Abstract
Background
Intramedullary devices for the fixation of intertrochanteric fractures are increasing in usage and popularity. This reflects either a shift in adoption of new technology or intertrochanteric fractures becoming more complex or unstable. This trend was observed in our institution, hence we set out to investigate if this was concordant with an associated change in the demographics of the patients or in the morphology of the intertrochanteric fracture pattern over a 10-year period.
Methods
This is a retrospective cross-sectional comparison undertaken for the first 100 consecutive elderly patients with intertrochanteric fractures admitted to our tertiary institution over 3 yearly intervals, in each of the years 2004, 2007, 2010, and 2013. Fractures were radiologically classified via the Evans and AO classifications. Patient demographics such as age, ethnicity, and comorbidities and surgical data including time, type of fixation, time to surgery, and length of stay were collected via case note reviews to identify possible trends.
Results
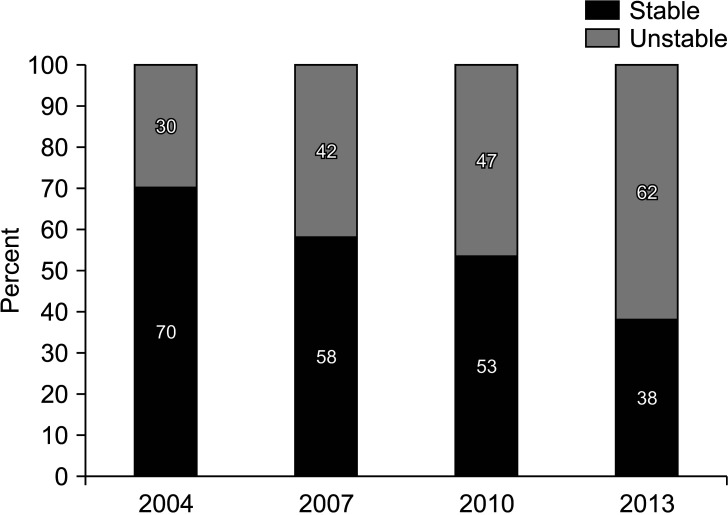
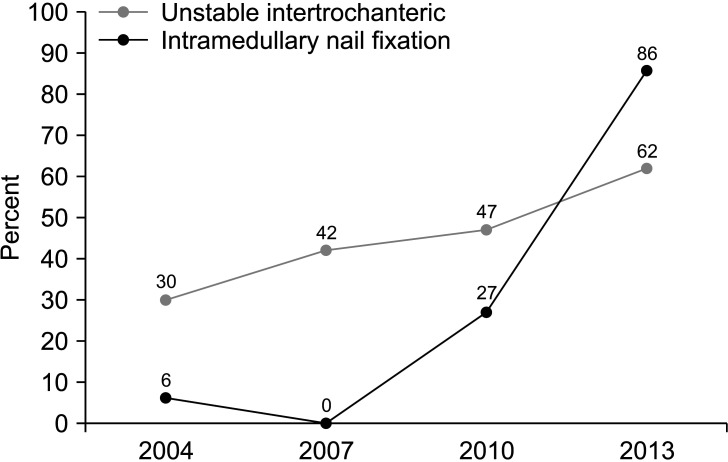
The overall mean age was 80.5 years, with no statistically significant trend among age, sex, ethnicity, and comorbidities over the 10-year period. The main finding was a rise in the proportion of unstable intertrochanteric fractures. The proportion of such fractures was 30% in 2004, 42% in 2007, 47% in 2010, and 62% in 2013 (p < 0.001). Patients admitted for intertrochanteric fractures also experienced a shorter hospital length of stay and an increasing trend towards early fracture fixation (p < 0.001), with a greater usage of intramedullary nails in the treatment of such fractures (p < 0.001).
Conclusions
Intertrochanteric fractures in elderly patients have evolved into more complex fractures over the past ten years, despite there being no change in the age of the patients over the same duration. This increasing proportion of unstable intertrochanteric fractures has brought about a greater tendency to fix these fractures with intramedullary implants.
