Abstract
Background
We performed a meta-analysis of randomized controlled trials (RCTs) assessing the effect of Aquatic High Intensity Interval Training (AHIIT) on cardiometabolic and physical health markers in women.
Methods
Systematic search used 7 databases (MEDLINE, PubMed, SPORTDiscus, Cochrane, Embase, CINAL complete, PsycINFO). The Physiotherapy Evidence Database (PEDro) score was used to evaluate the methodological quality of the studies. Clinical trials compared AHIIT with a control group that receive no exercise training. We integrated randomized controlled trials published in English, and participants were women aged ≥18 years. The outcome of interest was the change in cardiometabolic and physical health markers.
Results
Among 242 articles screened, 18 articles (13 trials) were included in this meta-analysis comparing AHIIT (n = 261) with a control group (n = 215). The median PEDro score was 5.5 out of 10 (range, 4–8). AHIIT significantly improved peak oxygen uptake (Hedges' g 0.610; 95% CI 0.277–0.943; P < 0.001), reduced resting heart rate (Hedges' g −0.495; 95% CI -0.866 to −0.124; P < 0.05), as well as chair to stand test. (Hedges’ g 0.548; 95% CI 0.019 to 1.077; P < 0.05).
Conclusion
AHIIT has a moderate effect in improving cardiometabolic and physical health markers in women.
Keywords: Aquatic high intensity interval exercise, Cardiometabolic health, Meta-analysis, Physical health, Women
1. Introduction
Cardiometabolic health is an important issue to address. Identifying cardiometabolic risk (CMR) factors, mortality, morbidity, and disability can reduce 73% of all deaths and 60% of the global health burden.1,2 Globally, more than a quarter of the world's adult population (1.4 billion adults) is insufficiently active.3 The association between physical inactivity and increased mortality appears with a reduction in cardiometabolic health.4 Thus, identifying and reducing modifiable CMR factors—namely, physical inactivity—will have an essential effect on diseases that would otherwise raise enormous public or health concerns.
Women are relatively less physically active than men. Among adults aged 18 years or older, 31.7% of women and 23.4% of men fail to achieve physical activities up to or exceeding the WHO recommended level of at least 600 metabolic equivalent (MET) minutes weekly.5 In addition, women have a higher prevalence of lower limb osteoarthritis and obesity; women over 45 years old were found to be much more obese than the rest of the population, with a body mass index (BMI) surpassing 25 kg/m2 in 47% of them and surpassing 30 kg/m2 in 9% of them.6,7 Recent public health promotions have highlighted interval training as an alternative exercise strategy that has gained popularity among the general population.8 High-intensity interval training (HIIT), for example, has numerous significant health benefits for cardiometabolic and physical health.9 Performing HIIT in an aquatic environment (AHIIT) can be an alternative to land-based HIIT. AHIIT has emerged for individuals who may be more likely to incorporate HIIT into their lifestyles while immersed in an aquatic environment.10 It offers a great option for cardiometabolic and physical training. Those who have participated in AHIIT studies were predominantly women; hence our review focused on female populations who are believed to have a higher CMR.11,12
Lack of time is a commonly cited reason for people failing to participate continuously in a traditional exercise program; it thus restricts physical activities. HIIT is focused on the inverse relationship between intensity and duration of training.13 Therefore, interspersing intervals of high levels of exercise with periods of rest or low to moderate levels of exercise can be a more time-efficient and effective option for physical activity than continuous training.10,13, 14, 15 AHIIT is considered to be effective because many physiological benefits are related to the physical properties of water.16 Water buoyancy reduces discomfort and stress placed on the joints. In addition, the hydrodynamic nature of water acts as a form of resistance to movements, optimising the development of muscle strength.17,18 With this water cushioning effect, AHIIT can be a safe option for many, as it minimises some of the hindrances to exercise associated with land-based training, such as pain, fear of movement, and balance.19
There is well-established evidence about the effects of HIIT on cardiometabolic or physical health, while similar evidence regarding AHIIT is lacking.14 To the best of our knowledge, one systematic review has been conducted on the effects of AHIIT. However, the outcome measures concerned aerobic capacity, muscle strength, and body composition.12 Evidence regarding other cardiometabolic health markers, including lipid profile, blood pressure, and bone mineral density (BMD), is lacking. Given this knowledge gap and lack of evidence, alongside the growing application of AHIIT, the objective of this study is to investigate the effects of AHIIT on the improvement of cardiometabolic and physical health markers in women.
2. Methods
A complete search of randomised controlled trials was performed up to January 2021. The reporting in this study adheres to the preferred reporting items for systematic reviews and meta-analysis guidelines (PRISMA).20 This review protocol was registered in the PROSPERO database of systematic reviews (CRD42021229631).
2.1. Study selection
Two reviewers (MK and BS) screened the titles and abstracts of the articles. The reviewers independently reviewed the full texts of the articles and agreed on their eligibility for inclusion in the review. If disagreement occurred, a third reviewer (SN) resolved any discrepancies between the two reviewers or the article was removed from the review.
2.2. Search strategies
An exhaustive search of the literature was conducted to identify publications related to the effectiveness of AHIIT. Articles were retrieved from seven electronic bibliographic databases: MEDLINE, CINAHL, PubMed, SPORTDiscus, PsycINFO, Embase, and Cochrane Library. The search strategy comprised the following medical subject headings (MeSH) or keywords: (1) aquatic exercise, aquatic or water exercise, hydrotherapy, water immersion, or head-out aquatics; (2) high-intensity interval training, intermittent exercise, or interval training; (3) cardiometabolic health, cardiorespiratory or metabolic markers, physical, or physical health; and (4) women or female. An example of the search strategy can be found in Appendix A.
2.3. Inclusion criteria
The articles included were based on the following criteria: 1) All participants must be women who were ≥18 years old; 2) the studies were published in full and were written in English; 3) the articles included must be randomised control trials; 4) the outcome measures must include cardiometabolic or physical health markers; and 5) head-out aquatic exercise was assessed. For the intervention to be considered high intensity, the work rate prescribed needed to elicit: i) maximal oxygen capacity (VO2 max) > 75%]; ii) HRmax >80–95%; and iii) rate of perceived exertion (RPE) of 15 or more on the BORG exertion scale. The definitions used in the present review are based on a general classification scheme for interval training suggested by Weston and colleagues.15 Control groups included were defined as not receiving exercise training.
2.4. Exclusion criteria
The studies were excluded if: 1) the participants were men; 2) the intervention was conducted for less than two weeks (the minimum time requirement to observe meaningful physiological changes in interval training); or 3) the intervention was not interval training.
2.5. Outcome measures
The outcome measures for this study were cardiometabolic and physical health markers. Cardiometabolic health markers include peak oxygen uptake (VO2 peak), resting heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), body fat percentage, high-density lipoprotein (HDL), and low-density lipoprotein (LDL). In addition, bone mineral density (BMD), knee flexion and extension strength, and the chair to stand (CS) test were the physical health markers measured.
2.6. Quality assessment
Two authors (MK and BS) independently graded the quality of the included studies using the Physiotherapy Evidence Database (PEDro) scale.18 Items related to internal validity and quality of reporting were scored across 10 criteria; “yes” was given a score of one and “no” a score of zero. When data were unavailable or unclear, the item was assigned a score of zero. Reliability and validity for the PEDro scale have been established.19
2.7. Data extraction
Two authors (MK and BS) independently extracted data regarding the methodology and outcome measures using a standardised data extraction sheet.
2.8. Meta-analysis
A further meta-analysis was carried out using comprehensive meta-analysis software (Version 3.0; Biostat, Englewood, NJ). The mean value and standard deviation of each study were inputted into the software. If the values were not available, the authors were contacted by email to obtain the raw data. If no raw data were available, the study was excluded from the meta-analysis. A random-effects model was used to estimate the distribution of observed effect sizes.
2.9. Effect size
The effect size in terms of Hedges' g and its 95% confidence interval (CI) was computed in all meta-analyses as various methods between trials assessed cardiometabolic and physical health markers. Hedges' g is a variation of Cohen's d, which corrects for a possible bias in small sample sizes.21 Effect size was quantified as large (>0.8), medium (0.5–0.8), small (0.2–0.5), or non-significant (<0.2) as a general rule of thumb, as suggested by Cohen (1988).
