ABSTRACT
Lung cancer screening (LCS) programs are increasing worldwide. Incidental findings (IFs) on LCS are defined as low-dose CT findings unrelated to the primary purpose of identifying lung cancer. Most IFs on LCS are benign and clinically insignificant but are being increasingly recognized, and some require urgent referral for further diagnostic workup. Other findings are expected and are known as smoking-related comorbidities, including COPD, cardiovascular disease, emphysema, and interstitial lung disease, and their diagnosis can have a significant impact on patient prognosis. The purpose of this pictorial essay is to illustrate the most common IFs on LCS, organized by organ. We will discuss the current literature on IFs on LCS, focusing on their prevalence, appropriate communication, and triggering of clinical pathway systems.
Keywords: Diagnostic screening programs, Lung neoplasms, Incidental findings
RESUMO
Os programas de rastreamento de câncer de pulmão (RCP) estão aumentando em todo o mundo. Achados incidentais (AI) no RCP são achados de TC de baixa dose sem relação com o propósito principal de identificar câncer de pulmão. A maioria dos AI no RCP é benigna e clinicamente insignificante, mas os AI estão sendo cada vez mais reconhecidos, e alguns requerem encaminhamento urgente para investigação diagnóstica adicional. Outros achados são esperados e conhecidos como comorbidades relacionadas ao tabagismo, tais como DPOC, doença cardiovascular, enfisema e doença pulmonar intersticial, e seu diagnóstico pode ter um impacto significativo no prognóstico do paciente. O propósito deste ensaio pictórico é ilustrar os AI mais comuns no RCP, organizados por órgão/sistema. Discutiremos a literatura atual a respeito de AI no RCP, com foco em sua prevalência, comunicação apropriada e desencadeamento de procedimentos clínicos.
Descritores: Programas de triagem diagnóstica, Neoplasias pulmonares, Achados incidentais
INTRODUCTION
With the increasing number of lung cancer screening (LCS) programs worldwide, incidental findings (IFs) have also increased significantly. 1 - 3 IFs on LCS can be defined as low-dose CT (LDCT) findings that can potentially affect the health of the patient and are unrelated to the primary purpose of identifying lung cancer. 1 , 4 , 5 Most IFs are benign and clinically insignificant-the most common being pulmonary findings (69%), cardiovascular findings (67%), and gastrointestinal findings (25%)-but some require urgent recognition and further management. 2
The reported prevalence of IFs on LCS ranges from 1% to 19%, being as high as 94% in more recent reports. 2 - 6 This wide variation is explained by the lack of standards regarding the reporting and management of IFs on LCS. IFs are also a cause of stress and anxiety. In an ongoing interdisciplinary population-based long-term cohort study, a report of IFs is expected to be given to 10% of participants. The study participants have stated that they are highly interested in this report and that they would not have participated otherwise, even if admitting to increased levels of stress when receiving mail from the study. 7 It is a reasonable expectation, shared by both patients and referring colleagues, that significant IFs should be communicated effectively or acted upon.
Communication standards for urgent and unexpected findings are clear, as addressed by guidelines from the American College of Radiology (ACR) and the European Society of Radiology (ESR). 8 , 9 IFs, however, may not be urgent nor necessarily unexpected. The ACR Incidental Findings Committee has developed by consensus a series of white papers addressing IFs in multiple organs and systems, including the chest (mediastinal and cardiovascular findings), upper abdomen, and thyroid, although not specific to LCS. These serve as important guidance on reporting, communication, and management of IFs until specific guidelines are developed. 10 - 14
Different communication strategies have been suggested for reporting IFs on LCS. The Lung CT Screening Reporting and Data System provides the S modifier for clinically significant or potentially clinically significant non-lung cancer findings 15 but does not specify which IFs should be reported or acted upon. The ESR and the European Respiratory Society (ERS) recommend that IFs that are clinically significant (i.e., with a major or adverse impact, or for which there is an established intervention that benefits the patient) and of general agreement (i.e., minimal interobserver variation) be reported and a recommendation for intervention be given. This recommendation falls within one of four categories (levels of management): immediate action, likelihood of nonpulmonary cancer, further investigation, and clinically insignificant (Table 1). 1
Table 1. Levels of management of incidental findings on lung cancer screening, as recommended by the European Society of Radiology/European Respiratory Society.
| Level of management | Action | |
|---|---|---|
| 1 | Immediate action | Emergency referral (e.g., pneumothorax) |
| 2 | Likelihood of nonpulmonary cancer | Referral to a specialist (e.g., breast mass) |
| 3 | Noncancer findings | Referral to a specialist or a general practitioner (e.g., diffuse lung disease and dilated aorta) |
| 4 | Clinically insignificant | Prone to observer variation and, because there is no established beneficial intervention, do not need to be reported (e.g., minor atelectasis and renal, liver, or thyroid cysts) |
Screening programs should develop a standard approach for the evaluation of these findings. Developing a standard approach to reporting and management of IFs on LCS would promote research into their impact on reducing overall mortality, as well as the development of automatic detection, measurement, and data-mining tools based on artificial intelligence. This evidence-based approach could inform public opinion and the political decision-making process, while optimizing the cost-effectiveness of LCS programs and the health gains to their participants.
This pictorial essay illustrates the systematic checklist proposed by the ESR/ERS position paper. 1 Our objective is to help radiologists familiarize with (and not to miss any) IFs, especially those with potential clinical relevance. Clinically significant IFs on LCS are summarized in Table 2.