Keywords: Intertrochanteric fractures, Hip fracture, Classification, Fracture fixation
Worldwide projections for hip fractures have predicted that the total number of hip fractures in those aged above 50 years will double from 1.5 million in 1990 to approximately 3 million in 2025, with a steady increase in these fractures, providing an economic strain on the society over recent years.1) Differences have been reported between intertrochanteric fractures and neck of femur fractures, with Fox et al.2) having demonstrated that patients were older and worse in the pre-injury health status in the group that sustained intertrochanteric hip fractures and less likely to recover to pre-fracture level of functioning at 2 months after fracture. Due to our country’s increasing ageing population, intertrochanteric fractures in particular will continue to be of clinical as well as economic importance in the face of rising healthcare costs.
Surgical implants employed to fix intertrochanteric fractures are dichotomized into being either intramedullary (nails) or extramedullary (sliding hip screws). The dynamic hip screw (DHS) has traditionally been the most commonly used implant for extracapsular hip fractures but this is now being taken over by cephalomedullary implants.3) Most level I studies indicate that there are no significant differences in loss of reduction, union rates, eventual functional outcomes, complication rates, and length of stay when comparing cephalomedullary devices with sliding hip screw constructs.4,5,6)
We have noted an increasing trend towards the use of intramedullary devices for the fixation of intertrochanteric fractures in our institution in recent years, hence we set out to investigate if this was concordant with an associated change in the demographics of patients or in the morphology of the intertrochanteric fracture pattern over a 10-year period. We therefore designed a study to investigate the fracture morphology of intertrochanteric fractures over a 10-year period and also to identify trends with regards to the use of extramedullary (plates) versus intramedullary (nails) devices and time to surgery, as well as patients’ hospitalization length of stay (HLOS).
METHODS
This is a retrospective radiological and descriptive study conducted at a trauma center with an established orthogeriatric co-managed hip fracture care pathway. Ethics board approval was obtained prior to the initiation of the study (NHG DSRB ref. 2014/00251). We sampled the population at 3 yearly intervals within a 10-year study period—the first 100 consecutive patients aged 60 years and above with intertrochanteric fractures admitted to our tertiary institution in each of the years 2004, 2007, 2010, and 2013 were identified and included. Patient information was obtained from the hospital’s hip registry and patient electronic medical records. Patients below 60 years of age and patients with unavailable initial radiographs, pathological, and periprosthetic fractures were excluded. Subtrochanteric fractures, atypical femoral fractures, occult intertrochanteric fractures, and polytrauma patients were also excluded from our study.
Data recorded included patient variables: age, sex, ethnicity, and comorbidities. All plain X-ray radiographs were classified preoperatively by the first author (JT) and corroborated by the senior author (EBKK). Intertrochanteric fractures 31-A1.1 through 31-A2.1 were grouped as stable intertrochanteric fractures as per the AO/Orthopaedic Trauma Association (OTA) classification, while 31-A2.2 through 31-A3.3 were labelled as unstable intertrochanteric fractures. A stable fracture is one that is compressed and minimally impacted and shortened by the weight-bearing force of a single-leg stance after reduction and fixation. Stability of these fractures is contributed by both the lateral cortical buttress beneath the vastus ridge, as well as the posteromedial calcar. Compromise of either of the above cortical regions will contribute to fracture instability.3) This was the primary outcome variable in the study. Inpatient outcome variables were secondary outcomes and data reviewed included HLOS, mode of treatment, time between admission and surgery, if it was performed, as well as the type of surgical implant used. The decision on the type of surgical implant used was made by the attending consultant in charge of the respective case at that time.
Statistical Analysis
Statistical analysis was performed with IBM SPSS ver. 20.0 (IBM Corp., Armonk, NY, USA). All categorical variables were represented as numbers and percentages. Continuous variables were reported as mean with standard deviation and median (interquartile range). Fisher’s exact test or chi-square test was used as required to analyze categorical variables. For a comparison of continuous variables in more than two groups, either Kruskal-Wallis test or one-way analysis of variance was employed. A p ≤ 0.05 was considered as statistically significant for all tests in the study.
