Abstract
(1) Background: the prevalence of postnatal depression (PND) reaches up to 20%. PND could be based on the interaction between a psychological vulnerability and chronic stress that pregnancy would activate. Vulnerability factors reflect a psychological profile mirroring mindfulness-trait (MT). A high level of MT is associated with an efficient regulation of both physiological and psychological stress, especially negative moods. Interestingly, mindfulness level can be improved by program based on mindfulness meditation. We hypothesize that MT is a protective factor for PND. We also postulate that negative moods increase during the pregnancy for women who develop a PND after delivery (2) Methods: we conducted a multicentric prospective longitudinal study including 85 women during their first trimester of their pregnancy and 72 from the childbirth to the baby’s first birthday”. At the inclusion, presence and acceptance of MT and various variables of personality and of psychological functioning were assessed. Mood evolution was monitored each month during the pregnancy and a delivery trauma risk was evaluated after delivery. PND detection was carried out at 48 h, 2, 6 and 12 months after the delivery with the Edinburgh Postnatal Depression Scale with a screening cut-off >11. (3) Results: high-acceptance MT is a protective factor for PND (OR: 0.79). Women without PND displayed less negative mood during pregnancy (p < 0.05 for Anxiety, Confusion and Anger). (4) Conclusions: these results suggest the value of deploying programs to enhance the level of mindfulness, especially in its acceptance dimension, before, during and after pregnancy, to reduce the risk of PND.
Keywords: mindfulness-trait, postnatal depression, chronic stress, acceptance
1. Introduction
Postnatal depression (PND) is the most common childbearing complication with a prevalence range of 5–25% in Western countries [1,2,3]. This prevalence differs between culture [2]. PND can have a broad range of depressive symptoms which varies in how severe they are. Symptoms may take some time to develop. It can start at any time within the first year after giving birth and may develop suddenly or gradually. This maternal pathology does not only affect the mother but the infant and family. The consequences for infants on the long-term emotional and cognitive development may be severe. Partner and family are also affected, thus PND appears to be a major public health problem [4]. The earlier it is recognized, diagnosed and treated, the faster the recovery will be. However, diagnosis of PND varies widely according to the methodological parameters. Currently, the Edinburgh Postnatal Depression Scale (EPDS) is the main screening tool widely used to detect, diagnose and assess the severity of the depression [5].
The mechanisms through which PND develop is not yet understood. During pregnancy and postpartum periods, the maternal organism undergoes remarkable biological, physical, social and emotional changes. Furthermore, an estimated 30% of pregnant women report psychosocial stress in their daily lives including job strain and depressive or anxiety symptoms [6]. Mounting evidence shows that the perinatal period is a time of increased vulnerability for mood disturbances and the onset of psychiatric disorders [7]. Altogether, the available data suggest that chronic stressors challenge women’ adaptability during the pregnancy and that the antenatal period offers a “window of opportunity” during which a preventative approach to this condition can be instituted. Although psychological and biological distress responses in pregnant women have been associated with poor fetal outcomes [8,9,10], little is known about the relationship between stress regulation ability and the risk of PND. Literature mainly focused on socio-psychological risk factors, among them personality factors, mediators of adaptation related to life event and to pregnancy, past-traumatic events or delivery trauma [1]. A particularly important risk factor would be a history of mood or anxiety disorder, especially having active symptoms during pregnancy [11]. Recently, the PND has been conceptualized from a biopsychosocial perspective [1].
In applied clinical psychology and psychiatry, the measurement of mood states is an important practical and behavior assessment consideration. Indeed, mood is less tightly linked to particular events than emotion and is thought to reflect the cumulative impact of multiple stressors (e.g., depression; [12]). The theory of mood postulates that mood involves a mechanism which monitors our physical and mental energy levels in relation to the perceived energy demands of our environment, and generates corresponding cognitive biases in our reasoning style, attention, memory, thought, and creativity [13,14]. Mood is likely to be relevant to understand behavior because it seems that subjects in a more positive mood state deal more easily with negative short-term experiences: a positive mood might therefore alleviate single negative events and stabilize emotional reactions. On the contrary, a negative mood state might taint experiences quite generally. For example, in sports, decreased Profile of Mood States vigor alert the coach to the risk of overtraining the athlete [15]. During intensified military training, depression ratings of participants suffering from the overtraining syndrome show a major increase, whereas depression ratings in healthy participants increase only little [16]. Keeping a careful watch for changes in mood can be useful in non-clinical population as such variations may reflect changes in others difficult to assess psychological states that are important. Mood states are thought to become particularly important and visible in situations of ambiguity and uncertainty where the expectation of a subject is pre-shaped to a smaller extent by the circumstances of the situation, as the pregnancy could be an example [17,18]. Furthermore, a body of literature suggests the interest of the dynamics of affective states to predict mood or sleep disorders, especially during pregnancy [19]. Since mood could represent the overall momentum, and its biasing is considered to influence on the perception of our environment, it is postulated that mood changes could reflect the potential dysfunctions of the adaption to our environment and that it might contribute to the symptoms of mood disorders [12,20,21]. Although few data on the follow-up of the mood of the pregnant woman are available, it seems relevant to better know the dynamics of the moods during the pregnancy as a follow-up that could reflect the cumulative impact of multiple stressors.
Stress regulation during pregnancy has been mainly studied by focusing on negative abilities for validated risk factors of PND with neuroticism, assessed during pregnancy, clearly in relationship with a subsequent PND [8,9]. However, the positive psychology initiative, with its focus on the science of wellbeing and optimal human functioning, also suggests the importance of understanding protective factors to psychopathology. A pertinent protective factor that is understudied in the PND is the mindfulness trait (MT). MT characterizes the awareness that emerges through paying attention on purpose, in the present moment, and nonjudgmentally to the unfolding experience moment by moment [22]. Mindfulness has been conceptualized as a kind of trait, i.e., the ability to be mindful in one’s everyday life, regardless of events and stably in time [23,24]. MT refers to at least two dimensions: acceptance and presence [22,25]. The acceptance dimension consists of accepting inner events such as emotions, thoughts or beliefs when one feels them without judging it as either good or bad and without any reference to resignation [26]. Presence is the feeling of being present here and now. The presence feeling is based on an enhanced awareness of information that comes from within (body awareness and self-awareness), and outside the body (world awareness). As shown by mindfulness studies, positive associations were found between mindfulness and efficient emotional regulation, reduced perceived stress, and lower rates of negative mood and of psychological distress, including depression [27,28]. Its association with the Big Five personality traits [29] shows that MT mitigates negative reactivity tendencies associated with neurotiscism [30,31]. Furthermore, in line with the relevance of mood for dealing with uncertainty naturalistic environment, it has been showed that mindwandering and external distraction (all the more that the situation is stressful) are both manifestations of a common state of reduced attention focus that could participate to the level of negative mood. One of the processes of MT is that mindfulness functioning could help to deal with mindwandering and external distraction for maintaining a better level of positive mood and a lower level of negative mood [32,33]. Recently, it has been shown that MT enhances a positive childbirth experience which is known as reducing levels of postpartum depression [34]. Altogether, these studies suggest that MT could be a protective factor for PND. Interestingly, in line with the well-known benefits of mindfulness interventions for depression and relapses of depression [35,36,37], including in the general population [38], recent pilot studies showed that prenatal mindfulness interventions have potential benefits for improving the emergence of perinatal depression [39,40].
So far, no study has investigated the links between MT and the risk of PND. By taking into account the most usual psychological factors of PND and in line with the literature showing that MT is a protective factor to psychopathologies, we first hypothesized that a high level of MT would be a protective factor for PND. We further hypothesize that mindfulness may be the most important protective factor among the factors already studied. Furthermore, referring to the better emotion regulation associated to MT, our second hypothesis postulated that a high level of MT would be associated with less negative emotions during the pregnancy. The cumulative framework of chronic stress leads to the postulation that the increase in negative mood may come at the end of pregnancy. This exploratory hypothesis aims to evaluate the relevance of a follow up of the mood states during the pregnancy.
2. Materials and Methods
2.1. Participants
We conducted a multicentric prospective longitudinal study between May 2017 and March 2021 including 85 pregnant women. The study took place in three French hospitals: Pôle HFME, CHR Mercy, Metz—Maternité GH Diaconesses Croix St Simon, Paris—Centre Aliénor d’Aquitaine, CHU Pellegrin, Bordeaux. The women involved in the study had to meet the following requirements: (1) Inclusion criteria: before 17th week of gestation, pregnancy monitoring planned within one of the four facilities involved in the project, women over 18 years, covered by the French National Health Service and (2) Non-inclusion criteria: pathological pregnancy requiring increased medical monitoring, multiple pregnancy, ongoing pathologies at the time of inclusion: (i) immune or endocrine conditions; (ii) any psychological disorders (PTSD, depression or anxiety disorders, etc.); or (iii) neurological pathologies such as multiple sclerosis, hormonal or psychotropic drug therapies.
The study received prior approval from the Ile de France III Personal Protection Committee (21/06/2016; ID RCB: 2016-A00887-44; NTC 03088319). All women received information on the protocol and gave written consent prior to participation.