Table 2. Checklist of clinically significant incidental findings on lung cancer screening (levels 1, 2, and 3). (Continued...).
| Neck | Level of management | ||
|---|---|---|---|
| Thyroid | |||
| Nodules | Ultrasound if > 1.5 cm and invasive or suspicious lymph nodes | 2 | |
| Enlargement | If airway deviation or compression | 3 | |
| Lymphadenopathy | Size, morphology, shape, margins, and distribution | 2 | |
| Chest | |||
| Airways | |||
| Bronchiectasis | + Referral for respiratory evaluation | 3 | |
| Lungs | |||
| Emphysema | Type and severity | 3 | |
| ILD/ILAs | + Referral to ILD team/MDT | 3 | |
| Infection | 3 | ||
| Pleura | |||
| Pneumothorax | + Emergency referral | 1 | |
| Pleural plaques | 3 | ||
| Pleural effusion | 3 | ||
| Heart and Pericardium | |||
| Coronary or valvular calcifications | + Cardiovascular risk assessment | 3 | |
| Stents, grafts, myocardial changes | 3 | ||
| Large pericardial effusion or cysts | May compress adjacent structures | 3 | |
| Pericardial thickening (> 3-4 mm) | 3 | ||
| Esophagus | |||
| Focal esophageal lesions | Smoking is a risk factor for esophageal cancer. | 2 | |
| Diffuse wall thickening | 3 | ||
| Esophageal dilation | 3 | ||
| Mediastinum | |||
| Pneumomediastinum | + Emergency referral | 1 | |
| Masses | 2 | ||
| Lymphadenopathy | 2 | ||
| Vessels | |||
| Aortic aneurysm/ectasia | + Referral to vascular MDT | 3 | |
| Pulmonary artery dilation | 3 | ||
| Atheromatous disease | 3 | ||
| Diaphragm | |||
| Complicated hernias | + Emergency referral | 1 | |
| Uncomplicated hernias | 3 | ||
| Diaphragmatic elevation | 3 | ||
| Breast | |||
| New or previously undiagnosed lesion | 2 | ||
| Previous surgery | 3 | ||
| Abdomen | |||
| Liver | |||
| Focal lesion | Based on the hepatic risk profile | 2 | |
| Biliary system | |||
| Cholecystitis/thickening | 2 | ||
| Cholelithiasis | 3 | ||
| Biliary obstruction | 2 | ||
| Pneumobilia | 3 | ||
| Pancreas, Stomach, and Spleen | |||
| Cysts | 2 | ||
| Solid masses | 2 | ||
| Splenomegaly | 3 | ||
| Kidneys | |||
| Solid renal masses | 2 | ||
| Complex renal cysts | 2 | ||
| Stones >1 cm or in the upper pole | 3 | ||
| Adrenal glands | |||
| Suspicious masses | if > 1 cm, > 10 HU, or growth | 2 | |
| Masses | if < 1 cm, < 10 HU, or stable for > 1 year => no follow-up required | 4 | |
| Peritoneum | |||
| Nodules, infiltrative masses, omental haziness, ascites, and peritoneal thickening | 2 | ||
| Previous surgery | 3 | ||
| Bone/Joints | |||
| Vertebral fractures | 3 | ||
| Low vertebral bone density | 3 | ||
| Suspicious bone masses | 2 | ||
| Skin/subcutaneous and Muscles | |||
| New or previously undiagnosed lesion | 2 | ||
ILD: interstitial lung disease; ILAs: interstitial lung abnormalities; and MDT: multidisciplinary team. Levels of management: (1) immediate action; (2) likelihood of nonpulmonary cancer; and (3) noncancer findings.
NECK
The thyroid gland and neck lymphadenopathy
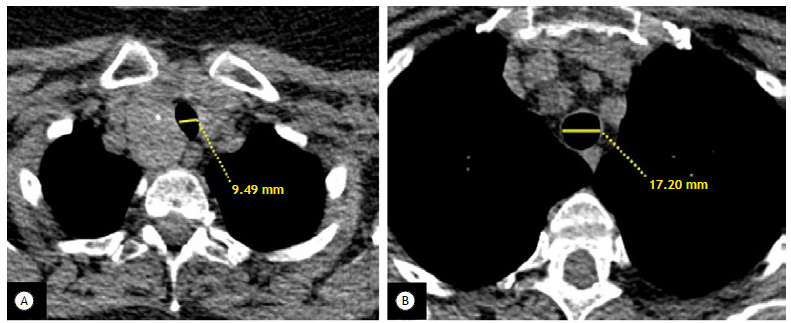
Depending on its anatomy or whether there is thyroid enlargement, the thyroid gland does not normally appear in its entirety on LDCT scans of the chest. Thyroid enlargement should be stated in the report if it causes deviation of the airway significant enough to cause respiratory symptoms (Figure 1). The most common IFs within the thyroid gland are calcifications, nodules, and cysts. The ACR white paper on incidental thyroid nodules recommends further ultrasound evaluation only for nodules larger than 1.5 cm with invasive behavior or associated with suspicious lymph nodes, because small incidental nodules are largely benign or represent indolent neoplasms (papillary carcinoma in most cases), with a 10-year survival rate of nearly 100%. 16
Figure 1. Goiter with tracheal compression. In A, axial image of the upper chest, showing enlargement of the left lobe of the thyroid gland, with coarse calcifications, causing displacement and narrowing of the trachea (tracheal lumen diameter, 9.49 mm). In B, tracheal lumen diameter is 17.20 mm.