RESULTS
Demographics
After application of our inclusion and exclusion criteria, 400 patients were identified and included. The mean age was 80.5 ± 8.8 years with range of 60 to 104 years. Female patients accounted for 62.5% (n = 250) and 37.5% (n = 150) were male patients. There was an overall minor increase in the proportion of male elderly patients sustaining intertrochanteric fractures over the study period. However, there was no significant trend with regards to the sex or age of these patients (p > 0.05) (Table 1).
Table 1. Patient Demographics.
| Variable | Total | Year of sampling (%) | p-value | ||||
|---|---|---|---|---|---|---|---|
| 2004 | 2007 | 2010 | 2013 | ||||
| Sex | 0.626 | ||||||
| Male | 150 (37.5) | 35 | 36 | 36 | 43 | ||
| Female | 250 (62.5) | 65 | 64 | 64 | 57 | ||
| Age (yr) | |||||||
| Range | 60–104 | 60.6–96.2 | 60.8–98.8 | 60–94.6 | 61.2–104 | ||
| Mean ± SD | 80.5 ± 8.8 | 80.8 ± 9.3 | 80.1 ± 8.3 | 79.4 ± 8.4 | 81.7 ± 9.1 | 0.266 | |
| Median (IQR) | 81.1 (74.6–87.1) | 82.0 (74.6–87.1) | 80.2 (75.9–86.8) | 80.0 (74.4–85.7) | 83.2 (74.5–87.7) | 0.279 | |
| Ethnicity | 0.360 | ||||||
| Chinese | 339 (84.8) | 88 | 81 | 82 | 88 | ||
| Malay | 25 (6.2) | 5 | 10 | 7 | 3 | ||
| Indian | 29 (7.2) | 7 | 8 | 7 | 7 | ||
| Others | 7 (1.8) | 0 | 1 | 4 | 2 | ||
Values are presented as number (%) unless otherwise indicated.
SD: standard deviation, IQR: interquartile range.
The majority of subjects (84.8%, n = 339) were Chinese, with the rest of the patient population being composed of Malay (6.2%, n = 25), Indian (7.2%, n = 29) and other ethnicities (1.8%, n = 7). This distribution was in line with the demographic makeup of our country. There was no significant trend with regards to ethnicities or comorbidities for the patients in study group over the 10-year period (p > 0.05) (Table 2). An analysis of patient comorbidities also revealed that there was no single disease that showed significant association with patients sustaining unstable intertrochanteric fractures. There was also no association between fracture stability and patients with more than 3 comorbidities.
Table 2. Patient Comorbidities.
| Variable | No. (%) | Year of sampling (%) | p-value | ||||
|---|---|---|---|---|---|---|---|
| 2004 | 2007 | 2010 | 2013 | ||||
| Comorbidity | |||||||
| Diabetes | 137 (34.3) | 29 | 38 | 39 | 31 | 0.345 | |
| Hypertension | 260 (65) | 55 | 67 | 69 | 69 | 0.113 | |
| Cardiac disease | 93 (23.3) | 17 | 30 | 18 | 28 | 0.056 | |
| Renal disease | 37 (9.3) | 5 | 11 | 10 | 11 | 0.400 | |
| Pulmonary disease | 50 (12.5) | 13 | 14 | 11 | 12 | 0.928 | |
| Previous stroke | 92 (23) | 23 | 24 | 21 | 24 | 0.953 | |
| Patients with > 3 comorbidities (%) | 0.390 | ||||||
| Yes | 34 (8.5) | ||||||
| Stable fracture | 21 (9.6) | ||||||
| Unstable fracture | 13 (7.2) | ||||||
| No | 366 (91.5) | ||||||
| Stable fracture | 198 (90.4) | ||||||
| Unstable fracture | 168 (92.8) | ||||||
Primary Outcome
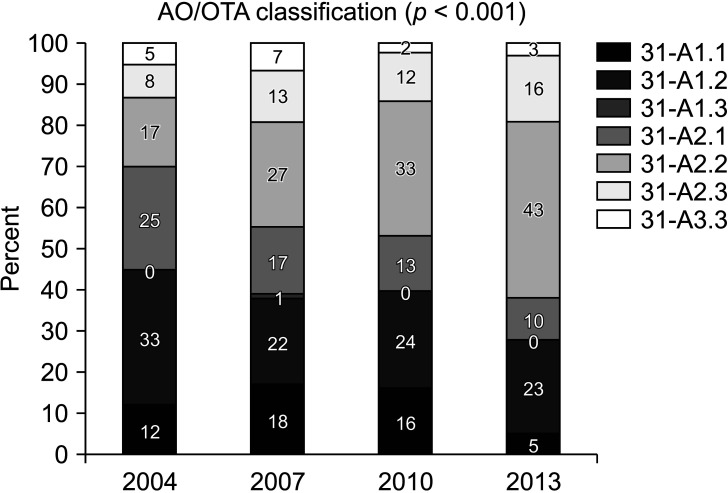
