Significance
Public health agencies worldwide have determined that there is no safe level for children’s exposure to lead, a neurotoxin. This study shows that lead in drinking water from private wells is significantly associated with juvenile delinquency. Compared to children in homes with public water supplies, those relying on private wells have a 21% higher risk of any delinquency and a 38% increased risk of serious delinquency. The steepest increases in risk occur at the lowest exposure levels. The results highlight the need to prevent lead-leaching from well components, plumbing, and fixtures in the 13% of US households relying on private wells. They also suggest the need to decrease blood and environmental lead thresholds currently used to identify at-risk children.
Keywords: drinking water, children's health, lead exposure, juvenile delinquency, private well water
Abstract
Early life exposure to environmental lead (Pb) has been linked to decreased IQ, behavior problems, lower lifetime earnings, and increased criminal activity. Beginning in the 1970s, limits on Pb in paint, gasoline, food cans, and regulated water utilities sharply curtailed US environmental Pb exposure. Nonetheless, hundreds of thousands of US children remain at risk. This study reports on how unregulated private well water is an underrecognized Pb exposure source that is associated with an increased risk of teenage juvenile delinquency. We build a longitudinal dataset linking blood Pb measurements for 13,580 children under age 6 to their drinking water source, individual- and neighborhood-level demographics, and reported juvenile delinquency records. We estimate how early life Pb exposure from private well water influences reported delinquency. On average, children in homes with unregulated private wells had 11% higher blood Pb than those with community water service. This higher blood Pb was significantly associated with reported delinquency. Compared to children with community water service, those relying on private wells had a 21% (95% CI: 5 to 40%) higher risk of being reported for any delinquency and a 38% (95% CI: 10 to 73%) increased risk of being reported for serious delinquency after age 14. These results suggest that there could be substantial but as-yet-unrecognized social benefits from intervention programs to prevent children’s exposure to Pb from private wells, on which 13% of the US population relies.
The US Centers for Disease Control and Prevention (CDC) has ranked childhood lead (Pb)-poisoning prevention as one of the 10 great public health achievements of the past several decades (1). Blood Pb in the US population has decreased by nearly 94% since the 1970s due to public health interventions including bans on Pb in paint, gasoline, and food cans, limits on Pb content in household plumbing and fixtures, and corrosion control programs to prevent Pb exposure from community water supplies (2). The benefits of these reductions have been estimated at $213 billion/y (3).
Despite these gains, recent public health surveillance data and epidemiologic studies indicate that Pb exposure continues to cause harm. In 2018, the CDC identified 87,144 US children under age six with blood Pb concentrations above its reference level for elevated blood Pb (5 µg/dL at the time) (4). The true number of children with elevated blood Pb is much higher, because these data only account for a small fraction of US children. Several states (Arkansas, California, Delaware, Idaho, Kentucky, Michigan, Montana, North Dakota, and Utah) did not report 2018 blood Pb surveillance data to the CDC; New York state data did not include records from New York City. Even in the states and communities reporting blood Pb surveillance data, only 17.6% of children under age 6 were tested. In addition, an increasingly large body of evidence indicates that neurocognitive damage to children occurs at blood Pb concentrations much lower than 5 µg/dL (5–7). Reflecting on this evidence, the CDC in October 2021 decreased its recommended reference level for elevated blood Pb to 3.5 µg/dL.
Our recent research suggests that lack of access to a regulated community water supply may be an underrecognized, insufficiently controlled source of Pb exposure risk in children (8, 9). Overall, 13% of the US population relies on unregulated drinking water supplies, mostly private wells (10). We found that children in homes without community water service have significantly higher blood Pb than those served by a regulated water utility (8). Presumably, the increased Pb exposure occurs because these unregulated systems are not subject to the Safe Drinking Water Act and therefore are neither routinely monitored nor treated to prevent Pb release from well components, household plumbing, and faucets and fixtures that often contain Pb-rich brasses, solders, and other materials (11, 12). Those without community water service must be stewards of their own water quality, and few test or treat their water to prevent the dissolution of Pb (13–15). Indeed, the costs of monitoring and treatment are beyond the reach of many low-income households (14–16).
Multiple previous studies have demonstrated that early life Pb exposure influences teenage risks for behavioral problems, including school suspension and juvenile delinquency (17–21). Studies also have linked early life Pb exposure to increased risk of criminal behavior during adulthood (18, 22, 23). However, none of the previous studies has assessed the effect of consuming Pb-contaminated drinking water early in life on future behaviors of US teens. Furthermore, little research is available, in general, on health risks from Pb in US private well water (8, 24).
In this study, we examine whether increased Pb exposure from drinking water among children in homes relying on private wells is associated with an increased risk of being reported for juvenile delinquency. Our analysis is based on a 20-y dataset of children’s blood Pb measurements, household water sources, and juvenile delinquency records. In addition to being a US study to examine the effects of Pb exposure from drinking water on children’s behavior, this is one of few recent studies linking individual-level early life blood Pb measurements to individual juvenile delinquency records many years later (25). By using drinking water source as an instrument for characterizing early life Pb exposure, we capture the impacts of chronic exposure to Pb in contrast to relying on a one-time blood test as the main exposure measure. This approach also decreases the potential for omitted-variable bias (26). For example, structural factors have led to differential exposure to environmental Pb by race (27) and also to inequities in how authorities (including school and law enforcement officials) respond to adolescent behaviors (28). It is possible that controlling for race in models to estimate the effects of Pb on juvenile delinquency risk does not fully correct for common structural factors influencing both Pb exposure and the risk of an encounter with the juvenile justice system. In this study, the potential for omitted-variable bias is decreased by using a two-stage, least-squares regression approach. Another distinguishing feature is the study’s scale. This study is based on a cohort of 13,580 children. In contrast, apart from a recent report from Rhode Island (21), previous studies with individual-level data have generally relied on smaller sample sizes (e.g., n = 195 for a widely cited study of blood Pb–delinquency relationships in Cincinnati, OH) (29).
Methods
The cohort of children in this study was drawn from records of all children who were tested for blood Pb in Wake County, NC (population 1.1 million), between 1998 and 2011. Wake County provides a useful case study site for examining how drinking water influences children’s blood Pb and later-life outcomes, because it is one of few areas where water service data are publicly available at the residential parcel scale (13, 30) and because compliance with recommended blood Pb screening is high. For example, in 2010, eight children were screened for blood Pb for every 10 live births (31). The county also has a mix of urban (including Raleigh, the North Carolina capital), suburban, and rural areas with varying water service levels.
As of 2015, ∼137,400 Wake County residents (about 13.4% of the population) relied on unregulated private wells for their drinking water, and the rest were connected to regulated community water systems. This population distribution of community water service levels is comparable to that at the national level (32). Reasons for relying on private well water in Wake County vary. Some homes are in rural areas lacking sufficient population density to support a community water system; about 6% of the county population lives in rural areas (33). Others are in wealthy, newer exurban developments with large lots (34). Such developments are relatively common in Wake County, one of the fastest-growing counties in the United States (Time magazine has nicknamed Raleigh, which is located in Wake County, “Sprawleigh”) (35). Some homes on well water are in relatively densely populated, majority Black communities that were historically excluded from municipal incorporation and access to municipal services through exclusionary zoning practices, a phenomenon that has been called “municipal underbounding” (16, 34, 36).
Our analysis assessed whether reliance on unregulated private well water during early childhood influences the risk of being reported for delinquency during teenage years through the effects of well water on Pb exposure. The analysis considered two binary outcomes:
-
1.
whether any official juvenile complaint was recorded against the child between age 14 and when they reached adult status as defined by the juvenile court system, and
-
2.
whether the child had a record for any serious complaint, defined as felony property or weapons offenses or misdemeanor assault.
Data Sources
Blood Pb measurements were provided by the NC Childhood Lead Poisoning Prevention Program for all children tested between 1998 and 2017. Blood Pb measurements were matched to each child’s drinking water source (private well or community system) at the time of their first blood Pb test as described elsewhere (8).
