches Sessions: Weekly sessions if needed for 3 months. At each session video contact from home was optional. On average 50% of sessions were via video Met provider first: optional Videoconference program: Vidyo (Ontario Telemedicine Network) |
|
| Leukhardt et al. 2021 Germany 30 |
Aim of study: To examine how the switch from traditional treatment to video-based treatment during the COVID-19 pandemic was experienced by patients and therapists with respect to the therapeutic relationship and the therapeutic process Design: Grounded Theory study Method: Semi-structured telephone interviews Analysis: Based on Grounded Theory methodology procedures included open, axial, and selective coding with the aim of formulating a theoretical model Typology: Thematic survey Language: German Author discipline: Psychology |
N: 9 Gender: 4 men and 5 women Age: Mean 42.5 years Diagnoses: Mood or affective disorders, anxiety disorders, or personality disorders Provider: Licensed psychotherapists or psychotherapists in training Sampling plan: Theoretical sampling |
Treatment type: Psychoanalytic or depth psychology Sessions: Weekly or biweekly sessions received from home Met provider first: yes Videoconference program: not stated |
|
| May et al. 2000 UK, England 31 |
Aim of study: To establish the acceptability of psychiatric referral by simple videophone Design: Qualitative evaluation Method: Semi-structured informal interviews Analysis: Conventional model of discourse analysis Typology: Conceptual description Language: English Author discipline: Sociology |
N: 22 Gender: not stated Age: not stated Diagnoses: Depression and/or anxiety disorders Providers: Psychiatrists supported by nurses in person Sampling plan: Purposive |
Treatment type: Diagnosis and management advice Sessions: Referrals from general practice where the patient was located during their psychiatric video consultation Met provider first: no Videoconference program: Simple videophone units—telephones with an additional LCD screen and fixed video camera joined by a high bandwidth (ISDN2) telephone line |
|
| Simpson et al. 2015 Australia, South Australia 32 |
Aim of study: To explore perceptions of and reaction to video therapy as described by participants Design: Mixed-methods design Method: Semi-structured interviews conducted over videoconference Analysis: Content analysis Typology: Thematic survey Language: English Author discipline: Psychology |
N: 6 Gender: 3 men and 3 women Age: Mean 34 years (20–58 years) Diagnoses: Most had comorbid disorders; all had depression, 3 had social anxiety or social phobia Providers: Provisional master's level trainee psychologists Sampling plan: Purposive |
Treatment type: Cognitive behavioral therapy and schema therapy Sessions: Participants had between 5 and 20 video sessions from within the mental health services Met provider first: no Videoconference program: Client site had Cisco C20 endpoint with a 50” plasma display; therapist site had Lifesize Express 220 unit with 40” LCD display |
|
| Tarp & Nielsen, 2017 Denmark 33 |
Aim of study: To describe patient perspectives on optional videoconferencing-based treatment for alcohol dependency Design: Qualitative descriptive study Method: Semi-structured interviews Analysis: Qualitative content analysis Typology: Thematic description Language: English Author discipline: Anthropology |
N: 27 (of whom 11 did not use video) Gender: Mostly men Age: Mean 47 years Diagnosis: Alcohol dependency or alcohol problems Providers: not stated Sampling plan: Subsample from a larger study |
Treatment type: Treatment as usual Sessions: Varied. At each session video contact was optional. There was a total of 60 video sessions among the 16 patients who used it. The patients received the video sessions in their homes Met provider first: yes Videoconference program: Cisco Telepresence videoconferencing client |
|
| Trondsen et al. 2018 Norway 34 |
Aim of study: To explore experiences of social interaction in which both patients, nurses, and psychiatrists are involved regarding video consultations in psychiatric emergencies Design: Qualitative exploratory design Method: Semi-structured interviews Analysis: Stepwise-deductive-inductive approach Typology: Interpretive explanation Language: English Author discipline: Sociology |
N: 5 Gender: 1 man and 4 women Age: 18–51 years Diagnoses: Varied Provider: Psychiatrists supported by nurses in person Sampling plan: Purposive |