Fig. 1 shows the breakdown of fracture classification using the AO/OTA classification across the four different years analyzed. The table highlights that the proportion of hip fractures of the 31-A2.1 subtype group decreased, while the 31-A2.2 and 31-A2.3 groups increased over the 10-year study period. The number of hip fractures within the 31-A3 subtype group remained largely similar. There was a significant trend (p < 0.001) of increasing comminuted fractures over the 10-year period. Likewise, there was a decrease in the overall incidence of simple intertrochanteric fractures over the similar period. When these fractures were grouped into stable and unstable fractures, there was a statistically significant increase in the number of unstable fractures over the 10-year period (p < 0.01) (Fig. 2).
Fig. 1. Trend of intertrochanteric fracture morphology. OTA: Orthopaedic Trauma Association.
Fig. 2. Trend of stable versus unstable intertrochanteric fractures: significant increase in unstable fractures (p < 0.001).
Further subgroup analysis was performed to identify trends between the ages of patients and fracture stability over the four separate years that were analyzed. Patients were stratified into four separate age groups based on deciles, and the proportion of stable versus unstable intertrochanteric fractures was evaluated. There was a distinct overall increase in unstable fracture configuration across all four age groups in each of the 4 study years being analyzed, with the trend being significant in the oldest group of patients aged 90 years and above (p = 0.034).
Secondary Outcomes
Over the 10-year period, there was a trend toward increasing usage of intramedullary implants for fixation of intertrochanteric fractures as demonstrated in Table 3 (p < 0.001). In 2004, the Gamma nail (Stryker, Mahwah, NJ, USA) was the only choice of implant for intramedullary nail fixation. The complete absence of the use of intramedullary fixation in 2007 was due to the company withdrawing technical support for the implant in our country. The Proximal Femoral Nail Antirotation (Synthes, Oberdorf, Switzerland) was introduced in 2009 and became available for use in subsequent years.
Table 3. Secondary Overcome Variables.
| Patient outcome variable | Overall | 2004 | 2007 | 2010 | 2013 | p-value | |
|---|---|---|---|---|---|---|---|
| Length of stay (day) | |||||||
| Range | 2–89 | 2–36 | 4–47 | 5–45 | 2–89 | ||
| Mean ± SD | 15.3 ± 8.6 | 17.2 ± 6.7 | 16.3 ± 8.3 | 13.9 ± 7.0 | 13.8 ± 11.2 | 0.007 | |
| Median (IQR) | 13 (10–19) | 17 (12–20) | 15 (10–20) | 12 (10–17) | 10 (8–15) | < 0.001 | |
| Time taken to surgery (day) | n = 304 | n = 79 | n = 66 | n = 81 | n = 78 | ||
| Range | 0–26 | 0–21 | 0–26 | 0–13 | 0–11 | ||
| Mean ± SD | 4.3 ± 3.4 | 4.5 ± 3.7 | 5.8 ± 4.3 | 4.0 ± 2.8 | 3.1 ± 2.2 | < 0.001 | |
| Median (IQR) | 3 (2–6) | 3 (2–5) | 4.5 (3–8) | 3 (2–6) | 2 (2–4) | < 0.001 | |
| Surgical implant | n = 304 | n = 79 | n = 66 | n = 81 | n = 78 | < 0.001 | |
| Extramedullary | 210 (69.1) | 74 (93.7) | 66 (100) | 59 (72.8) | 11 (14.1) | ||
| Intramedullary | 94 (30.9) | 5 (6.3) | 0 | 22 (27.2) | 67 (85.9) | ||
Values are presented as number (%) unless otherwise indicated.
