Abstract
Background:
The aim of this study was to characterize the risk of glove perforation among surgical team members performing a typical set of trauma procedures, as well as to identify the rate at which these people recognize potential perforations.
Methods:
Gloves used in orthopedic trauma room procedures were collected from all participating team members over 2 weeks and were subsequently examined for perforations. Perforation rates based on glove position, type, wearer and procedure were assessed.
Results:
Perforations were found in 5.9% of gloves; 4.3% of the perforations were found in outer gloves and 1.6% in inner gloves. Among the outer gloves, 30.7% of the perforations were recognized by the wearer at the time of perforation; none of the inner glove perforations were recognized, even when they were associated with an accompanying outer glove perforation. Significantly more perforations were identified in the gloves of attending staff than in those of other team members. Attending staff experienced more perforations than other wearers, regardless of whether they were acting as the primary surgeon or as an assistant. Perforations were more common in open reduction internal fixation and amputation procedures. For open reduction internal fixation procedures, longer operative times were associated with more frequent glove perforations.
Conclusion:
The rates of glove perforation are high in orthopedic trauma surgeries, and often these perforations are not recognized by the wearer. Attending staff are at an elevated risk of glove perforation. It is recommended that all members of the surgical team change both pairs of gloves whenever an outer glove perforation is observed.
Abstract
Contexte:
Le but de cette étude était de caractériser le risque de perforation des gants chez le personnel du bloc opératoire chargé d’effectuer un ensemble typique d’interventions dans un contexte de traumatologie, et de mesurer à quel point il sait reconnaître les perforations potentielles.
Méthodes:
Les gants utilisés pour les interventions au bloc opératoire de traumatologie/orthopédie ont été recueillis auprès de tous les membres de l’équipe participants pendant 2 semaines et ont ensuite été examinés pour y déceler des perforations. Les taux de perforation ont été mesurés selon la position, le type, la personne qui portait les gants et l’intervention effectuée.
Résultats:
Nous avons trouvé des perforations dans 5,9 % des gants; 4,3 % des perforations se trouvaient sur les gants extérieurs et 1,6 % sur les gants intérieurs. Pour les gants extérieurs, 30,7 % des perforations ont été reconnus par la personne qui les portait au moment où elles ont eu lieu; aucune des perforations des gants intérieurs n’a été reconnue, même lorsqu’elles étaient associées à une perforation de la couche supérieure. Un nombre significativement plus élevé de perforations ont été identifiées dans les gants des médecins traitants que dans ceux des autres membres de l’équipe. Les médecins traitants ont eu plus de perforations que les autres personnes qui portaient des gants, indépendamment de leur rôle en tant que chirurgien principal ou qu’assistant. Les perforations ont été plus fréquentes lors d’interventions pour des réductions ouvertes et des fixations internes et d’amputations. Dans les cas de réductions ouvertes et de fixations internes, la durée plus longue de l’intervention a été associée à des perforations de gant plus fréquentes.
Conclusion:
Les taux de perforation des gants sont élevés lors de chirurgies orthopédiques traumatologiques, et souvent, ces perforations surviennent à l’insu de la personne qui porte les gants. Les médecins traitants sont exposés à un risque élevé de perforation des gants. Il est recommandé que tous les membres de l’équipe chirurgicale change les 2 couches de gants dès qu’une perforation affecte le gant extérieur.
Glove perforations are common in orthopedic procedures,1,2 especially in trauma surgeries,3,4 and they can pose health risks to both patients and surgical personnel. Several studies have identified glove perforation and resultant contamination as an independent risk factor for surgical site infection.4–6 Additionally, operating room personnel are often not aware that their protective equipment has been compromised, increasing the risk of disease transmission.5
Studies investigating glove perforation in orthopedic surgical procedures have analyzed differences in glove consistency,7,8 techniques such as double gloving9–11 and modifying the duration of wear,12 and the risk of perforation during high-risk manoeuvres or procedures.3,4,13 Although literature exists to suggest that glove perforation is common in orthopedic procedures, to our knowledge no studies have been done to characterize the relative risk for all operating room team members, including attending staff, surgical assistants and scrub nurses. Of particular interest to the study team was the possibility of unrecognized glove perforations among scrub nurses, as these people frequently perform many activities that have previously been identified as high risk, such as cleaning drill bits.4
The primary aim of this study was to examine a cross-section of typical orthopedic trauma room cases to characterize the risk of glove perforation among all participating members of the surgical team. The secondary aim was to describe the frequency with which operating room staff recognize potential perforations.