Juvenile delinquency reports for the children in the database of linked blood Pb measurements and drinking water sources were retrieved by the NC Department of Public Safety (DPS) for all children who reached at least age 14 by December 31, 2019 (n = 17,868). DPS searched its delinquency database through December 31, 2019, using names and birthdates to match records (refer to SI Appendix for a description of the matching algorithms). Until December 1, 2019, youths only had juvenile status until their 16th birthday; subsequently, this age cutoff was increased to 18.
To account for the effects of neighborhood socioeconomic and demographic characteristics on the children’s teenage behavior, information on their residential address at age 14 was obtained from the NC Education Research Data Center (NCERDC) using various combinations of each child’s first and last name, birthdate, and address at the time of blood-testing (refer to SI Appendix for an explanation of the matching algorithm). Overall, NCERDC located teenage addresses for 76.0% (13,580 of 17,869) of the children. Possible reasons for failure to match included the following:
-
1.
the family relocated to another state;
-
2.
the child was enrolled in a private or parochial school at age 14 or was being homeschooled;
-
3.
the child died; or
-
4.
there was some disparity in the recording of the name between the Pb test record and the school record that was not captured by NCERDC’s sequential matching algorithm (described in the supporting information), which searched for such mismatches.
There were no significant differences between children with and without matched teenage addresses on the key exposure variables of interest: blood Pb and drinking water source (SI Appendix, Table S2). However, those with and without matched school records differed on several demographic covariates. The children without matched school records lived in neighborhoods with slightly lower Black population proportions than those with records (25% versus 28%, P < 0.001; SI Appendix, Table S2). In addition, unmatched children lived higher-value homes at the time of blood-testing ($205,000 versus $185,000, P < 0.001; SI Appendix, Table S2). Children without matched teen addresses were more likely to be female (51.7% versus 49.8%, P < 0.01) and less likely to have a juvenile complaint record (1.3% versus 3.1% for children matched in the NCERDC dataset, P < 0.001; SI Appendix, Table S2). Because the NCERDC and DPS both searched their databases statewide (not just in Wake County), the much-lower reported delinquency rate among those without matched educational records during their teen years likely indicates many had moved out of state. The higher socioeconomic status among those without matched records suggests that attendance in private or parochial schools may also explain some of the lack of complete matching, since the NCERDC database includes only children attending public or charter schools, although the rate of private school attendance in NC is very low (as of 2016, fewer than 8% of the state’s children were enrolled in private schools) (37). Demographic differences between children with matched teenage address information and those lost in the matching were handled by including these covariates in all statistical models.
Construction of Quasi-Experimental Dataset
In this study cohort, children on private well water differed significantly from those on community water along important demographic and socioeconomic characteristic (Table 1). Compared to children with community water service, those on private well water were less likely to be Black (20.8% versus 28.2%), lived in higher-income neighborhoods (median income $82,0.795 versus $69,729), and lived in neighborhoods with a lower proportion of African American residents (22.5% versus 25.7%).
Table 1.
Summary statistics for full dataset
| Variable | Full sample | Community water | Private well | P value for difference |
| N | 13,372 | 11,209 | 2,163 | |
| Characteristics of child | ||||
| Gender (N) (%) | 0.847 | |||
| Female | 6,658 (50.2) | 5,580 (50.2) | 1,078 (50.4) | |
| Male | 6,597 (49.8) | 5,537 (49.8) | 1,060 (49.6) | |
| Race (N) (%) | <0.001 | |||
| All other | 9,758 (73.0) | 8,044 (71.8) | 1,714 (79.2) | |
| Non-Hispanic Black | 3,614 (27.0) | 3,165 (28.2) | 449 (20.8) | |
| Age at time of Pb test, months (N) (%) | 0.259 | |||
| 0 to 8 | 93 (0.695) | 79 (0.705) | 14 (0.647) | |
| 9 to 14 | 7,324 (54.8) | 6,106 (54.5) | 1,218 (56.3) | |
| 15 to 19 | 904 (6.76) | 757 (6.75) | 147 (6.80) | |
| 20 to 29 | 1,977 (14.8) | 1,650 (14.7) | 327 (15.2) | |
| >30 | 3,074 (23.0) | 2,617 (23.3) | 457 (21.1) | |
| Age indicator (mean) (SD) | 0.798 (0.310) | 0.797 (0.311) | 0.803 (0.304) | 0.465 |
| Year of blood test (mean) (SD) | 2005 (1.88) | 2005 (1.88) | 2005 (1.86) | 0.107 |
| Blood draw type (N) (%) | 0.971 | |||
| Capillary | 1,301 (10.7) | 1,091 (10.7) | 210 (10.7) | |
| Venous | 10,815 (89.3) | 9,065 (89.3) | 1,750 (89.3) | |
| Child outcomes | ||||
| Blood Pb, µg/dL (mean) (SD) | 2.30 (1.77) | 2.36 (1.78) | 2.52 (1.65) | <0.001 |
| Blood Pb ≥ 5 µg/dL (N) (%) | 1,241 (9.28) | 1,006 (8.97) | 235 (10.9) | 0.006 |
| Any juvenile complaint (N) (%) | 415 (3.10) | 351 (3.13) | 64 (2.96) | 0.672 |
| Number of juvenile complaints (mean) (SD) | 0.122 (1.251) | 0.117 (1.223) | 0.144 (1.386) | 0.688 |
| Any serious complaint (N (%)) | 191 (1.43) | 160 (1.43) | 31 (1.43) | 0.983 |
| Number of serious complaints (mean) (SD) | 0.0462 (0.606) | 0.0435 (0.579) | 0.0587 (0.730) | 0.975 |
| Characteristics of child’s home at time of blood test | ||||
| Home value (mean) (SD) | $226,468 ($194,458) | $226,448 ($180,381) | $226,575 ($257,904) | 0.984 |
| Built before 1978 (N) (%) | 3,847 (29.7) | 3,249 (29.5) | 598 (31.0) | 0.171 |
| Year built (N) (%) | <0.001 | |||
| Before 1950 | 863 (6.66) | 739 (6.59) | 124 (6.43) | |
| 1950–1977 | 2,984 (23.0) | 2,510 (22.8) | 474 (24.6) | |
| 1978–1987 | 1,959 (15.1) | 1,676 (15.2) | 283 (14.7) | |
| 1988–1997 | 2,673 (20.6) | 2,191 (19.9) | 482 (25.0) | |
| 1998–2002 | 2,941 (22.7) | 2,599 (23.6) | 342 (17.7) | |
| 2003 or later | 1,539 (11.9) | 1,315 (11.9) | 224 (11.6) | |
| Characteristics of child’s census block group, blood test year | ||||
| Median income (mean) (SD) | $71,839 ($31,797) | $69,729 ($31,149) | $82,795 ($32,866) | <0.001 |
| % Black (mean) (SD) | 0.274 (0.233) | 0.287 (0.242) | 0.210 (0.168) | <0.001 |
| Characteristics of child’s census block group, age 14 | ||||
| Median income (mean) (SD) | $76,069 ($33,635) | $75,863 ($33,785) | $77,134 ($32,833) | 0.058 |
| % Black (mean) (SD) | 0.252 (0.224) | 0.257 (0.229) | 0.225 (0.194) | <0.001 |
To support an analysis of the influence of Pb exposure on a population of children with characteristics representative of those in Wake County relying on private wells (as compared to the total county population of children), we created a quasi-experimental dataset in which children on well water were matched to similar children served by a community water system. Children were paired on blood test year, age at time of blood test, year of construction of the home in which they lived at the time of their blood test, dollar value of the home in which they lived when tested for blood Pb (expressed in quartiles of the distribution over all home values), biological sex, and race (non-Hispanic Black or other than non-Hispanic Black). When more than one child with community water service matched a child with private well water on all these characteristics, a match was selected at random from the set of possible matches. At least one match was identified for 1,949 (90.1%) of the 2,163 children on well water, yielding a paired dataset with observations for 3,898 children. The 1,949 children with at least one match on a community water supply did not differ significantly from the full set of 2,163 children on well water along any of the covariates of interest (SI Appendix, Table S3), showing that this dataset is sufficiently representative of Wake County children on well water.