Treatment type: Psychiatric assessment in emergency consultations Sessions: Patients were at regional psychiatric centers where nurses assessed if the patients needed to talk with a psychiatrist. The patient had one video consultation with the psychiatrist where the nurse was present without intervening Met provider first: no Videoconference program: not stated |
|
| Ye et al. 2012 USA, Georgia and California 35 |
Aim of study: To examine the extent to which Korean patients accept a telepsychiatric service Design: Questionnaire survey Method: Qualitative open-ended questions in survey Analysis: Responses were reviewed to identify themes and patterns in the text. Each theme was further coded into several categories Typology: Thematic survey Language: English Author discipline: Public Health and Communication |
N: 16 patients speaking Korean Gender: 5 men and 11 women Age: Mean 45.1 years Diagnoses: Depressive disorders, anxiety disorders, and adjustment disorders Provider: A psychiatrist with Korean background Sampling plan: Purposive |
Treatment type: Medication management and supportive psychotherapy Sessions: All received an initial diagnostic assessment that lasted 45–90 min. Each patient received up to three additional sessions that lasted 30 min. The patients were in Georgia and the psychiatrist in California. Sessions were in Korean Met provider first: no Videoconference program: Tandberg Movi on laptop computers |
|
Findings
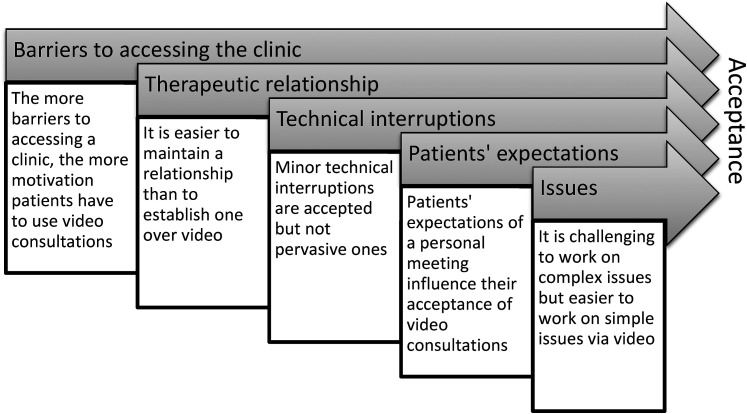
Five themes emerged that captured the patients’ view of factors that would influence their acceptance of video consultations. The factors have a certain hierarchy in the sense that the first factor is more critical than the second factor. The factors also interact with each other. For example, patients were more willing to accept establishing a therapeutical relationship over video, technical interruptions, and handling more complex issues over video, when access to the clinic was hampered. Moreover, technical interruptions made it harder to establish a therapeutic relationship, and patients’ expectations and issues affected the requirements for the therapeutic relationship. Patients’ expectations of how personal they wanted their sessions with their therapists to feel like are, additionally, dependent on the issues that needed to be addressed in that particular session. Figure 2 shows the relationship between the factors.
Figure 2.
Factors influencing patients’ acceptance of video consultations.
Barriers to accessing the clinic
The reason why patients in all of the included studies were using video consultations was that they had difficulties accessing a mental health clinic or a specialist. Patients expressed that videoconferencing was convenient and sometimes the only option for receiving therapy, e.g. due to COVID-19 restrictions.28,30 They especially emphasized that they could save time. This was considered particularly relevant for those who lived furthest away from services, but also for those where the sessions would have an anticipated short duration due to the trade-off between transportation and therapy.25,26,28,29,33 Rough weather and dependency on public transportation were also considered by some patients as an obstacle to accessing the clinic. 33 Barriers and inconvenience were, however, also found at home. Some patients experienced that it was difficult to establish a private place at home,25,27,28,30 and some mentioned that staying home kept them socially isolated. 25
Specialized care is often centralized which increases distances to services for more people. Two of the studies included patients from a regional psychiatric center and a general practice who were provided access with a psychiatrist for psychiatric assessments. Patients would otherwise not have had direct contact to a psychiatrist which led most of the patients to be very satisfied with these services.31,34 In another study, patients could get access to a clinic specialized in military-related post-traumatic stress disorder, 25 and in the second study, Korean immigrants could get access to a psychiatrist with the same cultural background who spoke the patients’ native language. 35 The ability to get access to specialized care was themes in both studies that affected the patients’ acceptability of video consultations.