2.10. Publication bias
Egger's regression asymmetry test was performed to assess the existence of publication bias. A P-value of <0.1 (two-tailed test) indicated the presence of publication bias.22
3. Results
3.1. Study selection
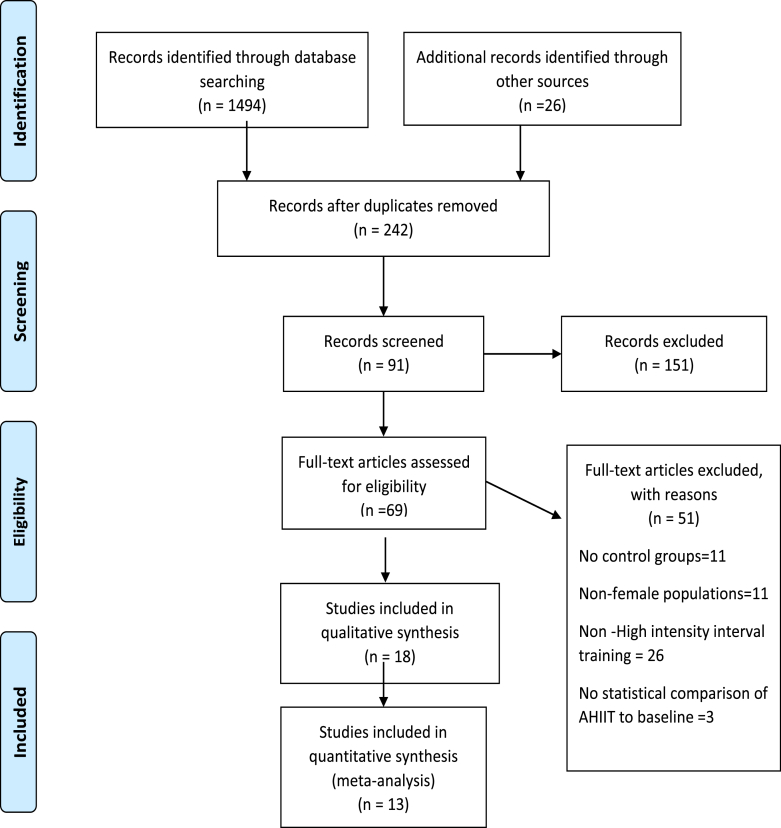
The review search identified 1520 articles published between 1994 and January 2021, of which 1278 articles were excluded because they were not relevant to the scope of this review or were duplicates. Out of the remaining 242 articles, 151 were excluded when the abstracts were reviewed, and 51 articles were excluded after reading the full texts. A total of 18 articles were ultimately identified as being relevant to the study6,23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39; 13 of these articles were included in the final analysis (Fig. 1).
Fig. 1.
PRISMA flow diagram.
3.2. Study characteristics
Descriptions of the participants and outcomes of the studies are summarised in Appendix B. All of the included studies employed AHIIT as an intervention. The characteristics of the interventions are summarised in Table 1.
Table 1.
Characteristics of Aquatic High Intensity Interval training.
| Author | Type of water training | Characteristics of AHIIT intervention |
Pool (Type & temperature) | Depth (immersion level) | Description of AHIIT (work-rest ratio) | High intensity measurement | Adverse events recorded | ||
|---|---|---|---|---|---|---|---|---|---|
| Times per week | Number of weeks | Time for each session (min) | |||||||
| L. S. Andrade et al., 2020a | Water based exercise program (stationary running, frontal kick and cross-country skiing) | 2 | 12 | 44 | Pool of a sports club linked to university of water temp 30 °C −32 °C, | Between xiphoid process and shoulder | 2min-2min | RPE 17.3–18.9 corresponds to 80–89% VO2 peak | Nil |
| L. S. Andrade et al., 2020b | Water based exercise program (stationary running, frontal kick and cross-country skiing) | 2 | 12 | 44 | Pool of a sports club linked to university of water temp 30 °C −32 °C, | Between xiphoid process and shoulder | 2min-2min | RPE 17.3–18.9 corresponds to 80–89% VO2 peak | Nil |
| Bento et al., 2014 | 1. Upper and lower limbs water aerobic exercise 2. Strengthening lower limb muscles using aquatic resistance devices |
3 | 12 | 60 | Indoor swimming pool of water temp 28 °C −30 °C | Xyphoid process | 1.40s-20s 2.2–3 sets of exercise with 8–12 RM and 2 min rest |
Exercises executed without the feet contacting the bottom of the pool to increase the exercise intensity | NR |
| Broman et al., 2006 | Deep water running with vest | 2 | 8 | 48 | 27 °C | Shoulder level | 10min-2min | >75% maximal HR | Nil |
| Connolly et al., 2016 | All out free style swimming (front crawl) | 3 | 15 | 15–25 | NR | Head out swim | 30s-2min | Mean HR and peak HR are 86 ± 3 and 96 ± 1% HR max in high intensity interval group | Nil |
| Costa et al., 2018 | Water aerobic exercises (9 upper limbs and lower limbs exercises) | 2 | 12 | 45 | Swimming pool of the university | Xiphoid process | NR | BORG 15 | NR |
| Aboarrage Junior et al., 2018 | Jump based aquatic exercise program | 3 | 24 | 30 | Aquatic centre of pool temp 29 °C | Xiphoid process | 30s-30s | All-out intensity, self-selected maximal intensity | Nil |
| Junior et al., 2018 | Aquatic exercises (a) jumping jacks (b) horizontal adduction and abduction of the shoulder; (c) stationary running with knee | NR | NR | 45 | Pool temp 29 °C | Xiphoid process | 30s-1min | 60–89% HRR (Vigorous intensity) | Nil |
| Mohr et al., 2015 | All out free style swimming (front crawl) | 2.9 (0.1) | 15 | 15–25 | NR | Head out swim | 30s-2min | Mean HR and peak HR are 86 ± 3 and 96 ± 1% HR max in high intensity interval training group | Nil |
| Mohr et al., 2014 | High Intensity Sprint swimming | 2.9 (0.5) | 15 | 15–25 | NR | Head out swim | 30s-120s | Mean HR and peak HR are 86 ± 3 and 96 ± 1% HR max in high intensity interval training group | Nil |
| Moreira et al., 2014 | Strength and power exercise and aquatic cardiorespiratory training | 3 | 24 | 50–60 | Covered swimming pool, with water temp 30-31 °C | Water depths 1.1–1.3 m | 1. Two sets of 30s each 2. Three sets of 20 s each, 3. Four sets of 15 s each, 4. 5 sets of 10s each |
1. 60% HR max in 16 min of session 5–9, 2. 70% HR max in 13 min of session in weeks 10–14, 3. 80% HR max in 9 min session in weeks 15–19, 4. 90% HR max in 7 min session in weeks 20–24, |
Nil |
| Moreira et al., 2013 | Strength and power exercise and aquatic cardiorespiratory training | 3 | 24 | 50–60 | Covered swimming pool, with water temp 30-31 °C | Water depths 1.1–1.3 m | 1. Two sets of 30s each 2. Three sets of 20 s each, 3. Four sets of 15 s each, 4. 5 sets of 10s each |
1. 60% HR max in 16 min of session 5–9, 2. 70% HR max in 13 min of session in weeks 10–14, 3. 80% HR max in 9 min session in weeks 15–19, 4. 90% HR max in 7 min session in weeks 20–24, |
Nil |
| Munukka et al., 2019 | Lower limbs aquatic resistance training | 2.6(0.5) | 16 | 60 | Heated pool, 30-32 °C | NR | 2 sets × 30 reps to 3 sets x 30–45 reps, with rest period 30–45s | -Average Intensity of each session RPE 15 (12–17), HRmax 144 (12) bpm -Intensity of training set at "as hard and fast as possible |
-Two medical consultations (bilateral knee pain and dyspnoea) after training |
| Munukka et al., 2016 | Lower limbs aquatic resistance training | 2.6(0.5) | 16 | 60 | Heated pool, 30-32 °C | NR | 2 sets × 30 reps to 3 sets x 30–45 reps, with rest period 30–45s | -Average Intensity of each session RPE 15 (12–17), Max HR144 (12) bpm -Intensity of training set at "as hard and fast as possible |
-Two medical consultations (bilateral knee pain and dyspnoea) after training |
| Nordsborg et al., 2015 | All out free style swimming (front crawl) | 3 | 15 | 15–25 | NR | Head out swim | 30s-2min | Mean HR and peak HR are 86 ± 3 and 96 ± 1% HR max in high intensity interval training group | Nil |
| Ryzkova et al., 2018 | Aqua-fitness program: HIIT program | 2 | 10 | 50 | Pool at the university of water-temperature of 28 °C | Central chest area up to shoulder | 20s-10s | High intensity training zone >80% HR reserve | NR |
| Samadi et al., 2019 | AHIIT training (20 min, quick movements of body) | 3 | 12 | 30 | NR | NR | 20s-10s | 80–95% HR max | NR |
| Waller et al., 2017 | Lower limbs aquatic resistance training | 2.6 (0.5) | 16 | 60 | Heated pool, 30-32 °C | NR | 2 sets × 30 reps to 3 sets x 30–45 reps, with rest period 30–45 s in between sets | -Average Intensity of each session RPE 15 (12–17), HR max144 (12) bpm -Intensity of training set at "as hard and fast as possible" |
-Two medical consultations (bilateral knee pain and dyspnoea) after training |
BORG, Borg scale of perceived exertion; bpm, beats per minute; HIIT, High Intensity Interval Training; HR, heart rate; HRmax, maximal heart rate; Min, minute; NR, not recorded; temp, temperature; RPE, rate of perceived exertion; reps, repetitions; s, second.