Lower neck lymphadenopathy should be reported including size, morphology, shape, margins, and distribution. The criteria for lymphadenopathy include increased size (i.e., > 1 cm in short-axis diameter and on axial images); morphological changes (i.e., rounded shape; ill-defined, irregular margins; and replacement of normal fatty hila with necrosis, cystic change, suspicious calcification, or abnormal enhancement); and asymmetric distribution (i.e., prominent nodes or more than 3 contiguous and confluent lymph nodes along the drainage chain). 17 , 18
THORACIC CAVITY
Trachea, bronchi, and bronchioles
Tracheal disease is usually clinically insignificant and is not commonly reported as an IF on LCS. It can present as changes in the tracheobronchial tree (e.g., diffuse dilation, stenosis, and collapse) or as focal lesions of the tracheal wall that can be benign, malignant, or non-neoplastic. 19
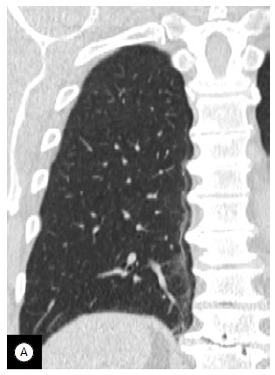
In LCS, most diffuse tracheal changes are associated with COPD, including saber-sheath trachea (Figure 2), tracheocele, and tracheomegaly (Figure 3). Solid focal lesions of the trachea do require further evaluation. 19
Figure 2. Saber-sheath trachea. In A, axial image of the proximal trachea, showing anatomical findings typical of a saber-sheath trachea (arrow). Note other morphological features of COPD (i.e., emphysema and bronchial wall thickening; white arrow). In B, 3D reconstruction showing decreased coronal diameter and increased sagittal diameter (white arrow).
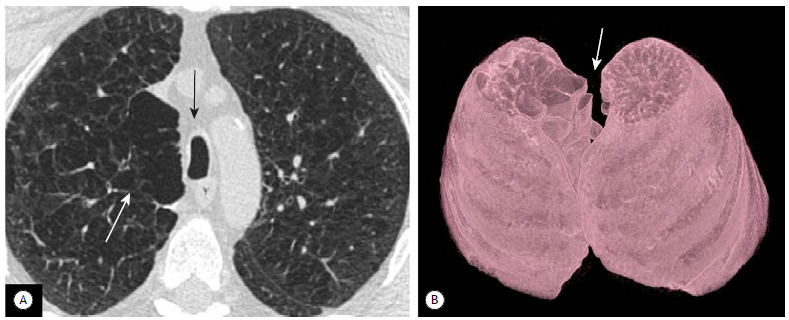
Figure 3. Airway manifestations of COPD. In A, axial image showing findings typical of pulmonary emphysema and bronchial wall thickening (arrows) in a COPD patient participating in a lung cancer screening program. In B, axial image of the right lower lobe, showing cylindrical bronchiectasis (arrows), some of which is filled with mucous plugging. In C, several subcarinal and bronchial diverticula in a heavy smoker.
Bronchial wall thickening is common among smokers and usually reflects the chronic bronchitis form of COPD (Figure 3). Reference values for bronchial wall thickness, up to the segmental bronchi, are 1.2-1.4 mm and < 20% of the internal bronchial luminal diameter. This is found on approximately 39% of LDCT scans (Figure 4A). 2
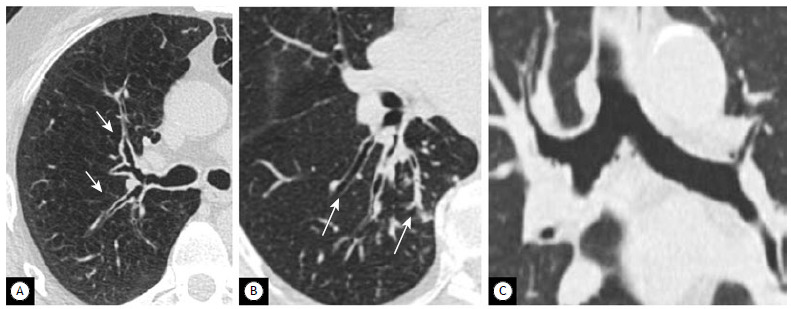
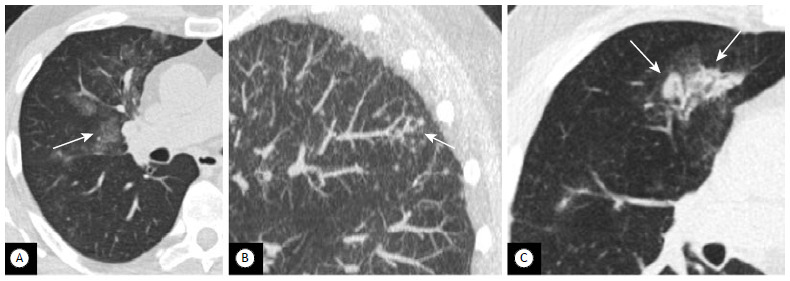
Figure 4. Interstitial lung disease. In A, axial image showing incidental findings of subpleural reticulation with honeycombing affecting the subpleural regions of the lower lobes. In B, a detail of the right lower lobe, showing traction bronchiectasis and mild honeycombing (arrows). The patient was referred for further evaluation, and the multidisciplinary team established a diagnosis of probable usual interstitial pneumonia.
Bronchiectasis is also common in LCS because of the high prevalence of smoking and COPD (Figure 3), with cylindrical bronchiectasis being the most common type. Signs of infection (e.g., mucous plugging and tree-in-bud sign) should be mentioned in the report because the patient will benefit from further respiratory evaluation. 20
Bronchial diverticula are also very common. They are mostly clinically insignificant and are not frequently reported.
Lungs
Pulmonary IFs are reported in 16-70% of LCS studies, with emphysema (Figure 5) being the most common pulmonary IF. 2 , 6 According to some authors, emphysema should be interpreted as an expected (i.e., not incidental) comorbidity related to smoking. 2 - 6
Figure 5. Osteophyte-induced lung fibrosis. Coronal image showing a line of fine fibrosis along the right paraspinal region. Progression of degenerative osteophytosis leads to compression of the adjacent lung parenchyma.