In Hensel et al.'s study, 29 of women with postpartum depression, they found that the more barriers to accessing the mental health clinic, or the lower tolerance for the inconvenience, the more motivated the women were for using videoconferencing. In Tarp and Nielsen's study, 33 of patients with alcohol use disorder, they similarly found that it was practical matters and inconvenience that influenced patients’ decision to use videoconferencing.
Given that many patients in the included studies describe that they prefer in-person sessions,26,27,29,33 patient experienced barriers and inconvenience regarding accessing mental health clinics are the primary reason to consider videoconferencing.
Patients’ relationship with their therapist
In all the studies where the patients met their therapist in person before they had psychotherapy via videoconference, patients mentioned that they thought it was particularly helpful to meet in person first, and that it was important to meet in person to establish a trusting relationship.25–27,30,33 Continuing a relationship over videoconference was in general not considered problematic. Hensel et al. 29 further found that an already established trustful relationship promoted interest in videoconferencing. In the study of Simpsons et al., 32 the patients never met their therapist. Yet, they managed to develop a strong therapeutic relationship. They would, though, prefer in-person sessions, until rapport was developed between them and their therapist. Patients, therefore, have more confidence in developing a relationship in person than over video.
In comparison to telephone conversations, video consultations were most often seen by patients as a superior way to communicate since the ability to see the other person increased trust25,26,29,33
Regarding the studies where the patients were being assessed by a psychiatrist, the patients, who were already supported in person by mental health nurses or general practitioners, had confidence in the psychiatrists’ competence and role as an expert even though they met via a videoconference.31,34
In conclusion, patients find it more acceptable to use videoconferencing for psychotherapy when a relationship with the therapist is already established.
Technical interruptions
Hensel et al. 29 found that access to and comfort with videoconferencing technology, including the ability to tolerate and troubleshoot technical difficulties, influenced actual engagement with videoconferencing. Many of the patients in most of the included studies had experienced technical interruptions, such as screen freezing and connection problems, however, they were typically considered annoying but not destructive for therapy.25–27,29–33,35 As an example, Hensel et al. 29 found that participants normalized and tolerated technological issues which, provided they were minor and/or resolved quickly, did not interfere with videoconferencing engagement. In a few other cases, the technology was too disruptive and let the participants to drop video sessions.29,33 In addition, Simpsons et al. 32 reported on a patient that explained that technical difficulties were tolerated due to the quality of the alliance with the therapist. Furthermore, older patients experienced that technical challenges could compromise the integrity of the therapeutic contact. 26 Therefore, the therapeutic relationship could be affected by technical interruptions, and how well technical interruptions were tolerated could depend on the therapeutic relationship already established.
In conclusion, the extent of technical interruptions and how they are resolved, is critical for videoconferencing use. Minor technical interruptions are, in general, accepted but not pervasive ones.