Methods
Over a period of 2 weeks, surgical gloves were collected during daytime orthopedic trauma procedures that were performed in the trauma operating room (OR) at a regional level 1 trauma centre and tertiary academic hospital. Given the variable volumes of trauma cases, 1 infected knee arthroplasty revision case and 1 spinal trauma case were performed in the trauma OR during the study period and included in the analysis.
All gloves used were collected, bagged and numbered as a pair, with the following variables recorded: procedure, operative time, role (primary surgeon, surgical assistant, scrub nurse), training level (attending staff, fellow, resident, clinical clerk, scrub nurse), glove position (inner, outer, single), glove type (orthopedic, regular latex, orthopedic latex-free, regular latex-free), reason for change (suspected perforation, contamination), routine (e.g., before cementing, after back table setup) and mechanism of suspected or confirmed perforation, if applicable.
Before the commencement of data collection, all participating OR personnel were provided with an information letter indicating that their surgical gloves could be collected and their role in the surgery documented anonymously. Participation in this study was voluntary. Patient consent was not obtained, as identifying patient information was not collected and there was no change to the standard of care provided. Ethics approval was obtained from the Queen’s University Health Sciences and Affiliated Teaching Hospitals Research Ethics Board (HSREB 6027221).
Perforation testing
Perforation was characterized by a visual inspection, followed by a microperforation and macroperforation test as described previously by the United States Food and Drug Administration.14 To identify macroperforations, each glove was filled with approximately 1000 mL of water (or enough to fill the glove before overflow), the glove opening was twisted to create a seal, then the glove was inspected for leaks. If no macroperforation was identified, the palm of the glove, followed by each individual finger, was manually squeezed. Any beading of water on the glove would indicate a microperforation. For individuals who wore a single pair of gloves, any perforations were counted as inner glove perforations. On analysis, all perforations were grouped together.
Statistical analysis
A χ2 analysis was used to investigate the rate of perforation depending on the role of the glove wearer, type of glove and type of surgical procedure. Additionally, the percentage of total glove perforations and the overall risk of perforation were quantified, along with the proportion of perforations recognized by the wearer at the time of perforation. We used independent-samples t tests to compare the mean operative times in procedures with and without perforations. Analyses were done using SPSS version 26.0 for Windows (SPSS Inc.).
Results
Glove perforations
A total of 304 individual gloves were collected (152 pairs). Among the gloves collected, perforations were identified in 18 gloves, 5 of which were inner glove perforations, yielding an overall 5.9% risk of any glove perforation and a 1.6% risk of an inner glove perforation (Table 1). Of the 13 instances in which there was an outer glove perforation, there were 5 associated inner glove perforations, indicating a 38% chance of an associated inner glove perforation in the presence of an outer glove perforation.
Table 1.
Gloves with identifiable perforations
| Item | No. of gloves collected | No. (%) of gloves with identifiable perforations |
|---|---|---|
| Outer gloves | 182 | 13 (4.3) |
| Inner gloves | 122 | 5 (1.6) |
| Total | 304 | 18 (5.9) |
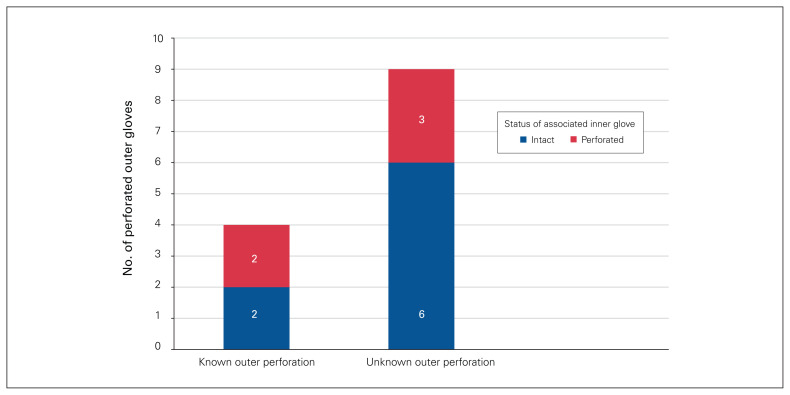
Of the 13 outer glove perforations, only 4 were identified by the glove wearer at the time of perforation (30.7%). Of these 4, 2 (50.0%) were associated with unknown inner glove perforations. Of the 9 unknown outer glove perforations, 3 (33.3%) were associated with unknown inner glove perforations (Figure 1). None of the 5 inner glove perforations were identified at the time of the procedure, even when they were associated with a known outer glove perforation.