2.2. Protocole
This study followed pregnant women from the first four months of pregnancy up to 12 months’ post-birth. Each woman had to attend 10 visits: one visit within the first 16 weeks of pregnancy (inclusion visit (VI)), one visit every month between month 5 to month 9 of the pregnancy (VP5 to VP9), one visit within the 48 h of the birth (VB1) and three visits 2, 6 and 12 months after delivery (VB2, VB3 and VB4, respectively). Except the last three VB visits which has been performed remotely, each visit was realized at the hospital by a midwife or a clinical research assistant. During each visit, participant had to complete different questionnaires, see Table 1 and Table 2 for detailed description. The last three VB visits were remotely performed.
Table 1.
Synopsis of study design. Study timeline for each participant.
|
1st
Trimester |
2nd
Trimester |
3rd
Trimester |
Delivery | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Month | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
| Visit | VI | VP5 | VP6 | VP7 | VP8 | VP9 | VB1 | VB2 | VB3 | VB4 | ||||||||||||
Table 2.
Synopsis of study design. Details of visit requirements. Each participant will have to attend 10 visits from their 1st trimester of pregnancy up to 12 months post-delivery. VI: inclusion visit, VP: pregnancy visits from the 4th month to the 9th month of pregnancy, VB: post-birth visits 48 h, 2, 8 and 12 months post-delivery. FMI: Freiburg Mindfulness Inventory, POMS: Profile of Mood Scale, EPDS: Edinburgh Postnatal Depression Scale, TCI-R: Temperament and Character Inventory-Revised, STAI: State-Trait Anxiety Inventory (Trait version), WEMWBS: Warwick-Edinburgh Mental Well-being Scale, SCL-90: Symptom Checklist-90 revised, QoL: Quality of Life, PAI: Prenatal Attachment Inventory, DAD-P: postpartum depression risk screening questionnaire, MSPSS: Multidimensional Scale of Perceived Social Support, LAS: Labour Agentry Scale, TES: Trauma Event Scale, PDEQ: Peritraumatic Dissociative Experiences Questionnaire, ITA: traumatic impact of childbirth questionnaire. The “x” mark indicates when the questionnaire was completed.
| Pregnancy | Post-Birth | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Inclusion Visit VI First Trimester |
Monthly Visit During Trimester 2 and 3 |
Follow-Up Visit Post Delivery |
|||||||||
| VP5 | VP6 | VP7 | VP8 | VP9 | VB1 | VB2 | VB3 | VB4 | |||
| Regulatory information | Notice—Consent form | x | |||||||||
| Keys-questionnaires | Socio-demographic information | x | |||||||||
| FMI | x | ||||||||||
| POMS | x | x | x | x | x | x | |||||
| EPDS | x | x | x | x | |||||||
| General psychological functioning | TCI-R | x | |||||||||
| STAI | x | ||||||||||
| WEMWBM | x | ||||||||||
| SCL-90 | x | ||||||||||
| QoL | x | x | x | x | x | x | |||||
| Specific psychological pregnancy and delivery functioning | PAI | x | x | x | x | x | x | ||||
| DAD-P | x | ||||||||||
| MSPSS | x | x | x | x | x | x | |||||
| LAS | x | ||||||||||
| Trauma and post-traumatic stress disorder questionnaires | TES | x | |||||||||
| PDEQ | x | ||||||||||
| ITA | x | ||||||||||
| Duration of questionnaires (minutes) | 120 | 15 | 15 | 15 | 15 | 15 | 30 | 5 | 5 | 5 | |
2.3. Variables
2.3.1. Sociodemographic Data
Sociodemographic information included age, social environment, professional and marital status, and the number of children. We also asked the women about their history of psychological care or support and their personal and familial history of depression. Questions about their pregnancy history and the condition of the current pregnancy were also asked.
2.3.2. Three Main Questionnaires
For the PND status: PND was assessed using the Edinburgh Postnatal Depression Scale (EPDS) with a screening cut-off >11 [41]. French validation showed good psychometric qualities [42]. The EPDS is a 10-item self-report questionnaire assessing the symptoms of depression and anxiety. Each self-descriptive statement about the 7 last days was evaluated using a four-point Likert scale ranging from 0 (no change from usual) to 3 (an important change from usual). It was fulfilled four times at VB1, VB2, VB3 and VB4.
For the mindfulness evaluation: the 14-item, self-administered Freiburg Mindfulness Inventory short form (FMI short form) assessed mindfulness [25] developed for people without any background knowledge in mindfulness [25]. French validation showed good psychometric qualities [43]. It constitutes a consistent and reliable scale evaluating several important aspects of mindfulness, which indexes trait mindfulness as presence and nonjudgmental acceptance [25]. Each self-descriptive statement was evaluated using a four-point Likert scale ranging from 1 (strongly disagree) to 4 (strongly agree). Depending on the suggested time frame, state-and trait-like components could be assessed. In the present study, the short form was used for measuring MT. It was fulfilled once at VIN.
For the mood follow-up: The mood was evaluated at the beginning of both sessions using an abbreviated version of the Profile of Mood States (POMS) [44]. French version replicated the English initial validation [45]. Abbreviated version of the POMS consisted in an adjective checklist of 37 items rated on a five-point scale that ranges from 1 (not at all) to 5 (extremely). The subjects were asked to answer according to their present mood. Six factors were then calculated: anxiety-tension, depression-dejection, anger-hostility, fatigue-inertia, vigor-activity and confusion-bewilderment. It was fulfilled during the pregnancy from VI to VP9, unless the woman gave birth before 9 months of pregnancy. Given that pregnancy produce a multitude of affective changes, the use of multidimensional mood model (not only positive or negative), as the POMS does, appears relevant.
2.3.3. Four Questionnaires for the General Psychological Functioning
Cloninger’s Temperament and Character Inventory-Revised (TCI-R) short-version is a 56 items self-report questionnaire with 5-grade Likert scale responses ranging from definitely false to true [46,47,48]. It is intended to assess the individual differences of the four temperaments (Harm Avoidance, Novelty Seeking, Reward Dependence and Persistence) and three character higher-order dimensions (Self-Directedness, Cooperativeness and Self- Transcendence). Each higher order dimension is further divided into sub-scales. It is considered as a useful instrument to assess Cloninger’s model of the 7 dimensions of personality in non-clinical samples [46,47,48].
Anxiety-trait level was assessed using the French version of the Spielberger State-Trait-Anxiety Inventory (S-STAI; [49,50]). The 20 items of the trait subscale ask subjects to indicate the intensity of their anxiety in general. In this study and the sample was categorized in three groups according to their score [36]: women with a high score (score > 65), women with a middle score of trait-anxious-trait (56 < score ≤ 65), and women with a low score (score < 56).
The Warwick-Edinburgh Mental Well-being Scale (WEMWBS, [51,52]) covers both hedonic constructs including the subjective experience of happiness and life satisfaction, and eudaemonic constructs addressing psychological functioning and self-realization in the previous two weeks [51]. It comprises 14 items and responses are made on a 5-point scale ranging from “none of the time” to “all of the time”. The scale is suitable for monitoring mental well-being in healthy populations as it shows few ceiling or floor effects [51].
The Symptom Checklist-90 revised (SCL90R, [53]), is a common mental health evaluation tool used to assess psychological problems. Each item is scored on a scale from 0 (“not at all”) to 4 (extremely”) based on how much an individual was bothered by each item in the last weeks. Five symptoms’ dimensions were evaluated: somatization—, obsessive-compulsive—OC, interpersonal sensitivity—IS, depression—D, and anxiety—A.
Four homemade analogic visual scales (from 0 “very bad/low” to 10 “very good/high”) were used for quality of life assessment: (1) ”in the past month, how would you rate the quality of your sleep?”, (2) “in the past month, how would you rate your stress level at work?”, (3) “ in the past month, how would you rate your level of stress at home?” and (4) “in the past month, how would you rate your level of apprehension about giving birth?”
2.3.4. Four Questionnaires for the Specific Pregnancy and Delivery Psychological Functioning
The Prenatal Attachment Inventory (PAI, [54]) is a 21 items questionnaire for expectant mothers which assess maternal-fetal attachment defined as the strength of mothers’ emotional ties with the fetus (and also known as prenatal bonding. It captures variability in expectant mothers’ behaviours, cognitions and emotions towards the fetus, which appear important for positive prenatal health practices [55]. Expectant women were asked to assess how often they engaged in specific thoughts or behaviours towards the fetus on a 4-point scale (1 « almost never » to 4 « almost always »).
The Questionnaire de Dépistage Anténatal du risque de Dépression du Postpartum (DAD-P; postpartum Depression Risk Screening Questionnaire), previously named le Questionnaire de Genève, was used to detect women at risk to develop PND already during pregnancy [56]. It is based on 10 items, six for screening, and four supplementary items for optimizing the screening leading to several screening strategies, depending on whether broad or targeted screening is.