The LCS radiologist should report the type of emphysema (centrilobular, paraseptal, or panlobular) and grade its severity as trace (0.5% of a lung zone), mild (0.5-5%), moderate (45%), confluent (spanning several secondary pulmonary lobules), or advanced destructive (with hyperexpansion of secondary pulmonary lobules and architectural distortion). 21
Interstitial lung disease (ILD) is an umbrella term used for a large group of diseases of the lungs (Figure 4) and should be reported, triggering an appointment with the respiratory team/multidisciplinary team. Smoking-related ILDs include smoking-related interstitial fibrosis, idiopathic pulmonary fibrosis, desquamative interstitial pneumonia, and respiratory bronchiolitis ILD. 21
Osteophyte-induced lung fibrosis is a benign and focal form of fibrosis, seen in older patients as a localized ground-glass opacity, linear atelectasis, or a reticular pattern adjacent to osteoarthritic protrusions or spinal osteophytes, and does not appear to progress. Osteophyte-induced lung fibrosis should not be confused with ILD (Figure 5), especially usual interstitial pneumonia, which has a similar appearance but basilar predominance and is not restricted to a paraspinal location. 22
Pulmonary infection has also been reported as an IF on LCS in approximately 6% of patients. Ground-glass opacities, consolidations, and tree-in-bud opacities (Figure 6) are nonspecific CT findings of infection and should be reported, prompting further clinical and laboratory evaluation. 21
Figure 6. Pulmonary infection. In A, axial image of the right middle lobe, showing focal areas of ground-glass attenuation (arrow) with ill-defined nodularity. In B, a tree-in-bud pattern (arrow). The patient had clinically and microbiologically confirmed pneumonia. In C, axial image of a different patient, showing consolidation with air bronchogram in a predominantly peribronchovascular distribution (arrow). The patient was clinically diagnosed with bronchopneumonia.
Atelectasis is another common IF on LCS. If it is linear and is not associated with a suspicious obstructive lesion, it is usually benign and does not require further evaluation. 21
Intrapulmonary lymph nodes are common, benign findings within the lung parenchyma, with a prevalence of up to 66%, and do not require further evaluation, as per the recommendations of the British Thoracic Society, Fleischner Society, and ACR. 23 , 24 The morphological criteria for intrapulmonary lymph nodes are well-defined, noncalcified solid nodules with homogeneous, smooth margins and an oval, lentiform, or triangular shape, < 12 mm in diameter and located in the middle or lower lobes.
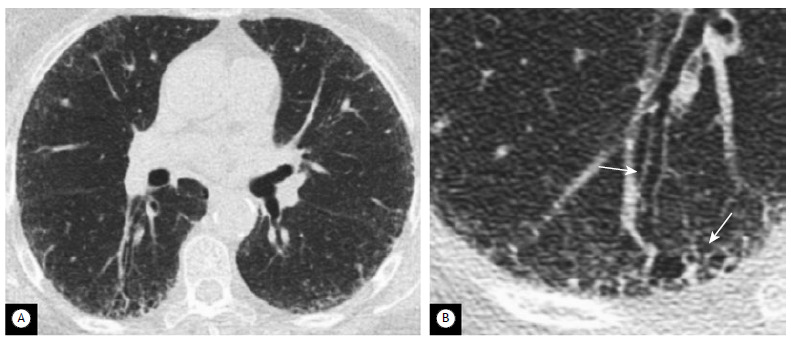
Pleura
The most common pleural IFs on LCS are pleural plaques (3.8%) and pleural effusion (1.2%). Pleural effusion may be due to benign conditions such as infection, pulmonary edema, autoimmune disease, and cardiovascular disease, but could also be a manifestation of primary or secondary malignancy and should always be reported and investigated. Pleural plaques are a marker of asbestos exposure (Figure 7). Pleural plaques should always be reported because there are important medical and legal implications to consider, and the patient should be referred to a respiratory specialist. 17
Figure 7. Pleural plaques. In A, axial image with bone window settings, showing several linear calcifications in the costal pleura (arrows). In B, 3D reconstruction of the same patient, showing that the pleural plaques are also affecting the mediastinal pleura and the diaphragmatic pleura.
Pneumothorax is uncommon as an IF on LCS but should be treated as a medical emergency and mentioned in the report, triggering an emergency referral and activation of alert systems in place. 21
Heart
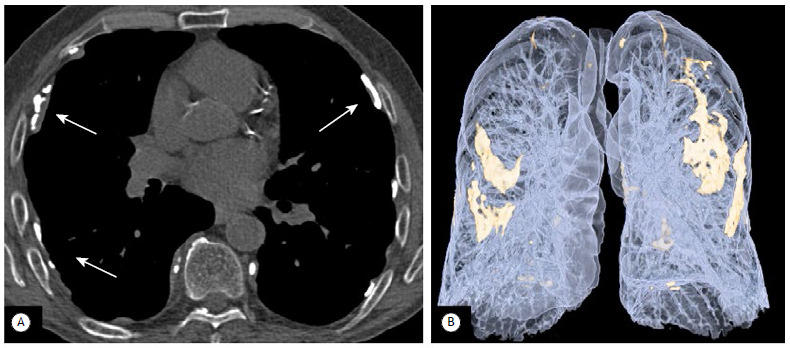
Cardiovascular IFs on LCS are common, with some studies reporting coronary calcifications on 30-56% of LDCT scans and aortic valve calcifications on 21%. 2 , 3
Smoking is a common risk factor for lung cancer and cardiovascular disease, and, as such, cardiovascular IFs on LCS should be considered smoking-related comorbidities. The risk of death from ischemic heart disease is estimated to be 3 times greater in current smokers in the 55- to 74-year age bracket than in nonsmokers. 17
Coronary artery calcium (CAC) is highly correlated with plaque burden in coronary artery disease, and a CAC score of 1,000 is associated with a 10-fold increased risk of all-cause mortality. Recent studies on CAC and LCS have shown that LDCT can be used for low-cost, noninvasive parallel evaluation of cardiovascular risk in lung screening cohorts. 23 - 26 Some LCS software programs include identification and quantification of coronary artery calcifications (mild, moderate, or severe; Figure 8), and, in our experience, they should be reported because patients benefit from cardiovascular risk assessment and possible intervention. 17
Figure 8. Coronary artery calcifications. In A, axial low-dose CT image showing mild scattered calcified plaques in the proximal left anterior descending coronary artery, findings that should be reported as mild calcifications of the coronary arteries (arrow). In B, severe calcifications of the coronary arteries with heavily calcified plaques distributed along the proximal and mid left anterior descending coronary artery, findings that should be reported as severe calcifications of the coronary arteries (arrow).