Data Analysis Approach
The influence of water source on Pb exposure and of Pb exposure on delinquency risk was analyzed using a two-stage, least-squares regression approach (38). Models were fitted to the full dataset (n = 13,580) and to the quasi-experimental paired dataset (n = 3,898).
The first stage estimated the effect of private well water on blood Pb in early childhood:
| [1] |
where BloodPbi is the child’s blood Pb before age 6, WaterSourcei is an indicator variable for water source at the time of blood-testing (0 = community water system, 1 = private well), represents the child’s age at the time of the blood test, includes the value and year of construction of the child’s home at the time of their blood Pb test, includes demographic and socioeconomic characteristics of the child’s census block group at the time of the blood test, Zi is the child’s zip code, Ti is the blood test year, are the covariates included in the second-stage model, , and are regression coefficients, and is an error term.
The second stage used the estimated blood Pb from Eq. 1 ( to predict the probability that a child would be reported for delinquency after age 14:
| [2] |
where P(Delinquent)i is the probability that the child will have a juvenile complaint record on or before December 31, 2019, are covariates, and the remaining terms are regression coefficients and an error. Covariates included are the child’s sex and race, the median household income and demographic composition of their neighborhood at age 14, and the fraction of age 16 that the child reaches by the end of the data collection period. The latter variable was defined as 0 if the child was exactly 14 on December 31, 2019, 1 if they were 16 or over, and a fractional number representing the distance between age 14 and their age at the end of data collection if they were between ages 14 and 16. It was not possible to include zip codes in the second-stage model, because doing so resulted in a computationally singular design matrix. In effect, our formulation uses zip codes as additional instruments to predict early life blood Pb.
To avoid loss of information due to missing data, missing covariates (but not dependent variables) were imputed using a k-nearest neighbors approach. This process was repeated 40 times to produce 40 complete datasets, and the two-stage regression models were fitted to each one. In addition, versions of the quasi-experimental dataset were created from each of these simulated datasets, each time selecting a match for each child on well water at random from the set of possible matches. For each sample population (the full dataset and the quasi-experimental dataset), reported coefficients and SEs were averaged from these 40 iterations. Results were substantively similar when estimated with a reduced dataset that included no imputations. SI Appendix provides additional details, including a link to the R code used and instructions for obtaining a de-identified dataset.
The two-stage least-squares regression results were used to obtain two estimates of interest. First, the coefficient in the second stage provided an estimate of the effect of early life blood Pb on delinquency risk that is unbiased by unobserved variables affecting both Pb exposure and delinquency risk. The validity of this estimate requires that water source is correlated with Pb exposure risk but not with any other determinants of delinquency risk other than covariates included in the model (Model Validation) (38). Second, the results from both stages were combined to estimate the effect of Pb exposure risk from private well water on teenage delinquency risk:
| [3] |
Model Validation
We test model validity by evaluating the veracity of four assumptions, as recommended in Lousdal for use of instrumental variables approaches in epidemiologic studies (39):
-
1.
Relevance assumption: The instrument Z (here, reliance on private well water) has a causal effect on exposure variable X (early life blood Pb).
-
2.
Exclusion restriction: Z affects the outcome Y (delinquency risk) only through X.
-
3.
Exchangeability assumption (instrument exogeneity): Z does not share common causes with the outcome Y (conditional on covariates).
-
4.
Monotonicity assumption: Z does not modify the X–Y causal effect.
We verified that these assumptions were satisfied, as follows:
-
1.
Relevance assumption: This assumption is typically tested using the F statistic from the first-stage regression model; an instrument is considered weak if F < 10 (39). Here, F = 86.6 for the dataset representing all Wake County children, and F = 25.3 for the quasi-experimental dataset, providing evidence that reliance on well water is a suitable instrument for blood Pb.
-
2.
Exclusion restriction: To test this assumption, we regressed delinquency risk on water source, blood Pb, and all covariates included in the stage 2 model (SI Appendix, Table S4). The coefficient on blood Pb was significant ( = 0.195, SE = 0.0641, and P < 0.01), while that on well water was not ( = 0.179, SE = 0.142, and P = 0.21), providing evidence that water source affects delinquency risk only through its effects on Pb exposure.
-
3.
Exchangeability assumption (instrument exogeneity): This assumption was evaluated using the J statistic, which tests the null hypothesis that the instruments are uncorrelated with the error term in the second-stage model (40). The null hypothesis was not rejected (SI Appendix, Table S5), supporting the validity of this assumption (SI Appendix). Additional evidence of the validity of this assumption was provided by the analysis of the quasi-experimental dataset, which accounts for potential endogeneity through the matching process used to pair children on well water with similar children on community water.
-
4.
Monotonicity assumption: That Pb neurotoxicity does not vary with source (for the bioavailable Pb fraction) is well established in medical and epidemiologic literature (41). There is no reason that the effect of Pb on health would be modified by water source.
Results
Sample Characteristics.
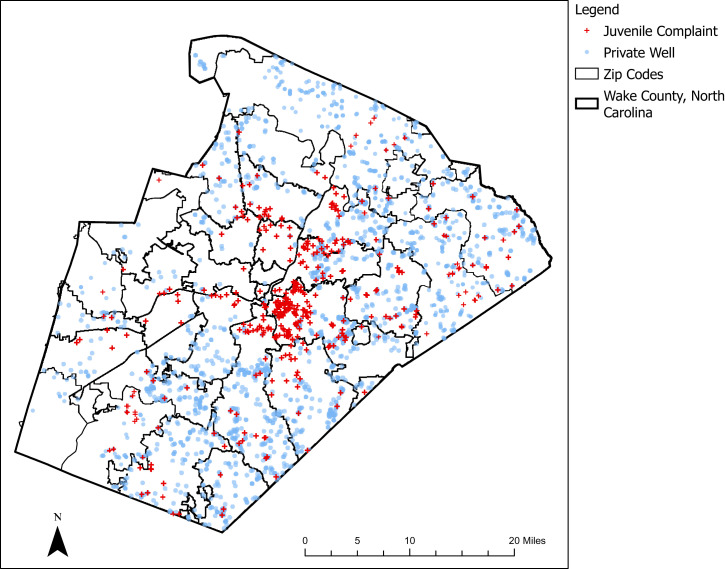
Early life water source information was available for 13,372 of the 13,580 children for whom early life blood Pb and teenage address were matched. Summary statistics for the sample are based on these 13,372 children. In early life (at the time of blood Pb testing), 2,163 (16.2%) relied on private wells, and the rest were served by a community water supply. Table 1 shows the key outcome variables (early life blood Pb and reported juvenile delinquency) and all covariates by water source. Fig. 1 shows locations where children rely on private well water.
Fig. 1.
Locations of children in households relying on private wells (blue dots) and of those with at least one report for delinquency (red crosses).
In the sample, 1,241 children (9.28%) had elevated blood Pb (≥5 µg/dL) as defined by the US CDC before October 2021. Those relying on private well water had a significantly higher risk of elevated blood Pb than children with community water (10.9% versus 8.97%; . Similarly, children on well water had significantly higher blood Pb on average than children on community water (mean = 2.52 µg/dL versus 2.36; P < 0.001).
At least one delinquency report was filed against 415 (3.10%) of the children. Fig. 1 shows (approximate) residential locations of these children. The fractions of children with any delinquency report were 2.96% and 3.13% for children on private wells and community water systems, respectively, and these did not differ significantly. Serious acts of delinquency were reported for 191 (1.43%) of the children, and this rate did not differ by water source.
Demographic characteristics of the children varied significantly by water source. Compared to children with community water service; children on private wells were less likely to identify as Black (20.8% versus 28.2%; P < 0.001). At the time of blood-testing and as teenagers, children on wells lived in census block groups with higher median incomes than those on community water ($82,795 versus $69,230, P < 0.001, at the time of blood-testing and $77,134 versus $75,863, P = 0.058, at age 14).