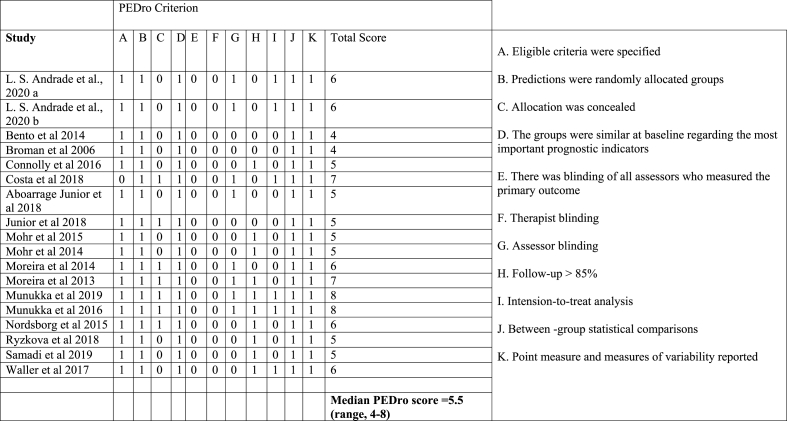
3.3. Quality assessment
Quality assessment of all the studies achieved a moderate quality median PEDro score of 5.5 out of 10 for all papers; the highest score was eight34,35 and the lowest was four24,25 (Table 2). There was no blinding of subjects in any of the studies reviewed due to the nature of intervention studies. PEDro scores of seven and above are considered high-quality studies; scores of five and six are considered to be of moderate quality; scores lower than four are considered poor quality.20 Four studies were considered high-quality, with PEDro scores of seven and above, mainly due to the intention to analyse the data.27,30,34,35 Twelve studies were of moderate quality, in which allocations were not concealed and the assessors were not blinded.6,26,28, 29, 30, 31,33,36, 37, 38, 39, 40 Two studies were of low quality, as a result of a lack of information about the follow-up procedures and blinding of assessors during the intervention.24,25
Table 2.
The PEDro score.
3.4. Effect of AHIIT on cardiometabolic health markers
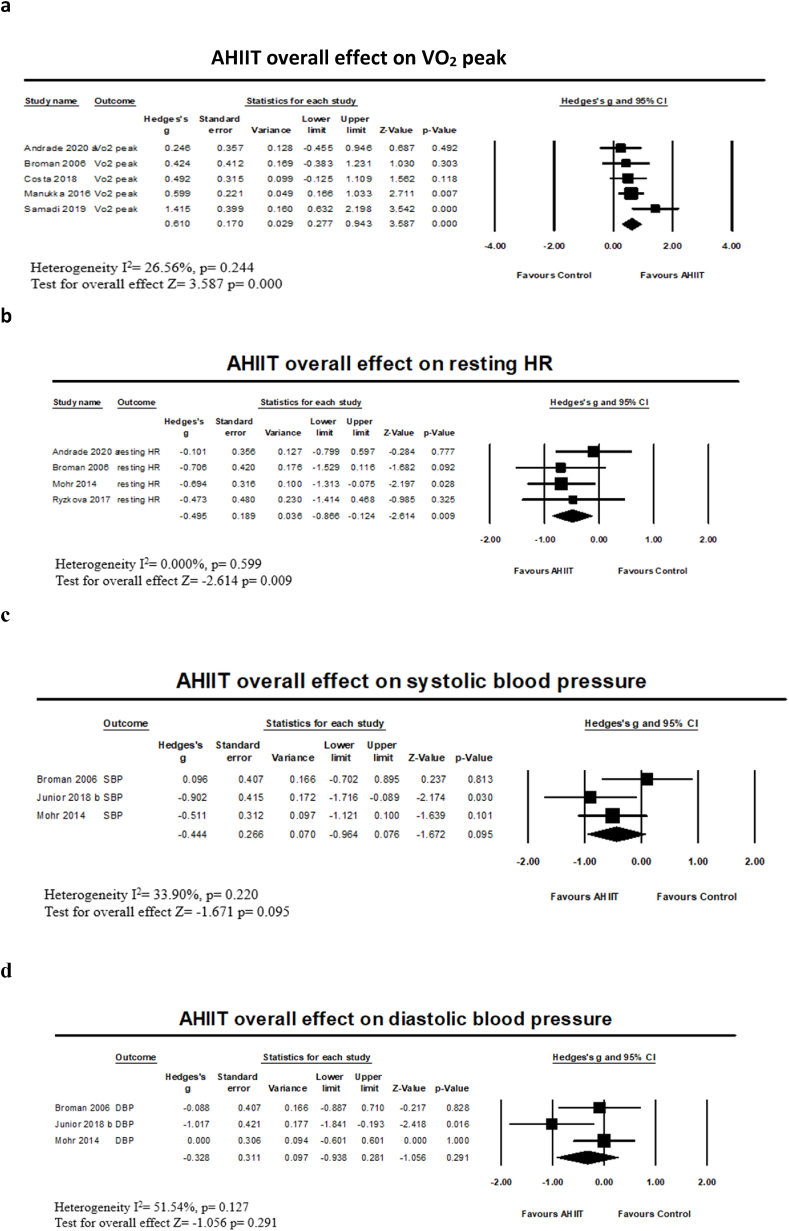
Our analysis of five studies23,24,27,34,38 revealed a significant (P < 0.001) moderate effect size point estimate of 0.610 in favour of AHIIT compared with the control for peak oxygen uptake (VO2 peak) (95% CI 0.277 to 0.943), with no significant heterogeneity found (I2 = 26.69%, P = 0.244) (Fig. 2a). Four studies23,24,31,37 indicated a significant (P = 0.009) moderate effect size point estimate of −0.495 (95% CI -0.866 to −0.124) in favour of reducing resting heart rate (HR), without significant heterogeneity across studies (I2 = 0%, P = 0.599) (Fig. 2b). However, our analysis of three studies24,28,31 on SBP and DBP indicated insignificant moderate effect size point estimates of −0.044 (95% CI -0.964 to 0.076) (P = 0.095) (I2 = 33.898%, P = 0.22) (Fig. 2c) and −0.328 (95% CI -0.938 to 0.281) (P = 0.291) (I2 = 51.539%, P = 0.127) (Fig. 2d), respectively, in favour of AHIIT, compared with the control.
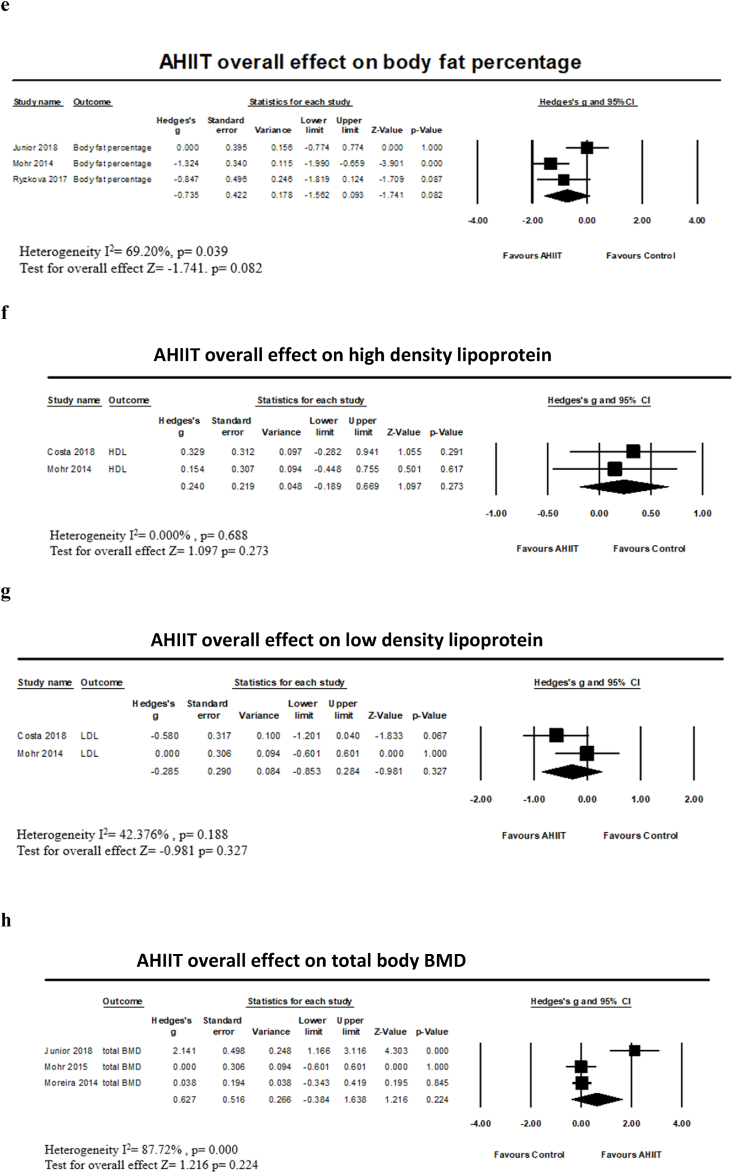
Fig. 2.
