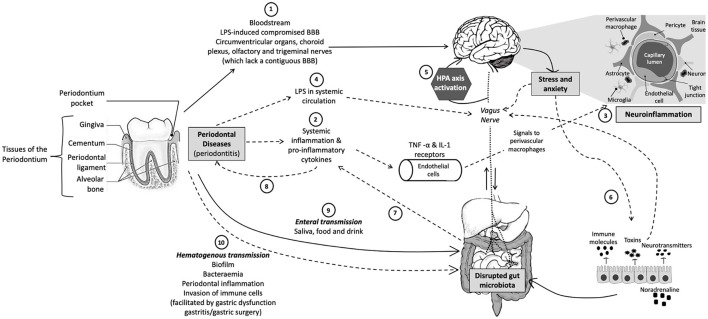
Figure 1.
Schematic representation of the oral-gut-brain axis. (1) Periodontal bacteria can directly reach the brain via the bloodstream or areas that lack an intact BBB or with a compromised BBB. (2) Periodontitis can indirectly affect the CNS via pro-inflammatory cytokines that activate endothelial cells that express TNF-α and IL-1 receptors, which, in turn, signal to the perivascular macrophages that communicate and activate microglia, resulting in (3) neuroinflammation. (4) Periodontitis can also result in leaky periodontium and LPS in systemic circulation, which can (5) activate the HPA axis and result in increased stress hormones or neurotransmitters, which subsequently (6) influence gut physiology, microbiota habitat, microbiota community composition, and bacterial gene expression. (7) An altered gut microbiota can result in systemic inflammation, which not only affects the CNS but also (8) exacerbates other inflammatory pathologies, such as periodontitis. Periodontal bacteria can directly influence gut microbial community composition and functioning via (9) enteral transmission or indirectly via (10) hematogenous transmission (which is facilitated by conditions such as gastritis, gastric surgery, or gastric dysfunction). CNS, central nervous system; TNF, tumor necrosis factor; IL-1, interleukin-1; LPS, lipopolysaccharide; BBB, blood–brain barrier; HPA, hypothalamic–pituitary–adrenal. Solid arrows indicate direct pathways and dotted arrows indicate indirect pathways.