The Multidimensional Scale of Perceived Social Support (MSPSS) is a 12 items questionnaire assessing the perceived social support from three sources: Family, Friends, and a Significant Other [57]. A seven-point Likert-type scale ranging from “strongly disagree (1)” to “strongly agree (7)” was used with a total score obtained by adding the score for each statement, divided by the total number of statements. It was validated for expectant women [58].
The Labour Agentry Scale (LAS) is a 29 items instrument measuring expectancies and experiences of personal control during childbirth [59]. It consists of short affirmative statements (e.g., ‘I felt confident’ and ‘I felt tense’). Women were asked to rate each statement on a seven-point Likert scale from 1 (representing rarely) to 7 (representing almost always).
2.3.5. Three Questionnaires for Delivery Trauma and Post-Traumatic Stress Disorder (PTSD)
The traumatic event scale (TES) was a 21 items questionnaire developed in accordance with DSM-IV criteria for the PTSD syndrome and comprises all the DSM-IVR symptoms and criteria of PTSD [60,61]. The TES was divided on two parts: the part one (TES 1) quantifies frequency and severity of single posttraumatic stress symptoms focusing on childbird; part two (TES 2) assesses how each of the 21 symptoms impacts the daily quality of life.
The Peritraumatic Dissociative Experiences Questionnaire (PDEQ) is 10-items self-questionnaire assessing peritraumatic dissociation that occurred at the time of a trauma [62,63]. Dissociation is well-recognized as a risk factor for developing PTSD. A five-point Likert-type scale ranging from “not true (1)” to “totally true (5)” was used. A score greater than or equal to 22 attests to the presence of clinically significant peri-traumatic dissociation [64].
The traumatic impact of childbirth questionnaire (ITA) assesses the recollection of experience during labour and delivery. It is constituted first, by 18 items rated from 1 to 7 (ITA-1), then, by 14 items rated from 1 to 6(ITA-2). This specific questionnaire has not yet been validated.
2.4. Statistical Analysis
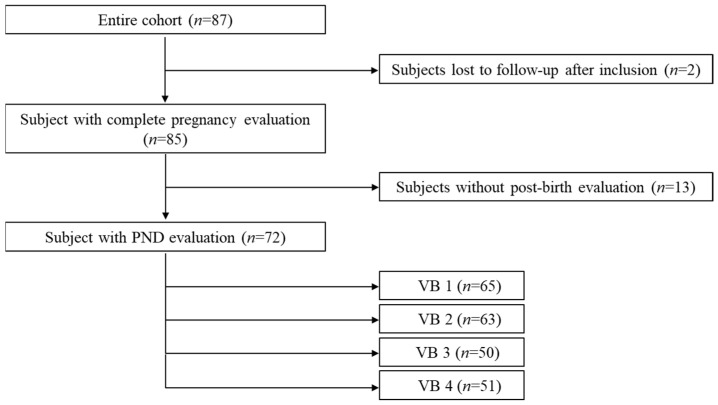
All statistical analyses were performed using SPSS software (SPSS INC, Chicago, IL, USA, version 24.0) and Stata software (Stata corp, College Station, Texas, USA, v.14). The reliability of each psychological measurement (self-administered questionnaire) was gauged by computing Cronbach’s alpha and all alphas were above 0.74, which indicates good reliability. The description of the population was complemented by a flow chart showing PND trajectories (Figure 1).
Figure 1.
Flow diagram showing subpopulations within the initial cohort with the sample size at each of the four VB sessions.
For the description of the sample at VI, we have completed the presentation of the sociobiographical data by separate comparisons on MT score at VI and POMS sub-scores at VI according to the PND status after delivery. Each comparison was applied using t-test or Mann-Whitney test if normal distribution was not found. PND status was evaluated using a score above 11 on the EPDS that is recognized as the sensitive and specific threshold for PND [28]. The PDN + group consisted of women with a score on the EPDS above 11 at least at one of the post-birth visits (VB1, VB2, VB3 or VB4). The PND - group consisted of women with EPDS score always below the threshold (11) whatever the post-birth visits.
For the first aim of the study, multivariate logistic regressions were used for evaluated the risk factors of the PND from variables that were recorded either at VI (SD, FMI, TCI-R, S-STAI, WEMWBS, SCL90, DAD-P), or during pregnancy (VG mean scores for each of the sub-factors of the POMS, of the MSPSS and at VB1 (LAS, TES, PDEQ and ITA) (Table 1 and Table 2). The variables significant at the 20% threshold in univariate (Table 5) were added to the multivariate model and then a backward selection was carried out until the final model with variables significant at the 5% threshold was obtained (Table 6). We calculated unadjusted odds ratios for significant variables. The fit to the statistical model verified by analysis of the residuals and the Hosmer-Lemeshow goodness-of-fit test.
For the second aim of the study, separate inter-group (PND + versus PND −) comparisons were carried out on each mood variable using repeated measures analysis of variances (ANOVAs) or Mann-Whitney test at each session of the pregnancy if normal distribution and homogeneity of variance were not found.
The significance level was set at p ≤ 0.05.
3. Results
3.1. Population
The studied cohort (n = 72) was extracted from the initial population (n = 85) by taking into account the women who had at least one EPDS assessment post-birth (Figure 1). The number of women with PND + was assessed among the 72 women with a response on the EPDS at least at one of the post-birth visits (VB1, VB2, VB3 or VB4). At VB1, 65 women completed the EDPS and 12 had a score above 11 (18.46%); at VB2, 63 women completed the EDPS and 12 had a score above 11 (19.05%); at VB3, 50 women completed the EDPS and 9 had a score above 11 (18%); and at VB4, 51 women completed the EDPS and 7 had a score above 11 (13.72%).
Taking into account the women who had at least one score strictly higher than 11 on the EPDS during the postpartum follow-up, 26 women had an episode of PND (PND+). There was no difference between the 3 centers in terms of the number of PNDs per center in relation to the number of women included in each center.
Socio-demographic characteristics of the initial cohort are summarized in Table 3.
Table 3.
Summary of the socio demographic data of the initial cohort.
| Characteristics | |||
|---|---|---|---|
| Age | 32.4 +/− 4.5 years (29.0–35.0) | ||
| Pregnancy Age at the Inclusion | 16.7 Weeks of Amenorrhea (WA) +/−2.0 WA (15.2–18.0 WA) | ||
| n | % | ||
| Site repartition | Paris | 43 | 50.6 |
| Bordeaux | 32 | 37.6 | |
| Metz | 10 | 11.8 | |
| Marital status | Couple | 81 | 96.4 |
| Couple but single living | 3 | 3.6 | |
| Geographical celibacy | 1 | 0.01 | |
| Missing data | 1 | 0.01 | |
| Historic of psychological care | Psychological support | 51 | 60 |
| No psychological support | 34 | 40 | |
| Number of children | No child | 57 | 67.9 |
| One child | 22 | 26.2 | |
| Two or more children | 6 | 6 | |
| Previous pregnancies | None | 48 | 56.5 |
| Previous pregnancy * | 15 | 17.6 | |
| Two or more pregnancies | 22 | 25.8 | |
| Type of pregnancy | Spontaneous | 79 | 92.9 |
| Medically assisted reproduction: | 6 | 7.1 | |
| Desired pregnancy | Yes | 74 | 88.1 |
| No | 10 | 11.9 | |
| Missing data | 1 | 0.01 | |
*: (including spontaneous miscarriage, voluntary termination of pregnancy, and medical termination of pregnancy).
3.2. PND
In accordance with the flow chart, comparisons were applied at VI between the two groups (PND + and PND −) for the FMI and POMS key questionnaires for the cohort of 72 women who had at least one EPDS assessment post-birth. As showed in Table 4, significant differences were found for mindfulness acceptance and mindfulness total mean scores. Except for confusion-bewilderment mood subscale, no difference was observed in terms of mood at inclusion.
Table 4.
Differences between PND + and PND − for the FMI and POMS key questionnaires at VI in the sample of 72 women.
| Variables | DPN + Mean (SD) |
DPN − Mean (SD) |
p-Value * | |
|---|---|---|---|---|
| Freiburg Mindfulness Questionnaire (FMI) |
Presence | 17.5(3) | 18(2.6) | 0.52 |
| Acceptance | 19.6(3.1) | 212(3.5) | 0.003 | |
| Total | 37.1(5) | 40(5.3) | 0.03 | |
| Profile of Mood Scale (POMS) |
Anxiety-tension | 6(5.5) | 3.8(3.8) | 0.08 |
| Anger-hostility | 3.2(3.7) | 1.8(3.7) | 0.11 | |
| Depression | 1.7(2.22) | 1.3(2.5) | 0.5 | |
| Fatigue-inertia | 5.5(4.7) | 5(3.8) | 0.63 | |
| Activity-vigor | 11.3(4.1) | 11.8(3.8) | 0.6 | |
| Confusion-bewilderment | 3(3) | 1.5(1.9) | 0.03 |
*: t-test.
3.3. Risk Factors for the PND
Among the 72 women who had at least one EPDS accessment post-birth, the univariate analysis showed that among the categorical explanatory variables (i.e., sociodemographic variables), none were significant except for the history of psychological care or support. It also showed the quantitative variables of interest (Table 5) among them FMI-acceptance and FMI total scores.