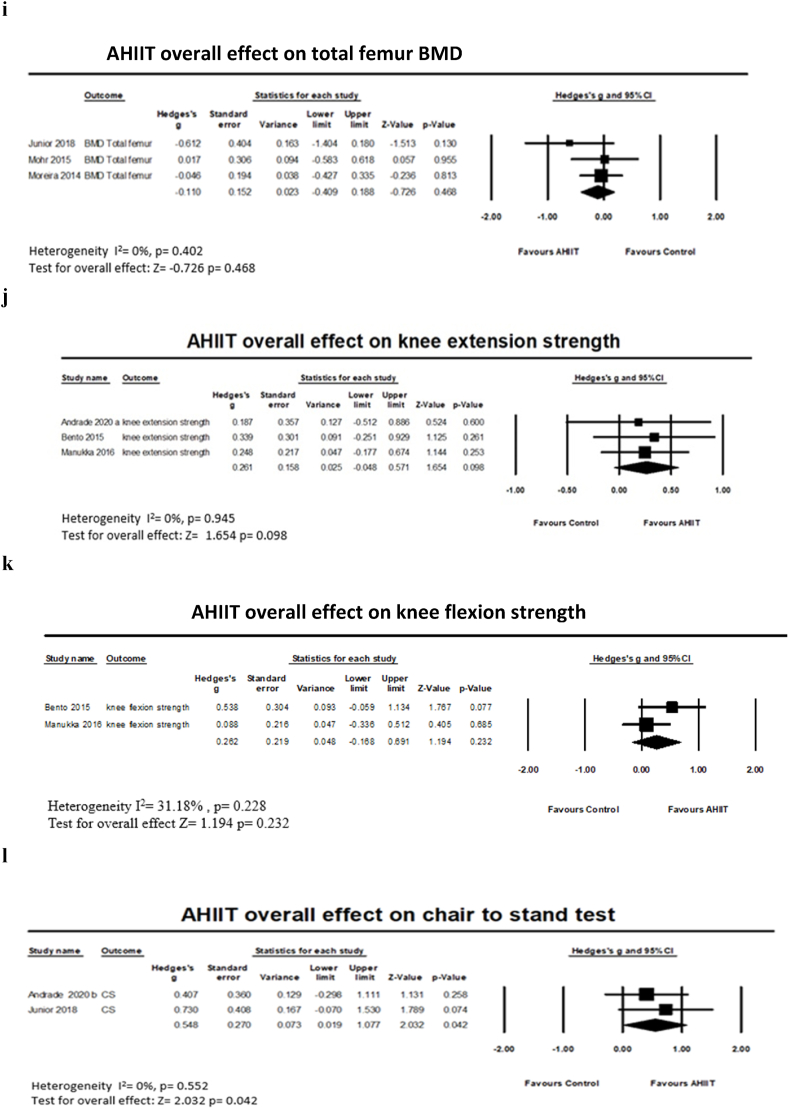
Meta-analysis and forest plots of (a) AHIIT on VO2 peak, (b) AHIIT on resting HR, (c) AHIIT on SBP, (d)AHIIT on DBP, (e) AHIIT on body fat percentage, (f) AHIIT on HDL (g) AHIIT on LDL, (h) AHIIT on total body BMD (i) AHIIT on total femur BMD, (j) AHIIT on knee extension strength (k) AHIIT on knee flexion strength and (l) AHIIT on chair to stand test.
For body fat percentage, three studies28,31,37 indicated an insignificant (P = 0.082) moderate effect size point estimate of −0.735 (95% CI -1.562 to 0.093) in favour of AHIIT compared with the control. There was significant moderate heterogeneity across studies (I2 = 69.197%, P = 0.039) (Fig. 2e). Although our analysis of two studies27,31 indicated that both blood lipid measurement regarding HDL and LDL had insignificant (P = 0.273) and small (P = 0.327) effect size point estimates of 0.240 (95% CI -0.189 to 0.669) and −0.285 (95% CI -0.853 to 0.284), respectively, there was no significant heterogeneity across studies: (I2 = 0%, P = 0.688) (Fig. 2f) and (I2 = 42.376%, P = 0.188) (Fig. 2g), respectively.
3.5. Effect of AHIIT and physical outcomes
For total body BMD and total femur BMD, our analysis of three studies28,30,31 indicated an insignificant (P = 0.224) moderate effect size point estimate of 0.627 (95% CI -0.384 to 1.638) and a small effect size point estimate of −0.110 (95% CI -0.409 to 0.188, P = 0.468) in favour of AHIIT compared with the control. There was significant large heterogeneity (I2 = 87.722%, P = 0.000) (Fig. 2h) and no significant heterogeneity across studies (I2 = 0.000%, P = 0.402) (Fig. 2i), respectively.
Our analysis of three studies23,25,34 on knee extension strength indicated an insignificant (P = 0.098) small effect size point estimate of 0.261 (95% CI -0.048 to 0.571) without significant heterogeneity across studies (I2 = 0.000%, P = 0.945) (Fig. 2j). Our analysis of two studies25,34 on knee flexion strength indicated an insignificant (P = 0.232) small effect size point estimate of 0.262 (95% CI -0.168 to 0.691) in favour of AHIIT compared with the control group. There was no significant heterogeneity across studies (I2 = 31.181%, P = 0.228) (Fig. 2k). Furthermore, our analysis of two studies6,28 on the chair to stand test indicated a significant (P = 0.042) moderate effect size point estimate of 0.548 (95% CI 0.019 to 1.077) in favour of AHIIT compared to the control group; no significant heterogeneity was found (I2 = 0%, P = 0.552) (Fig. 2l).
3.6. Publication bias
According to the results of Egger's test, no significant publication bias was observed in the meta-analysis of cardiometabolic health markers (P = 0.249) and physical outcomes (P = 0.855).
4. Discussion
To the best of our knowledge, this systematic review with meta-analysis is the first to examine the effects of AHIIT on cardiometabolic and physical health markers in women. Our main findings revealed AHIIT resulted in a moderate improvement in cardiometabolic markers in regard to VO2 peak, resting HR, and physically in the CS test.
VO2 peak is considered to be directly reflective of maximal oxygen capacity (VO2 max), the highest value of VO2 attained upon a high-intensity exercise test.41 The test of VO2 peak is designed to bring the subject to the limit of tolerance, a gold standard measure of cardiorespiratory fitness and a solid indicator that can predict mortality and improve prognosis.42 Our findings demonstrated that the VO2 peak significantly increased with a moderate effect when AHIIT was compared to control groups.23,24,27,34,38 With training, centrally, the left ventricle of the heart can stretch to allow for more forceful contractions, which increase stroke volume and result in increased VO2 peak.43 HIIT is also able to increase the VO2 peak rapidly via increasing mitochondrial density, resulting in the generation of more adenosine triphosphate (ATP) for working muscles.44 Another possible explanation is that VO2 is influenced by a restriction in chest expansion when inspiratory muscle contractions are unable to equal or overcome the force of hydrostatic pressure.43 It is suggested that central hypervolaemia influences lung volumes by reducing lung compliance and promoting gas trapping, which narrows the airways.45 With such unique physiological adaptations during aquatic training, minute ventilation and breathing frequency were significantly increased when compared with land-based training with an equivalent exercise intensity.46
Our findings also revealed an overall moderate effect in reducing resting HR in women following AHIIT, consistent with another study.47 With increased water immersion due to hydrostatic gradient, AHIIT increases stroke volume, which induces increased cardiac contractability and reduced heart rate.48 It has been proposed that the reduction of heart rate is due to an increase in parasympathetic activity and a decrease in the sympathetic activity of the heart.49 With an increase in resting HR response indicating a risk factor for all-cause mortality, a reduction in resting HR through AHIIT minimises risk factor mortality.50 Such improvements in VO2 peak and resting HR provided by AHIIT are crucial, since both are independent predictors of cardiometabolic disease, particularly cardiovascular disease mortality.51 It has been shown that every 1-MET increase in VO2 peak is associated with 10–25% improvements in survival rate and an 18% reduction in events related to cardiac-related diseases.52 Hence, improving VO2 peak and resting HR to improve cardiometabolic health can be easily achieved with the help of AHIIT.
Blood pressure is another common cardiometabolic measure. A lack of significant reduction in both SBP and DBP was observed. This lack of significance could be because the included participants in the studies were exclusively hypertensive aged women, and it is known that SBP increases progressively with age.53 Similarly, changes in lipid profile were not significant in this review. A possible reason for this result is that lipid metabolism reflects HDL and LDL levels, and depends on the concentration of other enzymes.27 Due to the limited number of review papers on lipid profile, the mechanism regarding the effect of AHIIT is still unknown.
HIIT appears to promote a significant reduction in body fat percentage in overweight men.54 Our results did not show an overall significant effect of AHIIT on body fat percentage in female populations. Likewise, there was a review that showed no overall effects on body composition utilising AHIIT among non-athletic populations.12 Despite these findings, when trained at the same relative intensity, a higher VO2 training value could be achieved in water than on land. This could potentially result in a higher caloric cost and, hence, a higher reduction in body fat percentage.55
When considering physical health markers, the hydrostatic pressure in the water created by resistance in movement at high speed promotes muscle action.56 High speeds promote the recruitment of type II fast-twitch muscle fibres.57 However, our results showed no significant difference in overall knee extension and flexion strength following AHIIT. Our results are contrary to the results of the meta-analysis conducted by Depiazzi and colleagues, but are similar to the findings of Heywood and colleagues, which showed no significant improvement in muscle strength.12,58 This discrepancy in muscle strength could result from a difference in movement speed and resistance loading exerted on the muscles. The improvement in muscle strength remains controversial at this stage and warrants further investigation.
