Figure 4. Serial brain MRIs from Patient 14 who had stable disease for 5 months.
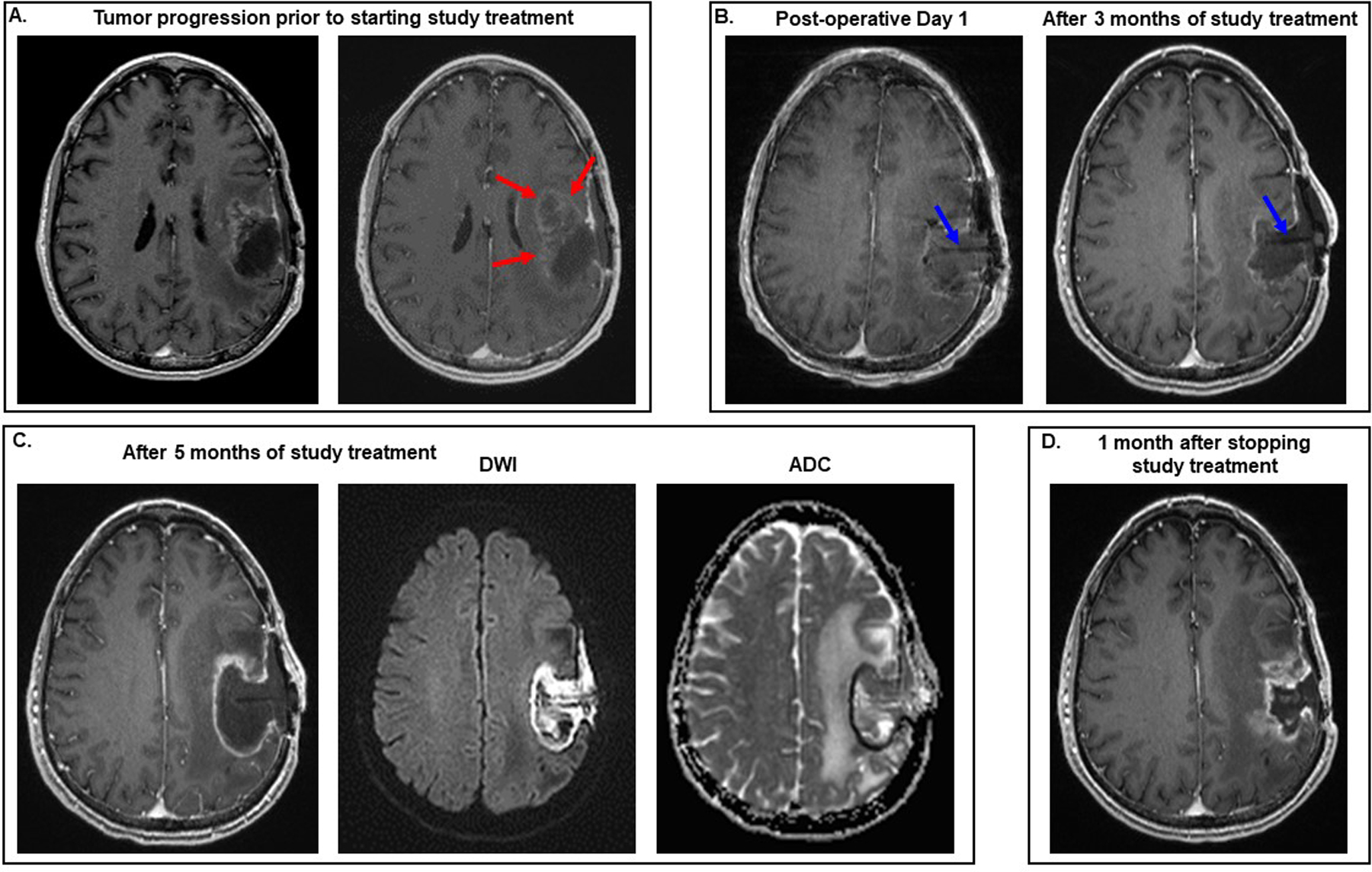
All images are T1 post-contrast except where indicated in the figure. (A) Prior to participating in the study, the patient was being treated with bevacizumab and alternating electric fields. The MRI on the right, which was performed 6 weeks later than the one on the left, documents that he developed tumor progression on this combination therapy, as evidenced by the increase in heterogeneous enhancement antero-medial to the surgical cavity (red arrows). (B) He underwent gross total resection of the recurrent tumor and started study therapy. No radiographic evidence of tumor growth was seen after 3 months of treatment with the CD-NSCs and 5-FU/leucovorin. Blue arrows point to the Rickham catheter seen within the surgical cavity. (C) His brain MRI performed approximately 5 months after the start of study treatment showed increase in the size of the surgical cavity and rim enhancement on the T1 post-contrast image. However, the rim and contents of the surgical cavity were bright on the diffusion weighted image (DWI) and dark on the apparent diffusion coefficient (ADC) image, indicating restricted diffusion. These imaging findings suggested that the changes in the surgical cavity and its contents on the T1 post-contrast image were due to the presence of a brain abscess rather than tumor progression. Aspiration of the Rickham reservoir revealed the presence of purulent fluid, and the patient then underwent surgery to drain the abscess. Biopsies of the surgical cavity obtained during this surgery showed no definite evidence of tumor regrowth. (D) MRI of his brain performed approximately 1 month after the surgery showed new enhancement at the surgical site consistent with tumor progression, which was then confirmed histopathologically by the presence of sheets of neoplastic cells with nuclear anaplasia associated with prominent microvasculature when another craniotomy was performed a week later.