Fig. 1.
The association between outer and inner glove perforations.
Role of the glove wearer
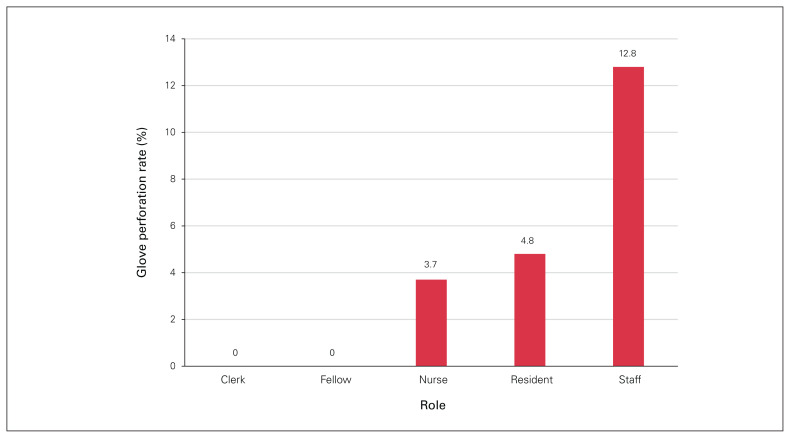
Significantly more glove perforations occurred among attending staff than among team members in other roles (p = 0.02) (Figure 2). Of the 86 gloves obtained from attending staff, 11 (12.8%, 95% confidence interval [CI] 6% to 20%) had perforations, which amounted to 61.1% of all identified perforations. Residents (5 gloves, 4.8%, 95% CI 1% to 9%) and scrub nurses (2 gloves, 3.7%, 95% CI 0% to 9%) experienced similar rates of perforation, which were significantly lower than the rate of perforation identified in the gloves obtained from attending staff. None of the gloves obtained from fellows or clinical clerks had identifiable perforations.
Fig. 2.
Glove perforations by surgical team member role.
Given that this study was conducted at a teaching hospital, in 43% of the procedures in our study a surgical resident was acting as the primary surgeon and the attending staff was acting as a surgical assistant. To determine whether the increased frequency of perforations observed in gloves worn by attending staff was due to their level of training or due to an increase in hands-on manoeuvres performed by this group, the gloves were subclassified on the basis of whether the wearer was the primary surgeon or an assisting surgeon. There was no difference in the perforation rates of the gloves worn by the primary surgeon compared with the perforation rates of the gloves worn by team members in the other roles, regardless of level of training (p = 0.21). When clerks, fellows and scrub nurses were removed from the analysis and attending staff were compared directly with residents, again there was no significant difference in the perforation rates of the gloves worn by the primary surgeon and the assisting surgeon (p = 0.89). This would indicate that attending surgeons have higher rates of glove perforations regardless of whether they are the primary or assisting surgeon.