SD: standard deviation, IQR: interquartile range.
Implant choices for surgical fixation of intertrochanteric hip fractures were further subanalyzed into stable and unstable fractures for the years 2010 and 2013 as these years saw a distinct increase in intramedullary device fixation. Compared to 2010, the use of the intramedullary device for both stable and unstable fracture configurations increased in 2013. At our institution in 2013, unstable fracture configurations were almost exclusively surgically managed with an intramedullary implant (p < 0.001). Stable fractures on the other hand in 2013 were managed both with intra- and extramedullary implants.
The HLOS for the 400 patients was analyzed with the average HLOS showing an overall significant decrease over the 10-year study period (p = 0.007) as shown in Table 3. Among patients who have undergone surgery, the mean time taken to surgery significantly decreased over the 10-year period (p < 0.001) from 4.5 days in 2004 to 3.1 days in 2013.
DISCUSSION
There has been literature analyzing the distribution of stability of intertrochanteric fractures over the recent decades, and these have shown a noticeable slow increase of unstable fractures over the years.7,8) It was shown by Zain Elabdien et al.9) that 65% to 75% of patients with stable intertrochanteric fractures had well-preserved bone. Contrastingly, based on cortical thickness of the thickest diaphyseal portion of the femur via radiological measurements, only 10% to 20% of patients with unstable fractures had well-preserved bone. In their study, they also observed that with increasing age, there were a greater number of comminuted trochanteric fractures. In our study, the pattern of distribution of intertrochanteric fractures between 2004 and 2013 also similarly demonstrated an increase in their complexity across the ages.
More recently, a 2019 Swedish study on radiographic analysis of 2,772 intertrochanteric fractures over a 30-year period showed no statistical difference among the number of stable versus unstable intertrochanteric fractures.10) They, however, did similarly report a trend towards more comminuted fractures in older patients and postulated it to be related to a gradually increasing lifespan, age-dependent inactivity, and possible decrease in bone mineral density. This increase is significant and bodes a worrying trend if the proportion of unstable intertrochanteric fractures continue to rise in the following decades, posing a challenge to accurate fracture reduction and stable surgical fixation.
Patients over our 10-year period did not develop a higher number of or had a great prevalence of comorbidities, indicating their medical fragility was largely unchanged. There has been anecdotal evidence of diabetes, as well as cardiac disease, individually being an independent risk factor for osteoporotic hip fractures.11) It has been proposed that patients with diabetes may have impaired bone quality, but the underlying mechanism and pathophysiology are still unclear. Histomorphometry data obtained in animal models indicate that the disease causes a low bone turnover condition with impaired bone formation and mineral apposition rates.12)
A subgroup analysis of unstable intertrochanteric fractures showed an increase in the proportion of younger patients (age group 60–70 years) sustaining unstable fractures. This led us to question if there was an earlier age onset of osteoporosis compared to a decade ago. Based on the comorbidity data that we collected, we did not find any significant differences in prevalence that could explain the trend towards increasing instability in intertrochanteric fractures at an earlier age. For young adults aged between 20 and 50 years, diagnosis and treatment of osteoporosis in this age population continued to be poorly studied and defined.13) Endocrine and nutritional disorders are a group of diseases that exert a critical influence on remodeling mechanisms of bone, affecting the accretion of bone mineral density and its distribution in both the trabecular and cortical compartments. Corticosteroid treatment, a mainstay of pharmacological therapy for numerous chronic rheumatological disorders, can also precipitate bone loss at a younger age.14)