Patients’ expectations
In most of the studies where the patients met their therapist before they had a video session, patients explained how the video sessions were similar to in person sessions. The sessions were about the same things, and the treatment was considered similar.25–27,33 In one study, 30 though, video sessions were considered as an independent type of therapy. However, in all of the studies, patients mentioned that the contact was less personal and intense than if it was in person. This was, among other things, due to that it was harder to read body language over a screen. That patients described their sessions as both similar to in-person sessions and not similar in terms of experienced intimacy might reflect their different expectations regarding the degree of how personal the consultations ought to be as found by Christensen et al. 26 They found that some patients preferred in-person sessions because of the more personal contact, and others were indifferent since they were able to experience a professional meeting with their therapist even when the sessions were less personal. In Frayn et al.'s 28 study, they similarly found that the impersonal nature of video sessions made one patient feel more able to be open toward the therapist and hence preferred video to in-person sessions, whereas for others, it had the opposite effect. That is, patients’ expectations regarding how personal a consultation needs to be influences their acceptance of the service. Patients’ expectations might, though, change over time since it appeared that experience with psychotherapy over video consultation made the patients feel more confident in the treatment modality.26,30,32
Complexity of issues
Some patients felt that video consultations would mostly be suitable for less deep conversations.26,33 In Lekhardt et al.'s 30 study, where the therapists used a psychoanalytic approach, the patients experienced that some topics were dealt with more superficially, and specific topics were, therefore, considered to be addressed more appropriately in in-person sessions only. In the study of Christensen et al., 26 patients described that they felt it was more difficult to delve into complex issues over video and, therefore, deemed video consultations less suitable during acute stages of illness, and more appropriate during stable stages. They further found that the degree of depression and purpose of the conversation seemed to influence whether an optimal relationship with their therapist could be created. It was easier for patients with mild depression to create a good relationship over video than it was for those with chronic and complex problems. Moreover, patients with mild depression tended to be more positive than those with moderate depression about using videoconferencing for all of their therapy sessions.
Regarding anxiety-related issues, some patients experienced that having therapy at home could alleviate the anxiety they had associated with leaving home. This was particularly relevant when the anxiety was intense. They were, therefore, more relaxed, and it was easier for them to attend, engage, and open up in terms of content and emotions in the home-based video sessions.25,29,30,33 However, the authors mentioned that the participants did not have complex issues.
In conclusion, patients’ issues, and the character of the subject of conversation in particular sessions, affect the acceptability of videoconferencing for specific consultations. In general, it is challenging to work on complex issues but easier to work on simple issues via videoconferencing.
Discussion
Comparisons between therapeutic courses held in person or via video have shown similar clinical effectiveness.13,14 In these studies, patients have been randomized into either the in-person or video format. However, video consultations display certain advantages and drawbacks, and to utilize this technology most efficiently, it is very relevant to know how to blend this service with usual practice. Previous studies have found psychiatric video consultations to be acceptable by most patients,1,5 but the studies are often limited to survey questions about easier access and usability of the technologies involved in particular settings. This synthesis sought to better understand what makes video consultations acceptable for the patients involved in general. Based on the synthesis, a hierarchical model with five factors is proposed. This model is intended to help clinicians decide when to consider offering video consultations to patients.
The first factor did relate to barriers in regard to accessing the clinic. The more barriers, the more acceptable the services were. During the COVID-19 pandemic, mental health services have been compelled to virtualize their services; a decisive barrier for in-person sessions. This has had an impact on all patients regardless of residence and socioeconomic status. Interestingly, Mishkind et al. 36 found that no-show rates for video consultation sessions dropped from more than 16.1% pre COVID-19 restrictions to 7.8% post, which might be due to the higher perceived barriers to in-person services, but at least it indicates that the services were acceptable for many patients during a health crisis.
The second factor found in the synthesis was that patients expressed a preference to meet their mental health provider before their first psychotherapeutic video session, and knowing the therapist increased their interest in trying video sessions. This is an aspect that many therapists feel as well. 37 However, to some patients, video sessions are the only contact option, and in these cases, the barriers to access therapy combined with the patient's mental health needs surpass the patient’s desire to meet the therapist beforehand.
The third factor was that technological disturbances were most often tolerated but not pervasive ones. This is relevant to consider when adopting new technologies for practice. Given that patients are more accepting of video consultations when they know their therapist introducing new videoconferencing services might be most suitable for patients who are already familiar with their therapist until the service is properly integrated and all technological challenges are solved. Furthermore, regarding home sessions, it is also important to consider what access to videoconferencing equipment the patients have in their home, and whether it is possible, justifiable, and efficient to lend equipment to patients with insufficient equipment for a period. Finally, the videoconferencing programs must be compatible with most devices and operating systems and follow national and regional legislation in that field.