Table 5.
The associations between potential predictors, measured at V1, VG or VP1, and postnatal depression, determined in univariate regression analyses. Only predictors that were significant at the 20% threshold in previous analyses are included.
| Sessions | Variables * | Odds-Ratio | IC 95 % | p-Value |
|---|---|---|---|---|
| VI | FMI_acceptance | 0.9 | 0.66–0.93 | 0.003 |
| FMI_total | 0.90 | 0.80–0.99 | 0.025 | |
| TCI_ Self-Directedness | 1.14 | 1.03–1.26 | 0.010 | |
| TCI_ Cooperativeness | 1.13 | 0.97–1.35 | 0.120 | |
| POMS_tension_anxiety | 1.11 | 1.00–1.25 | 0.050 | |
| POMS_ anger-hostility | 1.11 | 0.98–1.28 | 0.110 | |
| POMS_ confusion-bewilderment | 1.29 | 1.05–1.63 | 0.013 | |
| STAI-Trait | 0.034 | |||
| Very low | — | — | ||
| Low | 4.52 | 1.25–21.76 | 0.033 | |
| Middle | 8.87 | 1.80–54.92 | 0.011 | |
| High | 6.33 | 0.21–194.45 | 0.232 | |
| WEMWBS | 0.94 | 0.87–1.02 | 0.127 | |
| SCL_obsessive-compulsive, | 4.21 | 1.75–11.93 | 0.001 | |
| SCL_ interpersonal sensitivity | 2.57 | 1.03–7.34 | 0.042 | |
| SCL_depression | 3.21 | 1.39–8.67 | 0.005 | |
| SCL_anxiety | 2.32 | 1.00–6.20 | 0.050 | |
| SCL_hostility | 3.28 | 1.13–11.11 | 0.028 | |
| SCL_Phobic anxiety | 4.12 | 0.57–40.20 | 0.160 | |
| SCL_Paranoid ideation | 2.71 | 0.76–10.86 | 0.124 | |
| SCL_Psychoticism | 5.30 | 1.49–32.65 | 0.005 | |
| SCL_General Severity Index | 6.38 | 1.76–31.34 | 0.003 | |
| SCL_Positive Symptom Total | 1.04 | 1.01–1.08 | 0.012 | |
| SCL_, Positive Symptom Distress Index | 0.72 | 0.52–0.93 | 0.012 | |
| MSPSS_Friends | 0.70 | 0.41–1.16 | 0.165 | |
| MSPSS_total | 0.61 | 0.32–1.11 | 0.104 | |
| QoL_ level of stress at work | 1.16 | 1.01–1.38 | 0.038 | |
| Age | 0.93 | 0.82–1.03 | 0.178 | |
| History of psychological care | 0.006 | |||
| No | — | — | ||
| Yes | 4.06 | 1.50–11.62 | 0.006 | |
| Number of children | 0.018 | |||
| 0 | — | — | ||
| 1 | 0.30 | 0.06–1.07 | 0.086 | |
| More than 2 | 6.44 | 0.87–131.50 | 0.108 | |
| VG ** | POMS_tension_anxiety | 1.41 | 1.15–1.79 | <0.001 |
| Prenatal Attachment Inventory | 0.94 | 0.88–1.00 | 0.066 | |
| MSPSS_Friends | 0.67 | 0.38–1.12 | 0.128 | |
| MSPSS_total | 0.57 | 0.29–1.09 | 0.088 | |
| QoL_ quality of sleep | 0.77 | 0.58–0.98 | 0.037 | |
| QoL_level of stress at work | 1.25 | 1.02–1.56 | 0.029 | |
| QoL_level of stress at home | 1.49 | 1.15–2.01 | 0.002 | |
| PND Risk Screening Questionnaire | 0.175 | |||
| Having no risk | — | — | ||
| Having a risk | 3.47 | 0.57–23.78 | 0.180 | |
| VP1 | Traumatic event scale 1 | 1.16 | 0.99–1.39 | 0.068 |
| Traumatic event scale 2 | 1.31 | 1.12–1.62 | <0.001 | |
| ITA_1 | 1.07 | 1.03–1.12 | <0.001 | |
| ITA_2 | 1.09 | 1.03–1.18 | 0.003 | |
| Labour Agentry | 0.90 | 0.84–0.95 | <0.001 | |
| Peritraumatic Dissociative Experiences | 0.001 | |||
| Score < 22 | — | — | ||
| Score ≥ 22 | 7.33 | 2.12–34.55 | 0.004 |
* FMI: Freiburg Mindfulness Inventory; TCI: Cloninger’s Temperament and Character Inventory; POMS: Profile of Mood Scale; STAI: State and Trait Anxiety Inventory; WEMWBS: Warwick-Edinburgh Mental Well-being Scale; SCL: Symptom Checklist; MPSS: Multidimensional Scale. — means that the modality in the row is the reference in the comparison with the other modalities of Perceived Social Support; QoL: Quality of Life; TES: traumatic event scale. ** VG was calculated as the average monthly scores.
The multivariate analysis highlighted odds ratios for unadjusted variables with the significant results Table 6.
Table 6.
The final model resulting from the multivariate b selection procedure. In this procedure only variables were included that were significant in the univariate regression analyses.
| Variables | OR * | CI 95% ** | p-Value |
|---|---|---|---|
| FMI_acceptance (VI) | 0.79 | 0.66–0.93 | 0.003 |
| SCL_obsessive-compulsive (VI) | 4.21 | 1.75–11.93 | 0.001 |
| Having an history of psychological care (VI) | 4.06 | 1.50–11.62 | 0.006 |
* OR: Odds ratios; ** CI: Confidence Interval, VI: visit at inclusion.
Finally, the index plot does not detect any outliers or suspicious structuring and the linear prediction/residuals graph is satisfactory. The Hosmer-Lemeshow goodness-of-fit test is compatible with the data (p > 0.05).
3.4. Mood Evolution during the Pregnancy According to PND Status
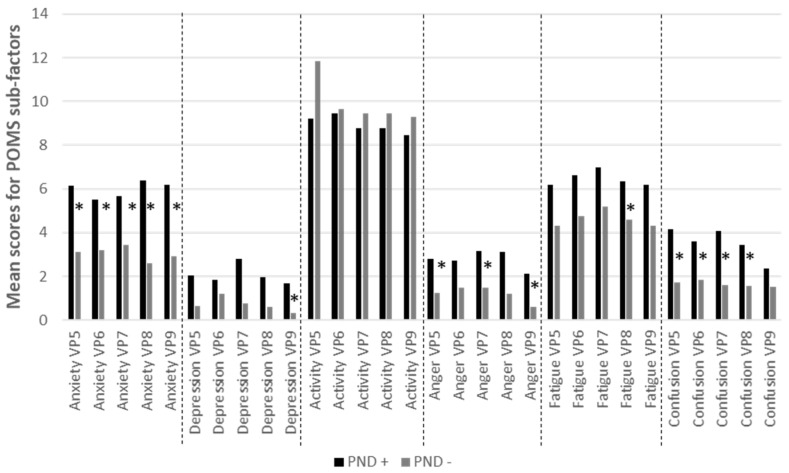
Overall, Mann-Whitney tests applied at each session among the 72 women who had at least one EPDS assessment post-birth showed that the PND + group had more negative moods than the PND- group. The significant differences observed are displayed in Figure 2. at each session of the pregnancy if normal distribution and homogeneity of variance were not found Briefly, DPN+ women appeared to have significantly higher score in Anxiety (at each time point), Confusion (4 time points out of 5) and Anger (3 time points out of 5).
Figure 2.
Differences between the two PND groups in their POMS mean sub-scores. Differences were tested with a Mann-Whitney test, *: p < 0.05.
Many trends towards a difference between the two groups are observed: VP7 depression (p = 0.054), VP8 depression (p = 0.076), VP6 fatigue (p = 0.063), VI confusion (p = 0.062), and VP9 confusion (p = 0.087). No difference was observed for activity-vigor measures during pregnancy.
4. Discussion
This study investigated the links between MD and the risk of PND in physiological pregnancy with the main hypothesis that MD would constitute a protective factor for the risk of PND. Results are partially in accordance with this hypothesis by showing that the acceptance dimension of MD is the only pregnancy-related protective factor.