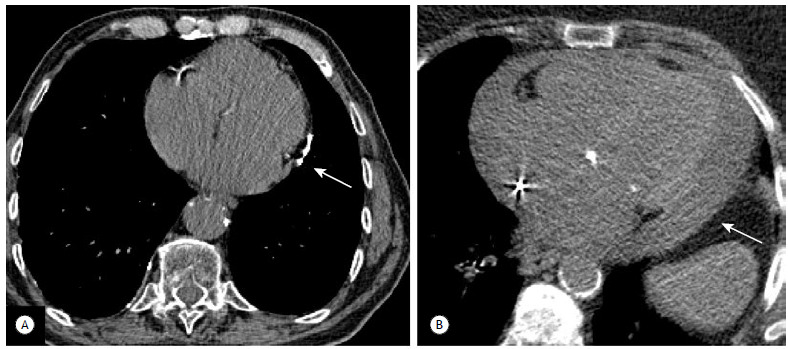
Pericardium
According to the ACR, 9 incidental pericardial findings include effusion, thickened pericardial layers, pericardial calcification (Figure 9A), and pericardial cysts. Small pericardial effusions are common and usually require no further workup, but large-volume effusions (Figure 9B) and thickening (> 3-4 mm) of pericardial layers should be reported and trigger further clinical evaluation. Pericardial cysts are the most common benign pericardial masses, presenting with thin walls and located at the cardiophrenic angles. Low-attenuation cysts do not require follow-up, unless they are large enough to risk compression of adjacent structures. 9
Figure 9. Pericardial effusion and calcifications. In A, axial image showing linear pericardial calcification (arrow), a finding that is likely related to a previous episode of pericarditis. In B, axial image showing a significant pericardial effusion (arrow). A review of the medical records showed that the patient had heart failure, with recent episodes of cardiac decompensation. The pericardial effusion was mentioned and triggered an alert to the cardiac team.
Esophagus
Evaluation of the esophagus on an unenhanced scan is limited, but significant luminal dilation should be reported and could be a sign of achalasia, scleroderma, or other inflammatory conditions. Diffuse esophageal wall thickening is seen in infectious or inflammatory conditions. Although not a common IF on LCS, focal lesions of the esophagus should be reported and trigger further diagnostic workup because smoking is a risk factor for esophageal cancer. 27
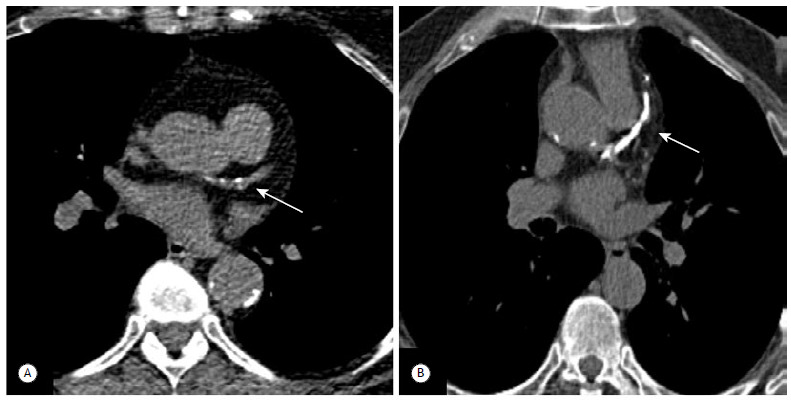
Mediastinum
Mediastinal masses are an uncommon IF on LCS, with a reported prevalence of only 0.77% in high-risk smokers. 17 The most common mediastinal masses are anterior mediastinal masses originating from the thymus or thyroid gland. Masses in the posterior mediastinum are likely neurogenic in origin and should be further evaluated by magnetic resonance imaging. 27 When a mediastinal mass is present, location, texture, and invasive behavior should be reported and the patient should be referred for further evaluation. 9 , 17 , 27
Mediastinal lymph nodes are a common normal finding on chest CT scans. Lymphadenopathy is frequently due to infection, edema, diffuse lung disease (e.g., sarcoidosis and fibrosis), and, less commonly, lymphoma or metastases. According to the ACR, incidentally detected lymph nodes of < 15 mm in short-axis diameter in patients with no other findings do not require further evaluation. 9
Pneumomediastinum is not a common IF on LCS but is a medical emergency and requires immediate action from the radiologist, with emergency referral and activation of alert systems in place.
Vessels
Aortic disease is a common IF on LCS, with dilation of the aorta being reported in up to 8.1% of LCS studies. 2 , 17 Aortic dissection and significant ulcerations are usually undetectable on LDCT given its unenhanced nature. 9
According to the ACR, the diameter of the aorta is influenced by sex, age, and body surface area. 9 The criteria for aortic aneurysm are more than 5 cm for the ascending aorta and more than 4 cm for the descending aorta. This should be reported, and the patient should be referred to a vascular specialist for further evaluation.
Pulmonary artery dilation has not been studied in the context of LCS but should be reported because an enlargement may reflect primary or secondary pulmonary arterial hypertension or be secondary to chronic pulmonary embolism or other pulmonary disease. 9 The criterion for a dilated main pulmonary artery is 3 cm or more in diameter, or equal in diameter to the ascending aorta.