The fourth factor related to what expectations patients have regarding the type of conversation they will be using videoconferencing for. Some patients mentioned that they felt that video sessions were less personal due to the decreased ability to read non-verbal cues and consequently preferred in-person sessions. Others did not have a preference since they experienced a useful and professional meeting even though it was less personal. Personality traits, attachment style, experience, and type of consultation all affect these expectations. During the COVID-19 restrictions, many patients and mental health care clinicians have gained experience with video consultations 36 and may, as a result, have acquired videoconferencing specific communication skills that will improve the ability to convey emotions and hence create the feeling of a more personal meeting. In Gullslett et al.'s 37 study, therapists did indicate that experience made it easier for them to interact with their patients. Moreover, more patients might experience that even though they may feel that the sessions are less personal, the session can still be professional and sufficient since the therapeutic bond that is created in videoconferencing psychotherapy does not appear to affect treatment outcome whereas agreement on therapeutic tasks and goals do. 38 Current increased experience might heighten the acceptability of video consultations in the near future, and due to the potential drift of patients. Perspectives, research following up on this seems very relevant to ensure the continuous work with implementing this service into usual practice.
Finally, the fifth factor related to the type of consultation where videoconference should be used. When patients had a more complex presentation of symptoms, video consultations were less useful, and vice versa for more straightforward cases. This might be explained by patients not being able to express themselves just as well over video and that the interaction thus is being challenged. Patients mentioned that some topics were dealt with more superficially, which is in line with Gullslett et al.'s 37 study. They found that therapists were concerned about not wanting to dig to deeply into vulnerable feelings or traumas over video. They explained that it was due to their reduced ability to read their patients’ emotional state sufficiently and their fear of leaving their patients in an unresolved state if technical break downs would occur in the middle of a critical conversation. On the other side, when the barriers to accessing a clinic are related to symptoms of illness, such as seen with certain anxiety disorders, video consultations might be considered very acceptable from the patients’ perspective. However, this factor of complexity is the least supported area, and more research is desirable.
Several barriers to widespread adoption exist and it has made therapists reluctant to implement video consultations into their practice. 17 The COVID-19 crisis has revealed the potential telepsychiatry holds, and accelerated policymakers’ actions to promote telepsychiatry and remove barriers.2,39 Building up a telepsychiatry network demands training for best practice. The actions taken during the COVID-19 crisis will, therefore, hopefully help improve healthcare systems’ response to future emergencies and sustain the increased access to mental health care. These actions may promote the use of video consultations in the future, making further research in this area exceptionally relevant.
Limitations
The included studies captured a wide range of settings, e.g. where different consultations, both psychotherapeutic and psychiatric assessments, were used; where the patient was at home or at a clinic; where video consultations were used flexible or during a full treatment course; and where participants belonged to different diagnostic groups. This enabled the ability to draw a broad conclusion across settings but limited the specificity. For example, the type of consultations patients with different problems may consider most acceptable for video sessions is not completely clear. However, this also refers to the number of included studies; only 11 meet the inclusion criteria. Thus, there is a potential to improve our model and understanding of patients’ perspectives with more research in the area. Even though we had a broad inclusion, we did not find any studies of patients diagnosed with schizophrenia or bipolar disorders. Neither did we look at allied health and psychosocial support providers. This limits the transferability.
It is also important to note that in these studies, patients had already consented to participate in video consultations, and the results may consequently be that patients had more positive attitudes toward video consultations than among the general population. Three of the included studies did, though, include patients who were offered video consultations but did not use it. The other patients had all used it and were able to explain how they found video sessions more or less acceptable based on their actual experience. However, a pre-implementation study by Bleyel et al. 40 looking at mental health patients anticipated benefits and barriers of accessing specialist care via video from general practice, found, similar to our findings, that the patients were specifically positive toward the increased and easier access which would lead them to accept the service but would, all things being equal, prefer in-person encounters.