Acceptance is characterized by an absence of resignation when perceiving one’s own experience through an attitude of acknowledging the experience rather than judging it as either good or bad. Although empirical research has mainly operationalized mindfulness as a unidimensional construct, or as a presence ability, research on the acceptance dimension has so far been limited. The exact nature of acceptance is not yes understood. Shedding further light on the differential roles of presence and acceptance would contribute to disentangling the processes through which mindfulness impacts pregnancy mental effects on women [65]. Thus, the acceptance dimension of the MD could actually act as an emotional buffer that allows reaction without overinterpreting the stressful situation induced by the pregnancy, the anticipation of delivery or the delivery itself. Furthermore, it can be proposed that acceptance prevent women who have suffered from losses or threats because of pregnancy as suggest by the absence of effect of having an unplanned pregnancy. This hypothesis needs further study for validation. Acceptance could also prevent women who have been psychologically weakened by them from reacting less judiciously to situations that arise in the future as suggested by the absence of effect of being pregnant for the first time or not. From this perspective, the mindfulness acceptance disposition could serve as a protective factor by providing access to beneficial resources during the process of pregnancy. This is suggested by the absence of protective effect of the perceived social support that the results highlighted. In order to face many changes and adaptations, mainly outside the woman’s control (e.g., bodily changes and physical complaints) that occur during pregnancy, different psychological processes can be called upon. It is not intended to be exhaustive, but rather to suggest processes that the limited existing literature on acceptance has already shown. Acceptance could first allow access to the feeling of self-efficacy [66] for dealing with the changes that a pregnancy implies. Given the relationship between flexibility and mindfulness for emotion regulation [67], acceptance could further foster flexibility and this would help women to cope with the singular time of the pregnancy and the stressful situation of delivery. Furthermore, fully conscious acceptance, i.e., being aware of one’s painful thoughts and emotions as they are, without trying to suppress or avoid them has been recently studied by the concept of self-compassion [68]. Several studies have reported the usefulness of self-compassion in the face of difficult situations: for example, it allows a better stress management by acting on biopsychosocial responses [69], protects against depression and negative affect [70,71,72].
Results also identified risk factors for PND. They highlighted two main risk factors by showing that the obsessive-compulsive dimension of the Symptom Checklist-90 and having an history of psychological care increases by 3 to 4 the risk of triggering a PND. Obsessive-compulsive disorder (OCD) has its own chapter (obsessive–compulsive and related disorders) in DSM-5 and is no longer considered an anxiety disorder (APA; 61). It is characterized by a combination of intrusive thoughts and ritualistic behaviors carried out in an attempt to allay the anxiety associated with these thoughts. The general community life-time prevalence of OCD throughout the world is approximately 1% whereas a higher rate of 2–3% is observed in pregnant and postpartum women [61]. Higher rates among women in the postpartum period were sometimes described with a prevalence of 11% at 2 weeks postpartum [73,74]. Almost half of these women had persistence of symptoms at 6 months postpartum [73,74]. Clinical studies of OCD indicate that symptoms are stress-responsive [73,74,75]. This suggests that stressful situations, such as pregnancy and the postpartum period, may exacerbate or perhaps even predispose women to OCD symptoms. The postpartum period appears to be a high-risk time for the development of OCD symptoms [76]. Although the overlap between OCD and depression is still a matter of debate, both in terms of the mechanisms involved and the risk factors [77], obsessive-compulsive personality disorder symptoms could be a risk factor for postpartum depressive symptoms [66,67,68,69,70,71,72,73,74,75,76,77,78]. If additional data reinforce this hypothesis, it suggests that an assessment of OCD or obsessive-compulsive personality disorder may be useful for screening pregnant women for PND risk. Our results found that a simple obsessive-compulsive symptoms evaluation, collected no later than the 4th month of pregnancy, lead to a relevant screening for PND risk. This result was in line with the influence of having an history of psychological care, which underlies a vulnerability profile. Indeed, findings have suggested some potential psychological vulnerability factors for development of obsessive-compulsive symptoms [79,80]. With an effect of the culture, the vulnerability profile includes cognitive factors of appraisal and thought control, religiosity, self-esteem and personality characteristics such as neuroticism [80]. This psychological vulnerability could be related to a physiological stress vulnerability [80,81]. Mothers showing a low-level parasympathetic activity may have fewer emotional, physiological, and psychological resources for dealing with the challenge of the post-birth [81,82,83]. Interestingly, this profile of vulnerability did not include risk factors related to the experience of pregnancy such as the prenatal attachment, prenatal depression risk or the labour agentry. Likewise, trauma as experience of traumatic delivery was not found to be risk factor of PND.
In accordance with our second hypothesis and given the relationship between acceptance and emotional regulation [71], we observed differences in negative mood level during pregnancy between women with PND and healthy women. All negative mood, including anxiety-tension, depression-dejection, anger-hostility, fatigue-inertia, and confusion-bewilderment were higher for PND+ whereas no difference was found in vigor-activity mood. The differences mainly appeared after the first trimester of the pregnancy with a peak in the last months of the pregnancy, except for the anger-hostility mood which was higher for the PND+ group compared to the PND- group at the inclusion visit. Anger is an emotional state or mood according to the duration of stat which is considered as the tip of the iceberg, while other underlying negative emotions, such as fear, disappointment, and anxiety, sometimes induce anger [84]. Anger is associated with cognitive distortions, verbal and motor behavior, and patterns of physical arousal and then depression [84]. More precisely, personal trait anger (i.e., high trait anger) lead to internalized anger and not expressing themselves, processes which increase the risk of depression [85,86]. In line, previous studies have found a clear relationship between maternal anger in post-natal and PND [85,86,87,88]. Pregnant women who have high trait anger tend to have greater difficulty in regulating their emotions, including anger, for dealing with the post-natal lifestyle changes [88,89]. However, anger during pregnancy has less been studied. In the last trimester, resilience was found as one of the mediator between trait anger and PND [89]. Our results suggest that anger expression is present from the first trimester of pregnancy in the PDN-to-be women. Interestingly, on one hand, previous work has suggested that angry and aggressive tendencies may be reduced in individuals with higher levels of dispositional mindfulness because of their better ability to regulate emotions [90,91], including acceptance awareness ability [92]. On the other hand, higher trait anger and anger suppression was reported for patients with OCD and was associated with non-acceptance of negative emotions compared to non-OCD subjects [90,91,92]. Mindfulness acceptance would be a protective factor for PND by allowing a better regulation and expression of anger. In addition, on a clinical point of view, mood assessment could be useful to screen for low levels of suffering that may or may not be an indicator of PND risk. Whether or not mood is a good marker of a risk of progressing to PND need further research. Nevertheless, mood assessment is neither stigmatizing nor anxiety-provoking. In addition to taking into account small changes in mood during pregnancy may simply allow the initiation of self-confidence to rely on perinatal professionals in order to better live the pregnancy.
Main limitations of this study concern the sample and the method. First, our sample is small and results need to be confirmed by further studies. Moreover, those preliminary results are only applicable to women with physiological pregnancy, since women with pathological pregnancy (as defined by requiring increased medical monitoring, multiple pregnancy, ongoing pathologies at the time of inclusion) were excluded. Second, we only used to the Cloninger’s Temperament and Character Inventory-Revise which assesses the individual differences of the four temperaments (Harm Avoidance, Novelty Seeking, Reward Dependence and Persistence) and three character higher-order dimensions (Self-Directedness, Cooperativeness and Self- Transcendence). We cannot infer trait anger or obsessive-compulsive type personality disorders. Third, the history of psychological treatment which is found to be a risk factor to PND was not studied in detail. It would be relevant to ask women more information about the psychological help that they received as how long did it last for better understanding this risk factor in its relationship with PND. Fourth, the statistical analyses were based on many questionnaires which is a weakness of the study but since it was an explanatory study, statistics were conducted without any preconception. Furthermore, we collected rather few sociodemographic variables compared to the number of psychometric variables. Finally, PND status was evaluated using a score above 11 on the EPDS at least at one of the post-birth visits (VB1, VB2, VB3 or VB4). This choice of categorization based on a single score above the threshold may have overestimated the number of women with PND. PND + status could have been confirmed by a clinician or decided after two successive measurements above the threshold.
5. Conclusions
This study highlights that women with a high level of acceptance were less at risk of developing a PND whereas women with a vulnerability profile including obsessive-compulsive symptoms and an history of psychological care before the pregnancy were more at risk of PND. Furthermore, anger mood was present at the beginning of the pregnancy for women who develop a PND. Further studies should be undertaken to focus on assessing the acceptance and presence dimensions more specifically in order to continue disentangling their potential different effects on PND risk.
Interestingly, mindfulness practices improve one’s ability to be mindful [93]. Mindfulness practices rely on training one’s mind to sustain attention on bodily experiences, primarily breathing, and deliberately return one’s attention to these experiences whenever they are distracted [94]. Recent studies found a benefit effect on mindfulness practices as a valuable preparation for the challenges they met during pregnancy, childbirth and parenthood [95] and as a prevention for PND in the perinatal period [96].
However, there is currently a real need to evaluate the benefit of mindfulness training during pregnancy. Practices that develop an individual’s capacity to be mindful have been individualized in the form of intervention programs. Meditation consists of concentrating on one’s sensations during breathing exercises, which then represent an attentional baseline, thus making it possible to notify any other body sensation in relation to this baseline. Among these practices, we should note "mindfulness-based stress reduction" (MBSR) [39,93] and the "mindfulness-based cognitive therapy" (MBCT) [97]. These first programs were used to focus on the management of chronic pain, stress and then depression. Training programs, as ACT (Acceptance Commitment Therapy; [67,98,99]), could be used preferentially to develop the acceptance dimension during pregnancy by focusing on developing the ability to focus on one’s own experience for dealing with the stress of the pregnancy. They also could be used as a psychological support for the stress of delivery as for the stress and daily worries that appear after delivery.