Diaphragm
Diaphragmatic hernias can be either intrapleural (Bochdalek hernias) or mediastinal, the latter further divided into prevascular (Morgagni-Larrey hernias) or visceral (pericardial or hiatal hernias). Hiatal hernia is the most common transdiaphragmatic IF on LCS, being reported in 9-14% of patients. 2 , 28
Most hiatal hernias are not significant but should be reported if they are large enough to cause cardiac compression. Diaphragmatic paralysis from phrenic nerve injury results in an asymmetric position of the diaphragmatic dome and does not need any special mention in the report.
ABDOMINAL CAVITY
A systematic review of the included upper abdomen is mandatory to exclude potentially significant clinical findings (e.g., malignancy) requiring urgent referral (Table 2). The ACR white papers on incidental abdominal findings provide useful guidance for lesions requiring further follow-up. 11 - 14
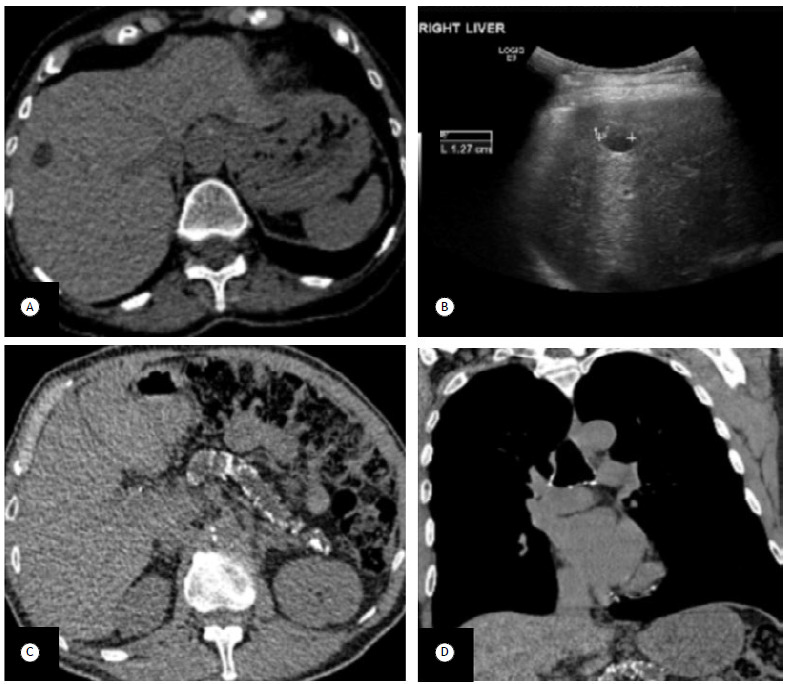
Liver
The most commonly encountered benign hepatic lesions are hepatic cysts, hemangiomas, and focal nodular hyperplasia, usually seen on LDCT scans as a focal hypodense lesion. 12
In a recent study of IFs on LCS, hepatic cysts were present in 34% of patients (Figure 10A) and are of little or no clinical significance. 28 The need for further characterization of focal liver lesions other than simple cysts is based on patient risk profile and lesion size, with known malignancy (primary liver cancer or other primary malignancy known to metastasize to the liver), hepatic dysfunction, and hepatic risk factors being taken into consideration. 12
Figure 10. Incidental abdominal findings. In A, axial image showing a focal hypodense liver lesion of 13 mm. Density was found to be inaccurately measured by low-dose CT. This was mentioned in the report, and the medical team decided to request an ultrasound scan. In B, ultrasound scan showing the benign features of a cyst. In C and D, axial and sagittal images of a different patient, showing another incidental finding, i.e., several coarse calcifications in the atrophic pancreatic parenchyma, with dilated pancreatic duct, in keeping with chronic pancreatitis. Pancreatic disease is not commonly depicted on low-dose CT scans for lung cancer screening, because low-dose CT has reduced sensitivity for pancreatic lesions and because the usual field of view does not cover the pancreas.
Gallbladder
The gallbladder does not always appear in its entirety on LCS scans depending on the field of view, patient body habitus, and patient height. In our experience, the most common findings are gallstones, with no further complications.
Pancreas, stomach, and spleen
Pancreatic IFs on LCS are reported in approximately 5% of LCS studies, including pancreatic calcifications (Figure 10B) and cancer. 2 According to the ACR, all incidental pancreatic cysts should be presumed mucinous in nature. 13 Pancreatic cysts and pancreatic solid masses should be reported and further evaluated. 13 Likewise, any gastric or splenic mass, splenic cyst, or splenomegaly should be referred for further evaluation.
Kidneys
Renal cancer has been reported as one of the most common extrapulmonary malignancies in LCS studies. 2 , 28 Any solid renal lesion should be reported and trigger further specialist evaluation and diagnostic workup (using a renal-mass CT protocol or magnetic resonance imaging study), especially if the lesion is accompanied by suspicious findings such as thick or irregular wall, mural nodule, septa, and calcification. Lesions smaller than 1 cm are likely benign, even if they are solid lesions. Well-defined homogeneous lesions smaller than 3 cm with high density (above 70 HU) can be confidently diagnosed as hyperattenuating cysts (Bosniak category II cysts) according to the ACR. 14 Simple cystic renal lesions are a common IF on routine imaging and are usually easy to recognize because of their water attenuation (0-20 HU).
Renal stones are also common findings on imaging studies. The prevalence of asymptomatic lithiasis in LCS is 10%, and renal stones are considered clinically irrelevant. 17 However, renal stones larger than 10 mm or located in the upper poles tend to be associated with an increased risk of symptoms and benefit from surgical evaluation (and should therefore be reported). If hydronephrosis is identified, it also requires further evaluation.