Many randomized controlled trials and meta-analyses have shown no difference in terms of functional outcomes between intra- and extramedullary devices for intertrochanteric fracture fixation.4,15,16,17,18) Intramedullary fixation has theoretical advantages over extramedullary fixation, as it has been studied to be biomechanically superior, can be inserted via minimally invasive techniques with less damage to surrounding soft tissues, and decreased probability of infection with arguably less operative time. Most studies have focused on radiographic evidence of failure and reoperation rates, without considering patient function. A study by the Canadian Orthopaedic Trauma Society in 2015 showed that intramedullary nails led to significantly less femoral neck shortening in the treatment of unstable intertrochanteric fractures, with almost 1cm more shortening in the DHS group at 12 months. However, this finding did not correlate with any functional impairment in the DHS cohort.16) A recent study that was sufficiently powered and randomized to comprehensively compare internal fixation of 1,000 patients with trochanteric fractures via a sliding hip screw or an intramedullary nail demonstrated no significant difference with regards to the surgery itself or functional result between the above two methods, other than the improved ability for patients to regain mobility for fractures fixed with an intramedullary nail.17) With specific regards to unstable trochanteric fractures, another recent larger retrospective study analyzing 3,230 unstable trochanteric fractures (AO/OTA type 31-A2) showed that the use of a cephalomedullary nail conveyed the best results in functional outcomes and lowest revision rates over a 12-month follow-up period when compared with an isolated DHS and a DHS combined with a trochanteric stabilization plate. This study also demonstrated an increased use of cephalomedullary nails over time with a concomitant reduction in DHS use.19)
Our study has demonstrated a dramatic shift towards the use of intramedullary implants over the 10-year study period compared to extramedullary devices. This trend is partly explained by the increasing instability of intertrochanteric fractures over the study period, in concordance with the increasing proportion of intramedullary implants as the surgical implant of choice for treatment of intertrochanteric hip fractures in our tertiary institution in later years. Similarly, the use of intramedullary implants steadily increased in North America from 3% to 67% between 1999 and 2006.20)
In our study, there was a disproportionate increase in intramedullary nail use compared to the increase in unstable fracture distribution as illustrated in Fig. 3. We believe this observation may have been driven by market forces, rather than its indicated use in unstable fractures. Prior documented studies show that the intramedullary nail has not shown to be the superlative implant compared to the DHS for majority of intertrochanteric fractures with regards to functional outcomes, especially stables ones.4,5,6,15,16,17,18) With a lack of consistent literature to show decreased complications or improved patient outcomes, most studies do not support the use of an intramedullary device over a sliding hip screw for mechanically stable intertrochanteric fractures.
Fig. 3. Trend of unstable fractures versus intramedullary nail fixation.
With regards to cost-effectiveness analysis of fixation options for intertrochanteric hip fractures, previous studies have reinforced the traditional belief that the sliding hip screw fixation is a more cost-effective implant for distinctly stable fractures (AO/OTA type 31-A1), whereas intramedullary nail fixation is the preferred surgical option for clearly unstable fractures (AO/OTA type 31-A3). AO/OTA type 31-A2 intertrochanteric fractures are understandably more difficult to predict in terms of failure risk and it was proposed that, within the range of failure rates reported in the literature, the more cost-saving surgical option on average would be the sliding hip screw.21) Although intramedullary nailing does provide some advantage in terms of decreasing the risk of failure, multiple meta-analysis results have shown it is unlikely that the extent of this advantage is significant enough to make the intramedullary nail surgical option the more cost-effective implant.22)
In our study, the HLOS and time taken to surgery both significantly decreased over the 10-year duration (p < 0.05). A meta-analysis by Moja et al.23) showed that elderly patients operated within the first 2 days from hospital admission for hip fractures had significantly less early mortality rates compared to patients undergoing hip surgery after the second day. This association remained consistently significant in their study, even after adjusting for age, sex prevalence, location and year of the study. For our institution, an Integrated Hip Fracture Care Pathway initiated in 2011 sought to improve care by having a combined orthogeriatric service with integrated patient care managers. This greatly expedited surgery for hip fractures to within 48 hours, therefore reducing the wait before surgery significantly between 2010 and 2013, as well as the HLOS.
