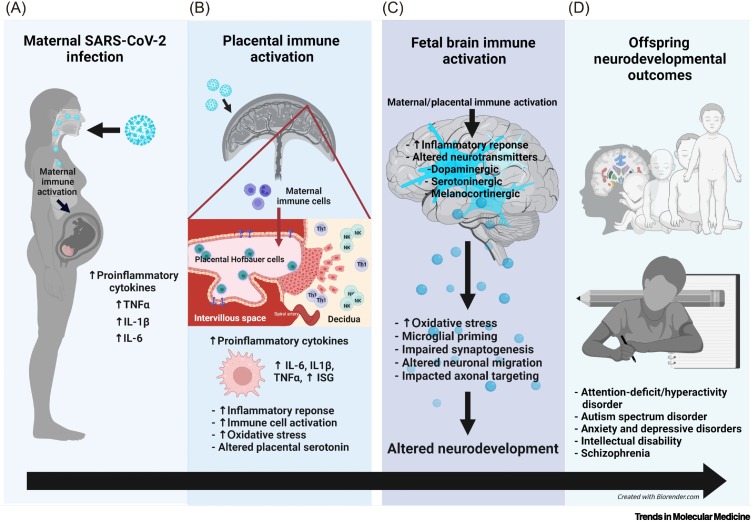
Figure 1.
Coronavirus disease 2019 (COVID-19) in pregnancy and implications for offspring neurodevelopment.
(A) Maternal severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection results in maternal immune activation (MIA) and increased proinflammatory cytokines in the maternal periphery. (B) Maternal SARS-CoV-2 infection can impact the placenta via two mechanisms: (i) placental immune activation and inflammation resulting from MIA (likely most common) or (ii) direct placental infection with SARS-CoV-2 (rare per the current literature). Placental immune activation and inflammation are associated with placental Hofbauer cell activation or priming, increased natural killer (NK) and T-helper 1 (Th1) cells at the maternal–fetal interface, increased proinflammatory cytokine production, upregulation of interferon-stimulated genes (ISGs), placental serotonin dysregulation, and increased oxidative stress. When direct placental infection with SARS-CoV-2 occurs (which is rare with the ancestral and other pre-Delta strains), the syncytiotrophoblast and cytotrophoblast layers are most commonly infected, and once the virus gains access to the intervillous space, it can theoretically gain access to the fetal circulation. (C) Both MIA and placental immune activation can lead to fetal brain immune activation, inflammation, and altered neurotransmitter signaling, including the serotonergic, dopaminergic, melanocortinergic, GABAergic, and glutamatergic systems. Fetal brain immune responses are associated with microglial priming, altered neural progenitor cell proliferation, impaired neuronal migration, synaptogenesis, and axonal targeting, all of which can result in altered offspring neurodevelopment. (D) Offspring affected by MIA are at increased risk for attention hyperactivity deficit disorder, autism spectrum disorder, anxiety, depression, impaired cognition, learning disabilities, and schizophrenia.