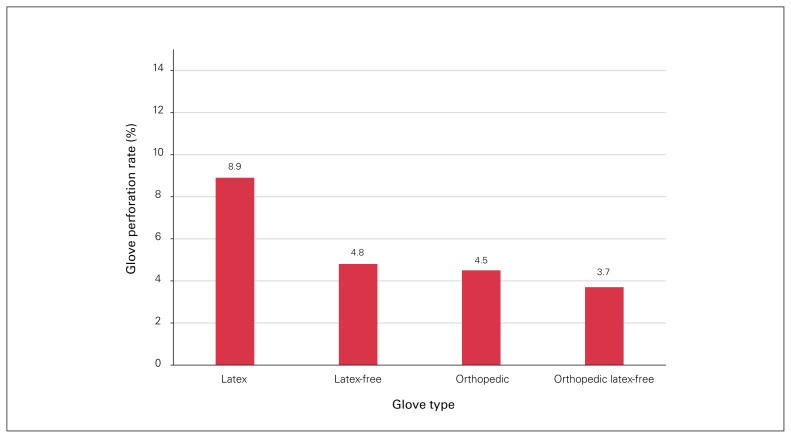
Type of glove
Among the 4 different glove types worn by surgical personnel (latex, latex-free, orthopedic, orthopedic latex-free), the highest proportion of perforations was observed in latex gloves (10 out of 112, 8.9%, 95% CI 4% to 15%); however, a χ2 analysis revealed no statistical difference in the perforation rate (p = 0.39) (Figure 3). Perforation rates were similar among all of the other glove types. Three of the 62 latex-free gloves (4.8%, 95% CI 0% to 10%) were perforated, 1 of the 22 orthopedic gloves (4.5%, 95% CI −4% to 13%) was perforated and 4 of the 108 orthopedic latex-free gloves (3.7%, 95% CI 0% to 7%) were perforated.
Fig. 3.
Glove perforations by type of glove worn.
Type of procedure
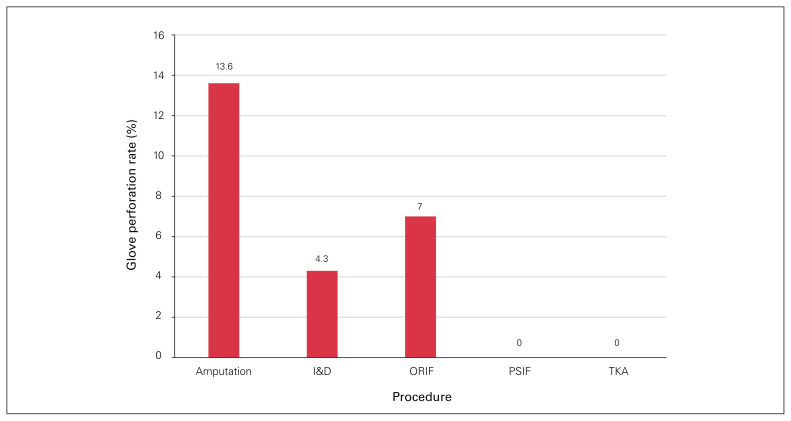
Gloves were collected from a total of 15 procedures. In 57% of these procedures (8 out of 15, 95% CI 32% to 87%) a glove perforation of any nature occurred, while an inner glove perforation occurred in 27% of the procedures (4 out of 15, 95% CI 6% to 51%). An increased risk of perforation was observed in amputations, where 13.6% of gloves were perforated (6 of 44, 95% CI 3% to 24%), and in open reduction internal fixations (ORIFs), where 7.0% of gloves (10 out of 142, 95% CI −3% to 11%) were perforated (p = 0.04) (Figure 4).
Fig. 4.
Glove perforation by procedure type. I&D = irrigation and débridement; ORIF = open reduction internal fixation; PSIF = posterior spinal instrumented fusion; TKA = revision total knee arthroplasty.
Length of procedure
Of the 15 procedures in which gloves were collected, operative times ranged from 21 to 179 minutes. Of the 18 gloves identified to have perforations, 14 were from procedures lasting longer than 60 minutes. However, when we compared the mean operative time of procedures in which perforations occurred (mean 75.5 [standard deviation (SD) 36.5] min) with that of procedures in which perforations did not occur (mean 90.3 [SD 61.6] min), there was no significant difference (t = −0.59, p = 0.57). These results were probably skewed by the fact that no perforations occurred in the posterior spinal instrumented fusion and infected knee arthroplasty revision procedures, which had the longest operative times. We therefore analyzed the operative time for ORIFs alone. The operative time of ORIF procedures in which perforations occurred (mean 100.2 [SD 22.5] min) was significantly longer than the operative time of ORIF procedures in which perforations did not occur (mean 54.0 [SD 16.8] min, t = 3.04, p = 0.02).