Regarding the quality of the included reports, only one had adequately considered the relationship between the researcher and participants. This means that they are lacking transparent self-reflection and their intention with their study presentation is not clear. Furthermore, about half of the included reports were defined as thematic surveys, and it can be questioned as to what degree they capture the essence of the patients’ experiences.
The systematic search with dual-author screening, eligibility assessment, and quality appraisal to minimize biased selection of studies, as well as the dual-author auditors in the analysis process ensured a thorough search. Regarding the search strategy, it turned out to be very difficult to find precise search words that would capture the videoconferencing technology. Words such as “telepsychiatry” and “telemedicine” refer to treatments at a distance and include several aspects other than videoconferencing, such as phone calls and e-mails. Hence the initial search revealed a very high number of studies. We, therefore, consider that the present search method has high recall but low precision. However, synthesis studies should emphasize recall over precision to ensure an exhaustive search. 24 Some relevant studies may, though, have been missed due to publication bias or exclusion of grey literature. Further, the literature review was not preregistered, and, therefore, not available for inspection by other researchers. Preregistration could have ensured a more thorough search. However, the search strategy was developed with the assistance of a professional university librarian.
Finally, a condition in qualitative analyses is that it might be influenced by the analyst's preconceptions, and this synthesis must therefore be considered as one interpretation among other possibilities.
Conclusion
The aim of this synthesis of qualitative research is to explore factors that affect mental health patients’ acceptability of video consultations. A five-factor model is proposed to explain what circumstances clinicians should be aware of when they consider offering video consultations to patients. Overall, it revealed that patients find video consultations acceptable when barriers to in-person services exist and when it is perceived not to intervene with their treatment and the therapeutic process. Eleven qualitative research reports were included, so more research in the field would further clarify acceptance among different patients in different settings. None of the studies included for instance patients with schizophrenia or bipolar disorder. Finally, given that experience made video consultations more acceptable, it would be interesting to conduct longitudinal studies to look at why that is, e.g. if it is related to improved interaction skills or different expectations, and whether the reorganization of in-person sessions to videoconferencing during the COVID-19 will increase its use prospectively.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Contributorship: AMM and LFC conducted the literature search. AMM conducted the analyzing steps and JPH and PTA audited these steps. AMM wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Ethical approval: Not applicable, because this article does not contain any studies with human or animal subjects.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a research grant from the Mental Health Services in the Region of Southern Denmark and a scholarship from the University of Southern Denmark.
Guarantor: AMM.
Informed consent: Not applicable, because this article does not contain any studies with human or animal subjects.
Peer review: Dr. Markus W Haun.
Trial registration: Not applicable, because this article does not contain any clinical trials.
ORCID iD: Anne Marie Moeller https://orcid.org/0000-0003-4183-563X
References
- 1.Greenwood J, Chamberlain C, Parker G. Evaluation of a rural telepsychiatry service. Australas Psychiatry 2004; 12: 268–272. [DOI] [PubMed] [Google Scholar]