Acknowledgments
This study is part of a project supported by the French Military Health Service with the participation of three maternities. The authors wish to thank the physicians and the midwives of these maternities. We are grateful to all participants for their collaboration.
Author Contributions
M.T. and A.M.D. designed the study and wrote the manuscript. Each author participated in the development of the last version of the manuscript. All authors read and approved the final manuscript. Each author contributed to the study’s design. E.S., M.B., A.-L.S.-D., T.H., D.T., F.H. and M.-L.E. were involved in women inclusion and follow-up. M.T., A.M.D., D.F. and D.T. carried out the study. S.M. carried out statistical analyses. A.M.D., D.F., C.V., C.B. and D.T. were responsible for data pre-analyses. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by grant number PDH-1-SMO-2-0407 (EUR 35,000) from the French Health Service (SSA) and the General Direction for Armament (DGA).
Institutional Review Board Statement
The study was conducted according to guidelines given in the Declaration of Helsinki, and approved by the Ethics Committee of Ile de France III (protocol code ID RCB: 2016-A00887-44; NTC 03088319 of 21 June 2016).
Informed Consent Statement
Written informed consent was obtained from participants to publish this paper.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. Data are not publicly available as they concern a specific population.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Martínez-Borba V., Suso-Ribera C., Osma J., Andreu-Pejó L. Predicting Postpartum Depressive Symptoms from Pregnancy Biopsychosocial Factors: A Longitudinal Investigation Using Structural Equation Modeling. Int. J. Environ. Res. Public Health. 2020;17:8445. doi: 10.3390/ijerph17228445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Woody C.A., Ferrari A.J., Siskind D.J., Whiteford H.A., Harris M.G. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J. Affect. Disord. 2017;219:86–92. doi: 10.1016/j.jad.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization Maternal Mental Health and Child Development in Low and Middle-Income Countries. 2008. [(accessed on 12 November 2021)]. Available online: www.who.int/mental_health/prevention/suicide/mmh_jan08_meeting_report.pdf.
- 4.Slomian J., Honvo G., Emonts P., Reginster J.Y., Bruyère O. Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Women’s Health. 2019;15:1745506519844044. doi: 10.1177/1745506519844044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moraes G.P., Lorenzo L., Pontes G.A., Montenegro M.C., Cantilino A. Screening and diagnosing postpartum depression: When and how? Trends Psychiatry Psychother. 2017;39:54–61. doi: 10.1590/2237-6089-2016-0034. [DOI] [PubMed] [Google Scholar]
- 6.Loomans E.M., van Dijk A.E., Vrijkotte T.G., van Eijsden M., Stronks K., Gemke R.J., Van den Bergh B.R. Psychosocial stress during pregnancy is related to adverse birth outcomes: Results from a large multi-ethnic community-based birth cohort. Eur. J. Public Health. 2013;23:485–491. doi: 10.1093/eurpub/cks097. [DOI] [PubMed] [Google Scholar]
- 7.Meltzer-Brody S., Howard L.M., Bergink V., Vigod S., Jones I., Munk-Olsen T., Honikman S., Milgrom J. Postpartum psychiatric disorders. Nat. Rev. Dis. Primers. 2018;4:18022. doi: 10.1038/nrdp.2018.22. [DOI] [PubMed] [Google Scholar]
- 8.Simons S.S.H., Zijlmans M.A.C., Cillessen A.H.N., De Weerth C. Maternal prenatal and early postnatal distress and child stress responses at age 6. Stress. 2019;22:654–663. doi: 10.1080/10253890.2019.1608945. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. [(accessed on 20 December 2021)]. Available online: https://www.who.int/mental_health/prevention/suicide/lit_review_postpartum_depression.pdf.
- 10.Walsh K., Mccormack C.A., Webster R., Pinto A., Lee S., Feng T., Krakovsky H.S., O’Grady S.M., Tycko B., Champagne F.A., et al. Maternal prenatal stress phenotypes associate with fetal neurodevelopment and birth outcomes. Proc. Natl. Acad. Sci. USA. 2019;116:23996–24005. doi: 10.1073/pnas.1905890116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stewart D.E., Vigod S.N. Postpartum Depression: Pathophysiology, Treatment, and Emerging Therapeutics. Annu. Rev. Med. 2019;70:183–196. doi: 10.1146/annurev-med-041217-011106. [DOI] [PubMed] [Google Scholar]
- 12.Eldar E., Rutledge R.B., Dolan R.J., Niv Y. Mood as Representation of Momentum. Trends Cogn. Sci. 2016;20:15–24. doi: 10.1016/j.tics.2015.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Raoult C.M.C., Moser J., Gygax L. Mood as Cumulative Expectation Mismatch: A Test of Theory Based on Data from Non-verbal Cognitive Bias Tests. Front. Psychol. 2017;8:2197. doi: 10.3389/fpsyg.2017.02197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wong M.Y. Towards a theory of mood function. Philos. Psychol. 2016;29:179–197. doi: 10.1080/09515089.2015.1024830. [DOI] [Google Scholar]
- 15.Kreher J.B., Schwartz J.B. Overtraining syndrome: A practical guide. Sports Health. 2012;4:128–138. doi: 10.1177/1941738111434406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vrijkotte S., Roelands B., Pattyn N., Meeusen R. The Overtraining Syndrome in Soldiers: Insights from the Sports Domain. Mil. Med. 2019;184:e192–e200. doi: 10.1093/milmed/usy274. [DOI] [PubMed] [Google Scholar]
- 17.Sorenson D.L. Uncertainty in pregnancy. Naacog’s Clin. Issues Perinat. Women’s Health Nurs. 1990;1:289–296. [PubMed] [Google Scholar]
- 18.Sevil Degirmenci S., Kosger F., Altinoz A.E., Essizoglu A., Aksaray G. The relationship between separation anxiety and intolerance of uncertainty in pregnant women. J. Matern.-Fetal Neonatal Med. 2020;33:2927–2932. doi: 10.1080/14767058.2018.1564030. [DOI] [PubMed] [Google Scholar]
- 19.Sperry S.H., Walsh M.A., Kwapil T.R. Emotion dynamics concurrently and prospectively predict mood psychopathology. J. Affect. Disord. 2020;261:67–75. doi: 10.1016/j.jad.2019.09.076. [DOI] [PubMed] [Google Scholar]
- 20.Bei B., Coo S., Trinder J. Sleep and Mood during Pregnancy and the Postpartum Period. Sleep Med. Clin. 2015;10:25–33. doi: 10.1016/j.jsmc.2014.11.011. [DOI] [PubMed] [Google Scholar]
- 21.Hillerer K.M., Neumann I.D., Slattery D.A. From stress to postpartum mood and anxiety disorders: How chronic peripartum stress can impair maternal adaptations. Neuroendocrinology. 2012;95:22–38. doi: 10.1159/000330445. [DOI] [PubMed] [Google Scholar]
- 22.Kabat-Zinn J. Wherever You Go, There You Are. Hyperion Books; New York, NY, USA: 1994. [Google Scholar]
- 23.Grossman P., Niemann LSchmidt S., Walach H. Mindfulness-based stress reduction and health benefits. A meta-analysis. J. Psychosom. Res. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 24.Lutz A., Jha APDunne J.D., Saron C.D. Investigating the Phenomenological Matrix of Mindfulness-related Practices from a Neurocognitive Perspective. Am. Psychol. 2015;70:632–658. doi: 10.1037/a0039585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Walach H., Buchheld N., Buttenmüller V., Kleinknecht N., Schmidt S. Measuring mindfulness—the Freiburg mindfulness inventory (FMI) Pers. Individ. Differ. 2006;40:1543–1555. doi: 10.1016/j.paid.2005.11.025. [DOI] [Google Scholar]
- 26.Hayes A.M., Feldman G. Clarifying the construct of mindfulness in the context of emotion regulation and the process of change in therapy. Clin. Psychol. Sci. 2004;11:255–262. doi: 10.1093/clipsy.bph080. [DOI] [Google Scholar]
- 27.Baer R.A., Smith G.T., Hopkins J., Krietemeyer L., Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- 28.Brown K.W., Ryan R.M. The benefits of being present: Mindfulness and its role in psychological well-being. J. Pers. Soc. Psychol. 2003;84:822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 29.Hanley A.W., Garland E.L. The mindful personality: A meta-analysis from a cybernetic perspective. Mindfulness. 2017;8:1456–1470. doi: 10.1007/s12671-017-0736-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barnhofer T., Duggan D.S., Griffith J.W. Dispositional mindfulness moderates the relation between neuroticism and depressive symptoms. Pers. Individ. Differ. 2011;51:958–962. doi: 10.1016/j.paid.2011.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Giluk T.L. Mindfulness, Big Five personality, and affect: A meta-analysis. Pers. Individ. Differ. 2009;47:805–811. doi: 10.1016/j.paid.2009.06.026. [DOI] [Google Scholar]