Adrenal glands
Non-hyperfunctioning adenomas are the most common adrenal lesions in the general population and are seen on as much as 13% of LCS scans. 28 According to the ACR, incidental adrenal lesions smaller than 1 cm in short-axis diameter, containing macroscopic fat, and with average attenuation of less than 10 HU or stable for more than 1 year should be considered benign and do not require follow-up. 11
Peritoneum
Suspicious signs of peritoneal disease, such as nodules or infiltrative masses in the peritoneal cavity, omental haziness, ascites, and peritoneal thickening, should be reported, and the patient will require referral for specialist and further diagnostic evaluation. 29
BONE/JOINTS
Incidental osseous findings on LCS include diffuse diseases such as osteoporosis, thoracic kyphosis, osteophytosis, and diffuse idiopathic skeletal hyperostosis, as well as focal lesions, both benign and malignant. 30
SKIN/SUBCUTANEOUS AND MUSCULAR SYSTEM
In one study of IFs on LCS, the presence of soft-tissue or muscular findings was very low, with incidental sebaceous cysts having only a 1% frequency, despite the fact that sarcopenia is a known smoking-related comorbidity. 28
The breast is a special soft-tissue compartment, with lesions being seen on up to 7% of LCS scans, with variable clinical significance, despite the fact that LDCT is not a good imaging modality for breast evaluation. 3 , 28 Breast IFs on LCS include primary and secondary malignancies, as well as benign lesions such as calcifications, fibroadenomas, and lipomas. Breast malignancy is the most worrying finding, and, as such, any new lesion or any lesion not previously documented as benign should be reported and referred for further evaluation.
FINAL CONSIDERATIONS
Clinically significant IFs on LCS are common, and their potential impact should be taken into consideration in the shared decision-making process. LCS programs should develop a standard approach for the evaluation of these findings.
Footnotes
Financial support: None.
REFERENCES
- 1.Kauczor HU, Baird AM, Blum TG, Bonomo L, Bostantzoglou C, Burghuber O. ESR/ERS statement paper on lung cancer screening. Eur Radiol. 2020;30(6):3277–3294. doi: 10.1007/s00330-020-06727-7. [DOI] [PubMed] [Google Scholar]
- 2.Morgan L, Choi H, Reid M, Khawaja A, Mazzone PJ. Frequency of Incidental Findings and Subsequent Evaluation in Low-Dose Computed Tomographic Scans for Lung Cancer Screening. Ann Am Thorac Soc. 2017;14(9):1450–1456. doi: 10.1513/AnnalsATS.201612-1023OC. [DOI] [PubMed] [Google Scholar]
- 3.Kucharczyk MJ, Menezes RJ, McGregor A, Paul NS, Roberts HC. Assessing the impact of incidental findings in a lung cancer screening study by using low-dose computed tomography. Can Assoc Radiol J. 2011;62(2):141–145. doi: 10.1016/j.carj.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 4.van de Wiel JC, Wang Y, Xu DM, van der Zaag-Loonen HJ, van der Jagt EJ, van Klaveren RJ, et al. Neglectable benefit of searching for incidental findings in the Dutch-Belgian lung cancer screening trial (NELSON) using low-dose multidetector CT. Eur Radiol. 2007;17(6):1474–1482. doi: 10.1007/s00330-006-0532-7. [DOI] [PubMed] [Google Scholar]
- 5.Weckbach S. Incidental Radiological Findings. Cham, Switzerland: Springer International Publishing; 2018. [DOI] [Google Scholar]
- 6.Priola AM, Priola SM, Giaj-Levra M, Basso E, Veltri A, Fava C. Clinical implications and added costs of incidental findings in an early detection study of lung cancer by using low-dose spiral computed tomography. Clin Lung Cancer. 2013;14(2):139–148. doi: 10.1016/j.cllc.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 7.Hegedüs P, von Stackelberg O, Neumann C, Selder S, Werner N, Erdmann P. How to report incidental findings from population whole-body MRI view of participants of the German National Cohort. Eur Radiol. 2019;29(11):5873–5878. doi: 10.1007/s00330-019-06077-z. [DOI] [PubMed] [Google Scholar]
- 8.European Society of Radiology ESR guidelines for the communication of urgent and unexpected findings. Insights Imaging. 2012;3(1):1–3. doi: 10.1007/s13244-011-0135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Munden RF, Carter BW, Chiles C, MacMahon H, Black WC, Ko JP. Managing Incidental Findings on Thoracic CT Mediastinal and Cardiovascular Findings. A White Paper of the ACR Incidental Findings Committee. J Am Coll Radiol. 2018;15(8):1087–1096. doi: 10.1016/j.jacr.2018.04.029. [DOI] [PubMed] [Google Scholar]
- 10.Mets OM, de Jong PA, Prokop M. Computed tomographic screening for lung cancer an opportunity to evaluate other diseases. JAMA. 2012;308(14):1433–1434. doi: 10.1001/jama.2012.12656. [DOI] [PubMed] [Google Scholar]
- 11.Mayo-Smith WW, Song JH, Boland GL, Francis IR, Israel GM, Mazzaglia PJ. Management of Incidental Adrenal Masses A White Paper of the ACR Incidental Findings Committee. J Am Coll Radiol. 2017;14(8):1038–1044. doi: 10.1016/j.jacr.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 12.Gore RM, Pickhardt PJ, Mortele KJ, Fishman EK, Horowitz JM, Fimmel CJ. Management of Incidental Liver Lesions on CT A White Paper of the ACR Incidental Findings Committee. J Am Coll Radiol. 2017;14(11):1429–1437. doi: 10.1016/j.jacr.2017.07.018. [DOI] [PubMed] [Google Scholar]
