Figure 9.
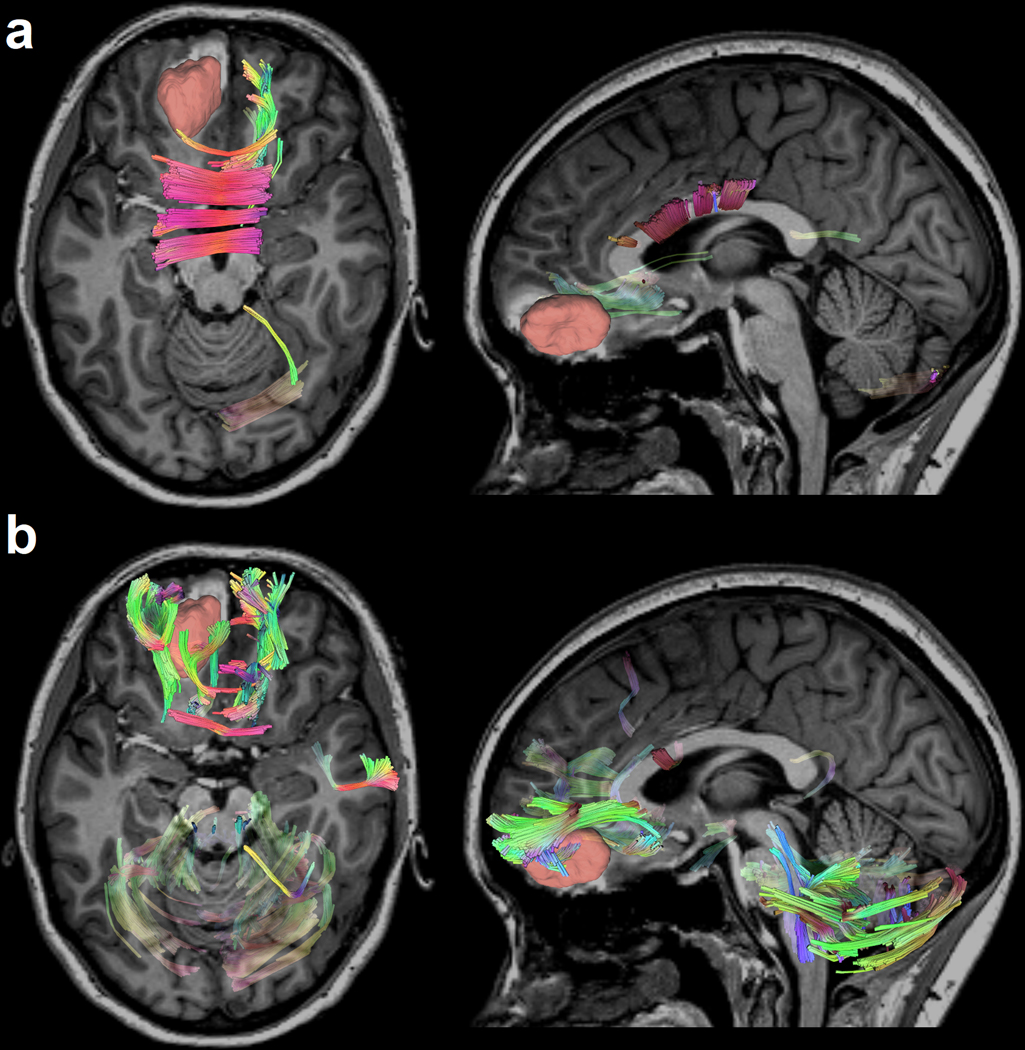
Differential tractography of a 19-year-old female TBI patient highlighting the exact segments of neuronal pathways with anisotropy changes between a baseline scan acquired acutely (i.e., within a week after injury) and a follow-up scan (approximately 6 months post-TBI). The patient features a relatively large primary lesion located in the left orbitofrontal cortex, which is particularly vulnerable to TBI. Differential tractography (Yeh et al., 2019) tracks the precise segments of pathways exhibiting (a) FA decreases of more than 5% relative to the acute baseline and (b) quantitative anisotropy (QA) decreases of more than 15% relative to the same baseline. Directional coding is used to color the tractogram (left-right: red; anterior-posterior: green; superior-inferior: blue). The results reveal perilesional tracts and the genu of the corpus callosum (CC), which is the CC portion closest to the primary lesion (red). Traumatic axonal injury (TAI) of the CC is prevalent in TBI and can be explained by the interaction of TBI kinematics with the biomechanics of cerebral displacement within the cranial cavity (Hill et al., 2016). The decrease in cerebellar FA and QA is consistent with previous findings, according to which cerebellar volume and connectivity are both frequently and substantially affected by moderate and severe TBI regardless of primary injury location (Spanos et al., 2007). Although this fact is well documented (Caeyenberghs et al., 2011; Irimia et al., 2012; Park et al., 2006), its causal mechanisms are poorly understood and may be related to cerebellar involvement in motor coordination, control, and other brain functions. These functions are frequently and substantially impacted both by the primary injury and by decreases in TBI patients’ abilities to carry out daily living activities as they recover. New tractography modalities like differential tractography may offer novel strategies to investigate white matter pathways and to answer outstanding questions in TBI research.