- 32.Hulsbosch L.P., Boekhorst M.G.B.M., Potharst E.S., Pop V.J.M., Nyklíček I. Trait mindfulness during pregnancy and perception of childbirth. Arch. Women’s Ment. Health. 2021;24:281–292. doi: 10.1007/s00737-020-01062-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baer R.A. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clin. Psychol. Sci. Pract. 2006;10:125–143. doi: 10.1093/clipsy.bpg015. [DOI] [Google Scholar]
- 34.Carmody J., Baer R.A. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J. Behav. Med. 2008;31:23–33. doi: 10.1007/s10865-007-9130-7. [DOI] [PubMed] [Google Scholar]
- 35.Hofmann S.G., Sawyer A.T., Witt A.A., Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J. Consult. Clin. Psychol. 2010;78:169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Freudenthaler L., Turba J.D., Tran U.S. Emotion regulation mediates the associations of mindfulness on symptoms of depression and anxiety in the general population. Mindfulness. 2017;8:1339–1344. doi: 10.1007/s12671-017-0709-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hall H.G., Beattie J., Lau R., East C., Anne Biro M. Mindfulness and perinatal mental health: A systematic review. Women Birth. 2016;29:62–71. doi: 10.1016/j.wombi.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 38.Matvienko-Sikar K., Lee L., Murphy G., Murphy L. The effects of mindfulness interventions on prenatal well-being: A systematic review. Psychol. Health. 2016;31:1415–1434. doi: 10.1080/08870446.2016.1220557. [DOI] [PubMed] [Google Scholar]
- 39.Sun Y., Li Y., Wang J., Chen Q., Bazzano A.N., Cao F. Effectiveness of Smartphone-Based Mindfulness Training on Maternal Perinatal Depression: Randomized Controlled Trial. J. Med. Internet Res. 2021;23:e23410. doi: 10.2196/23410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Woolhouse H., Mercuri K., Judd F., Brown S.J. Antenatal mindfulness intervention to reduce depression, anxiety and stress: A pilot randomised controlled trial of the MindBabyBody program in an Australian tertiary maternity hospital. BMC Pregnancy Childbirth. 2014;14:369. doi: 10.1186/s12884-014-0369-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cox J.L., Holden J.M., Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 42.Guedeney N., Fermanian J. Validation study of the French Version of the Edinburgh Postnatal Depression Scale (EPDS): New results about use and psychometric properties. Eur. Psychiatry. 1998;13:83–89. doi: 10.1016/S0924-9338(98)80023-0. [DOI] [PubMed] [Google Scholar]
- 43.Trousselard M., Steiler D., Raphel C., Cian C., Duymedjian R., Claverie D., Canini F. Validation of a French version of the Freiburg Mindfulness Inventory-short version: How mindfulness deals with the stress in a working middle-aged opulation. Biopsychosoc. Med. 2010;4:8. doi: 10.1186/1751-0759-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shacham S. A shortened version of profile of mood states. J. Pers. Assess. 1983;47:305–306. doi: 10.1207/s15327752jpa4703_14. [DOI] [PubMed] [Google Scholar]
- 45.Fillion L., Gagnon P. French Adaptation of the Shortened Version of the Profile of Mood States. Psychol. Rep. 1999;84:188–190. doi: 10.2466/pr0.1999.84.1.188. [DOI] [PubMed] [Google Scholar]
- 46.Cloninger C.R., Svrakic D.M., Przybeck T.R. A psychobiological model of temperament and character. Arch. Gen. Psychiatry. 1993;50:975–990. doi: 10.1001/archpsyc.1993.01820240059008. [DOI] [PubMed] [Google Scholar]
- 47.Cloninger C.R., Svrakic N.M., Svrakic D.M. The Role of personality self-organization in development of mental order and disorder. Dev. Psychopathol. 1997;9:881–906. doi: 10.1017/S095457949700148X. [DOI] [PubMed] [Google Scholar]
- 48.Adan A., Serra-Grabulosa J.M., Natale V. A reduced Temperament and Character Inventory (TCI-56). Psychometric properties in a non-clinical sample. Pers. Individ. Differ. 2009;46:687–692. doi: 10.1016/j.paid.2009.01.023. [DOI] [Google Scholar]
- 49.Spielberger C. Manual for the State-Trait-Anxiety Inventory: STAI (Form Y) Consulting Psychologists Press; Palo Alto, CA, USA: 1983. [Google Scholar]
- 50.Spielberger C.D., Smith L.H. Anxiety (drive), stress, and serial-position effects in serial-verbal learning. J. Exp. Psychol. 1966;72:589–595. doi: 10.1037/h0023769. [DOI] [PubMed] [Google Scholar]
- 51.Tennant R., Hiller L., Fishwick R., Platt S., Joseph S., Weich S., Parkinson J., Secker J., Stewart-Brown S. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): Development and UK validation. Health Qual. Life Outcomes. 2007;5:63. doi: 10.1186/1477-7525-5-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Trousselard M., Canini F., Dutheil F., Claverie D., Fenouillet F., Naughton G., Steward-Brown S., Franck N. Investigating well-being in healthy population and schizophrenia with the WEMWBS. Psychiatry Res. 2016;245:282–290. doi: 10.1016/j.psychres.2016.08.050. [DOI] [PubMed] [Google Scholar]
- 53.Derogatis L.R., Lipman R.S., Rickels K., Uhlenhuth E.H., Covi L. The Hopkins Symptom Checklist (HSCL): A self-report symptom inventory. Behav. Sci. 1974;19:1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- 54.Muller M.E. Development of the Prenatal Attachment Inventory. West J. Nurs. Res. 1993;15:199–211. doi: 10.1177/019394599301500205. [DOI] [PubMed] [Google Scholar]
- 55.Foley S., Hughes C. Great expectations? Do mothers’ and fathers’ prenatal thoughts and feelings about the infant predict parent-infant interaction quality? A meta-analytic review. Dev. Rev. 2018;48:40–54. doi: 10.1016/j.dr.2018.03.007. [DOI] [Google Scholar]
- 56.Righetti-Veltema M., Conne-Perréard E., Bousquet A., Manzano J. Construction et validation multicentrique d’un questionnaire prépartum de dépistage de la dépression postpartum. Psychiatr. Enfant. 2007;49:513–541. doi: 10.3917/psye.492.0513. [DOI] [Google Scholar]
- 57.Zimet G.D., Dahlem N.W., Zimet S.G., Farley G.K. The Multidimensional Scale of Perceived Social Support. J. Pers. Assess. 1988;52:30–41. doi: 10.1207/s15327752jpa5201_2. [DOI] [Google Scholar]
- 58.Denis A., Callahan S., Bouvard M. Evaluation of the French version of the Multidimensional Scale of Perceived Social Support during the postpartum period. Matern. Child Health J. 2015;19:1245–1251. doi: 10.1007/s10995-014-1630-9. [DOI] [PubMed] [Google Scholar]
- 59.Hodnett E.D., Simmons-Tropea D.A. The Labour Agentry Scale: Psychometric properties of an instrument measuring control during childbirth. Res. Nurs. Health. 1987;10:301–310. doi: 10.1002/nur.4770100503. [DOI] [PubMed] [Google Scholar]
- 60.Wijma K., Söderquist J., Wijma B. Posttraumatic stress disorder after childbirth: A cross sectional study. J. Anxiety Disord. 1997;11:587–597. doi: 10.1016/S0887-6185(97)00041-8. [DOI] [PubMed] [Google Scholar]
- 61.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Autho; Washington, DC, USA: 1994. [Google Scholar]
- 62.Marmar C.R., Weiss D.S., Metzler T.J. The Peritraumatic Dissociative Experiences Questionnaire. In: Wilson J.P., Marmar C.R., editors. Assessing Psychological Trauma and Posttraumatic Stress Disorder. The Guilford Press; New York, NY, USA: 1997. pp. 412–428. [Google Scholar]
- 63.Birmes P., Brunet A., Benoit M., Defer S., Hatton L., Sztulman H., Schmitt L. Validation of the Peritraumatic Dissociative Experiences Questionnaire self-report version in two samples of French-speaking individuals exposed to trauma. Eur. Psychiatry. 2005;20:145–151. doi: 10.1016/j.eurpsy.2004.06.033. [DOI] [PubMed] [Google Scholar]
- 64.Birmes P., Carreras D., Ducassé J.-L., Charlet J.-P., Warner B.A., Lauque D., Schmitt L. Peritraumatic Dissociation, Acute Stress, and Early Posttraumatic Stress Disorder in Victims of General Crime. Can. J. Psychiatry. 2001;46:649–651. doi: 10.1177/070674370104600711. [DOI] [PubMed] [Google Scholar]
- 65.Kohls N., Sauer S., Walach H. Facets of mindfulness–Results of an online study investigating the Freiburg mindfulness inventory. Pers. Individ. Differ. 2009;46:224–230. doi: 10.1016/j.paid.2008.10.009. [DOI] [Google Scholar]