It is well established that Black and low-income children in the US have higher blood Pb than children of other races and higher socioeconomic status (27). In addition, racial disparities in risks of being reported for juvenile delinquency are well documented (42). Because children on well water in this dataset are less likely to be Black and more likely to live in higher-income areas than children on community water, we would expect them to have lower blood Pb concentrations and lower risks of being reported for juvenile delinquency than children on community water systems. However, instead, children on well water had higher blood Pb, and their risk for juvenile delinquency did not differ significantly from that of children on community water. These bivariate statistics therefore indicate that children on well water may be at increased risk of exposure to Pb, which may in turn increase their risks for teenage delinquency beyond what would be predicted from demographic information. The two-stage least-squares regression results further explore these hypotheses.
Effect of Water Source on Early Childhood Blood Pb.
The stage 1 regression models (Table 2 and SI Appendix, Table S6) provide very strong evidence that reliance on private well water is associated with higher blood Pb even when controlling for other variables known to influence Pb exposure risk (race, income, age of housing, neighborhood socioeconomic and demographic characteristics, and zip code). In both the full population of children and the quasi-experimental population matching children on well water to similar children on community water, blood Pb was about 11% higher among the children with well water compared to those with community water (Table 2 shows that the exponentiated regression coefficients for the effect of well water on the log of blood Pb were 1.11 for the full and quasi-experimental datasets). This result suggests that Pb exposure is higher among children on well water, regardless of their race, socioeconomic status, or sources of exposure to Pb other than water.
Table 2.
Influence of water source and other variables on blood Pb in early childhood
| Variable | Model 1: Full dataset (n = 13,580)* | Model 2: Quasi-experimental matched dataset (n = 3,898)*,† |
| Private well water (reference = community water) | 1.11*** | 1.11*** |
| Year of blood test | 0.889*** | 0.894*** |
| Home value (natural log) | 0.921*** | 0.899*** |
| Construction year of residence during early childhood (reference = before 1950) | ||
| 1950 through1977 | 0.869*** | 0.835** |
| 1978 through 1987 | 0.818*** | 0.819** |
| 1988 through 1997 | 0.786*** | 0.818** |
| 1998 through 2002 | 0.720*** | 0.723*** |
| 2003 or later | 0.781*** | 0.775*** |
| Age at time of blood test, months (reference ≤ 9 mo) | ||
| 9 through 14 | 1.11 | 1.65 |
| 15 through 19 | 1.35*** | 2.14 |
| 20 through 29 | 1.37*** | 2.08 |
| >30 | 1.32*** | 1.93 |
| Blood draw type venous (reference = capillary) | 1.20*** | 1.23*** |
| Black race (reference = all other races) | 1.27*** | 1.20*** |
| Male sex at birth (reference = female) | 1.02 | 0.994 |
| Census block group median income (natural log) at time of blood test | 0.958 | 0.954 |
| Census block group % Black at time of blood test | 1.03 | 0.813 |
| Census block group median income (natural log) at age 14 | 0.973 | 1.025 |
| Census block group % Black at age 14 | 1.19*** | 1.48*** |
| Fraction of age 16 reached at end of data collection | 0.888*** | 0.879* |
*Exponentiated coefficients from model of natural log of blood Pb regressed on all variables indicated with controls for zip code (SI Appendix, Table S6).
†1,949 children in the dataset relying on private well water were matched to 1,949 with community-supplied water on race, biological sex, age at time of blood test, blood test year, year home was built, and home value quartile.
***P < 0.001; **P < 0.01; *P < 0.05
Other Factors Influencing Early Childhood Blood Pb.
Other demographic, economic, and environmental factors were associated blood Pb in both populations (all Wake County children and the quasi-experimental dataset representative of those on well water). Among Black children, blood Pb was 27% higher in the full dataset and 20% higher in the quasi-experimental dataset compared to children of other races (Table 2). Similarly, blood Pb increased with the proportion of Black children in the child’s census block group, regardless of the child’s race. Blood Pb also was significantly higher for children living in older houses, likely reflecting the increased risk of exposure to Pb-based paint before use of Pb in household paint was phased out and ultimately banned in 1978. Blood Pb also decreased as the value of a child’s home increased.
Effect of Early Life Blood Pb on Reported Teen Juvenile Delinquency.
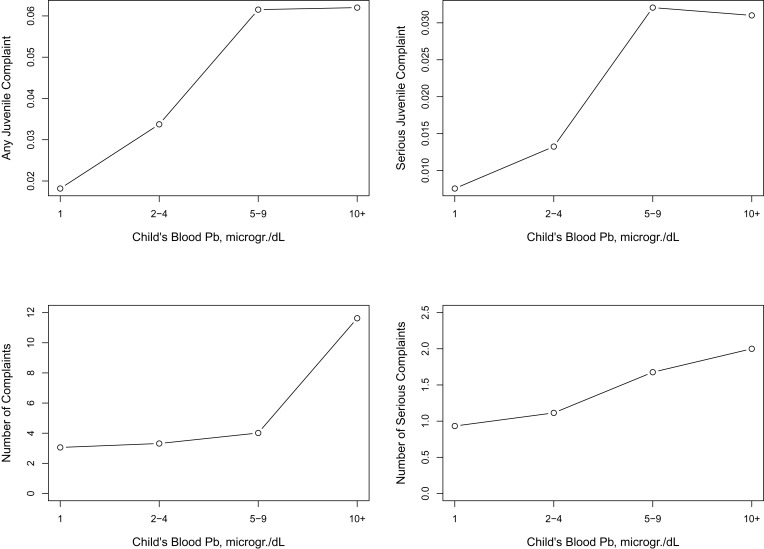
The proportion of teenagers with any record for juvenile delinquency increased with blood Pb as measured during early childhood (Fig. 2). Fewer than 2% of children with early life blood Pb of ≤1 µg/dL had a juvenile complaint record compared to more than 6% for children with ≥5 µg/dL. Similarly, fewer than 0.5% of children with the lowest blood Pb (≤1 µg/dL) had a serious complaint record, compared to more than 3% among those with blood Pb ≥5 µg/dL. The number of complaints and the number of serious complaints against a child also increased as early life blood Pb increased (Fig. 2, Bottom).
Fig. 2.
(Top) Fraction of children in the full sample sample (n = 13,580) reported to the juvenile justice system for any act of delinquency (Left) or serious delinquency (Right) as a function of early life blood Pb. (Bottom) Number of juvenile complaints against children in the dataset as a function of early life blood Pb.
The pattern of increased risk of being reported for juvenile delinquency with increased early life blood Pb also was observed in the results of the two-stage least-squares regression models. In the full population of children, the odds of being reported for juvenile delinquency increased by 3.27 (P < 0.001) for every one-unit change in the log of early life blood Pb (Table 3 and SI Appendix, Tables S7 and S8). The effect size was even stronger when estimating effects using the quasi-experimental dataset: the odds of being reported for delinquency increased by 6.35 (P < 0.001) for every unit increase in the log of early life blood Pb (Table 3, column 3). Equivalently, for a White male in a census block group with demographic characteristics equivalent to the population means reported in Table 1 for private well households, an increase in blood Pb from the first quartile of this population (1 µg/dL) to the third quartile (3 µg/dL) is associated with an increase in the probability of being reported for teenage delinquency from 0.64 to 4.7%. For a Black male, this probability is estimated to increase from 2.5 to 16.5%.
Table 3.
Influence of blood Pb on risk that a child will be reported for juvenile delinquency at age 14 or older
| Variable | Model 1: Full dataset (n = 13,580)* | Model 2: Quasi-experimental matched dataset (n = 3,898)*,† |
| Any delinquency | ||
| Blood Pb (natural log) predicted from water source and other variables (stage 1 model; Table 2) | 3.27*** | 6.35*** |
| Age indicator | 3.05*** | 2.21 |
| Male sex at birth (reference = female) | 2.51*** | 3.44*** |
| Black race (reference = all other) | 2.78*** | 4.01*** |
| Census block group median income (natural log) at age 14 | 0.437*** | 0.284*** |
| Census block group % Black at age 14 | 1.19 | 0.480 |
| Serious delinquency | ||
| Blood Pb (natural log) predicted from water source and other variables (stage 1 model; Table 2) | 4.39*** | 23.4*** |
| Age indicator | 2.36* | 2.88 |
| Male sex at birth (reference = female) | 3.33*** | 2.86** |
| Black race (reference = all other) | 3.05*** | 2.82** |
| Census block group median income (natural log) at age 14 | 0.431*** | 0.295** |
| Census block group % Black at age 14 | 1.29 | 0.419 |
*Exponentiated coefficient from logistic regression model with reported delinquency as dependent variable.
