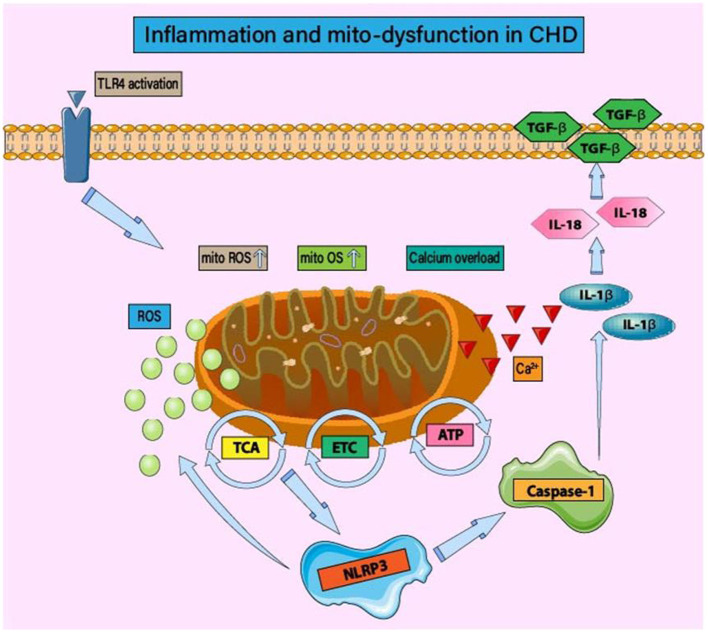
Figure 1.
Inflammation and mitochondrial dysfunction in CHD. Under mitochondrial oxidative stress and structural/functional imbalance, the activation of inflammatory bodies is regulated by mitochondrial function. The main mechanism is that the imbalance of mitochondrial homeostasis leads to the production of inflammatory body components NLRP3, caspase-1, and IL-1 β/IL-18. In the early stage of CHD, the activation of TLR4 leads to mitochondrial energy metabolism disorder, tricarboxylic acid cycle disorder, and insufficient ATP production. Mitochondrial dysfunction also affects the regulatory function of ETC. ROS-induced oxidative stress injury is accompanied by calcium homeostasis disorder and calcium overload. The activation of NLRP3 and the occurrence of inflammatory injury lead to the excessive production of ROS and the persistence of the vicious cycle of “inflammation-oxidative stress.” Mitochondrial homeostasis disorder can induce post-translational modification of NLRP3, stabilize NLRP3 in an inactive but activated state of signal transduction, and then affect the activation of inflammatory signal pathways such as NF-κB.