- 13.Megibow AJ, Baker ME, Morgan DE, Kamel IR, Sahani DV, Newman E. Management of Incidental Pancreatic Cysts A White Paper of the ACR Incidental Findings Committee. J Am Coll Radiol. 2017;14(7):911–923. doi: 10.1016/j.jacr.2017.03.010. [DOI] [PubMed] [Google Scholar]
- 14.Herts BR, Silverman SG, Hindman NM, Uzzo RG, Hartman RP, Israel GM. Management of the Incidental Renal Mass on CT A White Paper of the ACR Incidental Findings Committee. J Am Coll Radiol. 2018;15(2):264–273. doi: 10.1016/j.jacr.2017.04.028. [DOI] [PubMed] [Google Scholar]
- 15.Dyer SC, Bartholmai BJ, Koo CW. Implications of the updated Lung CT Screening Reporting and Data System (Lung-RADS version 1 1) for lung cancer screening. J Thorac Dis. 2020;12(11):6966–6977. doi: 10.21037/jtd-2019-cptn-02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoang JK, Langer JE, Middleton WD, Wu CC, Hammers LW, Cronan JJ. Managing incidental thyroid nodules detected on imaging white paper of the ACR Incidental Thyroid Findings Committee. J Am Coll Radiol. 2015;12(2):143–150. doi: 10.1016/j.jacr.2014.09.038. [DOI] [PubMed] [Google Scholar]
- 17.Tsai EB, Chiles C, Carter BW, Godoy MCB, Shroff GS, Munden RF. Incidental Findings on Lung Cancer Screening Significance and Management. Semin Ultrasound CT MR. 2018;39(3):273–281. doi: 10.1053/j.sult.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 18.Hoang JK, Vanka J, Ludwig BJ, Glastonbury CM. Evaluation of cervical lymph nodes in head and neck cancer with CT and MRI tips, traps, and a systematic approach. AJR Am J Roentgenol. 2013;200(1):W17–W25. doi: 10.2214/AJR.12.8960. [DOI] [PubMed] [Google Scholar]
- 19.Barnes D, Gutiérrez Chacoff J, Benegas M, Perea RJ, de Caralt TM, Ramirez J. Central airway pathology clinic features, CT findings with pathologic and virtual endoscopy correlation. Insights Imaging. 2017;8(2):255–270. doi: 10.1007/s13244-017-0545-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martínez-García MÁ, Soler-Cataluña JJ, Donat Sanz Y, Catalán Serra P, Agramunt Lerma M, Ballestín Vicente J. Factors associated with bronchiectasis in patients with COPD. Chest. 2011;140(5):1130–1137. doi: 10.1378/chest.10-1758. [DOI] [PubMed] [Google Scholar]
- 21.Chung JH, Richards JC, Koelsch TL, MacMahon H, Lynch DA. Screening for Lung Cancer Incidental Pulmonary Parenchymal Findings. AJR Am J Roentgenol. 2018;210(3):503–513. doi: 10.2214/AJR.17.19003. [DOI] [PubMed] [Google Scholar]
- 22.Salvatore M, Henschke CI, Yip R, Kaur S, Li K, Padilla M. Osteophyte induced lung fibrosis prevalence and osteophyte qualities predicting disease. Clin Imaging. 2017;44:1–4. doi: 10.1016/j.clinimag.2017.02.008. [DOI] [PubMed] [Google Scholar]
- 23.Callister ME, Baldwin DR, Akram AR, Barnard S, Cane P, Draffan J. British Thoracic Society guidelines for the investigation and management of pulmonary nodules [published correction appears in. Thorax. 2015;70(12):1188–1188. doi: 10.1136/thoraxjnl-2015-207168. [DOI] [PubMed] [Google Scholar]
- 24.MacMahon H, Naidich DP, Goo JM, Lee KS, Leung ANC, Mayo JR. Guidelines for Management of Incidental Pulmonary Nodules Detected on CT Images From the Fleischner Society 2017. Radiology. 2017;284(1):228–243. doi: 10.1148/radiol.2017161659. [DOI] [PubMed] [Google Scholar]
- 25.Chelala L, Hossain R, Kazerooni EA, Christensen JD, Dyer DS, White CS. Lung-RADS Version 1 1: Challenges and a Look Ahead, From the AJR Special Series on Radiology Reporting and Data Systems. AJR Am J Roentgenol. 2021;216(6):1411–1422. doi: 10.2214/AJR.20.24807. [DOI] [PubMed] [Google Scholar]
- 26.Gaudio C, Tanzilli A, Mei M, Moretti A, Barillà F, Varveri A. Concomitant screening of coronary artery disease and lung cancer with a new ultrafast-low-dose Computed Tomography protocol A pilot randomised trial. Sci Rep. 2019;9(1):13872–13872. doi: 10.1038/s41598-019-50407-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Henschke CI, Lee IJ, Wu N, Farooqi A, Khan A, Yankelevitz D. CT screening for lung cancer prevalence and incidence of mediastinal masses. Radiology. 2006;239(2):586–590. doi: 10.1148/radiol.2392050261. [DOI] [PubMed] [Google Scholar]
- 28.Klysik M, Lynch D, Stence N, Garg K. Incidental Non-Cardiovascular, Non-Pulmonary Findings Identified in a Low-Dose CT Lung Cancer Screening Population Prevalence and Clinical Implications. Int J Radiol Imaging Technol. 2015;1:1–1. doi: 10.23937/2572-3235.1510002. [DOI] [Google Scholar]
- 29.Cho JH, Kim SS. Peritoneal Carcinomatosis and Its Mimics Review of CT Findings for Differential Diagnosis. J Belg Soc Radiol. 2020;104(1):8–8. doi: 10.5334/jbsr.1940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buckens CF, van der Graaf Y, Verkooijen HM, Mali WP, Isgum I, Mol CP, et al. Osteoporosis markers on low-dose lung cancer screening chest computed tomography scans predict all-cause mortality. Eur Radiol. 2015;25(1):132–139. doi: 10.1007/s00330-014-3361-0. [DOI] [PubMed] [Google Scholar]