†1,949 children in the dataset relying on private well water were matched to 1,949 with community-supplied water on race, biological sex, age at time of blood test, blood test year, year home was built, and home value quartile.
***P < 0.001; **P < 0.01
The effect of early life Pb exposure on the risk of being reported for serious delinquency was even greater than that for overall delinquency. As estimated using the full population of children, the odds of being reported for serious delinquency report increased by a factor of 4.39 (P < 0.001) per unit increase in the log of blood Pb (Table 3). Using the quasi-experimental dataset, the odds of serious delinquency increase by a factor of 23.4 per unit change in the log of early life blood Pb (Table 3). Equivalently, an increase in blood Pb from 1 to 3 µg/dL in early childhood is expected to increase the probability of being reported for serious delinquency ∼30-fold, from 0.10 to 3.7% for a White male and from 0.34 to 9.8% for a Black male living in an “average” census block group.
These results provide evidence that even very low levels of Pb exposure are associated with substantial population-level effects on children’s risk of delinquency. Notably, effects occur well below the former CDC action level of 5 µg/dL (used until October 2021 as the boundary between “normal” and elevated blood Pb). The two-stage least-squares regression approach increases confidence that these estimates are free from bias that might arise from the omission of unobserved variables that could affect both blood Pb and delinquency risk.
Effect of Water Source on Delinquency Risk through Pb Exposure.
Taken as a whole, the results suggest that young children on private well water are at increased risk of exposure to Pb, which in turn is associated with an increase in their risk of juvenile delinquency during their teen years. The difference in delinquency risk for children on private well water, compared to those with community water service, can be computed from Eq. 3 and the coefficients in Tables 2 and 3. Table 4 shows the results of these computations.
Table 4.
Odds of being reported for juvenile delinquency after age 14 for children on private well water, compared to children with community water
| Outcome | Model 1: Full dataset (n = 13,580)* | Model 2: Quasi-experimental matched dataset (n = 3,898)*,† |
| Any delinquency | 1.13 (1.05 to 1.21) | 1.21 (1.05 to 1.40) |
| Serious delinquency | 1.16 (1.06 to 1.27) | 1.38 (1.10 to 1.73) |
*Estimated from product of coefficient on well water in Table 1 and coefficient on log of blood Pb in Table 2
†1,949 children in the dataset relying on private well water were matched to 1,949 with community-supplied water on race, biological sex, age at time of blood test, blood test year, year home was built, and home value quartile.
In the full population of children, well water was associated with a 13% (95% CI: 5 to 21%) increase in the odds of being reported for any juvenile complaint through its effect on blood Pb and with a 16% (95% CI: 6 to 27%) increase in the odds of a serious complaint. This result suggests that seven of 64 children who relied on private well water and were reported for delinquency could have been prevented from these delinquencies if they had access to water of comparable quality (with respect to Pb exposure risk) as that of the children with community water. Among the 31 children with serious reports of delinquency, four children could have been prevented from reportedly committing these serious acts.
The quasi-experimental dataset suggests an even larger effect of Pb in well water on delinquency risk. Using this dataset, well water was associated with a 21% (95% CI: 5 to 40%) increased risk of being reported for any delinquency and a 38% (95% CI: 10 to 73%) increased risk of being reported for serious delinquency. These results suggest that 11 of 64 children could have been prevented from committing acts of delinquency, and eight of 31 could have been prevented from serious delinquencies.
The larger effect size observed in model 2 (using the matched dataset) may reflect that in Wake County, children on well water are wealthier and less likely to be Black than children with community water service, as shown in the summary statistics in Table 1. Racial disparities in exposure to Pb in the environment (for example, due to closer proximity to historic Pb sources such as smelters and roadways) are well documented (43). Because children on well water are less likely to be Black, they are therefore also less likely to be exposed to Pb from sources other than water. They also are less likely to experience the negative effects of racial bias in economic and social disadvantages that increase the risk of an official report for delinquency. By relying on a dataset that matches children on well water with demographically and socioeconomically similar children on community water, Model 2 may provide better control for other factors that influence Pb exposure and the risk of being reported for delinquency. Both models suggest that early life Pb exposure from private well water is damaging regardless of a child’s race or socioeconomic status.
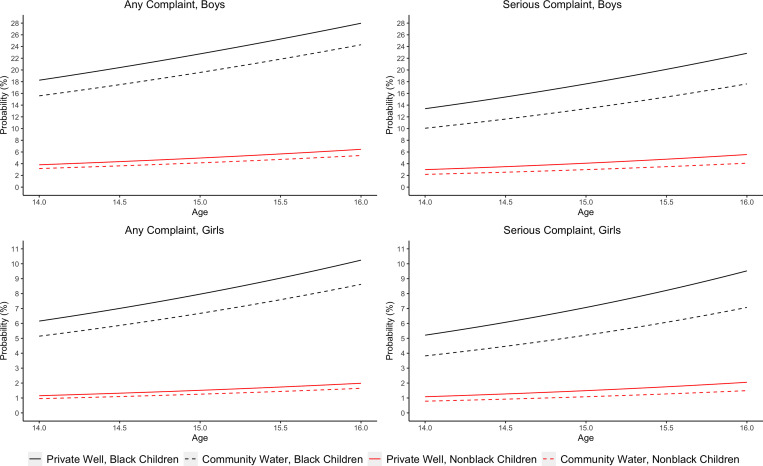
Fig. 3 shows the predicted probability of delinquency by age, race, and gender for the population reflected in the quasi-experimental dataset. The results suggest that for a “median” White male child whose home relied on an unregulated private well during early childhood, the probability of being reported for delinquency by age 16 could have been decreased from 6.5 to 5.4% had the child’s home been served by a community water supply (assuming median values for all variables other than race and gender). For a Black male child, an early life change from private well water to a community system could have decreased the probability of teenage delinquency from 28.0 to 24.3%. Benefits of Pb exposure prevention also would accrue for females, though the effect is less pronounced because of the much-lower reported juvenile delinquency rates among girls compared to boys.
Fig. 3.
Probability that a child will be reported to the juvenile justice system by age, water source, and race for a population representative of the children in this sample relying on private well water. Solid lines represent the status quo. Dashed lines represent the potential change in delinquency risk if the children were supplied with treated water from a community supply, in place of their private well water. Black lines represent Black children, and red lines show children of all other races. These predictions were generated using Eqs. 1 through 3. Age at the time of blood test was set at 15 to 19 mo, construction year of house was fixed to 1988 to 1997, and all other independent variables were held constant at median values for the population of children on private wells.
Discussion
This research assessed whether children relying on unregulated domestic wells for their drinking water in early life are at increased risk of being reported for juvenile delinquency as teens due to their increased exposure to Pb. Children on unregulated domestic wells (about 13% of all children in the United States) have higher risks of Pb exposure from drinking water than those served by community water systems, because domestic wells are not regulated under the Safe Drinking Water Act and are therefore rarely tested for Pb or treated to prevent Pb dissolution from household plumbing and fixtures (13, 44). Awareness of these risks among households relying on private wells is very low due to the lack of routine water testing and also misperceptions about well water being clean because it is “natural” (15, 45, 46). Our analysis of a quasi-experimental dataset matching children on well water to similar children with community water found that reliance on well water in early life was associated with a 21% increase in the odds of being reported for any act of delinquency and 38% higher odds of serious delinquency. Our results also suggest that early life Pb exposure from any source elevates the risk of being reported for teenage juvenile delinquency. An increase in early life blood Pb from 1 to 3 µg/dL (representing a change from the first to the third quartile) was associated with a nearly an eightfold increase in the odds of being reported for delinquent behavior. Overall, our results highlight that the consequences of failing to prevent Pb exposure from private well water—an underrecognized Pb exposure source in the United States—may be serious. They also indicate that the Pb continues to harm to children, despite the tremendous progress made in preventing exposure from gasoline, paint, food cans, and community water supplies over the past four decades. Even the relatively low blood Pb levels in the cohort in this study (mean = 1.97 µg/dL; maximum = 44 µg/dL) were associated with increased risks of reported juvenile delinquency.