Our results revealed no overall significant changes in total body BMD or total femur BMD. Impact or resistive exercise in an aquatic environment results in different loadings exerted on bone cells; according to Wolff's law, mechanical loading is considered to be an active osteogenic stimulus.59 Nonetheless, no significant results were found in total body BMD and total femur BMD. This finding could be explained by the level of immersion during AHIIT exercises (e.g., exercises performed at chest level associated with reduced mechanical loading on the bones).60
Our results showed a significant effect on functional improvement in the CS test despite only two studies on the CS test being included in the analysis.6,29 These studies indicate that the CS test has good test-retest reliability (R ≥ 0.8) and reasonably good criterion-related validity relative to knee extensor strength.61 Our review, however, showed a significant improvement in the CS test without a substantial improvement in knee extensor strength. This result may be because the CS test is significantly associated with the eccentric contraction of the knees, instead of the maximal dynamic strength measured.62 Given the improvement in the ability of women to perform the CS test after AHIIT, it seems to be a reliable tool with which to assess lower-body strength and performance.63 It might therefore be considered an alternative tool to determine maximal dynamic strength and potentially simulate daily living tasks, resulting in a functional gain.
Finally, data presented in this analysis indicate that AHIIT is safe for female populations in regard to safety issues. This result is consistent with other reviews, which also show a trivial number of adverse events associated with HIIT and aquatic training.15,19
4.1. Study limitations
Although the synthesised evidence in this review is encouraging, this study has several limitations. Discrepancies exist in defining high intensity across different kinds of training, using maximal oxygen uptake, and HR or RPE scales. The relatively small number of studies included in each outcome resulted in a small sample size, and limiting the sample to female populations may affect the generalisability of the results. Our literature search was also limited to databases and publications in English peer-reviewed journals. The quality of the majority of studies included is between low and moderate in terms of reporting. Although no other intervention groups were used for comparison in this study, the data of the involved studies in the present analysis were carefully and systematically assessed. Overcoming the shortcomings of this research should be considered in the design of future studies.
5. Conclusion
This is the first systematic review and meta-analysis of the overall effectiveness of AHIIT interventions in improving cardiometabolic health markers in regard to VO2 peak, resting HR, and physical outcomes in the CS test among female populations. Although AHIIT appears to be effective, future research is needed to compare AHIIT with other exercise interventions and to develop optimal AHIIT parameters to benefit cardiometabolic and physical health.
Authors' contribution
1) Manny M.Y. Kwok and Billy C.L.So have given substantial contributions to the study concept and design of the work;
2) Manny M.Y. Kwok and S.S. Man gave contributions to formal analysis and interpretation of data;
3) Manny M.Y. Kwok has drafted the manuscript, Billy C.L. So and Shamay S. M. Ng revised and edited critically for important intellectual content;
4) All authors read and approved the final version of the manuscript.
5) All authors agreed to take responsibility for all aspects of the manuscript in ensuring that research questions related to the accuracy or integrity of the manuscript were appropriately investigated and resolved.
Declaration of competing interest
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
The authors wish to express their gratitude to Dr Raymond Chung, PhD, for his contributions as scientific advisor of this manuscript.
Contributor Information
Manny M.Y. Kwok, Email: manny.kwok@connect.polyu.hk.
Shamay S.M. Ng, Email: shamay.ng@polyu.edu.hk.
S.S. Man, Email: shing.man@polyu.edu.hk.
Billy C.L. So, Email: billy.so@polyu.edu.hk.
Appendix A.
An Example of search strategy.
| Search keywords | aquatic exercise or aquatic or water exercise or hydro therapy or water immersion or head out aquatics exercise or swim or water aerobics) AND (high intensity interval training or intermittent exercise or interval training or high intensity or all-out exercise)) AND (cardiometabolic health or cardiorespiratory or metabolic markers or physical or physical health)) AND (women or female or gender) |
|---|---|
| Database | PubMed |
| Results | 659 |
| Translations | aquatic: "aquatic"[All Fields] OR "aquatically"[All Fields] OR "aquatics"[All Fields] exercise: "exercise"[MeSH Terms] OR "exercise"[All Fields] OR "exercises"[All Fields] OR "exercise therapy"[MeSH Terms] OR (exercise"[All Fields] AND "therapy"[All Fields]) OR "exercise therapy"[All Fields] OR "exercise's"[All Fields] OR "exercised"[All Fields] OR "exerciser"[All Fields] OR "exercisers"[All Fields] OR "exercising"[All Fields] aquatic: "aquatic"[All Fields] OR "aquatically"[All Fields] OR "aquatics"[All Fields] water: "water"[MeSH Terms] OR "water"[All Fields] OR "drinking water"[MeSH Terms] OR ("drinking"[All Fields] AND "water"[All Fields]) OR "drinking water"[All Fields] OR "watering"[All Fields] OR "waters"[All Fields] OR "water's"[All Fields] OR "watered"[All Fields] OR "waterer"[All Fields] OR "waterers"[All Fields] OR "waterings"[All Fields] exercise: "exercise"[MeSH Terms] OR "exercise"[All Fields] OR "exercises"[All Fields] OR "exercise therapy"[MeSH Terms] OR ("exercise"[All Fields] AND "therapy"[All Fields]) OR "exercise therapy"[All Fields] OR "exercise's"[All Fields] OR "exercised"[All Fields] OR "exerciser"[All Fields] OR "exercisers"[All Fields] OR "exercising"[All Fields] hydro: "hydro"[All Fields] OR "hydros"[All Fields] therapy: "therapeutics"[MeSH Terms] OR "therapeutics"[All Fields] OR "therapies"[All Fields] OR "therapy"[Subheading] OR "therapy"[All Fields] OR "therapy's"[All Fields] OR "therapys"[All Fields] water: "water"[MeSH Terms] OR "water"[All Fields] OR "drinking water"[MeSH Terms] OR ("drinking"[All Fields] AND "water"[All Fields]) OR "drinking water"[All Fields] OR "watering"[All Fields] OR "waters"[All Fields] OR "water's"[All Fields] OR "watered"[All Fields] OR "waterer"[All Fields] OR "waterers"[All Fields] OR "waterings"[All Fields] immersion: "immerse"[All Fields] OR "immersed"[All Fields] OR "immerses"[All Fields] OR "immersing"[All Fields] OR "immersion"[MeSH Terms] OR "immersion"[All Fields] OR "immersions"[All Fields] OR "immersive"[All Fields] OR "immersiveness"[All Fields] head: "head"[MeSH Terms] OR "head"[All Fields] aquatics: "aquatic"[All Fields] OR "aquatically"[All Fields] OR "aquatics"[All Fields] exercise: "exercise"[MeSH Terms] OR "exercise"[All Fields] OR "exercises"[All Fields] OR "exercise therapy"[MeSH Terms] OR ("exercise"[All Fields] AND "therapy"[All Fields]) OR "exercise therapy"[All Fields] OR "exercise's"[All Fields] OR "exercised"[All Fields] OR "exerciser"[All Fields] OR "exercisers"[All Fields] OR "exercising"[All Fields] swim: "swimming"[MeSH Terms] OR "swimming"[All Fields] OR "swim"[All Fields] water: "water"[MeSH Terms] OR "water"[All Fields] OR "drinking water"[MeSH Terms] OR ("drinking"[All Fields] AND "water"[All Fields]) OR "drinking water"[All Fields] OR "watering"[All Fields] OR "waters"[All Fields] OR "water's"[All Fields] OR "watered"[All Fields] OR "waterer"[All Fields] OR "waterers"[All Fields] OR "waterings"[All Fields] aerobics: "aerobic"[All Fields] OR "aerobically"[All Fields] OR "bacteria, aerobic"[MeSH Terms] OR ("bacteria"[All Fields] AND "aerobic"[All Fields]) OR "aerobic bacteria"[All Fields] OR "aerobe"[All Fields] OR "aerobes"[All Fields] OR "exercise"[MeSH Terms] OR "exercise"[All Fields] OR "aerobics"[All Fields] high intensity interval training: "high-intensity interval training"[MeSH Terms] OR ("high-intensity"[All Fields] AND "interval"[All Fields] AND "training"[All Fields]) OR "high-intensity interval training"[All Fields] OR ("high"[All Fields] AND "intensity"[All Fields] AND "interval"[All Fields] AND "training"[All Fields]) OR "high intensity interval training"[All Fields] intermittent: "intermittant"[All Fields] OR "intermittence"[All Fields] OR "intermittencies"[All Fields] OR "intermittency"[All Fields] OR "intermittent"[All Fields] OR "intermittently"[All Fields] exercise: "exercise"[MeSH Terms] OR "exercise"[All Fields] OR "exercises"[All Fields] OR "exercise therapy"[MeSH Terms] OR ("exercise"[All Fields] AND "therapy"[All Fields]) OR "exercise therapy"[All Fields] OR "exercise's"[All Fields] OR "exercised"[All Fields] OR "exerciser"[All Fields] OR "exercisers"[All Fields] OR "exercising"[All Fields] interval: "interval"[All Fields] OR "intervals"[All Fields] training: "education"[Subheading] OR "education"[All Fields] OR "training"[All Fields] OR "education"[MeSH Terms] OR "train"[All Fields] OR "train's"[All Fields] OR "trained"[All Fields] OR "training's"[All Fields] OR "trainings"[All Fields] OR "trains"[All Fields] intensity: "intense"[All Fields] OR "intensely"[All Fields] OR "intensities"[All Fields] OR "intensity"[All Fields] OR "intensively"[All Fields] exercise: "exercise"[MeSH Terms] OR "exercise"[All Fields] OR "exercises"[All Fields] OR "exercise therapy"[MeSH Terms] OR ("exercise"[All Fields] AND "therapy"[All Fields]) OR "exercise therapy"[All Fields] OR "exercise's"[All Fields] OR "exercised"[All Fields] OR "exerciser"[All Fields] OR "exercisers"[All Fields] OR "exercising"[All Fields] cardiometabolic: "cardiometabolic"[All Fields] OR "cardiometabolically"[All Fields] health: "health"[MeSH Terms] OR "health"[All Fields] OR "health's"[All Fields] OR "healthful"[All Fields] OR "healthfulness"[All Fields] OR "healths"[All Fields] metabolic: "metabolic"[All Fields] OR "metabolical"[All Fields] OR "metabolically"[All Fields] OR "metabolics"[All Fields] OR "metabolism"[MeSH Terms] OR "metabolism"[All Fields] OR "metabolisms"[All Fields] OR "metabolism"[Subheading] OR "metabolic networks and pathways"[MeSH Terms] OR ("metabolic"[All Fields] AND "networks"[All Fields] AND "pathways"[All Fields]) OR "metabolic networks and pathways"[All Fields] OR "metabolities"[All Fields] OR "metabolization"[All Fields] OR "metabolize"[All Fields] OR "metabolized"[All Fields] OR "metabolizer"[All Fields] OR "metabolizers"[All Fields] OR "metabolizes"[All Fields] OR "metabolizing"[All Fields] markers: "biomarkers"[MeSH Terms] OR "biomarkers"[All Fields] OR "marker"[All Fields] OR "markers"[All Fields] physical: "physical examination"[MeSH Terms] OR ("physical"[All Fields] AND "examination"[All Fields]) OR "physical examination"[All Fields] OR "physical"[All Fields] OR "physically"[All Fields] OR "physicals"[All Fields] physical: "physical examination"[MeSH Terms] OR ("physical"[All Fields] AND "examination"[All Fields]) OR "physical examination"[All Fields] OR "physical"[All Fields] OR "physically"[All Fields] OR "physicals"[All Fields] health: "health"[MeSH Terms] OR "health"[All Fields] OR "health's"[All Fields] OR "healthful"[All Fields] OR "healthfulness"[All Fields] OR "healths"[All Fields] women: "womans"[All Fields] OR "women"[MeSH Terms] OR "women"[All Fields] OR "woman"[All Fields] OR "women's"[All Fields] OR "womens"[All Fields] female: "femal"[All Fields] OR "female"[MeSH Terms] OR "female"[All Fields] OR "females"[All Fields] OR "female's"[All Fields] OR "femals"[All Fields] gender: "gender identity"[MeSH Terms] OR ("gender"[All Fields] AND "identity"[All Fields]) OR "gender identity"[All Fields] OR "gendered"[All Fields] OR "gender's"[All Fields] OR "gendering"[All Fields] OR "genderized"[All Fields] OR "genders"[All Fields] OR "sex"[MeSH Terms] OR "sex"[All Fields] OR "gender"[All Fields] |
Appendix B.