- 66.Menges J., Caltabiano M. The effect of mindfulness on academinc self-efficcacy: A randomosed controlled trial. Int. J. Educ. Psychol. Couns. 2019;4:170–186. doi: 10.35631/IJEPC.4310015. [DOI] [Google Scholar]
- 67.Hayes S.C., Luoma J.B., Bond F.W., Masuda A., Lillis J. Acceptance and commitment therapy: Model, processes and outcomes. Behav. Res. Ther. 2006;44:1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 68.Neff K. Self-Compassion: An Alternative Conceptualization of a Healthy Attitude Toward Oneself. Self Identity. 2003;2:85–101. doi: 10.1080/15298860309032. [DOI] [Google Scholar]
- 69.Arch J.J., Brown K.W., Dean D.J., Landy L.N., Brown K., Laudenslager M.L. Self-compassion training modulates alpha-amylase, heart rate variability, and subjective responses to social evaluative threat in women. Psychoneuroendocrinology. 2014;42:49–58. doi: 10.1016/j.psyneuen.2013.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Brown L., Bryant C., Brown V., Bei B., Judd F. Self-compassion, attitudes to ageing and indicators of health and well-being among midlife women. Aging Ment. Health. 2016;20:1035–1043. doi: 10.1080/13607863.2015.1060946. [DOI] [PubMed] [Google Scholar]
- 71.Ford J., Klibert J.J., Tarantino N., Lamis D.A. Savouring and Self-compassion as Protective Factors for Depression: Protective Factors for Depression. Stress Health. 2017;33:119–128. doi: 10.1002/smi.2687. [DOI] [PubMed] [Google Scholar]
- 72.Sauer S., Walach H., Schmidt S., Hinterberger T., Horan M., Kohls N. Implicit and explicit emotional behavior and mindfulness. Conscious. Cogn. 2011;20:1558–1569. doi: 10.1016/j.concog.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 73.Russell E.J., Fawcett J.M., Mazmanian D. Risk of obsessive compulsive disorder in pregnant and postpartum women: A meta-analysis. J. Clin. Psychiatry. 2013;74:377–385. doi: 10.4088/JCP.12r07917. [DOI] [PubMed] [Google Scholar]
- 74.Sharma V., Sommerdyk C. Obsessive–compulsive disorder in the postpartum period: Diagnosis, differential diagnosis and management. Women’s Health. 2015;11:543–552. doi: 10.2217/WHE.15.20. [DOI] [PubMed] [Google Scholar]
- 75.Findley D.B., Leckman J.F., Katsovich L., Lin H., Zhang H., Grantz H., Otka J., Lombroso P.J., King R.A. Development of the Yale Children’s Global Stress Index (YCGSI) and its application in children and adolescents with Tourette’s syndrome and obsessive-compulsive disorder. J. Am. Acad. Child Adolesc. Psychiatry. 2003;42:450–457. doi: 10.1097/01.CHI.0000046816.95464.EF. [DOI] [PubMed] [Google Scholar]
- 76.Toro J., Cervera M., Osejo E., Salamero M. Obsessive-compulsive disorder in childhood and adolescence: A clinical study. J. Child Psychol. Psychiatry. 1992;33:1025–1037. doi: 10.1111/j.1469-7610.1992.tb00923.x. [DOI] [PubMed] [Google Scholar]
- 77.Goodwin G.M. The overlap between anxiety, depression, and obsessive-compulsive disorder. Dialogues Clin. Neurosci. 2015;17:249–260. doi: 10.31887/DCNS.2015.17.3/ggoodwin. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Miller E.S., Chu C., Gollan J., Gossett D.R. Obsessive-compulsive symptoms during the postpartum period. A prospective cohort. J. Reprod. Med. 2013;58:115–122. [PMC free article] [PubMed] [Google Scholar]
- 79.Van Broekhoven K.E.M., Karreman A., Hartman E.E., Lodder P., Endendijk J.J., Bergink V., Pop V.J.M. Obsessive-compulsive personality disorder symptoms as a risk factor for postpartum depressive symptoms. Arch. Women’s Ment. Health. 2019;22:475–483. doi: 10.1007/s00737-018-0908-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Barcaccia B., Tenore K., Mancini F. Early childhood experiences shaping vulnerability to Obsessive-Compulsive Disorder. Clin. Neuropsychiatry. 2015;12:141–147. [Google Scholar]
- 81.Yorulmaz O., Gençöz T., Woody S. Vulnerability factors in OCD symptoms: Cross-cultural comparisons between Turkish and Canadian samples. Clin. Psychol. Psychother. 2010;17:110–121. doi: 10.1002/cpp.642. [DOI] [PubMed] [Google Scholar]
- 82.Lord C., Hall G., Soares C.N., Steiner M. Physiological stress response in postpartum women with obsessive—Compulsive disorder: A pilot study. Psychoneuroendocrinology. 2011;36:133–138. doi: 10.1016/j.psyneuen.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 83.Musser E.D., Ablow J.C., Measelle J.R. Predicting maternal sensitivity: The roles of postnatal depressive symptoms and parasympathetic dysregulation. Infant Ment. Health J. 2012;33:350–359. doi: 10.1002/imhj.21310. [DOI] [PubMed] [Google Scholar]
- 84.Goleman D. Emotional Intelligence: Why It Can Matter More than IQ. Bloomsbury Publishing; London, UK: 1996. [Google Scholar]
- 85.Balsamo M. Anger and depression: Evidence of a possible mediating role for rumination. Psychol. Rep. 2010;106:3–12. doi: 10.2466/PR0.106.1.3-12. [DOI] [PubMed] [Google Scholar]
- 86.Ascenzo N., Collard J.J. Anger, forgiveness, and depression in the postnatal experience. Ment. Health Fam. Med. 2018;13:689–698. [Google Scholar]
- 87.Bruno A., Laganà A.S., Leonardi V., Greco D., Merlino M., Vitale S.G., Triolo O., Zoccali R.A., Muscatello M.R.A. Inside–out: The role of anger experience and expression in the development of postpartum mood disorders. J. Matern. Fetal. Neonatal. Med. 2018;31:3033–3038. doi: 10.1080/14767058.2017.1362554. [DOI] [PubMed] [Google Scholar]
- 88.Ou C.H., Hall W.A. Anger in the context of postnatal depression: An integrative review. Birth. 2018;45:336–346. doi: 10.1111/birt.12356. [DOI] [PubMed] [Google Scholar]
- 89.Tobe H., Kita S., Hayashi M., Umeshita K., Kamibeppu K. Mediating effect of resilience during pregnancy on the association between maternal trait anger and postnatal depression. Compr. Psychiatry. 2020;102:152190. doi: 10.1016/j.comppsych.2020.152190. [DOI] [PubMed] [Google Scholar]
- 90.Bishop S.R., Lau M., Shapiro S., Carlson L., Anderson N.D., Carmody J., Segal Z.V., Abbey S., Speca M., Velting D., et al. Mindfulness: A proposed operational definition. Clin. Psychol. 2004;11:230–241. doi: 10.1093/clipsy.bph077. [DOI] [Google Scholar]
- 91.Gillespie S.M., Garofalo C., Velotti P. Emotion regulation, mindfulness, and alexithymia: Specific or general impairments in sexual, violent, and homicide offenders? J. Crim. Justice. 2018;58:56–66. doi: 10.1016/j.jcrimjus.2018.07.006. [DOI] [Google Scholar]
- 92.Garofalo C., Gillespie S.M., Velotti P. Emotion regulation mediates relationships between mindfulness facets and aggression dimensions. Aggress. Behav. 2020;46:60–71. doi: 10.1002/ab.21868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cludius B., Mannsfeld A.K., Schmidt A.F., Jelinek L. Anger and aggressiveness in obsessive–compulsive disorder (OCD) and the mediating role of responsibility, non-acceptance of emotions, and social desirability. Eur. Arch. Psychiatry Clin. Neurosci. 2021;271:1179–1191. doi: 10.1007/s00406-020-01199-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kabat-Zinn J., Lipworth L., Burney R. The Clinical Use of Mindfulness Meditation for the Self-Regulation of Chronic Pain. J. Behav. Med. 1985;8:163–190. doi: 10.1007/BF00845519. [DOI] [PubMed] [Google Scholar]
- 95.Chiesa A., Serretti A. Mindfulness-based stress reduction for stress management in healthy people: A review and meta-analysis. J. Altern. Complement. Med. 2009;15:593–600. doi: 10.1089/acm.2008.0495. [DOI] [PubMed] [Google Scholar]
- 96.Lönnberg G., Nissen E., Niemi M. What is learned from Mindfulness Based Childbirth and Parenting Education?—Participants’ experiences. BMC Pregnancy Childbirth. 2018;18:466. doi: 10.1186/s12884-018-2098-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations preliminary results. Gen. Hosp. Psychiatry. 1982;4:33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]
- 98.Segal Z.V., Williams J.M.G., Teasdale J.D. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse. Guilford Press; New York, NY, USA: 2022. p. 351. [Google Scholar]
- 99.Flaxman P.E., Bond F.W. Acceptance and Commitment Therapy (ACT) in the Workplace. In: Baer R.A., editor. Mindfulness-Based Treatment Approaches: Clinician’s Guide to Evidence Base and Applications. Elsevier Academic Press; Amsterdam, The Netherlands: 2006. pp. 377–402. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. Data are not publicly available as they concern a specific population.