Comparison to Prior Research.
The results of our stage 1 model linking blood Pb to children’s water source are consistent with prior research. For example, a prior study of a cohort of 59,483 Wake County, NC, children found that children on well water had blood Pb that was, on average, 20% higher than that of children on community water systems (8); that cohort included younger children than the children in this study (with birth years as late as 2017 compared to 2005 as the latest birth date for children born in this study). The higher effect size in that study may reflect the fact that as other environmental Pb sources have been increasingly controlled, the importance of water as a source of Pb exposure has increased (47). More recently, a study including 398,584 children screened for blood Pb between 2011 and 2018 found that those on well water had 13% higher blood Pb than children with community water service (48). Other studies have linked measured Pb concentrations in drinking water from community systems to children’s blood Pb (47, 49).
Findings in this study concerning factors other than Pb exposure that influence delinquency risk also are consistent with prior research. For example, Black children in the full dataset had 2.78 higher odds of being reported for delinquency compared to White children with similar socioeconomic status living in similar neighborhoods. This result is consistent with the many previous studies that have documented persistent racial inequities in the risk of being reported for delinquency (50). Between 2005 and 2015, Black youth were between 2.7 and 3.1 times more likely to be referred to juvenile court than White youth, according to national data (50). These disparities may reflect a variety of factors including increased social disadvantages that place Black youth at greater risk of delinquency and biases in arrests, referrals to juvenile court, and adjudications (28, 51) in addition to disproportionate exposure to neurotoxic environmental contaminants (29)
Results of this study also are consistent with prior research on early life Pb exposure and juvenile delinquency published over the past 20 y. Dietrich et al. found that among 195 Cincinnati, Ohio, teens aged 15 to 17, subjects with prenatal blood Pb above 20 µg/dL committed 2.3 times more delinquent acts than those with prenatal Pb below 10 µg/dL (29). Needleman et al. found that youth aged 12 to 18 arrested and adjudicated for juvenile delinquency in Allegheny County, Pennsylvania, were four times as likely to have bone Pb above 25 ppm compared to controls (52). Fergusson, Boden, and Horwood showed that Christchurch, New Zealand, teens who had tooth Pb above 12 µg/g at ages 6 to 8 reported nearly eight times as many delinquent acts as those with dentin Pb below 2 µg/g (53). Using historic US state-level leaded gasoline consumption data to predict children’s blood Pb, Reyes found that the risk of arrest by age 17 increased by 37% for every unit increase in predicted blood Pb at the study population mean blood Pb of 7.5 μg/dL (25). Barrett found that the juvenile arrest rate in 77 Chicago neighborhoods in 2009 increased by about 5% for every unit increase in the percentage of children ages 0 to 6 y with elevated blood Pb (defined as above 10 µg/dL) a decade earlier (54). Aizer and Currie linked preschool blood Pb for Rhode Island children born between 1990 and 2004 to later-life crime records, finding that the risk of detention or incarceration by age 23 increased 15% for each 1-µg/dL increment in preschool blood Pb (21).
We identified no previous studies of the influence of Pb in US private well water (or in US drinking water in general) on juvenile delinquency. There are multiple possible explanations for the lack of prior research. A major challenge is the lack of information on drinking water sources at the residential scale. After 1990, the US Census eliminated questions about access to community water service, and no subsequent system has been developed to collect this information in its place (13, 55). Wake County, NC, is one of few places nationwide where such data are readily available, since they are included with property tax records. In addition, tracking children’s sources of drinking water over time is challenging when children move. We were able to address this limitation by linking water source data to school records.
Limitations.
A limitation of this study is the lack of co-occurring measurements of Pb concentrations in drinking water and children’s blood. Our two-stage model uses private well water as an instrument for Pb exposure, but we were unable to confirm the relationship between Pb in drinking water and Pb in blood because household water samples for the children in the cohort were not collected simultaneously with blood Pb measurements. Nonetheless, the association between blood Pb and reliance on private well water in this cohort is highly significant (P < 0.001), and the results are consistent with multiple prior studies showing high risks for elevated Pb in private well water (9, 56–58) and associations between Pb in drinking water and Pb in children’s blood (e.g., during the Flint water crisis) (59).
A related limitation is that it is possible that metals other than Pb may contribute to the observed associations between water source and reported juvenile delinquency. For example, recent studies suggest that concentrations of the essential nutrient manganese that are either too high or too low may harm children’s intellectual development (60). Manganese occurs commonly in private well water due to its presence in aquifer media (indeed, it is the fifth-most commonly occurring metallic trace element) (61). However, prior studies of manganese in private well water in the study area have found that concentrations tend to be low relative to levels associated with health concern (9).
A third limitation is that the two-stage, least-squares regression approach requires that reliance on wells can only affect delinquency through its effects on blood Pb. It is possible that wells are a proxy for a kind of neighborhood that may be associated with delinquency risk. Nonetheless, we believe that we have controlled for this possibility by including race and measures of income as covariates. Furthermore, given that communities where houses rely on private wells have higher median incomes than areas with community water service, it is highly unlikely that wells are located in areas with above-average crime rates.
An additional limitation relates to the main outcome measures. The study relies on official reports of juvenile delinquency rather than actual delinquent behavior. Juvenile delinquency reports are only a signal of potential behavioral problems and do not capture the true prevalence rate of illegal teen behavior. Although studies have consistently found correlations between reported acts of delinquency and delinquent behavior as reported by teens or their parents (62–64), given the well-documented racial inequities in the juvenile justice system, these reports undoubtedly are biased. Nonetheless, controlling for race and socioeconomic status, as we have done, helps address this limitation. Our results suggest that exposure to Pb from private well water contributes to delinquent teen behavior, regardless of race.
Conclusion
This study reveals an achievable opportunity to improve outcomes for vulnerable children by preventing early life exposure to Pb in drinking water in the 13% of US homes relying on unregulated private wells. Possible interventions to prevent these exposures include building new community water systems for or extending existing systems to unserved neighborhoods and/or strengthening programs to promote private well stewardship. Interim measures also could include deploying household water-treatment systems . The former solution (construction of new systems or extension of existing ones) is suitable only for areas with sufficient population density due to the need for economies of scale. In our dataset, 20.5% of the children relying on private wells lived in municipal extraterritorial jurisdictions during early childhood. These are areas that border cities or towns but are not incorporated into them. These neighborhoods are good candidates for community water service extensions due to their close proximity to existing infrastructure. Our research has shown that Black neighborhoods in North Carolina extraterritorial jurisdictions are less likely than White neighborhoods to get access to community water service, indicating a racial component to exclusion from existing infrastructure in these areas (30, 34). Others have found similar exclusionary practices in access to town water infrastructure in other parts of the country (65–69).
Private well households more distant from existing infrastructure and where population density is too low to make new infrastructure cost-effective could be provided with household water filters, perhaps at subsidized rates depending on income. A recent study found that a low-cost ($100), under-sink water filter available at typical US hardware stores can consistently remove 98% of influent Pb over the filter’s lifetime even under highly variable private well-water quality and water-use conditions (70). Filter manufacturers recommend replacing cartridges every 6 mo (at a cost of $70). Even when considering these replacement costs, the expense of purchasing and maintaining a filter over the first 6 y of a child’s life, when they are most vulnerable to Pb, is very low ($279 total present value at a 3% discount rate).
A previous study estimated that “saving” one youth at risk for becoming entrenched in the adult criminal justice system yields social benefits of $1.3 to 1.5 million in 1997 dollars, equivalent to $2.2 to 2.5 million today (71). Long-term costs of high-risk youth quantified in the study include victim costs of crime, criminal justice costs, and foregone earnings. Considering these costs, our results suggest that at a population scale, Pb exposure-prevention programs for households with private wells could improve outcomes for vulnerable children while yielding sizeable benefits to communities. Technology to solve this problem is readily available. Putting it in place is a matter of political will and should be part of upgrading infrastructure in the United States.