Table of summary of participants characteristics, study outcomes.
| Author | Country | Participants |
Outcomes |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Women Population | AHIIT Mean Age (SD) | Control Mean Age (SD) | Aquatic | Control | Land | other groups | |||
| L. S. Andrade et al., 2020a | Brazil | older women (n = 41) | 64.8 (3.6) | 63.9 (3.7) | n = 20 | n = 12 | 0 | 0 | Cardiometabolic health markers -Cardiorespiratory capacity Physical markers- muscle thickness and muscle quality, neuromuscular activity |
| L. S. Andrade et al., 2020b | Brazil | older women (n = 41) | 64.8 (3.6) | 63.9 (3.7) | n = 20 | n = 12 | 0 | 0 | physical markers- functional tests, 30 seconds chair to stand test, 6-min walk test, 5 metre habitual gait velocity, Quality of Life |
| Bento et al., 2014 | Brazil | older women able to walk and carry out activity of daily livings (n = 87) | 65.5 | 66.2 | n = 25 | n = 19 | n = 23 | 0 | physical markers- muscle strengths of dynamic knee flexion and knee extension |
| Broman et al., 2006 | Sweden | healthy women (n = 29) | 69(4) | 69.8 (3.5) | n = 18 | n = 11 | 0 | 0 | cardiometabolic health markers - Maximal oxygen uptake, oxygen capacity, maximal heart rate, body weight, heart rate, blood pressure |
| Connolly et al., 2016 | UK | inactive pre-menopausal women with mild to moderate arterial hypertension (n = 62) | 44(5) | 45 (4) | n = 21 | n = 20 | 0 | Low intensity continuous training n = 21 | Cardiometabolic health markers- Blood sampling for plasma insulin and plasma glucose, insulin sensitivity |
| Costa et al., 2018 | Brazil | pre-menopausal sedentary women with dyslipidaemia (n = 40) | 46.24 (3.6) | 46.77 (4.5) | n = 20 | n = 20 | 0 | 0 | Cardiometabolic health markers- Total cholesterol, triglycerides, high density lipoprotein, low density lipoprotein, peak oxygen consumption |
| Aboarrage Junior et al., 2018 | Brazil | elderly women (n = 25) | NR | NR | n = 15 | n = 10 | 0 | 0 | Cardiometabolic health markers -body mass index (BMI), body fat percentage, Physical markers- lumbar spine, total femur, whole body bone mineral density (BMD), chair to stand test (CS), timed up and go test (TUG) |
| Junior et al., 2018 | Brazil | hypertensive females (n = 12) | 66.8 (4.8) | 66.8 (4.8) | n = 12 | n = 12 | 0 | 0 | Cardiometabolic health markers-Systolic blood pressure, diastolic blood pressure, Mean blood pressure at rest, 15,60, 45, 60min post session and systolic and diastolic post exercise hypotension |
| Mohr et al., 2014 | Denmark | sedentary premenopausal women with mild and moderate hypertension (n = 62) | 44 (2) | 45 (2) | n = 21 | n = 20 | 0 | Moderate intensity swim (n = 21) | Cardiometabolic health markers- systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure, resting heartrate, blood sampling for Total cholesterol, high density lipoprotein (HDL), low density lipoprotein (LDL), Dual-energy X-ray (DXA), for whole body fat and lean body mass, hip waist circumference and body weight |
| Mohr et al., 2014 | Denmark | sedentary premenopausal women with mild and moderate hypertension (n = 83) | 44 (9) | 45 (9) | High intensity swim: (n = 21) Moderate Intensity swim: (n = 21) |
n = 20 | soccer n = 21 |
0 | Physical markers-Whole body bone mineral content (BMC) and area bone mineral density (BMD) evaluated by Dual-energy X-ray (DXA), Fat mass and lean mass, Blood sampling analysed for bone turnover markers |
| Moreira et al., 2013 | Brazil | sedentary women (n = 108) | 58.6 (6.7) | 59.3 (6.07) | n = 64 | n = 44 | 0 | 0 | Physical markers- number of falls and fallers, flexibility using walls sit and reach test (FLEX), static balance using Unipedal Stance Test (UST), mobility using timed up and go test (TUG), handgrips strength of dominant hand (HGS), maximal isometric strength of back extensors muscles (SBE), strength of hip flexor muscles (SHF) and strength of knee extensor muscles (SKE), iPTH (intact parathyroid hormone), vitamin D and total calcium |
| Moreira et al., 2014 | Brazil | sedentary women (n = 108) | 58.8 (6.7) | 59.3 (6.07) | n = 64 | n = 44 | 0 | 0 | Physical markers- markers of bone turnover- fasting blood sample collected for measures of iPTH (intact parathyroid hormone), PINP (bone formation marker) and CTx (bone resorption marker), bone mass of lumbar spine (L1-L4), proximal femur and total body using Dual-energy X-ray (DXA),. |
| Munukka et al., 2016 | Finland | post-menopausal women, mild knee osteoarthritis (n = 87) | 64(2) | 64(2) | n = 43 | n = 44 | 0 | 0 | Physical markers- the biochemical composition of medial and lateral tibiofemoral cartilage was estimated using T2 map and delayed gadolinium-enhanced magnetic resonance imaging of cartilage (dGEMRIC) index, isometric knee extensor, flexor force, Knee Injury and Osteoarthritis questionnaire Score (KOOS) questionnaire Cardiometabolic health markers- cardiorespiratory fitness |
| Munukka et al., 2020 | Finland | post-menopausal women, mild knee osteoarthritis (n = 87) | 64 (2) | 64 (2) | n = 43 | n = 44 | 0 | 0 | Physical markers: Western Ontario and McMaster University Osteoarthritis Index (WOMAC) and health related quality of life (SF-36) at baseline, 4 months, 12 months follow up. |
| Nordsborg et al., 2015 | Denmark | sedentary premenopausal women with mild and moderate hypertension (n = 62) | 45(6) | 45 (4) | n = 21 | n = 20 | 0 | 0 | Physical markers- muscles biopsy of deltoid, vastus lateralis and measure the protein expressions and muscle glycogen, Dual-energy X-ray (DXA) for body composition, arm leg lean body mass |
| Ryzkova et al., 2017 | Slovakia | female students (n = 16) | 21 (3.2) | 21 (3.2) | n = 8 | n = 8 | 0 | 0 | Physical markers- including body weight, waist circumference, hip circumference, right and left arm circumference, right and left leg circumference, body fat, body mass index (BMI), waist to hip ratio Motor variables- including static balance tests on standing on one leg with eyes opened, stand on two legs with eye opened, standing on two legs with eyes closed, performance tests, tandem walk, sit to reach tests. |
| Samadi et al., 2020 | Iran | women with polycystic ovary syndrome (PCOS) (n = 30) |
20–35 | 20–35 | n = 15 | n = 15 | 0 | 0 | Cardiometabolic health markers- fasting blood samples for measuring levels of insulin resistance (IR), sex hormone binding globulin (SHBG), free testosterone (FT), total testosterone (TT), luteinising hormone (LH), dehydroepiandrosterone sulphate (DHEAS) and follicle-stimulating hormone (FSH), maximal oxygen capacity Physical markers- body mass index (BMI), fat mass, waist to hip ratio, |
| Waller et al., 2017 | Finland | post-menopausal women, mild knee osteoarthritis (n = 87) | 64(2) | 64 (2) | n = 43 | n = 44 | 0 | 0 | Physical markers- 1. Body composition (total body fat and lean body mass (kg) measured with Dual-energy X-ray (DXA), 2. walking speed calculated from walking test 3. self-reported symptoms, pain and activities of daily livings measured by KOOS (knee injury and osteoarthritis outcome score KOOS) 4. Leisure time physical activity calculated by daily physical activity diary |
References
- 1.World Health O . World Health Organization; 1995. The World Health Report: Report of the Director-General. [Google Scholar]
- 2.Organization WH . World Health Organization; 2014. Global Status Report on Noncommunicable Diseases 2014. [Google Scholar]