Discussion
Intraoperative glove perforations contaminate the sterile surgical field and have been shown to have a negative impact on patient outcomes.5,6 During the study period, a high rate of glove perforations was observed (5.9% of all gloves worn), and the majority were not identified by the wearer at the time of perforation. Although 30.7% of outer glove perforations were recognized at the time of perforation, no associated inner glove perforations were recognized by the wearer, even though 50% of inner gloves were perforated in instances in which there was a detectable outer glove perforation. These data suggest that whenever an outer glove perforation occurs, the wearer should suspect an associated inner glove perforation and consider changing both pairs of gloves. This also adds support to the common practice of double gloving in orthopedics, which has been shown to reduce rates of inner glove perforations.15–17
Perforations were experienced by multiple members of the surgical team. Identifiable perforations were found in gloves from the attending staff, resident and scrub nurse, suggesting that everyone on the surgical team should be vigilant about routine glove changes. Our results suggest that attending staff in particular should be cognizant of the risk of glove perforation, regardless of whether they function as the primary or assisting surgeon. In our centre, fellows often take a more passive role in operating, to promote resident learning. This probably explains the lack of perforations in gloves worn by fellows.
We did not find that the type of glove worn made a significant difference in terms of perforation rate, a finding that has been observed in previous studies.7,8 However, our study was underpowered to detect a true difference in perforation rates between glove types, as evidenced by the wide confidence intervals in the perforation rates of specific glove types.
The current literature suggests that certain procedures and tasks, such as cleaning drill bit flutes, are associated with greater rates of perforation.4 Although amputations and ORIF procedures resulted in higher rates of perforation in our study, the limited sample size of procedures limits the conclusions that can be drawn from this finding.
Previous studies have found that the rate of glove perforation in total joint arthroplasty increases with the duration of glove wear, indicating that routinely changing gloves throughout longer procedures may help prevent contamination caused by glove perforations. 18,19 Recommendations for routine glove changes vary from routine changes every 60 minutes7 to changes after draping20 to changes before handling implants.21 Unfortunately, we could not find any studies that provide specific recommendations for routine gloves changes in orthopedic trauma surgery. The majority of the gloves included in our study were removed at the end of the procedure; however, a number of gloves were changed during the procedure. The reasons for this included suspected perforations, contaminations and routine changes (such as before cementing). None of the gloves that were changed because of routine glove-changing protocols were found to have perforations. Although we found no association between perforations and operative times overall, we found that glove perforations were associated with longer ORIF operative times. Future research should aim to quantify the risk of glove perforation in ORIFs with increasing time, which could provide information on which to base recommendations for routine glove changes to reduce the risk of surgical site infection, while weighing the added financial costs and increased environmental waste.
Limitations
This study has some limitations. Although the overall number of gloves collected and tested was relatively large, they were used in a small number of surgical procedures. Further, comparisons for this study were limited in some respects because of the different numbers of gloves collected for each role, procedure type and glove type. These aspects were not standardized, as the intention was to document a typical series of procedures, but statistical analysis was consequently limited to some degree.
Conclusion
Glove perforations are common in orthopedic trauma procedures.1–4 Attending staff seem to be at an increased risk irrespective of whether they act as the primary or assisting surgeon. Additionally, as half of outer glove perforations recognized by the wearer were associated with an inner glove perforation that was not identified during surgery, when any outer glove perforation is identified the wearer should change both their inner and outer gloves.
Footnotes
Competing interests: None declared.
Contributors: I. Thomson, A. McGuire and S. Mann conceived the study. I. Thomson, N. Krysa, A. McGuire and S. Mann acquired the data, which I. Thomson analyzed. I. Thomson and N. Krysa wrote the article, which all authors critically revised. All authors agreed to be accountable for all aspects of the work.