There are some limitations to our study. Firstly, it is a retrospective descriptive study limited to a single tertiary institution in our country, and hence has inherent flaws. Data such as subsequent functional or clinical outcomes of the patients were not collected as part of the study design. Also, bone mineral density scans were not performed routinely for hip fracture patients until the late 2000s, hence we were not able to complete data collection for details of bone density measurement and utilize this for further subanalysis in our study, which would be useful comparing the stability of fractures against bone density scores. Lastly, the earlier highlighted absence of intramedullary nail use in the year 2007 is acknowledged to weaken statistical power of the study, but it should be noted it did not affect the overall trend in the study.
The strength of our study is that we presented a 10-year analysis of the management of intertrochanteric fractures across the spectrum of fracture stability, without financial incentivisation or bias. This is an original article in its methodology and while other studies also looked at implant trends, no other study looked at associated trends in fracture configuration compared to patient demographics. Our study also presented the requirement for a randomized high-quality controlled trial to further investigate if the increasing trend of intramedullary nail use in the treatment of intertrochanteric fractures is in concordance with an associated decrease in fracture stability.
In this study, we found that there was an increasing proportion of unstable intertrochanteric fractures over the 10-year period of the study, with patient demographics being unchanged across the same period. However, this trend was associated with a disproportionately greater tendency to fix these fractures with intramedullary implants.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7(5):407–413. doi: 10.1007/pl00004148. [DOI] [PubMed] [Google Scholar]
- 2.Fox KM, Magaziner J, Hebel JR, Kenzora JE, Kashner TM. Intertrochanteric versus femoral neck hip fractures: differential characteristics, treatment, and sequelae. J Gerontol A Biol Sci Med Sci. 1999;54(12):M635–M640. doi: 10.1093/gerona/54.12.m635. [DOI] [PubMed] [Google Scholar]
- 3.Socci AR, Casemyr NE, Leslie MP, Baumgaertner MR. Implant options for the treatment of intertrochanteric fractures of the hip: rationale, evidence, and recommendations. Bone Joint J. 2017;99(1):128–133. doi: 10.1302/0301-620X.99B1.BJJ-2016-0134.R1. [DOI] [PubMed] [Google Scholar]
- 4.Adams CI, Robinson CM, Court-Brown CM, McQueen MM. Prospective randomized controlled trial of an intramedullary nail versus dynamic screw and plate for intertrochanteric fractures of the femur. J Orthop Trauma. 2001;15(6):394–400. doi: 10.1097/00005131-200108000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Ahrengart L, Tornkvist H, Fornander P, et al. A randomized study of the compression hip screw and Gamma nail in 426 fractures. Clin Orthop Relat Res. 2002;(401):209–222. doi: 10.1097/00003086-200208000-00024. [DOI] [PubMed] [Google Scholar]
- 6.Baumgaertner MR, Curtin SL, Lindskog DM. Intramedullary versus extramedullary fixation for the treatment of intertrochanteric hip fractures. Clin Orthop Relat Res. 1998;(348):87–94. [PubMed] [Google Scholar]
- 7.Martinez AA, Cuenca J, Panisello JJ, Herrera A, Tabuenca A, Canales V. Changes in the morphology of hip fractures within a 10-year period. J Bone Miner Metab. 2001;19(6):378–381. doi: 10.1007/s007740170008. [DOI] [PubMed] [Google Scholar]
- 8.Lakstein D, Hendel D, Haimovich Y, Feldbrin Z. Changes in the pattern of fractures of the hip in patients 60 years of age and older between 2001 and 2010: a radiological review. Bone Joint J. 2013;95(9):1250–1254. doi: 10.1302/0301-620X.95B9.31752. [DOI] [PubMed] [Google Scholar]