- 3.Hallal P.C., Andersen L.B., Bull F.C., Guthold R., Haskell W., Ekelund U. Physical activity 1 global physical activity levels: surveillance progress, pitfalls, and prospects. The Lancet (British edition) 2012;380(9838):247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- 4.Paffenbarger R.S., Hyde R., Wing A.L., Hsieh C-c. Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med. 1986;314(10):605–613. doi: 10.1056/NEJM198603063141003. [DOI] [PubMed] [Google Scholar]
- 5.Guthold R., Stevens G.A., Riley L.M., Bull F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Global Health. 2018;6(10):e1077–e1086. doi: 10.1016/S2214-109X(18)30357-7. [DOI] [PubMed] [Google Scholar]
- 6.Andrade L., Pinto S., Silva M., et al. Randomized clinical trial of water-based aerobic training in older women (WATER study): functional capacity and quality of life outcomes. J Phys Activ Health. 2020;17:1–9. doi: 10.1123/jpah.2019-0552. [DOI] [PubMed] [Google Scholar]
- 7.Ng M., Fleming T., Robinson M., et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thompson W.R. Worldwide survey of fitness trends for 2020. ACSM's Health & Fit J. 2019;23(6):10–18. [Google Scholar]
- 9.Karlsen T., Aamot I.-L., Haykowsky M., Rognmo Ø. High intensity interval training for maximizing health outcomes. Prog Cardiovasc Dis. 2017;60(1):67–77. doi: 10.1016/j.pcad.2017.03.006. [DOI] [PubMed] [Google Scholar]
- 10.Nagle E.F., Sanders M.E., Franklin B.A. Aquatic high intensity interval training for cardiometabolic health: benefits and training design. Am J Lifestyle Med. 2017;11(1):64–76. doi: 10.1177/1559827615583640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Campbell J.A., D'Acquisto L.J., D'Acquisto D.M., Cline M.G. Metabolic and cardiovascular response to shallow water exercise in young and older women. Med Sci Sports Exerc. 2003;35(4):675–681. doi: 10.1249/01.MSS.0000058359.87713.99. [DOI] [PubMed] [Google Scholar]
- 12.Depiazzi J.E., Forbes R.A., Gibson N., et al. The effect of aquatic high-intensity interval training on aerobic performance, strength and body composition in a non-athletic population: systematic review and meta-analysis. Clin Rehabil. 2018;33(2):157–170. doi: 10.1177/0269215518792039. [DOI] [PubMed] [Google Scholar]
- 13.Gibala M.J. High-intensity interval training: a time-efficient strategy for health promotion? Curr Sports Med Rep. 2007;6(4):211–213. [PubMed] [Google Scholar]
- 14.Batacan R.B., Duncan M.J., Dalbo V.J., Tucker P.S., Fenning A.S. Effects of high-intensity interval training on cardiometabolic health: a systematic review and meta-analysis of intervention studies. Br J Sports Med. 2017;51(6):494. doi: 10.1136/bjsports-2015-095841. [DOI] [PubMed] [Google Scholar]
- 15.Weston K.S., Wisløff U., Coombes J.S. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. Br J Sports Med. 2014;48(16):1227–1234. doi: 10.1136/bjsports-2013-092576. [DOI] [PubMed] [Google Scholar]
- 16.Becker B.E., Hildenbrand K., Whitcomb R.K., Sanders J.P. Biophysiologic effects of warm water immersion. Int J Aquat Res Educ. 2009;3(1) [Google Scholar]
- 17.Rana S.H., Sophie E.H., Anthony R.D. Aquatic physical therapy for hip and knee osteoarthritis: results of a single-blind randomized controlled trial. Phys Ther. 2007;87(1):32–43. doi: 10.2522/ptj.20060006. [DOI] [PubMed] [Google Scholar]
- 18.Harrison R.A., Hillman M., Bulstrode S. Loading of the lower limb when walking partially immersed: implications for clinical practice. Physiotherapy. 1992;78(3):164–166. [Google Scholar]
- 19.Barker A.L.P., Talevski J.B.S., Morello R.T.M.P.H., Brand C.A.M.P.H., Rahmann A.E.P., Urquhart D.M.P. Effectiveness of aquatic exercise for musculoskeletal conditions: a meta-analysis. Arch Phys Med Rehabil. 2014;95(9):1776–1786. doi: 10.1016/j.apmr.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 20.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339(7716):332–336. [PMC free article] [PubMed] [Google Scholar]
- 21.Higgins J.P.T. second ed. Cochrane; Hoboken, New Jersey: 2019. Cochrane Handbook for Systematic Reviews of Interventions. [Google Scholar]
- 22.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Andrade L.S., Pinto S.S., Silva M.R., et al. Water-based continuous and interval training in older women: cardiorespiratory and neuromuscular outcomes (WATER study) Exp Gerontol. 2020;134:110914. doi: 10.1016/j.exger.2020.110914. [DOI] [PubMed] [Google Scholar]
- 24.Broman G., Quintana M., Lindberg T., Jansson E., Kaijser L. High intensity deep water training can improve aerobic power in elderly women. Eur J Appl Physiol. 2006;98(2):117–123. doi: 10.1007/s00421-006-0237-2. [DOI] [PubMed] [Google Scholar]
- 25.Bento P.C.B., Rodacki A.L.F. Muscle function in aged women in response to a water-based exercises program and progressive resistance training. Geriatr Gerontol Int. 2015;15(11):1193–1200. doi: 10.1111/ggi.12418. [DOI] [PubMed] [Google Scholar]
- 26.Connolly L.J., Nordsborg N.B., Nyberg M., Weihe P., Krustrup P., Mohr M. Low-volume high-intensity swim training is superior to high-volume low-intensity training in relation to insulin sensitivity and glucose control in inactive middle-aged women. Eur J Appl Physiol. 2016;116(10):1889–1897. doi: 10.1007/s00421-016-3441-8. [DOI] [PubMed] [Google Scholar]
- 27.Costa R.R., Pilla C., Buttelli A.C.K., et al. Water-based aerobic training successfully improves lipid profile of dyslipidemic women: a randomized controlled trial. Res Q Exerc Sport. 2018;89(2):173–182. doi: 10.1080/02701367.2018.1441485. [DOI] [PubMed] [Google Scholar]
- 28.Junior EAdS., Suassuna J.A.S., de Melo A.B.S.R., et al. High-intensity interval aquatic exercise session promotes post-exercise hypotension in hypertensive elderly: a randomized controlled trial. J. Exercise Physiol. Online. 2018;21(1):149. [Google Scholar]
- 29.Aboarrage Junior A.M., Teixeira C.V.L.S., dos Santos R.N., et al. A high-intensity jump-based aquatic exercise program improves bone mineral density and functional fitness in postmenopausal women. Rejuvenation Res. 2018;21(6):535–540. doi: 10.1089/rej.2018.2069. [DOI] [PubMed] [Google Scholar]
- 30.Moreira L.D.F., Fronza F.C.A.O., dos Santos R.N., et al. The benefits of a high-intensity aquatic exercise program (HydrOS) for bone metabolism and bone mass of postmenopausal women. J Bone Miner Metabol. 2014;32(4):411–419. doi: 10.1007/s00774-013-0509-y. [DOI] [PubMed] [Google Scholar]
- 31.Mohr M., Nordsborg N.B., Lindenskov A., et al. High-intensity intermittent swimming improves cardiovascular health status for women with mild hypertension. BioMed Res Int. 2014:1–9. doi: 10.1155/2014/728289. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Denise Fernandes Moreira L., Fronza F.C.A.O., dos Santos R.N., Teixeira L.R., Kruel L.F.M., Lazaretti-Castro M. High-intensity aquatic exercises (HydrOS) improve physical function and reduce falls among postmenopausal women. Menopause. 2013;20(10):1012–1019. doi: 10.1097/GME.0b013e3182850138. [DOI] [PubMed] [Google Scholar]
- 33.Mohr M., Helge E.W., Petersen L.F., et al. Effects of soccer vs swim training on bone formation in sedentary middle-aged women. Eur J Appl Physiol. 2015;115(12):2671–2679. doi: 10.1007/s00421-015-3231-8. [DOI] [PubMed] [Google Scholar]
- 34.Munukka M.M., Waller B.M., Rantalainen T.P., et al. Efficacy of progressive aquatic resistance training for tibiofemoral cartilage in postmenopausal women with mild knee osteoarthritis: a randomised controlled trial. Osteoarthritis Cartilage. 2016;24(10):1708–1717. doi: 10.1016/j.joca.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 35.Munukka M., Waller B., Häkkinen A., et al. Effects of progressive aquatic resistance training on symptoms and quality of life in women with knee osteoarthritis: a secondary analysis. Scand J Med Sci Sports. 2020;30(6):1064–1072. doi: 10.1111/sms.13630. [DOI] [PubMed] [Google Scholar]