- 2.Kannarkat JT, Smith NN, McLeod-Bryant SA. Mobilization of telepsychiatry in response to COVID-19-moving toward 21(st) century access to care. Adm Policy Ment Health 2020; 47: 489–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Simpson J, Doze S, Urness D, et al. Telepsychiatry as a routine service--the perspective of the patient. Telemed J E Health 2001; 7: 155–160. [DOI] [PubMed] [Google Scholar]
- 4.Simpson S. Psychotherapy via videoconferencing: a review. Br J Guid Counc 2009; 37: 271–286. [Google Scholar]
- 5.Whitten P, Kuwahara E. A multi-phase telepsychiatry programme in michigan: organizational factors affecting utilization and user perceptions. J Telemed Telecare 2004; 10: 254–261. [DOI] [PubMed] [Google Scholar]
- 6.Bird MD, Chow GM, Meir G, et al. The influence of stigma on college students’ attitudes toward online video counseling and face-to-face counseling. J Coll Couns 2019; 22: 256–269. [Google Scholar]
- 7.Clement S, Schauman O, Graham T, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med 2015; 45: 11–27. [DOI] [PubMed] [Google Scholar]
- 8.Backhaus A, Agha Z, Maglione ML, et al. Videoconferencing psychotherapy: a systematic review. Psychol Serv 2012; 9: 111–131. [DOI] [PubMed] [Google Scholar]
- 9.Chakrabarti S. Usefulness of telepsychiatry: a critical evaluation of videoconferencing-based approaches. World J Psychiatry 2015; 5: 286–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Christensen LF, Moller AM, Hansen JP, et al. Patients’ and providers’ experiences with video consultations used in the treatment of older patients with unipolar depression: a systematic review. J Psychiatr Ment Health Nurs 2019; 27: 258–271. [DOI] [PubMed] [Google Scholar]
- 11.Hilty DM, Ferrer DC, Parish MB, et al. The effectiveness of telemental health: a 2013 review. Telemed J E Health 2013; 19: 444–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jenkins-Guarnieri MA, Pruitt LD, Luxton DD, et al. Patient perceptions of telemental health: systematic review of direct comparisons to In-person psychotherapeutic treatments. Telemed J E Health 2015; 21: 652–660. [DOI] [PubMed] [Google Scholar]
- 13.Norwood C, Moghaddam NG, Malins S, et al. Working alliance and outcome effectiveness in videoconferencing psychotherapy: a systematic review and noninferiority meta-analysis. Clin Psychol Psychother 2018; 25: 797–808. [DOI] [PubMed] [Google Scholar]
- 14.Thomas N, McDonald C, deBoer K, et al. Review of the current empirical literature in using videoconferencing to deliver individual psychotherapies to adults with mental health problems. Psychol Psychother 2021; 94: 854–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O’Reilly R, Bishop J, Maddox K, et al. Is telepsychiatry equivalent to face-to-face psychiatry? Results from a randomized controlled equivalence trial. Psychiatr Serv 2007; 58: 836–843. [DOI] [PubMed] [Google Scholar]
- 16.Christensen LF, Gildberg FA, Sibbersen C, et al. Disagreement in satisfaction between patients and providers in the Use of videoconferences by depressed adults. Telemed J E Health 2020; 26: 614–620. [DOI] [PubMed] [Google Scholar]
- 17.Cowan KE, McKean AJ, Gentry MT, et al. Barriers to Use of telepsychiatry: clinicians as gatekeepers. Mayo Clin Proc 2019; 94: 2510–2523. [DOI] [PubMed] [Google Scholar]
- 18.Wynn R, Bergvik S, Pettersen G, et al. Clinicians’ experiences with videoconferencing in psychiatry. Stud Health Technol Inform 2012; 180: 1218–1220. [PubMed] [Google Scholar]
- 19.Simpson SG, Reid CL. Therapeutic alliance in videoconferencing psychotherapy: a review. Aust J Rural Health 2014; 22: 280–299. [DOI] [PubMed] [Google Scholar]
- 20.Wind TR, Rijkeboer M, Andersson G, et al. The COVID-19 pandemic: the ‘black swan’ for mental health care and a turning point for e-health. Internet Interv 2020; 20: 100317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miller EA. Telemedicine and doctor-patient communication: an analytical survey of the literature. J Telemed Telecare 2001; 7: 1–17. [DOI] [PubMed] [Google Scholar]
- 22.Sandelowski M, Barroso J. Classifying the findings in qualitative studies. Qual Health Res 2003; 13: 905–923. [DOI] [PubMed] [Google Scholar]
- 23.Critical Appraisal Skills Programme. CASP Qualitative Checklist, https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist-2018.pdf (2018, accessed 1 March 2021).