Supplementary Material
Acknowledgments
We are grateful to the NC Childhood Lead Poisoning Prevention Program for providing access to the children’s blood Pb data central to this research. In particular, we thank Program Manager Ed Norman, Data Manager Tena Hand, and Public Health Epidemiologist Melanie Napier. We are also extremely grateful to the NC DPS for data on juvenile justice reports for the children in this sample, especially to Megan Howell and Phillip Maychek. Thanks are also due to Clara Muschkin and Kara Bonneau at NCERDC for information on residential addresses of the children at age 14. This research was funded by the US Environmental Protection Agency Science to Achieve Results Program under Grant no. 83927901.
Footnotes
The authors declare no competing interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2110694119/-/DCSupplemental.
Data Availability
Anonymized de-identified children's blood Pb, water source, household information, census block group information, and juvenile justice report data have been deposited in https://scholarworks.iu.edu/dspace/handle/2022/27027 (72, 73). https://scholarworks.iu.edu/dspace/handle/2022/25638.
References
- 1.Centers for Disease Control and Prevention (CDC), Ten great public health achievements--United States, 2001-2010. MMWR Morb. Mortal. Wkly. Rep. 60, 619–623 (2011). [PubMed] [Google Scholar]
- 2.Dignam T., Kaufmann R. B., LeStourgeon L., Brown M. J., Control of Lead Sources in the United States, 1970-2017: Public Health Progress and Current Challenges to Eliminating Lead Exposure. J. Public Health Manag. Pract. 25 (Suppl 1, Lead Poisoning Prevention), S13–S22 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grosse S. D., Matte T. D., Schwartz J., Jackson R. J., Economic gains resulting from the reduction in children’s exposure to lead in the United States. Environ. Health Perspect. 110, 563–569 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.U.S. Centers for Disease Control and Prevention, Blood Lead Levels (μg/dL) among U.S. Children under 72 Months of Age, by State, Year, and Blood Lead Level (BLL) Group (Atlanta, GA, 2021). https://www.cdc.gov/nceh/lead/docs/cbls-national-data-table-508.pdf. Accessed 11 January 2022. [Google Scholar]
- 5.Mazumdar M., et al. , Low-level environmental lead exposure in childhood and adult intellectual function: A follow-up study. Environ. Health 10, 24 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Canfield R. L., et al. , Intellectual impairment in children with blood lead concentrations below 10 microg per deciliter. N. Engl. J. Med. 348, 1517–1526 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shefa S. T., Héroux P., Both physiology and epidemiology support zero tolerable blood lead levels. Toxicol. Lett. 280, 232–237 (2017). [DOI] [PubMed] [Google Scholar]
- 8.Gibson J. M., Fisher M., Clonch A., MacDonald J. M., Cook P. J., Children drinking private well water have higher blood lead than those with city water. Proc. Natl. Acad. Sci. U.S.A. 117, 16898–16907 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stillo F. J., MacDonald Gibson J., Racial disparities in access to municipal water supplies in the American South: Impacts on children’s health. Int. Public Health J. 10, 309–323 (2018). [Google Scholar]
- 10.Dieter C., Maupin M., Public Supply and Domestic Water Use in the United States, 2015 (U.S. Geological Survey, Reston, VA, 2017). [Google Scholar]
- 11.U.S. Congress, Safe Drinking Water Act, 42 U.S.C. §§300f-300j-26 (United States).
- 12.U.S. Environmental Protection Agency, Lead and Copper: Final Rule, 40 CFR Part 141 Subpart I (1991).
- 13.Fox M. A., Nachman K. E., Anderson B., Lam J., Resnick B., Meeting the public health challenge of protecting private wells: Proceedings and recommendations from an expert panel workshop. Sci. Total Environ. 554-555, 113–118 (2016). [DOI] [PubMed] [Google Scholar]
- 14.Stillo F. J., Bruine de Bruin W., Zimmer C., Gibson J. M., Well water testing in African-American communities without municipal infrastructure: Beliefs driving decisions. Sci. Total Environ. 686, 1220–1228 (2019). [DOI] [PubMed] [Google Scholar]
- 15.Fizer C., De Bruin W. B., Stillo F., Gibson J. M., Barriers to managing private wells and septic systems in underserved communities: Mental models of homeowner decision making. J. Environ. Health 81, 8–15 (2018). [Google Scholar]
- 16.Lockhart S., Wood E., MacDonald Gibson J., Impacts of exclusion from municipal water service on water availability: A case study. New Solut. 30, 127–137 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Needleman H. L., McFarland C., Ness R. B., Fienberg S. E., Tobin M. J., Bone lead levels in adjudicated delinquents. A case control study. Neurotoxicol. Teratol. 24, 711–717 (2002). [DOI] [PubMed] [Google Scholar]
- 18.Sampson R. J., Winter A. S., Poisoned development: Assessing childhood lead exposure as a cause of crime in a birth cohort followed through adolescence. Criminology 56, 269–301 (2018). [Google Scholar]
- 19.Morris R. D., Audet A. M., Angelillo I. F., Chalmers T. C., Mosteller F., Chlorination, chlorination by-products, and cancer: A meta-analysis. Am. J. Public Health 82, 955–963 (1992). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amato M. S., et al. , Early lead exposure (<3 years old) prospectively predicts fourth grade school suspension in Milwaukee, Wisconsin (USA). Environ. Res. 126, 60–65 (2013). [DOI] [PubMed] [Google Scholar]
- 21.Aizer A., Currie J., Lead and juvenile delinquency: New evidence from linked birth, school, and juvenile detention records. Rev. Econ. Stat. 101, 575–587 (2019). [Google Scholar]
- 22.Mielke H. W., Zahran S., The urban rise and fall of air lead (Pb) and the latent surge and retreat of societal violence. Environ. Int. 43, 48–55 (2012). [DOI] [PubMed] [Google Scholar]
- 23.Boutwell B. B., et al. , The intersection of aggregate-level lead exposure and crime. Environ. Res. 148, 79–85 (2016). [DOI] [PubMed] [Google Scholar]
- 24.Nigra A. E., Environmental racism and the need for private well protections. Proc. Natl. Acad. Sci. U.S.A. 117, 17476–17478 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reyes J. W., Lead exposure and behavior: Effects on antisocial and risky behavior among children and adolescents. Econ. Inq. 53, 1580–1605 (2015). [Google Scholar]
- 26.Angrist J. D., Pischke J.-S., Mostly Harmless Econometrics: An Empiricist’s Companion (Princeton University Press, Princeton, NJ, 2009). [Google Scholar]
- 27.Yeter D., Banks E. C., Aschner M., Disparity in risk factor severity for early childhood blood lead among predominantly African-American black children: The 1999 to 2010 US NHANES. Int. J. Environ. Res. Public Health 17, 1–26 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sampson R. J., Lauritsen J. L., Racial and Ethnic Disparities in Crime and Criminal Justice in the United States. Crime and Justice 21, 311–374 (1997).
- 29.Dietrich K. N., Ris M. D., Succop P. A., Berger O. G., Bornschein R. L., Early exposure to lead and juvenile delinquency. Neurotoxicol. Teratol. 23, 511–518 (2001). [DOI] [PubMed] [Google Scholar]
- 30.Leker H. G., MacDonald Gibson J., Relationship between race and community water and sewer service in North Carolina, USA. PLoS One 13, e0193225 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.North Carolina Division of Public Health, EHS: CEHU: Childhood Lead Poisoning Prevention Program Data (2018). https://ehs.ncpublichealth.com/hhccehb/cehu/lead/data.htm. Accessed 3 July 2018.
- 32.Dieter C. A., et al. , Estimated use of water in the United States in 2015 (2018). https://pubs.er.usgs.gov/publication/cir1441. Accessed 11 January 2022.
- 33.NHGIS Data Finder. https://data2.nhgis.org/. Accessed 13 November 2021.