References
- 1.Gerberding JL, Littell C, Tarkington A, et al. Risk of exposure of surgical personnel to patients’ blood during surgery at San Francisco General Hospital. N Engl J Med 1990;322:1788–93. [DOI] [PubMed] [Google Scholar]
- 2.Panlilio AL, Foy DR, Edwards JR, et al. Blood contacts during surgical procedures. JAMA 1991;265:1533–7. [PubMed] [Google Scholar]
- 3.Eckersley JRT, Williamson DM. Glove punctures in orthopaedic trauma unit. Injury 1990;21:177–8. [DOI] [PubMed] [Google Scholar]
- 4.Lakomkin N, Cruz AI, Fabricant PD, et al. Glove perforation in orthopaedics: probability of tearing gloves during high-risk events in trauma surgery. J Orthop Trauma 2018;32:474–9. [DOI] [PubMed] [Google Scholar]
- 5.Harnoss JC, Peartecke LI, Heidecke CD, et al. Concentration of bacteria passing through puncture holes in surgical gloves. Am J Infect Control 2010;38:154–8. [DOI] [PubMed] [Google Scholar]
- 6.Misteli H, Weber WP, Reck S, et al. Surgical glove perforation and the risk of surgical site infection. Arch Surg 2009;144:553–8. [DOI] [PubMed] [Google Scholar]
- 7.Demicray E, Unay K, Bilgili MG, et al. Glove perforation in hip and knee arthroplasty. J Orthop Sci 2010;15:790–4. [DOI] [PubMed] [Google Scholar]
- 8.Sanders R, Fortin P, Ross E, et al. Outer gloves in orthopaedic procedures. Cloth compared with latex. J Bone Joint Surg Am 1990;72:914–7. [PubMed] [Google Scholar]
- 9.Matta H, Thompson AM, Rainey JB. Does wearing two pairs of gloves protect operating theatre staff from skin contamination? BMJ 1988;297:597–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thanni LOA, Yinusa W. Incidence of glove failure during orthopedic operations and the protective effect of double gloves. J Natl Med Assoc 2003;95:1184–8. [PMC free article] [PubMed] [Google Scholar]
- 11.Thomas S, Agarwal M, Mehta G. Intraoperative glove perforation — single versus double gloving in protection against skin contamination. Postgrad Med J 2001;77:458–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Partecke LI, Goerdt AM, Langer I, et al. Incidence of microperforation for surgical gloves depends on duration of wear. Infect Control Hosp Epidemiol 2009;30:409–14. [DOI] [PubMed] [Google Scholar]
- 13.Carter AH, Casper DS, Parvizi J, et al. A prospective analysis of glove perforation in primary and revision total hip and total knee arthroplasty. J Arthroplasty 2012;27:1271–5. [DOI] [PubMed] [Google Scholar]
- 14.Food and Drug Administration. Leakage test method for surgical and examination gloves. Med Dev Doc Instr Rep 1988;14:11. [Google Scholar]
- 15.Guo YP, Wong PM, Li Y, et al. Is double-gloving really protective? A comparison between the glove perforation rate among perioperative nurses with single and double gloves during surgery. Am J Surg 2012;204:210–5. [DOI] [PubMed] [Google Scholar]
- 16.Laine T, Aarnio P. How often does glove perforation occur in surgery? Comparison between single gloves and a double-gloving system. Am J Surg 2001;181:564–66. [DOI] [PubMed] [Google Scholar]
- 17.Martin-Bertolin S, Gonzales-Martinez R, Gimenez CN, et al. Does double gloving protect surgical staff from skin contamination during plastic surgery? Plast Reconstr Surg 1997;99:956–60. [DOI] [PubMed] [Google Scholar]
- 18.Al-Maiyah M, Bajwa A, Finn P, et al. Glove perforation and contamination in primary total hip arthroplasty. J Bone Joint Surg Br 2005;87:556–9. [DOI] [PubMed] [Google Scholar]
- 19.Kim K, Zhu M, Munro JT, et al. Glove change to reduce the risk of surgical site infection or prosthetic joint infection in arthroplasty surgeries: a systematic review. ANZ J Surg 2019;89:1009–15. [DOI] [PubMed] [Google Scholar]
- 20.McCue SF, Berg EW, Saunders EA. Efficacy of double-gloving as a barrier to microbial contamination during total joint arthroplasty. J Bone Joint Surg Am 1981;63:811–3. [PubMed] [Google Scholar]
- 21.Ward WG, Cooper JM, Lippert D, et al. Glove and gown effects on intraoperative bacterial contamination. Ann Surg 2014;259:591–7. [DOI] [PubMed] [Google Scholar]