- 9.Zain Elabdien BS, Olerud S, Karlstrom G. The influence of age on the morphology of trochanteric fracture. Arch Orthop Trauma Surg. 1984;103(3):156–161. doi: 10.1007/BF00435546. [DOI] [PubMed] [Google Scholar]
- 10.Farhang M, Mukka S, Bergstrom U, Svensson O, Sayer-Noor AS. The trend of radiological severity of hip fractures over a 30 years period: a cohort study. BMC Musculoskelet Disord. 2019;20(1):358. doi: 10.1186/s12891-019-2739-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tan WL, Low SL, Shen L, Das De S. Osteoporotic hip fractures: 10-year review in a Singaporean hospital. J Orthop Surg (Hong Kong) 2015;23(2):150–154. doi: 10.1177/230949901502300206. [DOI] [PubMed] [Google Scholar]
- 12.Napoli N, Schwartz AV, Palermo L, et al. Risk factors for subtrochanteric and diaphyseal fractures: the study of osteoporotic fractures. J Clin Endocrinol Metab. 2013;98(2):659–667. doi: 10.1210/jc.2012-1896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferrari S, Bianchi ML, Eisman JA, et al. Osteoporosis in young adults: pathophysiology, diagnosis, and management. Osteoporos Int. 2012;23(12):2735–2748. doi: 10.1007/s00198-012-2030-x. [DOI] [PubMed] [Google Scholar]
- 14.Feng X, McDonald JM. Disorders of bone remodeling. Annu Rev Pathol. 2011;6:121–145. doi: 10.1146/annurev-pathol-011110-130203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reindl R, Harvey EJ, Berry GK, Rahme E Canadian Orthopaedic Trauma Society (COTS) Intramedullary versus extramedullary fixation for unstable intertrochanteric fractures: a prospective randomized controlled trial. J Bone Joint Surg Am. 2015;97(23):1905–1912. doi: 10.2106/JBJS.N.01007. [DOI] [PubMed] [Google Scholar]
- 16.Babhulkar S. Unstable trochanteric fractures: issues and avoiding pitfalls. Injury. 2017;48(4):803–818. doi: 10.1016/j.injury.2017.02.022. [DOI] [PubMed] [Google Scholar]
- 17.Kaplan K, Miyamoto R, Levine BR, Egol KA, Zuckerman JD. Surgical management of hip fractures: an evidence-based review of the literature. II: intertrochanteric fractures. J Am Acad Orthop Surg. 2008;16(11):665–673. doi: 10.5435/00124635-200811000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Parker MJ. Sliding hip screw versus intramedullary nail for trochanteric hip fractures: a randomised trial of 1000 patients with presentation of results related to fracture stability. Injury. 2017;48(12):2762–2767. doi: 10.1016/j.injury.2017.10.029. [DOI] [PubMed] [Google Scholar]
- 19.Tucker A, Donnelly KJ, Rowan C, McDonald S, Foster AP. Is the best plate a nail? A review of 3230 unstable intertrochanteric fractures of the proximal femur. J Orthop Trauma. 2018;32(2):53–60. doi: 10.1097/BOT.0000000000001038. [DOI] [PubMed] [Google Scholar]
- 20.Anglen JO, Weinstein JN American Board of Orthopaedic Surgery Research Committee. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice: a review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg Am. 2008;90(4):700–707. doi: 10.2106/JBJS.G.00517. [DOI] [PubMed] [Google Scholar]
- 21.Swart E, Makhni EC, Macaulay W, Rosenwasser MP, Bozic KJ. Cost-effectiveness analysis of fixation options for intertrochanteric hip fractures. J Bone Joint Surg Am. 2014;96(19):1612–1620. doi: 10.2106/JBJS.M.00603. [DOI] [PubMed] [Google Scholar]
- 22.Parker MJ, Handoll HH. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev. 2010;(9):CD000093. doi: 10.1002/14651858.CD000093.pub3. [DOI] [PubMed] [Google Scholar]
- 23.Moja L, Piatti A, Pecoraro V, et al. Timing matters in hip fracture surgery: patients operated within 48 hours have better outcomes. A meta-analysis and meta-regression of over 190,000 patients. PLoS One. 2012;7(10):e46175. doi: 10.1371/journal.pone.0046175. [DOI] [PMC free article] [PubMed] [Google Scholar]