- 34.MacDonald Gibson J., DeFelice N., Sebastian D., Leker H., Racial disparities in access to community water supply service in Wake County, North Carolina. Front. Public Heal. Serv. Syst. Res. 3, Article 6 (2014). [Google Scholar]
- 35.Goldberg S., Reigning in Sprawleigh. Time (2011). http://content.time.com/time/specials/packages/article/0,28804,2026474_2026675_2061559,00.html. Accessed 11 January 2022. [Google Scholar]
- 36.Aiken C. C. S. , Race as a factor in municipal underbounding. Ann. Assoc. Am. Geogr. 77, 37–41 (1987). [Google Scholar]
- 37.Public Schools First NC, The Facts Public vs. Private Schools (Raleigh, NC, 2016). [Google Scholar]
- 38.Angrist J. D., Imbens G. W., Two-stage least squares estimation of average causal effects in models with variable treatment intensity. J. Am. Stat. Assoc. 90, 431–442 (1995). [Google Scholar]
- 39.Lousdal M. L., An introduction to instrumental variable assumptions, validation and estimation. Emerg. Themes Epidemiol. 15, 1–7 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hanck C., Arnold M., Gerber A., Schmelzer M., Introduction to Econometrics with R (University of Duisburg-Essen, Essen, Germany, 2018). [Google Scholar]
- 41.Needleman H. L., Landrigan P. J., The health effects of low level exposure to lead. Annu. Rev. Public Health 2, 277–298 (1981). [DOI] [PubMed] [Google Scholar]
- 42.Henning K., The challenge of race and crime in a free society: The racial divide in fifty years of juvenile justice reform. George Washington Law Rev. 86, 1604–1666 (2018). [Google Scholar]
- 43.Cassidy-Bushrow A. E., et al. , Burden of higher lead exposure in African-Americans starts in utero and persists into childhood. Environ. Int. 108, 221–227 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zheng Y., Flanagan S. V., The case for universal screening of private well water quality in the U.S. and testing requirements to achieve it: Evidence from arsenic. Environ. Health Perspect. 125, 085002 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kreutzwiser R., et al. , Understanding stewardship behaviour: Factors facilitating and constraining private water well stewardship. J. Environ. Manage. 92, 1104–1114 (2011). [DOI] [PubMed] [Google Scholar]
- 46.Colley S. K., Kane P. K. M., MacDonald Gibson J., Risk communication and factors influencing private well testing behavior: A systematic scoping review. Int. J. Environ. Res. Public Health 16, E4333 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Triantafyllidou S., Edwards M., Lead (Pb) in tap water and in blood: Implications for lead exposure in the United States. Crit. Rev. Environ. Sci. Technol. 42, 1297–1352 (2012). [Google Scholar]
- 48.Kamai E. M., “Lead and children in North Carolina: Patterns of lead testing across the state and a case study of point sources in Forsyth County, North Carolina,” Dissertation, University of North Carolina, Chapel Hill, NC (2021).
- 49.Ngueta G., Abdous B., Tardif R., St-Laurent J., Levallois P., Use of a cumulative exposure index to estimate the impact of tap water lead concentration on blood lead levels in 1- to 5-year-old children (Montréal, Canada). Environ. Health Perspect. 124, 388–395 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Leiber M. J., Fix R., Reflections on the impact of race and ethnicity on juvenile court outcomes and efforts to enact change. Am. J. Crim. Justice 44, 581–608 (2019). [Google Scholar]
- 51.Evangelist M., Ryan J. P., Victor B. G., Moore A., Perron B. E., Disparities at adjudication in the juvenile justice system: An examination of race, gender, and age. Social Work Research 41, 199–211 (2017). 10.1093/swr/svx017. [DOI] [Google Scholar]
- 52.Needleman H. L., McFarland C. E., Ness R., Bone lead levels in adjudicated delinquency: A case-control study. Neurotoxicol. Teratol. 24, 11–17 (2002). [DOI] [PubMed] [Google Scholar]
- 53.Fergusson D. M., Boden J. M., Horwood L. J., Dentine lead levels in childhood and criminal behaviour in late adolescence and early adulthood. J. Epidemiol. Community Health 62, 1045–1050 (2008). [DOI] [PubMed] [Google Scholar]
- 54.Barrett K. L., Exploring community levels of lead (Pb) and youth violence. Sociol. Spectr. 37, 205–222 (2017). [Google Scholar]
- 55.MacDonald Gibson J., Pieper K. J., Strategies to improve private well water quality: A North Carolina perspective. Environ. Health Perspect. 125, 076001 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pieper K. J., Krometis L. A. H., Gallagher D. L., Benham B. L., Edwards M., Incidence of waterborne lead in private drinking water systems in Virginia. J. Water Health 13, 897–908 (2015). [DOI] [PubMed] [Google Scholar]
- 57.Pieper K. J., Krometis L. A., Gallagher D., Benham B., Edwards M., Profiling private water systems to identify patterns of waterborne lead exposure. Environ. Sci. Technol. 49, 12697–12704 (2015). [DOI] [PubMed] [Google Scholar]
- 58.Pieper K. J., et al. , Elevated lead in water of private wells poses health risks: Case study in Macon county, North Carolina. Environ. Sci. Technol. 52, 4350–4357 (2018). [DOI] [PubMed] [Google Scholar]
- 59.Hanna-Attisha M., LaChance J., Sadler R. C., Champney Schnepp A., Elevated blood lead levels in children associated with the Flint drinking water crisis: A spatial analysis of risk and public health response. Am. J. Public Health 106, 283–290 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vollet K., Haynes E. N., Dietrich K. N., Manganese exposure and cognition across the lifespan: Contemporary review and argument for biphasic dose-response health effects. Curr. Environ. Health Rep. 3, 392–404 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rodríguez-Barranco M., et al. , Association of arsenic, cadmium and manganese exposure with neurodevelopment and behavioural disorders in children: A systematic review and meta-analysis. Sci. Total Environ. 454-455, 562–577 (2013). [DOI] [PubMed] [Google Scholar]
- 62.Curry G. D., Self-reported gang involvement and officially recorded delinquency. Criminology 38, 1253–1274 (2000). [Google Scholar]
- 63.Kirk D. S., Examining the divergence across self-report and official data sources on inferences about the adolescent life-course of crime. J. Quant. Criminol. 22, 107–129 (2006). [Google Scholar]
- 64.Piquero A. R., Schubert C. A., Brame R., Comparing official and self-report records of offending across gender and race/ethnicity in a longitudinal study of serious youthful offenders. J. Res. Crime Delinq. 51, 526–556 (2014). [Google Scholar]
- 65.VanDerslice J., Drinking water infrastructure and environmental disparities: Evidence and methodological considerations. Am. J. Public Health 101 (suppl. 1), S109–S114 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Anderson M. W., Cities inside out: Race, poverty, and exclusion at the urban fringe. UCLA Law Rev. 55, 1095–1160 (2008). [Google Scholar]
- 67.Durst N. J., Municipal annexation and the selective underbounding of colonias in Texas’ Lower Rio Grande Valley. Environ. Plann. A 46, 1699–1715 (2014). [Google Scholar]
- 68.Pannu C., Drinking water and exclusion: A case study from California’ s central valley. Califorina Law Rev 100, 223–268 (2012). [Google Scholar]
- 69.Ranganathan M., Balazs C., Water marginalization at the urban fringe: Environmental justice and urban political ecology across the North–South divide. Urban Geogr. 36, 403–423 (2015). [Google Scholar]
- 70.Mulhern R., MacDonald Gibson J., Under-sink activated carbon water filters effectively remove lead from private well water for over six months. Water 12, 3584 (2020). [Google Scholar]
- 71.Cohen M. A., The monetary value of saving a high-risk youth. J. Quant. Criminol. 14, 5–33 (1998). [Google Scholar]
- 72.Gibson J. M. et al., Early-Life Lead Exposure from Private Well Water Increases Juvenile Delinquency Risk Among U.S. Teens. IUScholarWorks. 10.5967/D0E0-FC38. Deposited 20 December 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Duke University Center for Child and Family Policy, North Carolina Education Research Data Center. https://childandfamilypolicy.duke.edu/north-carolina-education-research-data/. Accessed 7 January 2022. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Anonymized de-identified children's blood Pb, water source, household information, census block group information, and juvenile justice report data have been deposited in https://scholarworks.iu.edu/dspace/handle/2022/27027 (72, 73). https://scholarworks.iu.edu/dspace/handle/2022/25638.