- 24.Sandelowski M, Barroso J. Handbook for synthesizing qualitative research. New York: Springer Publishing Company, 2007. [Google Scholar]
- 25.Ashwick R, Turgoose D, Murphy D. Exploring the acceptability of delivering cognitive processing therapy (CPT) to UK veterans with PTSD over skype: a qualitative study. Eur J Psychotraumatol 2019; 10: 1573128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Christensen LF, Wilson R, Hansen JP, et al. A qualitative study of patients’ and providers’ experiences with the use of videoconferences by older adults with depression. Int J Ment Health Nurs 2021; 30: 427–439. [DOI] [PubMed] [Google Scholar]
- 27.Frank F, Ower N, Zech J, et al. Videokonferenzbasierte psychotherapeutische anschlussbehandlung: qualitative fallstudie mit einem CBASP-aansatz [video conference-based psychotherapeutic follow-up treatment. Qualitative case study using a CBASP approach]. Psychotherapeut 2017; 62: 355–360. [Google Scholar]
- 28.Frayn M, Fojtu C, Juarascio A. COVID-19 and binge eating: patient perception of eating disorder symptoms, tele-therapy, and treatment implications. Curr Psychol 2021; 40: 6249–6258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hensel JM, Yang R, Vigod SN, et al. Videoconferencing at home for psychotherapy in the postpartum period: identifying drivers of successful engagement and important therapeutic conditions for meaningful use. Couns Psychother Res 2021; 21: 535–544. [Google Scholar]
- 30.Leukhardt A, Heider M, Reboly K, et al. Videobasierte behandlungen in der psychodynamischen psychotherapie in zeiten der COVID-19-pandemie. Interviewstudie mit psychotherapeut*innen und patient*innen [video-based treatment in psychodynamic psychotherapy in times of the COVID-19 pandemic. Interview study with patients and psychotherapists]. Psychotherapeut 2021; 66: 398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.May C, Gask L, Ellis N, et al. Telepsychiatry evaluation in the north-west of england: preliminary results of a qualitative study. J Telemed Telecare 2000; 6: S20–S22. [DOI] [PubMed] [Google Scholar]
- 32.Simpson S, Guerrini L, Rochford S. Telepsychology in a university psychology clinic setting: a pilot project. Aust Psychol 2015; 50: 285–291. [Google Scholar]
- 33.Tarp K, Nielsen AS. Patient perspectives on videoconferencing-based treatment for alcohol Use disorders. Alcohol Treat Q 2017; 35: 344–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Trondsen MV, Tjora A, Broom A, et al. The symbolic affordances of a video-mediated gaze in emergency psychiatry. Soc Sci Med 2018; 197: 87–94. [DOI] [PubMed] [Google Scholar]
- 35.Ye J, Shim R, Lukaszewski T, et al. Telepsychiatry services for Korean immigrants. Telemed J E Health 2012; 18: 797–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mishkind MC, Shore JH, Bishop K, et al. Rapid conversion to telemental health services in response to COVID-19: experiences of Two outpatient mental health clinics. Telemed J E Health 2021; 27: 778–784. [DOI] [PubMed] [Google Scholar]
- 37.Gullslett MK, Kristiansen E, Nilsen ER. Therapists’ experiences of video consultation in specialized mental health services during the COVID-19 pandemic: qualitative interview study. JMIR Hum Factors 2021; 8: e23150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marcotte-Beaumier G, Bouchard S, Gosselin P, et al. The role of intolerance of uncertainty and working alliance in the outcome of cognitive behavioral therapy for generalized anxiety disorder delivered by videoconference: mediation analysis. JMIR Ment Health 2021; 8: e24541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.United Nations. Policy Brief: COVID-19 and the Need for Action on Mental Health, https://unsdg.un.org/sites/default/files/2020-05/UN-Policy-Brief-COVID-19-and-mental-health.pdf (2020, accessed 1 March 2021).
- 40.Bleyel C, Hoffmann M, Wensing M, et al. Patients’ perspective on mental health specialist video consultations in primary care: qualitative preimplementation study of anticipated benefits and barriers. J Med Internet Res 2020; 22: e17330. [DOI] [PMC free article] [PubMed] [Google Scholar]