- 36.Nordsborg N.B., Connolly L., Weihe P., et al. Oxidative capacity and glycogen content increase more in arm than leg muscle in sedentary women after intense training. J Appl Physiol. 2015;119(2):116–123. doi: 10.1152/japplphysiol.00101.2015. [DOI] [PubMed] [Google Scholar]
- 37.Rýzková E., Labudová J., Grznár L.U., Šmída M. Effects of aquafitness with high intensity interval training on physical fitness. J. Phys. Edu. Sport. 2018;18:373–381. [Google Scholar]
- 38.Samadi Z., Bambaeichi E., Valiani M., Shahshahan Z. Evaluation of changes in levels of hyperandrogenism, hirsutism and menstrual regulation after a period of aquatic high intensity interval training in women with polycystic ovary syndrome. Int J Prev Med. 2019;10(1):187. doi: 10.4103/ijpvm.IJPVM_360_18. 187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Waller B., Munukka M., Rantalainen T., et al. Effects of high intensity resistance aquatic training on body composition and walking speed in women with mild knee osteoarthritis: a 4-month RCT with 12-month follow-up. Osteoarthritis Cartilage. 2017;25(8):1238–1246. doi: 10.1016/j.joca.2017.02.800. [DOI] [PubMed] [Google Scholar]
- 40.Andrade L.S., Pinto S.S., Silva M.R., et al. Water-based continuous and interval training in older women: cardiorespiratory and neuromuscular outcomes (WATER study) Exp Gerontol. 2020;134:110914. doi: 10.1016/j.exger.2020.110914. [DOI] [PubMed] [Google Scholar]
- 41.Whipp B.J., Whipp B.J., Ward S.A., Ward S.A. Physiological determinants of pulmonary gas exchange kinetics during exercise. Med Sci Sports Exerc. 1990;22(1):62–71. [PubMed] [Google Scholar]
- 42.Keteyian S.J.P., Brawner C.A.M.S., Savage P.D.M.S., et al. Peak aerobic capacity predicts prognosis in patients with coronary heart disease. Am Heart J. 2008;156(2):292–300. doi: 10.1016/j.ahj.2008.03.017. [DOI] [PubMed] [Google Scholar]
- 43.McDaniel B.B., Naquin M.R., Sirikul B., Kraemer R.R. Five weeks of aquatic-calisthenic high intensity interval training improves cardiorespiratory fitness and body composition in sedentary young adults. J Sports Sci Med. 2020;19(1):187–194. [PMC free article] [PubMed] [Google Scholar]
- 44.Gibala M.J., Jones A.M. Physiological and performance adaptations to high-intensity interval training. Limits Human Endurance. 2013;76:51–60. doi: 10.1159/000350256. [DOI] [PubMed] [Google Scholar]
- 45.McNamara R.J., McKeough Z.J., McKenzie D.K., Alison J.A., McNamara R.J. Water-based exercise training for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2013;(12):CD008290. doi: 10.1002/14651858.CD008290.pub2. 2013. CD008290. [DOI] [PubMed] [Google Scholar]
- 46.Silvers W.M., Rutledge E.R., Dolny D.G. Peak cardiorespiratory responses during aquatic and land treadmill exercise. Med Sci Sports Exerc. 2007;39(6):969–975. doi: 10.1097/mss.0b013e31803bb4ea. [DOI] [PubMed] [Google Scholar]
- 47.Plotnick G.D., Becker L.C., Fisher M.L., et al. Use of the Frank-Starling mechanism during submaximal versus maximal upright exercise. Am J Physiol Heart Circ Physiol. 1986;251(6):H1101–H1105. doi: 10.1152/ajpheart.1986.251.6.H1101. [DOI] [PubMed] [Google Scholar]
- 48.Helgerud J., Hoydal K., Wang E., et al. Aerobic high-intensity intervals improve VO2max more than moderate training. Med Sci Sports Exerc. 2007;39(4):665–671. doi: 10.1249/mss.0b013e3180304570. [DOI] [PubMed] [Google Scholar]
- 49.Carter J.B., Banister E.W., Blaber A.P. Effect of endurance exercise on autonomic control of heart rate. Sports Med. 2003;33(1):33–46. doi: 10.2165/00007256-200333010-00003. [DOI] [PubMed] [Google Scholar]
- 50.Jensen M.T., Suadicani P., Hein H.O., Gyntelberg F. Elevated resting heart rate, physical fitness and all-cause mortality: a 16-year follow-up in the Copenhagen Male Study. Heart. 2013;99(12):882–887. doi: 10.1136/heartjnl-2012-303375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lau K., Malik A., Foroutan F., et al. Resting heart rate as a predictor of mortality in patients with heart failure. Can J Cardiol. 2019;35(10):S61. S61. [Google Scholar]
- 52.Myers J., Prakash M., Froelicher V., Do D., Partington S., Atwood J.E. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346(11):793–801. doi: 10.1056/NEJMoa011858. [DOI] [PubMed] [Google Scholar]
- 53.Strandberg T.E., Pitkala K. What is the most important component of blood pressure: systolic, diastolic or pulse pressure? Curr Opin Nephrol Hypertens. 2003;12(3):293–297. doi: 10.1097/00041552-200305000-00011. [DOI] [PubMed] [Google Scholar]
- 54.Poon E.T.-C., Little J.P., Sit C.H.-P., Wong S.H.-S. The effect of low-volume high-intensity interval training on cardiometabolic health and psychological responses in overweight/obese middle-aged men. J Sports Sci. 2020;38(17):1997–2004. doi: 10.1080/02640414.2020.1766178. [DOI] [PubMed] [Google Scholar]
- 55.Hall J., Grant J., Blake D., Taylor G., Garbutt G. Cardiorespiratory responses to aquatic treadmill walking in patients with rheumatoid arthritis. Physiother Res Int. 2004;9(2):59–73. doi: 10.1002/pri.303. [DOI] [PubMed] [Google Scholar]
- 56.Pöyhönen T., Sipilä S., Keskinen K.L., Hautala A., Savolainen J., Mälkiä E. Effects of aquatic resistance training on neuromuscular performance in healthy women. Med Sci Sports Exerc. 2002;34(12):2103–2109. doi: 10.1249/01.MSS.0000039291.46836.86. [DOI] [PubMed] [Google Scholar]
- 57.Wing-Hoi C., Wing-Sze L., Ling Q., Ning T., Vivian Wing-Yin H., Kwok-Sui L. Type IIB human skeletal muscle fibers positively correlate with bone mineral density irrespective to age. Chinese Med J. 2010;123(21):3009–3014. [PubMed] [Google Scholar]
- 58.Heywood S.M., McClelland J.P., Mentiplay B.B., Geigle P.P., Rahmann A.P., Clark R.P. Effectiveness of aquatic exercise in improving lower limb strength in musculoskeletal conditions: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2016;98(1):173–186. doi: 10.1016/j.apmr.2016.08.472. [DOI] [PubMed] [Google Scholar]
- 59.Wolff I., van Croonenborg J.J., Kemper H.C.G., Kostense P.J., Twisk J.W.R. The effect of exercise training programs on bone mass: a meta-analysis of published controlled trials in pre- and postmenopausal women. Osteoporos Int. 1999;9(1):1–12. doi: 10.1007/s001980050109. [DOI] [PubMed] [Google Scholar]
- 60.Martyn-St James M., Carroll S. A meta-analysis of impact exercise on postmenopausal bone loss: the case for mixed loading exercise programmes. Br J Sports Med. 2009;43(12):898–908. doi: 10.1136/bjsm.2008.052704. [DOI] [PubMed] [Google Scholar]
- 61.Bohannon R.W. Body weight-normalized knee extension strength explains sit-to-stand independence: a validation study. J Strength Condit Res. 2009;23(1):309–311. doi: 10.1519/JSC.0b013e31818eff0b. [DOI] [PubMed] [Google Scholar]
- 62.Vaidya T., Chambellan A., de Bisschop C. Sit-to-stand tests for COPD: a literature review. Respir Med. 2017;128:70–77. doi: 10.1016/j.rmed.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 63.Zanini A., Aiello M., Cherubino F., et al. The one repetition maximum test and the sit-to-stand test in the assessment of a specific pulmonary rehabilitation program on peripheral muscle strength in COPD patients. Int J Chronic Obstr Pulm Dis. 2015;10:2423–2430. doi: 10.2147/COPD.S91176. [DOI] [PMC free article] [PubMed] [Google Scholar]